Abstract
Purpose
The aim of our study was to establish a safe and convenient diagnostic method for acute gastrointestinal (GI) graft-versus-host disease (GVHD) in children by determining the sensitivity and negative predictive values of upper and lower endoscopic biopsies for children suspected of GI GVHD.
Methods
Patients suspected of GI GVHD who received endoscopic evaluation within 100 days after stem cell transplantation and endoscopies between January 2012 and March 2014 in Seoul National University Children's Hospital were included in our study.
Results
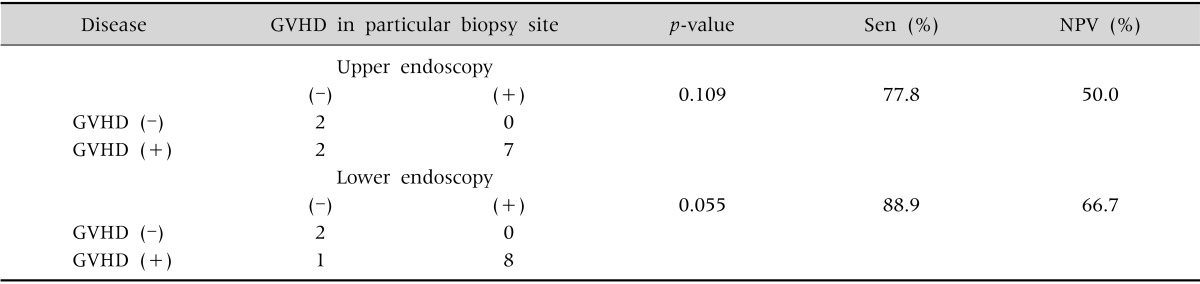
Fifteen patients with a total of 20 endoscopic procedures were included in our study. Sensitivity at the esophagus, stomach, and duodenum were 22.2%, 30.0%, and 80.0%, respectively. Negative predictive values at the esophagus, stomach, and duodenum were 22.2%, 30.0%, and 60.0%, respectively. Overall sensitivity and negative predictive values of upper endoscopic biopsy for GVHD were 77.8% and 50.0%, respectively. Overall sensitivity and negative predictive values of lower endoscopic biopsy for GVHD were 88.9% and 66.7%, respectively.
Conclusion
We recommend flexible sigmoidoscopy as a safe and accurate diagnostic tool for GVHD, similar to other studies reported previously. However, if there is no evidence of GVHD on sigmoidoscopy with high index of suspicion of GI bleeding, full colonoscopy and upper endoscopy should be considered.
Keywords: Graft-versus-host disease, Child, Endoscopy
INTRODUCTION
Acute graft-versus-host disease (GVHD) occurs within first 100 days after transplantation [1,2]. Severe acute GVHD results in significant morbidity and mortality. It is the major cause of treatment failure in patients undergoing transplantation for low-risk malignancy [2,3].
Acute GVHD involving intestinal tracts presents with non-specific symptoms such as secretory diarrhea, nausea, vomiting, anorexia, weight loss, and abdominal pain [1,4]. In severe acute GVHD, diarrhea can be copious. Bleeding, painful cramping, and ileus may result from mucosal ulceration [2,4,5].
Symptoms of gastrointestinal (GI) GVHD are not specific. Diagnosis of GI GVHD is often inaccurate based on clinical manifestation alone. Therefore, a definite diagnosis of GVHD requires histological confirmation [1,6,7]. However, there is still controversy on the best diagnostic strategy for GI GVHD in children [8,9,10]. Previous studies have reported that rectosigmoid biopsy is a preferred procedure for diagnosing GI GVHD in children [8,10].
The aim of our study was to establish a safe and convenient diagnostic method for acute GI GVHD in children by evaluating the sensitivity and negative predictive values of upper and lower endoscopic biopsies for children with suspected GI GVHD.
MATERIALS AND METHODS
Patients
Patients suspected of GI GVHD who received endoscopic evaluation within 100 days after stem cell transplantation (SCT) and endoscopies between January 2012 and March 2014 in Seoul National University Children's Hospital (Seoul, Korea) were included in our study. Age, gender, underlying disease, transplantation type, symptom promoting endoscopic biopsy, endoscopic findings, pathologic findings of endoscopic biopsies, skin biopsies, and liver biopsies were extracted from the patient's medical records. Stool Clostridium difficile toxin examination and stool bacterial culture were performed for some patients. Our study was approved by the Institutional Review Board of our hospital (IRB No. 1501-038-639).
Gastrointestinal endoscopy and biopsy
All patient's blood samples were obtained to determine complete blood cell count, prothrombin time, and activated partial prothrombin time before procedures to prevent possibility of bleeding. Prophylactic antibiotics were not used routinely.
During esophagogastroduodenoscopy (EGD), biopsies were obtained from the following segments: esophagus, stomach, and duodenum second portion for all patients except one who did not receive esophageal biopsy. When patients had GI bleeding, we carried out EGDs as well as full colonoscopies if bowel preparation was sufficient. We classified lower endoscopic biopsies into the following three biopsy groups: cecum, colon, and rectosigmoid colon. Endoscopic findings were classified based on endoscopic diagnosis of GI GVHD [11].
Histological criteria for intestinal GVHD
Diagnostic criterion for GVHD was the presence of epithelial single-cell apoptosis [1,6,7]. This pattern of mucosal damage can be observed in the immediate post transplantation period (within 20 days) due to toxic effect of conditioning chemotherapy on gut epithelium [1]. In our study, a GI pathologist reviewed all specimens to confirm the diagnosis of GVHD. We considered a case as GI GVHD even if there was just a single endoscopic biopsy result showing a compatible reading with GVHD. Some specimens underwent cytomegaloviral (CMV) immunohistochemical (IHC) study.
Statistical analysis
All dichotomous variables were analyzed with Fisher's exact test. IBM SPSS Statistics version 21.0 for Windows (IBM Co., Armonk, NY, USA) was used for statistical analysis. A p-value less than 0.05 was considered as statistically significant.
We also evaluated the sensitivity and negative predictive values of both upper and lower endoscopic biopsies.
RESULTS
Patient characteristics
A total of 15 patients with suspected GI GVHD were included in our study. Patient demographic characteristics are summarized in Table 1. Median time of endoscopic biopsies following SCT was 34 (range, 19–61) days. The most common underlying diseases were acute myeloid leukemia (40.0%) and other leukemias 46.7% (1+3+1+1+1/15=46.666%).
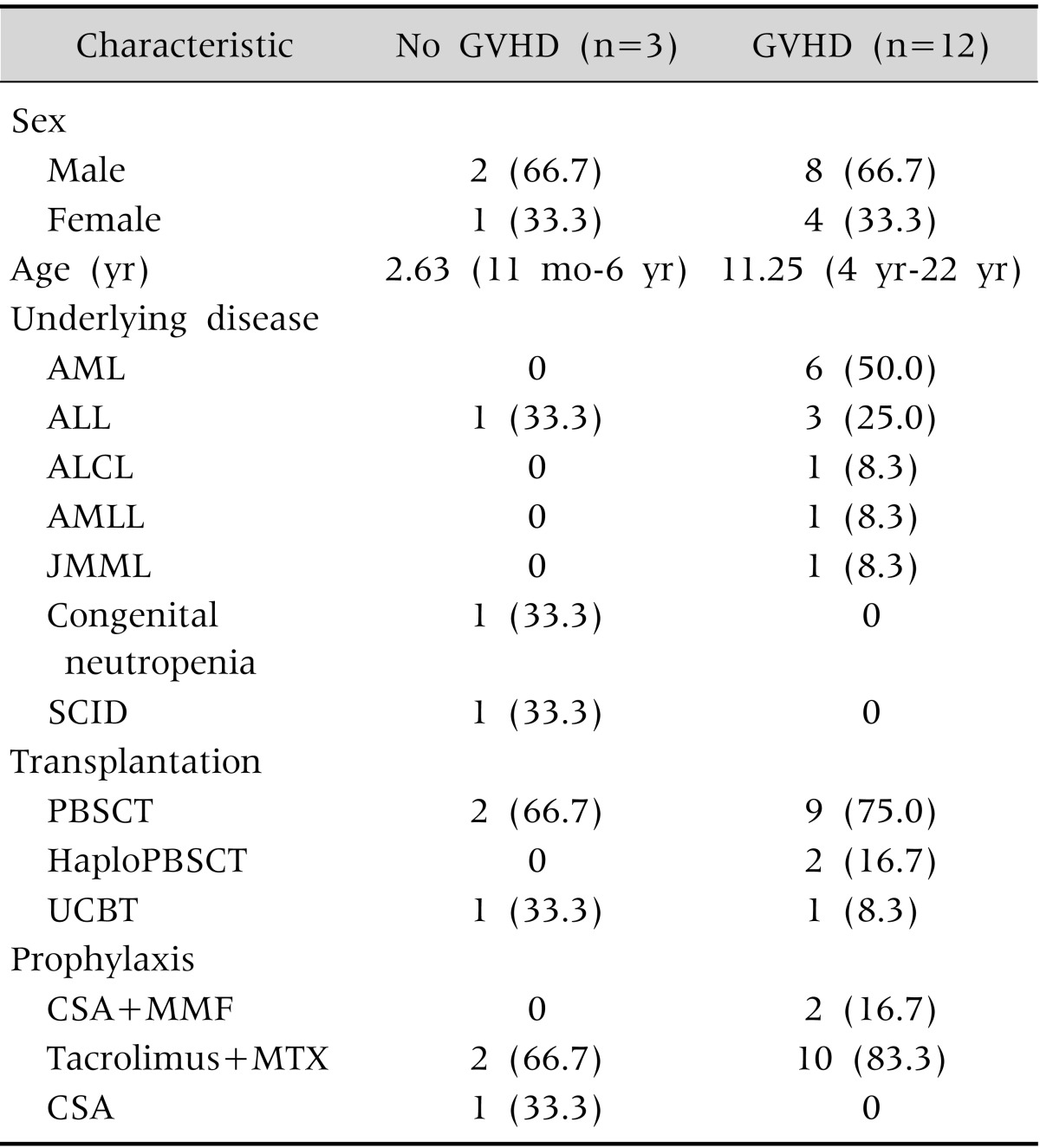
Table 1. Patient Demographic Characteristics (n=15).
Values are presented as number (percentage within group) or median (range).
GVHD: graft-versus-host disease, AML: acute myeloid leukemia, ALL: acute lymphoid leukemia, ALCL: anaplastic large cell lymphoma, AMLL: acute mixed lineage leukemia, JMML: juvenile myelomonocytic leukemia, SCID: severe combined immunodefeciency, PBSCT: peripheral blood stem cell transplantation, HaploPBSCT: haploidentical PBSCT, UCBT: umblical cord blood transplantation, CSA: cyclosporin A, MMF: mycophenolate mofetil, MTX: methotrexate.
There was no statistically significant difference in age, sex, underlying disease, kinds of SCT, or prophylactic agents between GVHD group and non-GVHD group (Table 1). Patient numbering and summarization of characteristics are attached in supplementary material. Of the 15 patients enrolled in our study, three received endoscopies twice.
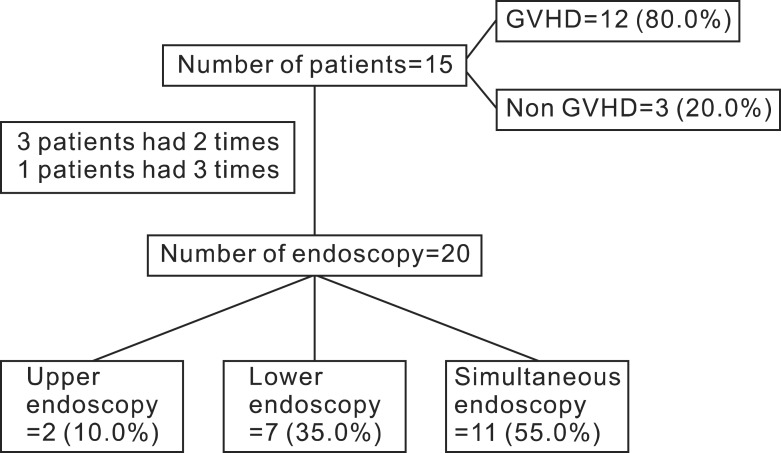
One patient (Patient 6) received it three times. Total count of all endoscopic procedures was 20. GVHD was diagnosed in 12 of 15 (80.0%) patients. The number of patient who received upper endoscopy, lower endoscopy, and simultaneous upper and lower endoscopies were 2 (10.0%), 7 (35.0%), and 11 (55.0%), respectively (Fig. 1).
Fig. 1. Study flow.
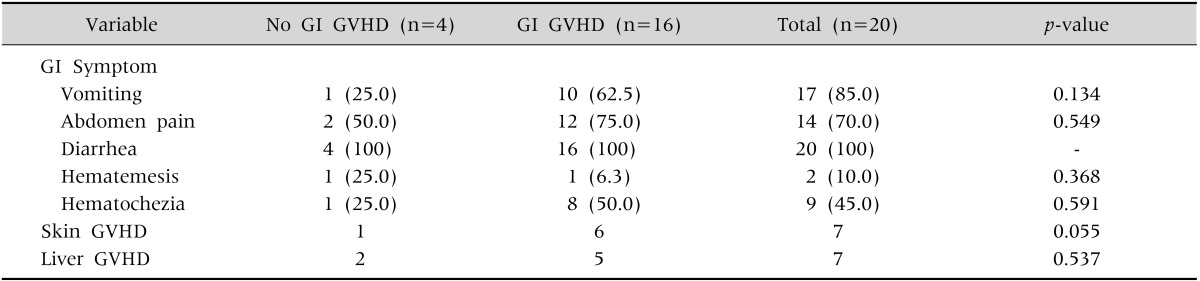
The most common symptoms prompting endoscopic evaluation were diarrhea (100%) and vomiting (85.0%). The most common symptoms of GVHD patients was diarrhea (100%) and vomiting (62.5%). Of skin GVHD patients, there were 6 (85.7%) GI GVHD; of liver GVHD, GI GVHD was 5 (71.4%). Any symptoms of GI GVHD could not be regarded statistically different to the non GVHD cases (Table 2).
Table 2. Association between Presence of GI GVHD and GI Symptoms, Skin GVHD and Liver GVHD.
Values are presented as number (percentage within group) or number only.
GI: gastrointestinal, GVHD: graft-versus-host disease.
Sensitivities and negative predictive values of endoscopic biopsies
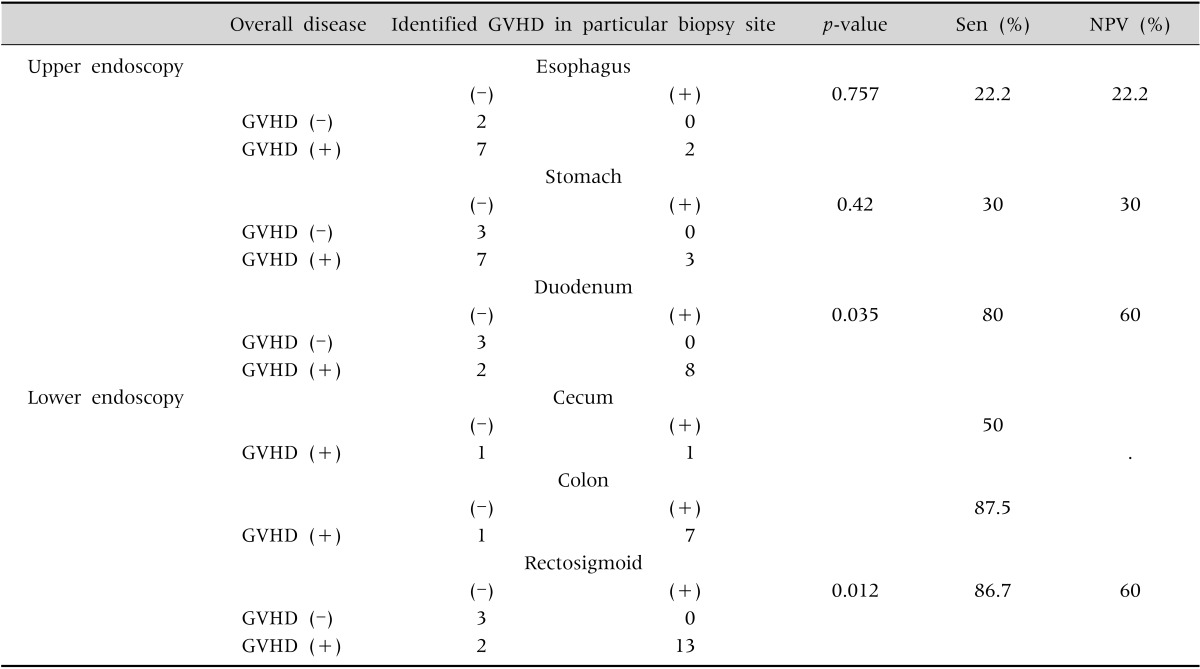
For those who received upper endoscopy, the sensitivity and negative predictive value at the esophagus was both at 22.2%. Both the sensitivity and negative predictive value at the stomach was 30%. The sensitivity and negative predictive value at the duodenum were 80.0% and 60.0%, respectively.
For 18 episodes when lower endoscopy performed, the number of episodes that were intubated at cecum was 5 (27.8%) and hepatic flexure was 2 (11.1%). Of the 5 patients who were intubated at the cecum, two received biopsies, including one who was diagnosed as GVHD. The sensitivity of biopsies obtained in colon was 87.5%. The sensitivity and negative predictive value of rectosigmoid biopsy was 86.7% and 60.0%, respectively (Table 3). The sensitivity of colonic biopsy was not statistically different from the sensitivity of rectosigmoid biopsy.
Table 3. Sensitivity and Negative Predictive Values of Upper and Lower Endoscopic Biopies.
GVHD: graft-versus-host disease, Sen: sensitivity, NPV: negative predictive value.
Eleven of 20 (55.0%) sessions had simultaneous upper and lower endoscopies. We classified biopsy results into two groups: upper and lower endoscopy. The sensitivity and negative predictive value of the upper endoscopic biopsy was 77.8% and 50.0%, respectively. The sensitivity and negative predictive value of the lower endoscopic biopsy was 88.9% and 66.7%, respectively (Table 4).
Table 4. Sensitivities and Negative Predictive Values of Concurrent Endoscopic Biopsies.
GVHD: graft-versus-host disease, Sen: sensitivity, NPV: negative predictive value.
One patient was diagnosed as GVHD only by upper endoscopy. However, he had coincidental CMV colitis in the lower GI tract. In pathologic review, there was no intact epithelial cell in his colonic biopsy specimen. Therefore, diagnosis of GVHD based on the apoptosis in the epithelial cell could not be made. However, colonic GVHD cannot be completely excluded also in this case.
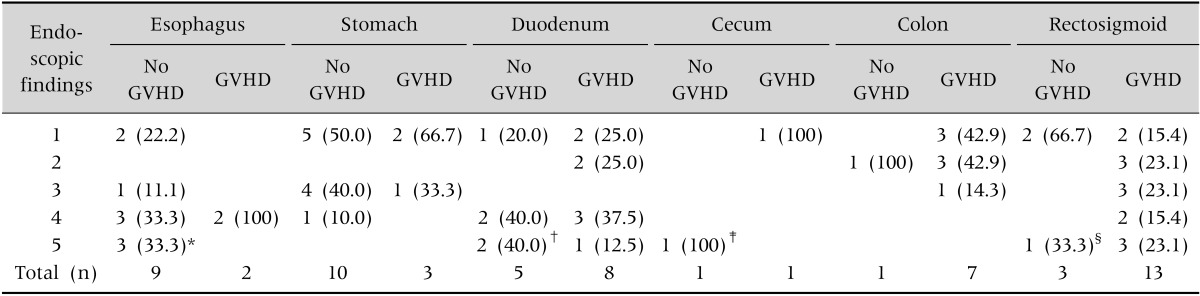
Gross endoscopic findings, serial endoscopic findings, and coinfections
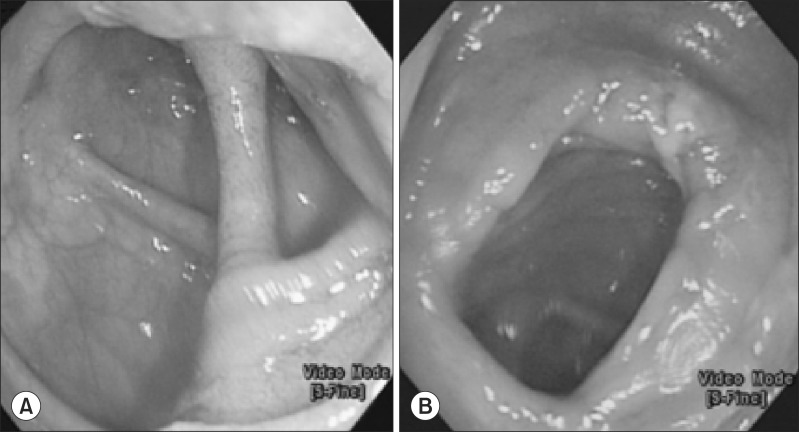
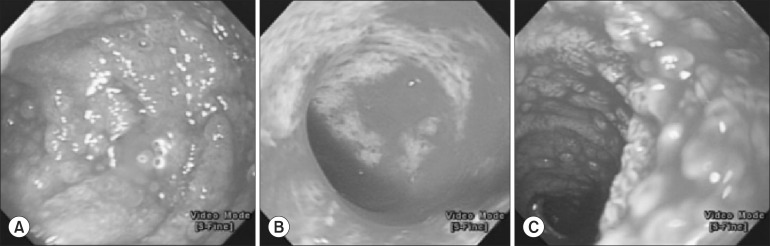
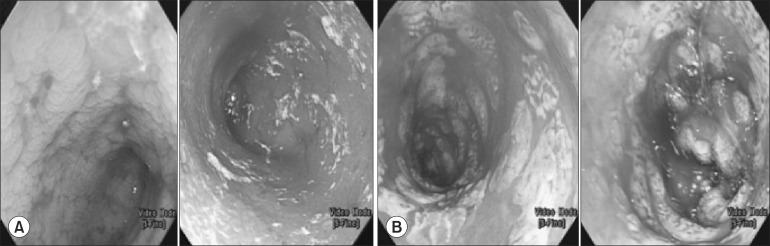
Table 5 shows endoscopic findings according to the Cruz-Correa's classification [11] and the presence of GVHD. There were several segments showing normal mucosa (Fig. 2A) in endoscopy. But there were GVHD in pathology results. The percentage of normal finding was 66.7% at the stomach, 25.0% at duodenum, 100% at cecum, 42.8% at colon, and 16.7% at rectosigmoid. On the other hand, 33.3–100% of non-GVHD patients showed severe ulceration, exudates, and bleeding on their endoscopy without pathologic diagnosis of GVHD. The pathologic findings in severe ulceration without GVHD was CMV typhilitis (Fig. 2B), duodenitis (Fig. 3B and 3C), and colitis (Fig. 4B). Other histologic findings in the severe ulceration segment were inflammatory granulation tissue, ulcer detritus, or acanthotic squamous epithelium.
Table 5. Associations between Endoscopic Findings and Presence of Graft-versus-Host Disease (GVHD).
Values are presented as number (percentage within group) or number only.
1: normal, 2: loss of vascular markings and/or focal mild erythema, 3: moderate edema and/or erythema, 4: edema, erythema, erosions and/or bleeding, 5: ulceration, exudates and bleeding.
*Inflammed granulation tissue, ulcer detritus, acanthotic squamous epithelium; †cytomegaloviral (CMV) duodenitis (Fig. 1B and 1C); ‡CMV typhlitis (Fig. 2B); §CMV sigmoid colitis.
Fig. 2. Cecum endoscopic findings of two patients. (A) It showed normal mucosa with graft-versus-host deisease (Patient 2–2). (B) It showed ulcer and exudate at endoscopy (Patient 12). Cytomegaloviral typhilitis was confirmed at histology.
Fig. 3. Duodenum of three patients. They showed grade 5 ulceration, exudate, and bleeding in endoscopy. (A) Graft-versus-host disease with ulcer (Patient 6–2). (B, C) Cytomegaloviral uodenitis (Patients 14 and 13).
Fig. 4. Serial rectosigmoidoscopic findings of the same patient (Patient 6). (A) It showed gross ulcer, exudates, and bleeding. The patient (Patient 6–1) was diagnosed as graft-versus-host disease (d20). However, steroid therapy failed to relieve his symptoms. (B) It showed d31 sigmoidoscopic finding of the same patient (Patient 6–2) showing exudates and bleeding. He was diagnosed as cytomegaloviral infection.
There are four patients who received serial endoscopy due to persistent symptoms, of which two (Patient 6 and 9) were initially diagnosed as GVHD and received steroid therapy. But their symptoms were persistent. Therefore, a second endoscopic biopsy was performed. Their diagnosis was changed to CMV infection or other nonspecific finding. Therefore, their treatments were also changed. Two patients (Patient 6–2, 12) had coincidental GVHD and CMV infection (upper GI GVHD and lower GI CMV infection). One patient showed duodenal bleeding and perforation after duodenal biopsy. No other complications such as sepsis were reported.
DISCUSSION
Our study provides two new points in the endoscopic diagnosis of GVHD in children. First, we calculated the sensitivity and negative predictive value of each biopsy site and compared them by site. There is no data on sensitivity and negative predictive values of each biopsy site in children. Second, we showed important serial endoscopic biopsy results in the same patients. Therefore, we suggest that serial endoscopy is important in children with the symptoms of GVHD in this complex clinical situation.
Acute GVHD is a major cause of morbidity and mortality in patients undergoing transplantation for low-risk malignancy [2,3,12]. For GI GVHD patients who present with non-specific symptoms such as anorexia, vomiting, abdominal discomfort, and diarrhea, histologic diagnosis of GVHD is important [1,6,7,13]. However, the best diagnostic strategy for GI GVHD in children remains unclear [8,9,10].
In our study, 11 patients had received concurrent upper and lower endoscopy. Sensitivity and negative predictive value revealed that lower endoscopic biopsy was better for diagnosis of GVHD in children than upper endoscopic biopsy. Five patients were diagnosed as GVHD only by lower endoscopy. There was no change of diagnosis in lower endoscopy by additional upper endoscopy except in one patient. This exceptional patient was diagnosed as GVHD by upper endoscopy. He also had severe CMV colitis in lower endoscopy, which could not be evaluated for the presence of GVHD due to severe inflammation. Mortality rate of our GVHD patients was high (40.0%, 6 of 15).
Several previous studies in adults also suggested that biopsy of rectosigmoid colon was the best for diagnosing GI GVHD [14,15]. A prospective study found that the biopsy site with the highest yield was distal colon [16]. Others insist that sigmoidoscopy is the safest and the most productive method of diagnosing acute GVHD in children [8,10]. But in 2012, a retrospective study in children found that rectosigmoid combined with upper endoscopic biopsies were equally sensitive for diagnosis of acute GI GVHD in children [9]. Some authors advocate gastric biopsy and other upper endoscopic biopsies as useful tools for the diagnosis of GI GVHD [4,13,17]. A prospective study conducted from August 2002 to February 2006 at Yale Gastrointestinal Procedure Center [18]. They performed 27 cases of concurrent upper and lower endoscopy for suspected acute GVHD. Their results showed diffuse upper and lower GI involvement of acute GVHD with similar diagnostic yield (sensitivity of stomach, 94.4%; duodenum, 94.4%; colon, 92.8%; rectosigmoid, 88.8%). Although absolute percentages of sensitivity were the highest at duodenum and stomach, there was no significant difference in sensitivity among segments. They recommended to use flexible sigmoidoscopy with rectal biopsy alone in patient who were poor candidates for full colonoscopy.
Biopsy of duodenum is known to have high risk of perforation and bleeding [8,19]. One of our patients showed complications of endoscopic biopsy, duodenal bleeding and perforation. In our study, association between patient's symptoms such as nausea, vomiting, diarrhea, hematochezia, hematemesis, and presence of GI GVHD was not statistically significant. This result is in consistent with results of previous studies [6,10,14]. These symptoms could be present with GI infection, chemotherapy, or medication induced side effects [4].
However, in our study, two patients' histologic findings from the second endoscopic biopsy were differed from those from the first endoscopic biopsy, leading to a change of therapy. A retrospective study has suggested that serial GI endoscopies could affect therapeutic decision-making for patients with persistent diarrhea after SCT [20].
There are many results showing that gross endoscopic findings not correlated with biopsy results [6,7,12,13,17]. However, some studies found high correlation between endoscopic findings and histologically proven GI GVHD [11]. In our results, the most common endoscopic finding of diagnosed GVHD had normal mucosa. Some patients had no GVHD, although they had endoscopic severe ulceration and bleeding. These results suggest that discrepancy between endoscopic finding and histologic assessment can occur. Histologic confirmation of endoscopic biopsy is important for the diagnosis of GVHD.
Our study had several limitations. First, this was a retrospective study with a small number of patients. In addition, CMV IHC was not performed for all cases. Although epithelial single-cell apoptosis can be seen in immediate post transplantation period (within 20 days) due to toxic effect of chemotherapy on gut epithelium [1], one patient had undergone early endoscopy at day 19.
There are many reports that flexible sigmoidoscopy is safe and easy to train [21,22]. In addition, it can be performed without sedation [10,12]. Complication of duodenal biopsy was also reported. Therefore, we also agree that flexible sigmoidoscopy should be regarded as an accurate and safe method for the initial diagnosis of acute GVHD in children.
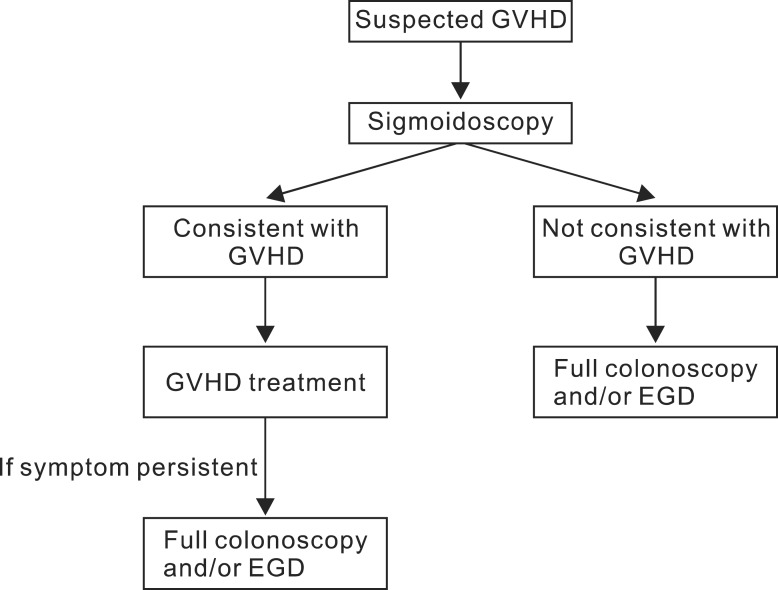
In conclusion, our results suggest that flexible sigmoidoscopy is a safe and accurate diagnostic tool for GVHD. However, if there is no evidence of GVHD on sigmoidoscopy with high index of suspicion of GI GVHD, full colonoscopy and upper endoscopy should be considered (Fig. 5).
Fig. 5. Stepwise endoscopic approaches for pediatric gastrointestinal graft-versus-host disease (GVHD). EGD: esophagogastroduodenoscopy.
Supplementary Material
Patients flow
References
- 1.Iqbal N, Salzman D, Lazenby AJ, Wilcox CM. Diagnosis of gastrointestinal graft-versus-host disease. Am J Gastroenterol. 2000;95:3034–3038. doi: 10.1111/j.1572-0241.2000.03250.x. [DOI] [PubMed] [Google Scholar]
- 2.Couriel D, Caldera H, Champlin R, Komanduri K. Acute graft-versus-host disease: pathophysiology, clinical manifestations, and management. Cancer. 2004;101:1936–1946. doi: 10.1002/cncr.20613. [DOI] [PubMed] [Google Scholar]
- 3.Ferrara JL, Deeg HJ. Graft-versus-host disease. N Engl J Med. 1991;324:667–674. doi: 10.1056/NEJM199103073241005. [DOI] [PubMed] [Google Scholar]
- 4.Wu D, Hockenberry DM, Brentnall TA, Baehr PH, Ponec RJ, Kuver R, et al. Persistent nausea and anorexia after marrow transplantation: a prospective study of 78 patients. Transplantation. 1998;66:1319–1324. doi: 10.1097/00007890-199811270-00010. [DOI] [PubMed] [Google Scholar]
- 5.Nevo S, Enger C, Swan V, Wojno KJ, Fuller AK, Altomonte V, et al. Acute bleeding after allogeneic bone marrow transplantation: association with graft versus host disease and effect on survival. Transplantation. 1999;67:681–689. doi: 10.1097/00007890-199903150-00007. [DOI] [PubMed] [Google Scholar]
- 6.Roy J, Snover D, Weisdorf S, Mulvahill A, Filipovich A, Weisdorf D. Simultaneous upper and lower endoscopic biopsy in the diagnosis of intestinal graft-versus-host disease. Transplantation. 1991;51:642–646. doi: 10.1097/00007890-199103000-00019. [DOI] [PubMed] [Google Scholar]
- 7.Xu CF, Zhu LX, Xu XM, Chen WC, Wu DP. Endoscopic diagnosis of gastrointestinal graft-versus-host disease. World J Gastroenterol. 2008;14:2262–2267. doi: 10.3748/wjg.14.2262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khan K, Schwarzenberg SJ, Sharp H, Jessurun J, Gulbahce HE, Defor T, et al. Diagnostic endoscopy in children after hematopoietic stem cell transplantation. Gastrointest Endosc. 2006;64:379–385. doi: 10.1016/j.gie.2005.08.040. quiz 389-92. [DOI] [PubMed] [Google Scholar]
- 9.Sultan M, Ramprasad J, Jensen MK, Margolis D, Werlin S. Endoscopic diagnosis of pediatric acute gastrointestinal graft-versus-host disease. J Pediatr Gastroenterol Nutr. 2012;55:417–420. doi: 10.1097/MPG.0b013e31825048eb. [DOI] [PubMed] [Google Scholar]
- 10.Crowell KR, Patel RA, Fluchel M, Lowichik A, Bryson S, Pohl JF. Endoscopy in the diagnosis of intestinal graft-versus-host disease: is lower endoscopy with biopsy as effective in diagnosis as upper endoscopy combined with lower endoscopy? Pediatr Blood Cancer. 2013;60:1798–1800. doi: 10.1002/pbc.24634. [DOI] [PubMed] [Google Scholar]
- 11.Cruz-Correa M, Poonawala A, Abraham SC, Wu TT, Zahurak M, Vogelsang G, et al. Endoscopic findings predict the histologic diagnosis in gastrointestinal graftversus-host disease. Endoscopy. 2002;34:808–813. doi: 10.1055/s-2002-34257. [DOI] [PubMed] [Google Scholar]
- 12.Yeh SP, Liao YM, Hsu CH, Chen CL, Shen YC, Hsueh CT, et al. Gastric bleeding due to graft-vs-host disease: discrepancy between endoscopic and histologic assessment. Am J Clin Pathol. 2004;122:919–925. doi: 10.1309/23DA-L9F6-P74X-WJHL. [DOI] [PubMed] [Google Scholar]
- 13.Velasco-Guardado A, López-Corral L, Alvarez-Delgado A, Flores-Corral T, Geijo-Martnez F, Caballero-Barrigón D, et al. Endoscopic evaluation and histological findings in graft-versus-host disease. Rev Esp Enferm Dig. 2012;104:310–314. doi: 10.4321/s1130-01082012000600005. [DOI] [PubMed] [Google Scholar]
- 14.Ross WA, Ghosh S, Dekovich AA, Liu S, Ayers GD, Cleary KR, et al. Endoscopic biopsy diagnosis of acute gastrointestinal graft-versus-host disease: rectosigmoid biopsies are more sensitive than upper gastrointestinal biopsies. Am J Gastroenterol. 2008;103:982–989. doi: 10.1111/j.1572-0241.2007.01639.x. [DOI] [PubMed] [Google Scholar]
- 15.Oomori S, Takagi S, Kikuchi T, Utsunomiya K, Yokoyama H, Negoro K, et al. Significance of colonoscopy in patients with intestinal graft-versus-host disease after hematopoietic stem cell transplantation. Endoscopy. 2005;37:346–350. doi: 10.1055/s-2005-861049. [DOI] [PubMed] [Google Scholar]
- 16.Thompson B, Salzman D, Steinhauer J, Lazenby AJ, Wilcox CM. Prospective endoscopic evaluation for gastrointestinal graft-versus-host disease: determination of the best diagnostic approach. Bone Marrow Transplant. 2006;38:371–376. doi: 10.1038/sj.bmt.1705453. [DOI] [PubMed] [Google Scholar]
- 17.Ponec RJ, Hackman RC, McDonald GB. Endoscopic and histologic diagnosis of intestinal graft-versus-host disease after marrow transplantation. Gastrointest Endosc. 1999;49:612–621. doi: 10.1016/s0016-5107(99)70390-1. [DOI] [PubMed] [Google Scholar]
- 18.Aslanian H, Chander B, Robert M, Cooper D, Proctor D, Seropian S, et al. Prospective evaluation of acute graft-versus-host disease. Dig Dis Sci. 2012;57:720–725. doi: 10.1007/s10620-011-1938-x. [DOI] [PubMed] [Google Scholar]
- 19.Ramakrishna J, Treem WR. Duodenal hematoma as a complication of endoscopic biopsy in pediatric bone marrow transplant recipients. J Pediatr Gastroenterol Nutr. 1997;25:426–429. doi: 10.1097/00005176-199710000-00012. [DOI] [PubMed] [Google Scholar]
- 20.Martínez C, Rosales M, Calvo X, Cuatrecasas M, Rodriguez-Carunchio L, Llach J, et al. Serial intestinal endoscopic examinations of patients with persistent diarrhea after allo-SCT. Bone Marrow Transplant. 2012;47:694–699. doi: 10.1038/bmt.2011.143. [DOI] [PubMed] [Google Scholar]
- 21.Volonaki E, Sebire NJ, Borrelli O, Lindley KJ, Elawad M, Thapar N, et al. Gastrointestinal endoscopy and mucosal biopsy in the first year of life: indications and outcome. J Pediatr Gastroenterol Nutr. 2012;55:62–65. doi: 10.1097/MPG.0b013e3182478f83. [DOI] [PubMed] [Google Scholar]
- 22.Groveman HD, Sanowski RA, Klauber MR. Training primary care physicians in flexible sigmoidoscopy--performance evaluation of 17,167 procedures. West J Med. 1988;148:221–224. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Patients flow