Abstract
Curtisia dentata is used in African traditional medicine to treat variety of infections. C. dentata leaves were collected from Buffelskloof Nature Reserve, South Africa. The ethanol, chloroform, ethyl acetate and acetone extracts were evaluated for antimicrobial activity using micro dilution assay against Escherichia coli, Pseudomonas aeruginosa, Mycobacterium smegmatis, Mycoplasma hominis, Candida albicans and some clinical isolates of Moraxella catarrhalis, Proteus mirabilis and Staphylococcus aureus isolated from HIV patient. Acetone extract exhibited lowest MIC of 0.01 mg/ml against Candida albicans compared to other extracts. Besides lupeol, betulinic acid and ursolic acid, β-sitosterol was isolated for the first time from C. dentata leaves and exhibited antimicrobial activity with MIC values ranging from 0.20 to 6.25 mg/ml. Furthermore, the ethanol extract and the four isolated compounds revealed microbicidal effect, with MIC index of less than 4. Ethanol extract revealed the best total activity of 2400 ml/g against Mycoplasma hominis. Cytotoxicity of the isolated compounds was further investigated against the Human embryonic kidney (HEK293) and Human hepatocellular carcinoma (HepG2) cell lines using the MTT assay. Ursolic acid exhibited the lowest LD50 of 122.4 µg/ml against HEK293 cell line while lupeol exhibited LD50 of 278.8 and 289.4 µg/ml against HEK293 and HepG2 respectively. Lupeol exhibited low selectivity index. Ethyl acetate and acetone extracts were further investigated for antioxidant activity against 2,2-diphenyl-1-picrylhydrazyl (DPPH). The acetone extract exhibited potent inhibition of DPPH compared to ethyl acetate extract. The findings of the current work validate the use of the plant species in the treatment of various human infections.
Keywords: Curtisia dentata, ß-sitosterol, ethnomedicine, cytotoxicity, antioxidant, antimicrobial
Introduction
Microbial resistance to common antibiotics is becoming a norm and an enormous threat to general health care facilities, especially in poorer countries with little or improper medical facilities and resources (Marasini et al., 2015[18]; Chovanová et al., 2013[5]; Vigneshwari et al., 2014[49]). The situation is worsened by increase in HIV-AIDS infections, tuberculosis and the defaulting patients in hospitals. Although medicinal plants serves as an alternative medicine to most rural communities, mode of action and their general safety remains unknown. Although pharmacological testing and research on natural products represent a major strategy for discovering and developing new drugs (Priyadharshini and Sujatha, 2013[37]; Nasri and Shirizad, 2013[27]), the cytotoxicity of major plant derived indigenous products used in most remote areas remains a challenge and risk to health of many rural people. The free radicals are generated by exogenous reactions and respiration in the human body. The reactive oxygen species (ROS) play a role in the development of various devastating ailments which includes cancer, arthritis, asthma, dementia, mongolism, carcinoma and others (Narayanaswamy and Balakrishnan, 2011[26]). However, some plant extracts and other plant derived materials and products have been implicated in quenching of those free radicals, thereby delaying or curing some illnesses (Mongalo et al., 2015[20]; Mosa et al., 2011[22]).
Generally Curtisia species are woody, leathery simple leaves with revolute margins, opposite phyllotaxy, lacking stipules, hermaphroditic flowers, inferior ovary and possess copious endosperm (Yembaturova et al., 2009[50]). Curtisia dentata is traditionally used in South African traditional medicine to treat stomach ache, diarrhoea, sexually transmitted infections, aphrodisiac, as blood purifier and as a purgative (Cunningham, 1988[6]; Hutchings et al., 1996[15]). Geographically, the species is restricted to Southern Africa, mostly long the southern and eastern coasts of South Africa and extends into eastern Zimbabwe, Mozambique and Swaziland (Yembaturova et al., 2009[50]). Besides being threatened by bark harvesting for the medicinal plant trade (Ndawonde, 2006[28]), the leaves of the species have been recently found to contain important pentacyclic triterpene compounds such as betulinic acid, ursolic acid, 2α-hydroxyursolic acid and lupeol (Fadipe et al., 2014[11]; Shai et al., 2008[40]).
Besides exhibiting lipid peroxidase and ferric oxide activity, the hydro-alcoholic extract of the stem bark exhibited moderate free radical scavenging activity against both ABTS and DPPH (Oyedemi et al., 2012[35]). The current paper is aimed at investigating the antimicrobial activity of various leaves extracts of Curtisia dentata and the isolated compounds, including β-sitosterol which was isolated for the first time, against opportunistic organisms, mostly isolated from HIV-AIDS patient. The paper further explores the cytotoxity properties against human cell lines and the free radical scavenging activity of the plant species against a known stable free radical.
Materials and Methods
Collection and storage of plant materials
Curtisia dentata leaves were collected from the Buffelskloof Nature Reserve situated in Mpumalanga Province, South Africa. The plant was authenticated and identified by Mr John Burrows, Botanist and Reserve Manager, Buffelskloof Private Nature Reserve and a voucher (specimen No: B.C.Turpin-2062) has been deposited in the Herbarium of the Buffelskloof Private Nature Reserve. The leaves were then washed with distilled water, dried on a laboratory bench for five weeks and ground into thin powder (2 mm mesh) using Scientec Hammer Mill, Germany. Powders were kept in plastic bottles at room temperature until required.
Chemicals and reagents
Acetone, chloroform, ethyl acetate, ethanol (all were AR grade from Merck, South Africa), DPPH, (Sigma, Germany), Muller Hinton broth, Muller Hinton agar (Oxoid) ADC Middlebrook supplement, Middlebrook 7H9 broth (Fluka), glycerol, Iodo-nitro-terazolium chloride (Fluka), Mycoplasma agar, Mycoplasma broth, Yeast malt broth and Yeast Malt agar (Oxoid).
Extractions
About 10 g of the ground leaves were extracted with 40 ml acetone, ethanol, chloroform and ethyl acetate three times separately using a sonicator at 15 °C. The extracts were then filtered through Whatman's No.1 paper and then concentrated using Buchi Rotary evaporator. The residues were then weighed and kept in a refrigerator until needed.
Antimicrobial activity
Minimum Inhibitory concentrations (MIC) assay
The micro plate broth dilution assay was used to assess the minimal inhibitory concentration (Eloff, 1998[9]) with slight modification. The 12 hour old culture was diluted 1:100 with freshly prepared Muller-Hinton broth. About 100 µl of extracts (50 mg/ml in 5 % respective original solvent) were added to multi well plate containing 100 µl of freshly prepared broth and serially diluted. Plates were then incubated over night at 37 °C. About 40 µl of 2 mg/ml freshly prepared iodo-nitro-tetrazolium chloride were added to each well and incubated for 1 hour at the same temperature. For M. hominis, Mycoplama CM0403 broth (Oxoid) was supplemented with mycoplasma supplement G, while M. smegmatis was grown on Middlebrook 7H9 broth (Fluka) supplemented with glycerol and ADC middlebrook growth supplement with an incubation time of 48 hrs. C. albicans was maintained on Yeast malt agar, grown on yeast malt broth and similar procedure was used as in bacterial strains and the plates were incubated for 12 hrs. The MIC was defined as the lowest concentration of the extract to inhibit bacterial growth.
Bactericidal/Fungicidal Concentrations (MBC/MFC), total activity and MIC index
Shortly, a loopful of the microorganism in the wells showing little or no growth in the MIC assay were selected and sub-cultured on the petri plates containing an agar for different microbes. The MBC or MFC were defined as the lowest concentration that showed no bacterial or fungal growth in the subcultures (N'guessan et al., 2007[30]). To compare the activity of various plant extracts, the total activity in mL/g was calculated by dividing the total mass in mg extracted from 1 g of the plant material by the MIC value in mg/ml (Eloff, 2000[8]), while the MIC index was calculated by dividing the MBC in mg/ml with the MIC exhibited by the same extract in mg/ml (Fernandez et al., 2012[14]). The MIC index of ≤ 4 was defined as exhibiting bactericidal/fungicidal effect, > 4 as bacteriostatic effect while ≥ 16 as ineffective (Stefanovic and Comic, 2011[44]; Okeleye et al., 2013[33]).
Antioxidant activity
DPPH free radical scavenging activity
DPPH scavenging activity of the methanol extract of the plant was carried out according to method previously described (Opoku et al., 2002[34]). Decolourisation of DPPH (purple) upon addition of the extract indicated radical scavenging activity and this was measured after 30-60 min at 517 nm. Percentage of inhibition was calculated as
% Scavenging Inhibition = [1-At/A0] X 100, and the results were reported as mean ± SE (n = 3).
Isolation of ß-sitosterol from Curtisia dentata leaves
Dried clean ethanol extract (8 g) was subjected to column chromatograph (40.5 X 530.5 mm) using silica gel 60(180 g, 0.04 -0.063 mm; 230-400 mesh) supplied by Merck (Darmstadt, Germany). The clean ethanol extracts were chromatographed using gradient elution of hexane-ethyl acetate in a 10 % increase and collecting 80 mL fractions. Twenty-five (25) fractions were collected and monitored based on their TLC (F254-Merck, Whitehouse Station, NJ, USA) by visualization was achieved by UV light (254 nm) and spray with 20% H2SO4 in MeOH followed by heating in the oven (105 °C ). Compound I (89.34 mg) obtained from fractions 7-11 as single spot. The compounds 2, 3 and 4 were isolated and reported before (Fadipe et al., 2014[11]).
Spetroscopic analysis
Infra-red (IR)
The infra-Red (IR) spectroscopy determination was carried out using Perkin Elmer Spectrum 100 FTIR spectrometer.
Nuclear magnetic resonance (NMR)
1H, 13C NMR and all 2D spectra were recorded on a Bruker Avance instrument operating at 400 MHz, Chemical shifts are reported as δ values (ppm) relative to an internal standard of tetramethylsilane (TMS) or to the solvent line of CDCl3 (δH = 7.26 ppm, δC = 77.16 ppm).
High-resolution-mass spectroscopy (HR-MS)
High-resolution mass data were obtained using a Bruker micro TOF-Q II ESI instrument operating at ambient temperature.
Melting point (mp)
Melting points of the compounds were determined on a Stuart Scientific SMP3 apparatus.
Compound 1
IR (cm-1): 3377.8 (OH group), 2921.4 (aliphatic C-H), 1645.7 (olefinic carbon at [C-5]), 1382.1 (geminal dimethyl group). 1H-NMR (CDCl3) δ (ppm) 3.2 (1H, m, H-3), 5.1(1H, t, H-6), 0.8 (3H, s, Me-18), 1.6 (3H, s, Me-19), 1.2 (3H, d, J =6.5 Hz,Me-21), 1.06 (3H, d, J =6.7 Hz, Me-26), 0.9 (3H, d, J =6.7 Hz,Me-27), 1.1 (3H, t, J=7.4 Hz, Me-29).13C-NMR (CDCl3) δ (ppm) 38.85 (C-1), 31.19 (C-2), 79.1 (C-3), 41.7 (C-4), 124.5 (C-5),121.8 (C-6), 32.7 (C-7), 33.4 (C-8), 47.7 (C-9), 37.2 (C-10), 23.78 (C-11), 39.7 (C-12), 46.9 (C-13), 59.1 (C-14), 26.6 (C-15), 28.1(C-16), 55.2 (C-17), 15.7 (C-18), 17.9 (C-19), 38.6 (C-20), 17.4(C-21), 34.8 (C-22), 27.34 (C-23), 47.3 (C-24), 29.7 (C-25), 18.4(C-26), 21.5 (C-27), 26.2 (C-28), 16.8 (C-29).
Cytotoxicity studies
Shortly, the cytotoxicity studies were carried out using MTT Cell Proliferation Assay as described by Mosman (1983[23]). The Human embryonic kidney (HEK293) and Human hepatocellular carcinoma (HepG2) cells were all grown to confluences in 25 cm3 flasks. This was then trypsinized and plated into 96 well plates at specific seeding densities (5x104 cells per well). Cells were incubated overnight at 37 °C. Medium was then removed and fresh medium (MEM + Glutmax + antibiotics) was added. Isolated compounds (50-300 μg/ml) were then added in triplicate and incubated for 4 h. Antibiotics used were 100 µg/ml of both pencicllin G and streptomycin. Thereafter medium was removed and replaced by complete medium (MEM + Glutmax + antibiotics + 10 % Fetal bovine serum). After 48 h cells were subjected to the MTT assay and the results for different concentrations were reported as mean±SE, using Microplate reader (Meter tech. Σ 960, USA) at 570 nm. The wells with cells only were used as control. The percentages of inhibition were then calculated using
Percentage cell inhibition = 100 -Abs (Sample) / Abs (Control) x 100
(Sreejaya and Santhy, 2013[43]), while the IC50 were obtained from the logarithmic curve of % inhibition v/s concentrations of the isolated compounds. The Selectivity index was calculated as follows: SI=LD50 in mg/ml/ MIC in mg/ml (Bagla et al., 2014[1]).
Results and Discussion
Antimicrobial activity
The microbial resistance of various strains against common antibiotics, especially in developing countries, has resulted in tremendous selective pressure on antibiotics. These have prompted the need to investigate the antimicrobial potential of traditional medicinal plants against pathogenic strains of both bacterial and fungal strains. A variety of extracts, essential oils and compounds from South African medicinal plants have been investigated for antimicrobial activity against variety of etiologic agents of devastating human infections (Buwa and Van Staden, 2006[3] ; Tshikalange et al., 2008[47]; van Vuuren, 2008[48]; Mulaudzi et al., 2015[25]) with the intention of finding new and alternative medicines.
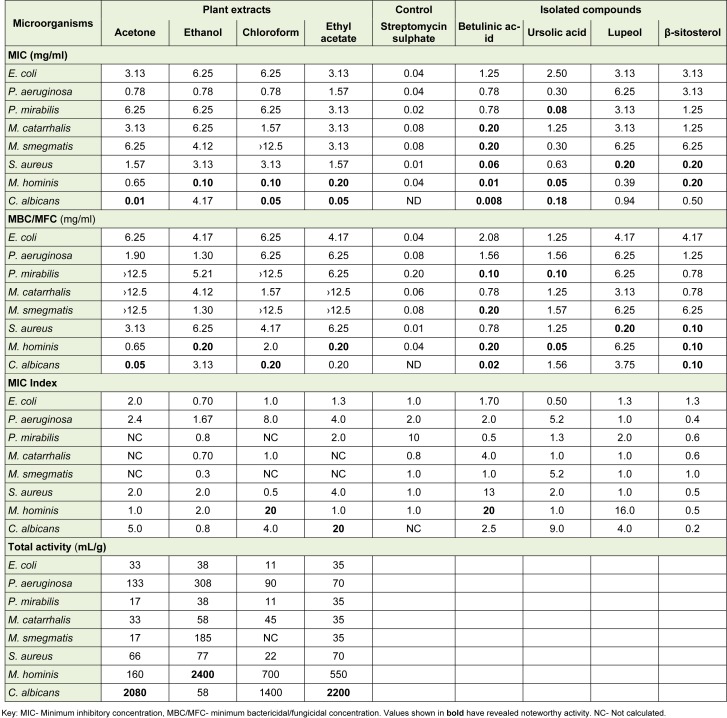
The antimicrobial properties of Curtisia dentata leaf extracts and isolated compounds are presented in Table 1(Tab. 1). The acetone extract exhibited lowest MIC of 0.01 mg/ml against Candida albicans compared to other extracts while ethanol and chloroform extracts exhibited MIC of 0.10 mg/ml against Mycoplasma hominis. Contrarily, Shai et al. (2009[39]), reported MIC values of leaves and stem bark acetone extracts of 0.11 and 0.61 mg/ml respectively. Recently, Nielsen et al. (2012[31]), reported the MIC values of the methanol extracts of the stem bark of 156.25 µg/ml against β-lactamase Escherichia coli, ampicillin-resitant Klebsiella pneumoniae, chloramphenicol resistant Citrobacter, methicilin-resistant Staphylococcus aureus (MRSA) and carbennicillin-resistant Pseudomonas aeruginosa (CRCF), while the leaves exhibited MIC values of 78.12 and 625 µg/ml against MRSA and CRCF respectively. Although these results are not comparable to the data presented in the current paper due to differences in type and origin of the microbial strains used and other environmental conditions, including collection times, they may well suggest that most of the biological active secondary metabolites may be embedded into the leaves than the stem bark.
Table 1. Antimicrobial activity of Curtisia dentata leaf extracts and isolated compounds.
The ethyl acetate and ethanol extracts exhibited potent MBC of 0.20 against Mycoplasma hominis while chloroform extract exhibited similar MBC against C. albicans. According to Chitemerere and Mukanganyama (2011[4]), MIC values of 0.06 to 0.5 mg/ml are referred to as potent when using similar method as the one in our study. Earlier, the diethyl ether extract exhibited moderate MIC of 3.13 mg/ml against Proteus mirabilis (Fadipe et al., 2014[11], 2015[12]). Betulinic acid revealed most potent antimicrobial activity compared to other isolated compounds. In other studies, betulinic acid isolated from different plants was found to possess variety of biological activity, including anti-HIV, anti-inflammatory, anti-malarial, anti-feedant, anti-parasitic, catalytic activity of Topo II, anticancer and actinociceptive activity (Theo et al., 2009[45], Moghaddam et al., 2012[19]).
Interestingly, the organic extracts from C. dentata revealed most potent MIC values against common pathogenic sexually transmitted infecting organisms and those isolated from HIV patient in our current study. These results in a way, validates the use of the plant species in the treatment of such infections. Besides being recognised as the genital and neonatal pathogen, M. hominis may inhabit the immune systems of both immune-compromised and immune-competent individuals, resulting in serious extra-genital infections such as pneumonia, mediastinitis, pericarditis, endocarditis, osteitis, arthritis and wound infections (Pascual et al., 2010[36]). Moreover it may cohabit with other organisms which may include C. albicans which causes vaginitis (Njunda et al., 2011[32]). Besides exhibiting bactericidal/fungicidal activity, the ethanol extract exhibited the best total activity of 2400 mL/g, suggesting that one gram may be diluted with 2400 ml of a solvent and still inhibit the growth of the organism. Interestingly, bactericidal antibiotics are recommended in the treatment of severely ill and immunosuppressed patients (Nemeth et al., 2015[29]). Although the results obtained in the current work validates the use of the plant in the treatment of variety of infections, the mode of action of these extracts and some isolated compounds remains unknown. Although both the extracts and isolated compounds exhibited potent antimicrobial activity against Candida albicans and Mycoplasma hominis, which are implicated as causative agents of sexually transmitted infections (STIs), there is a need to explore the biological activity of the plant species against other organisms belonging to the similar sphere like Neisseria gonorrhoea, Trichomonas vaginalis and other organisms causing several related infections.
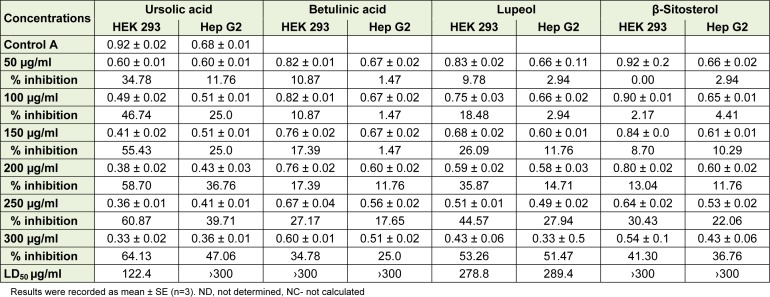
Cytotoxicity studies
According to Doughari et al. (2011[7]), the rigorous toxicity studies of C. dentata needs to be carried out to enable identification of new biologically active compounds and cautions to be issued on dangerous practices or toxicity effects, if any, as the species is extensively used in the treatment various human infections. The results for the cytotoxicity investigations are shown below (Table 2(Tab. 2)) and suggest that the isolated compounds inhibit the growth of selected human cells in a dose dependent manner. Earlier, the acetone and dichloromethane extracts of C. dentata reportedly exhibited LC50 of 0.007 and 0.024 µg/ml respectively in an MTT assay against Monkey kidney cells (Shai et al., 2008[41]). The higher LD50 implies that it would take a large quantity of the extract to cause a toxic response, while small LD50 values are highly toxic and could be dangerous (Okeleye et al., 2013[33]). In our current study, both betulinic acid and β-sitosterol exhibited LD50 of > 300 µg/ml against the selected cell lines, suggesting that the compounds are less toxic. Ursolic acid exhibited the lowest LD50 of 122.4 µg/ml against HEK 293 cell line while lupeol exhibited LD50 of 278.8 and 289.4 4 µg/ml against HEK 293 and Hep G2 respectively. However, according to Sahranavard et al. (2009[38]), the isolated compounds are referred to as toxic when exhibiting LD50 of about 100 µg/ml or less. Some isolated compounds and plant extracts from plant materials reportedly exhibited very low IC50, hence toxic (Mthethwa et al., 2014[24]; Behzad et al., 2014[2]; Tiwary et al., 2015[46]).
Table 2. Cytotoxicity studies of the isolated compounds from Curtisia dentata leaves.
The β-sitosterol and betulinic acid revealed percentage inhibition of 25.0 to 41. 30 %. According to El-Sharkawy et al. (2013[10]), the percentage of inhibition ranging from 25 to 50 is referred to as normal. Elsewhere, β-sitosterol exhibited LD50 of 21.9 and 21.6 against normal (HFB4) and cancer (MCF7) cells respectively (Singab et al., 2012[42]). Generally, the isolated compounds are less toxic hence relevant to use in pharmacological setups.
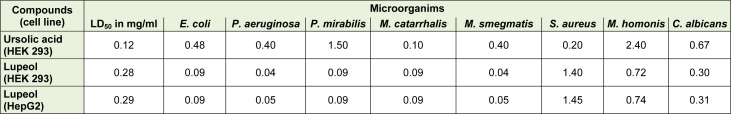
Selectivity index
The selectivity index (SI) of ursolic acid and lupeol against HEK 293 and HepG2 are reported in Table 3(Tab. 3). SI indicates the cytotoxic selectivity or safety of the crude extract or isolated compound against the selected cell lines (Machana et al., 2011[16]). The compounds exhibited low selectivity index values, indicating the similar cytotoxicity and antimicrobial activity. According to Makhafola et al. (2014[17]), the in-vitro toxicity does not equate to in vivo toxicity because of difference in physiological microenvironment in live animal and tissue culture. Moreover, other factors relating to chemical kinetics which may include absorption, biotransformation, distribution and excretion, which influence the exposure at the level of target cells in vivo, cannot be adequately simulated in vitro.
Table 3. Selectivity index of isolated compounds in mg/ml.
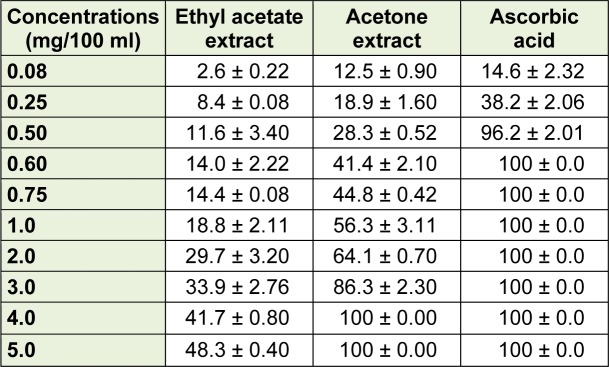
Antioxidant activity
The results for the antioxidant activity of both acetone and ethyl acetate are shown in Table 4(Tab. 4). The acetone extract exhibited better inhibition of DPPH than ethyl acetate extract, while ascorbic acid completely inhibits DPPH at lower concentrations. Acetone extract inhibits DPPH at a comparable state at 0.08 mg/100 ml. According to Mongalo et al. (2012[21]), the extract is a good inhibitor of DPPH if it gives inhibition of about 75 % at 0.75 mg/100ml, suggesting that the acetone extract of the plant species in the current study exhibited moderate free radical scavenging activity while ethyl acetate was relatively poor.
Table 4. Antioxidant activity of extracts from Curtisia dentata leaves.
However, there is a need to explore the antioxidant properties of the extracts against other forms of radicals. The antioxidant activity may be of greater important in preventing oxidative stress which may be involved in many fatal infections and diseases.
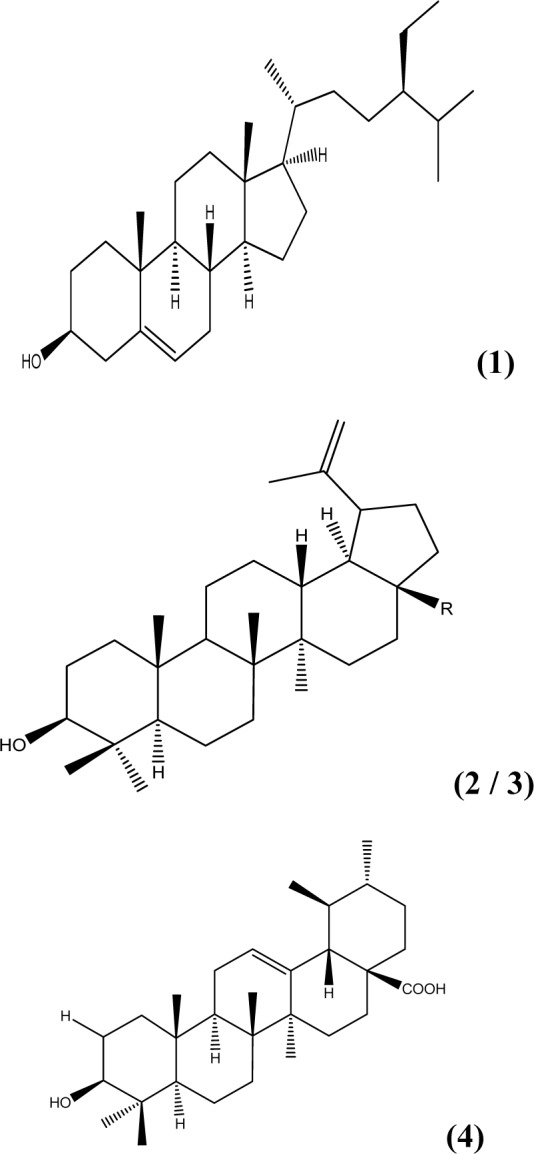
Isolated compounds
The newly isolated compound (1) was isolated and identified as β-Sitosterol (NMR data not shown), while the other three compounds (2, 3 and 4) were identified earlier (Fadipe et al., 2014[11]) (Figure 1(Fig. 1)).
Figure 1. Isolated compounds: (1) β-Sitosterol, (2) Lupeol, (3) R=CH3, Betulinic acid - R=COOH, (4) Ursolic acid.
Conclusions
Curtisia dentata leaves extracts exhibited good antimicrobial activity against the selected microbial strains. The activity exhibited by ethanol extract further resulted in the isolation of compounds such as lupeol, betulinic acid ursolic acid and the newly isolated compound known as β-sitosterol which also exhibited potent antimicrobial activity. The isolated compounds were less toxic to HepG and HEK 293 cell lines. The acetone extract exhibited better DPPH free radical scavenging activity compared to the ethyl acetate extract. However, there is a need to explore the antioxidant activity of these extracts using other assays. The current study validates the use of the plant species in the treatment of various human infections, including sexually transmitted infections. However, there is still a need to investigate the antimicrobial activity of these extracts against other pathogenic organisms.
Future Studies
We are currently assessing the anti-mycobacterial activity of the isolated compounds individually and in combination. We also need to explore the antimicrobial effect of the aqueous extracts of the plant species against pathogenic human strains. We are also investigating the phyto-chemistry of the acetone extract as it revealed activity against selected microbes.
Acknowledgements
Authors are deeply thankful to the District Hospital (Kwa-Nongoma area) for the generous donation of microorganisms. We are also deeply thankful to National Botanical Institute (Nelspruit) for allowing us to collect the leaves of the plant species used in the current study.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Bagla VP, McGaw LJ, Elgorashi EE, Eloff JN. Antimicrobial activity, toxicity and selectivity index of two biflavonoids and a flavone isolated from Podocarpus henkelii (Podocarpaceae) leaves. BMC Complement Altern Med. 2014;14:383. doi: 10.1186/1472-6882-14-383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Behzad S, Pirani A, Mosaddegh M. Cytotoxic activity of some medicinal plants from Hamedan district of Iran. Iran J Pharm Res. 2014;13:199–205. [PMC free article] [PubMed] [Google Scholar]
- 3.Buwa LV, van Staden J. Antibacterial and antifungal activity of traditional medicinal plants used against venereal diseases in South Africa. J. Ethnopharmacol. 2006;103:139–142. doi: 10.1016/j.jep.2005.09.020. [DOI] [PubMed] [Google Scholar]
- 4.Chitemerere TA, Mukanganyama S. In Vitro antibacterial activity of selected medicinal plants from Zimbabwe. Afr J Plant Sci. 2011;5:1–7. [Google Scholar]
- 5.Chovanov R, Mikulov M, Vaverkov In vitro antibacterial and antibiotic resistance modifying effect of bioactive plant extracts on methicillin-resistant Staphylococcus epidermidis. Int J Microbiol. 2013;2013:760969. doi: 10.1155/2013/760969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cunningham AB. An investigation of the herbal medicine trade in Natal/KwaZulu. Invesigational report no 29, Institute of Natural Resources. Pitermaritzburg: University of Natal; 1988. [Google Scholar]
- 7.Doughari HJ, Ndakidemi PA, Human IS, Benade S. Curtisia dentata: Ethnopharmacological application. J Med Plant Res. 2011;5:1606–1612. [Google Scholar]
- 8.Eloff JN. A proposal on expressing the antibacterial activity of plant extracts - A small first step in applying scientific knowledge to rural primary health care in South Africa. S Afr J Sci. 2000;96:116–118. [Google Scholar]
- 9.Eloff JN. A sensitive and quick micro plate method to determine the minimal inhibitory concentration of plant extracts for bacteria. Planta Med. 1998;64:711–713. doi: 10.1055/s-2006-957563. [DOI] [PubMed] [Google Scholar]
- 10.El-Sharkawy ER, Matloub AA, Atta EM. Cytotoxicity of new flavonoid compound isolated from Farsetia aegyptia. Int J Pharm Sci Inv. 2013;2:23–27. [Google Scholar]
- 11.Fadipe VO, Mongalo NI, Opoku AR. Antibacterial properties of Curtisia dentata leaves and some triterpenes/active principles isolated from them. 3rd International Conference on Medicinal Chemistry & Computer Aided Drug Designing; 2014. p. 21. Available from: http://dx.doi.org/10.4172/2161-0444.S1.013. [Google Scholar]
- 12.Fadipe VO, Mongalo NI, Opoku AR. Antibacterial properties of Curtisia dentata leaves and some triterpenes/active principles isolated from them. South Afr J Botany. 2015;18:208. Available from: http://dx.doi.org/10.1016/j.sajb.2015.03.148. [Google Scholar]
- 13.Fatemeh K, Khosro P. In vitro cytotoxic activity of aqueous root extract of Althea kurdica against Endothelial human bone marrow cells (line k562) and human lymphocytes. Bull Environ Pharmacol Life Sci. 2013;2:23–29. [Google Scholar]
- 14.Fernandes L, Daruliza K, Sudhakaran S, Jegathambigai R. Antimicrobial activity of the crude extracts of Piper sarmentosum against methicillin-resistant Staphylococcus aureus (MRSA), Escherichia coli, Vibrio cholera and Streptococcus pneumoniae. Eur Rev Med Pharmacol Sci. 2012;16:105–111. [PubMed] [Google Scholar]
- 15.Hutchings A, Scott AH, Lewis G, Cunningham AB. Zulu medicinal plants: An inventory. Scottsville, SA: University of KwaZulu-Natal Press; 1996. pp. 226–227. [Google Scholar]
- 16.Machana S, Weerapreeyakul N, Barusrux S, Nonpunya A, Sripanidkulchai B, Thitimetharoch T. Cytotoxic and apoptotic effects of six herbal plants against the human hepatocarcinoma (HepG2) cell line. Chin Med. 2011;6(1):39. doi: 10.1186/1749-8546-6-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Makhafola TJ, McGaw LJ, Eloff JN. In vitro cytotoxicity and genotoxicity of five Ochna species (Ochnaceae) with excellent antibacterial activity. S Afr J Bot. 2014;91:9–13. [Google Scholar]
- 18.Marasini P, Baral P, Aryal P, Ghimire KR, Neupane S, Dahal N, et al. Evaluation of antibacterial activity of some traditionally used medicinal plants against human pathogenic bacteria. Biomed Res Int. 2015;2015:265425. doi: 10.1155/2015/265425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moghaddam MG, Ahmad FBH, Samzadeh-Kermani A. Biological activity of betulinic acid: A review. Pharmacol Pharm. 2012;3:119–123. [Google Scholar]
- 20.Mongalo NI, McGaw LJ, Finnie JF, van Staden J. Securidaca longipedunculata Fresen (Polygalaceae): A review of its ethnomedicinal uses, phytochemistry, pharmacological properties and toxicology. J Ethnopharmacol. 2015;165:215–226. doi: 10.1016/j.jep.2015.02.041. [DOI] [PubMed] [Google Scholar]
- 21.Mongalo NI, Opoku AR, Zobolo AM. Antibacterial and antioxidant activity of the extracts of Waltheria indica Linn. Collected from Capricorn District, Limpopo Province. S Afr J Med Plant Res. 2012;6:5593–5598. [Google Scholar]
- 22.Mosa RA, Lazarus GG, Gwala PE, Oyedeji O, Opoku AR. In vitro anti-platelet aggregation, antioxidant and cytotoxic activity of extracts of some Zulu medicinal plants. J Nat Prod. 2011;4:136–146. [Google Scholar]
- 23.Mosmann T. Rapid colorimetric assay for cellular growth and survival. J Immunol Methods. 1983;65:55–63. doi: 10.1016/0022-1759(83)90303-4. [DOI] [PubMed] [Google Scholar]
- 24.Mthethwa NS, Oyedeji BAO, Obi CL, Aiyegoro OA. Anti-staphylococcal, anti-HIV and cytotoxicity studies of four South African medicinal plants and isolation of bioactive compounds from Cassine transvaalensis (Burtt. Davy) codd. BMC Complementa Altern Med. 2014;14:512. doi: 10.1186/1472-6882-14-512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mulaudzi RB, Ndhlala AR, Van Staden J. Ethnopharmacological evaluation of a traditional herbal remedy used to treat gonorrhea in Limpopo Province, South Africa. S Afr J Bot. 2015;97:117–122. [Google Scholar]
- 26.Narayanaswamy N, Balakrishnan KP. Evaluation of some medicinal plants for their antioxidant properties. Int J Pharm Tech Res. 2011;3:381–385. [Google Scholar]
- 27.Nasri H, Shirzad H. Toxicity and safety of medicinal plants. J Herb Med Pharmacol. 2013;2:21–22. [Google Scholar]
- 28.Ndawonde BG. Medicinal plant sales: A case study in Northern Zululand. MSc Dissertation. South Africa: University of Zululand; 2006. [Google Scholar]
- 29.Nemeth J, Oesch G, Kuster S. Bacteriostatic versus bactericidal antibiotics antibiotics for patients with serious bacterial infections: systematic review and meta-analysis. J Antimicrob Chemother. 2015;70:382–395. doi: 10.1093/jac/dku379. [DOI] [PubMed] [Google Scholar]
- 30.Nguessan JD, Dinzedi MR, Guessennd N, Coulibaly A, Dosso M, Djaman AJ, et al. Antibacterial activity of the aqueous extracts of Thonningia sanguinea against Extended-Spectrum-?-lactamases (ESBLs) producing Escherichia coli and Klebsiella pneumoniae. Trop J Pharm Res. 2007;6:779–783. [Google Scholar]
- 31.Nielsen TR, Kuete V, Jger AK, Meyer JJM, Lall N. Antimicrobial activity of selected South African medicinal plants. BMC Complement Altern Med. 2012;12:74. doi: 10.1186/1472-6882-12-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Njunda AL, Nsagha DS, Assob JCN, Palle JN, Kamga HL, Nde PF, et al. Genital mycoplasmas in women attending the Yaounde University Teaching Hospital, Cameroon. J Publ Health Afr. 2011;2:68–71. doi: 10.4081/jphia.2011.e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Okeleye BI, Mkwetshana NT, Ndip RN. Evaluation of the antibacterial and antifungal potential of Peltophorum africanum: Toxicological effect on human chang liver cell line. Sci World J. 2013;2013:article ID 878735 (9 pp). doi: 10.1155/2013/878735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Opoku AR, Maseko NF, Terblanche SE. The in-vitro antioxidative activity of some traditional Zulu medicinal plants. Phyt Res. 2002;16:S51–S56. doi: 10.1002/ptr.804. [DOI] [PubMed] [Google Scholar]
- 35.Oyedemi SO, Oyedemi BO, Arowosegbe S, Afolayan AJ. Phytochemicals analysis and medicinal potentials of hydroalcoholic extract from Curtisia dentata (Burm.f) C.A. Sm stem bark. Int J Mol Sci. 2012;13:6189–6203. doi: 10.3390/ijms13056189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pascual A, Jaton K, Ninet B, Bille J, Greub G. New diagnostic real-time PCR for specific detection of mycoplasma hominis DNA. Int J Microbiol. 2010;2010:article ID 317512 (4 pp). doi: 10.1155/2010/317512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Priyadharshini SD, Sujatha V. Antioxidant and cytotoxic studies on two known compounds isolated from Hyptis suaveolens leaves. Int J Pharm Pharm Sci. 2013;5:283–290. [Google Scholar]
- 38.Sahranavard S, Naghibi F, Mosaddegh M, Esmaeili S, Sarkhail P, Taghvaei M, et al. Cytotoxic activities of selected medicinal plants from Iran and phytochemical evaluation of the most potent extract. Res Pharm Sci. 2009;4:133–137. [PMC free article] [PubMed] [Google Scholar]
- 39.Shai LJ, Bizimenyera ES, Bagla V, Mcgaw LJ, Eloff JN. Curtisia dentata (Cornaceae) leaf extracts and isolated compounds inhibit motility of parasitic and free-living nematodes. Onderstepoort J Vet Res. 2009;76:249–276. doi: 10.4102/ojvr.v76i2.49. [DOI] [PubMed] [Google Scholar]
- 40.Shai LJ, Mcgaw LJ, Aderogba MA, Mdee LK, Eloff JN. Four pentacyclic triterpenoids with antifungal and antibacterial activity from Curtisia dentata (Burm.f) C.A. Sm leaves. J Ethnopharmacol. 2008;119:238–244. doi: 10.1016/j.jep.2008.06.036. [DOI] [PubMed] [Google Scholar]
- 41.Shai LJ, Mcgaw LJ, Masoko P, Eloff JN. Antifungal and antibacterial activity of seven traditionally used South African plant species active against Candida albicans. S Afr J Bot. 2008;74:677–684. [Google Scholar]
- 42.Singab AN, EL-Ahmady S, Milad R, Saad S. Kalanchoe thrysifora Harv. and Kalanchoe marmorata Baker;DNA profiling, biological guided fractionation of different extracts, isolation and identification of cytotoxic compounds. J Appl Pharm Sci. 2012;2:215–220. [Google Scholar]
- 43.Sreejaya SB, Santhy KS. Cytotoxic properties of Acorus calamus in MCF-7 breast cancer cells. Int J Curr Res Acad Rev. 2013;1(1):106–111. [Google Scholar]
- 44.Stefanovic O, Comic L. Inhibitory effect of Cytisus capitatus Scop. on growth of bacteria. Afr J Microbiol Res. 2011;5:4725–4730. [Google Scholar]
- 45.Theo A, Masebe T, Suzuki Y, Kikuchi H, Wada S, Obi CL, et al. Peltophorum Africanum, a traditional South African Medicinal Plant, contains an Anti HIV-1 constituent, Betulinic Acid. Tohoku J Exp Med. 2009;217:93–99. doi: 10.1620/tjem.217.93. [DOI] [PubMed] [Google Scholar]
- 46.Tiwary BK, Bihani S, Kumar A, Chakraborty R, Ghosh R. The in vitro cytotoxic activity of ethno-pharmacological important plants of Darjeeling district of West Bengal against different human cancer cell lines. BMC Complement Altern Med. 2015;15:22. doi: 10.1186/s12906-015-0543-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tshikalange TE, Meyer JJ, Lall N, Munoz E, Sancho R, Van de Venter M, et al. In vitro anti-HIV-1 properties of ethnobotanically selected South African plants used in the treatment of sexually transmitted diseases. J Ethnopharmacol. 2008;119:478–481. doi: 10.1016/j.jep.2008.08.027. [DOI] [PubMed] [Google Scholar]
- 48.Van Vuuren SF. Antimicrobial activity of South African medicinal plants. J Ethnopharmacol. 2008;119:462–472. doi: 10.1016/j.jep.2008.05.038. [DOI] [PubMed] [Google Scholar]
- 49.Vigneshwari C, Nagaraj R, Karmegam N. Synergistic anti-Staphylococcus aureus (methicillin resistant) activity of ethnomedicinal plants from Shevaroy Hills (Eastern Ghats), South India. Int J Curr Res Biosci Plant Biol. 2014;1:51–59. [Google Scholar]
- 50.Yembaturova EY, Van Wyk B-E, Tinley PM. A review of the genus Curtisia (Curtisiaceae) Bothalia. 2009;39:87–96. [Google Scholar]