Abstract
Problem
An outbreak of chronic liver disease of unidentified cause, also called “Unidentified Liver Disease” or “ULD” was first observed in a rural village in Tigray, Ethiopia in 2001. Little was known about the geographical extent, trend, and epidemiology of this disease.
Approach
We initiated a local active surveillance system to characterize and monitor trends for this emerging disease and to identify cases for treatment and follow up.
Local setting
Tigray is a rural, resource-limited setting characterized by a lack of electricity, rugged terrain, limited transportation, and few healthcare facilities and trained healthcare workers.
Relevant changes
The Ethiopian Health and Nutrition Research Institute, Centers for Disease Control and Prevention, World Health Organization, and Tigray Regional Health Bureau established the ULD surveillance system in 2009 and conducted a large-scale official training for the surveillance staff on case identification, management and reporting. In absence of a confirmatory test, the system used simple case definitions that could be applied by frontline staff with varying clinical training. To maximize resources, health extension workers already conducting household visits in affected communities identified cases and increased community awareness about the disease. A team was placed in Shire, in close proximity to the outbreak region, to provide support and collect reports from health facilities and district health offices.
Lessons learned
Long term dedication by frontline staff, using simple case definitions to identify cases, and active collection of missing reports were critical for surveillance of this chronic non-infectious disease of unknown cause in a rural, resource-limited setting.
Introduction
A chronic liver disease of unidentified cause, known as “Unidentified liver disease” (ULD) by the local community, was first observed in a rural village in the northwestern region of Tigray, Ethiopia in 2001 (1). ULD was characterized by epigastric pain, abdominal distention, ascites, and hepato/splenomegaly, with fatality rates estimated to be 30 to 40% (1–3). Early investigations ruled out infectious causes, directing investigators to investigate potential toxic etiologies (1–6). Questions regarding the basic epidemiology of the disease included geographic, temporal, and seasonal trends; case demographics; clinical characteristics; and incidence and mortality rates. An active surveillance system was established to monitor the outbreak and to answer these questions. Our objective is to report the lessons learned from implementing this surveillance system and the results from an assessment performed two years after the system was established.
Approach
In 2009, the Ethiopian Health and Nutrition Research Institute (EHNRI), Centers for Disease Control and Prevention (CDC), the World Health Organization (WHO), and Tigray Regional Health Bureau (TRHB) established an active surveillance system in the Tigray region to monitor the ongoing ULD outbreak. The objectives of the surveillance system were to determine the magnitude and distribution of ULD, identify disease trends, connect cases with clinical care, and inform health officials and funding bodies for resource allocation.
Setting
Tigray is a remote, semi-arid region that is one of the most drought-prone and food insecure regions of Ethiopia (7, 8). Affected villages were rural with rugged terrain, limited means of transportation and access to healthcare, and limited or no electricity. The health posts and centers were basic with limited clinical services and staff; most frontline staff had limited clinical training.
Stakeholders
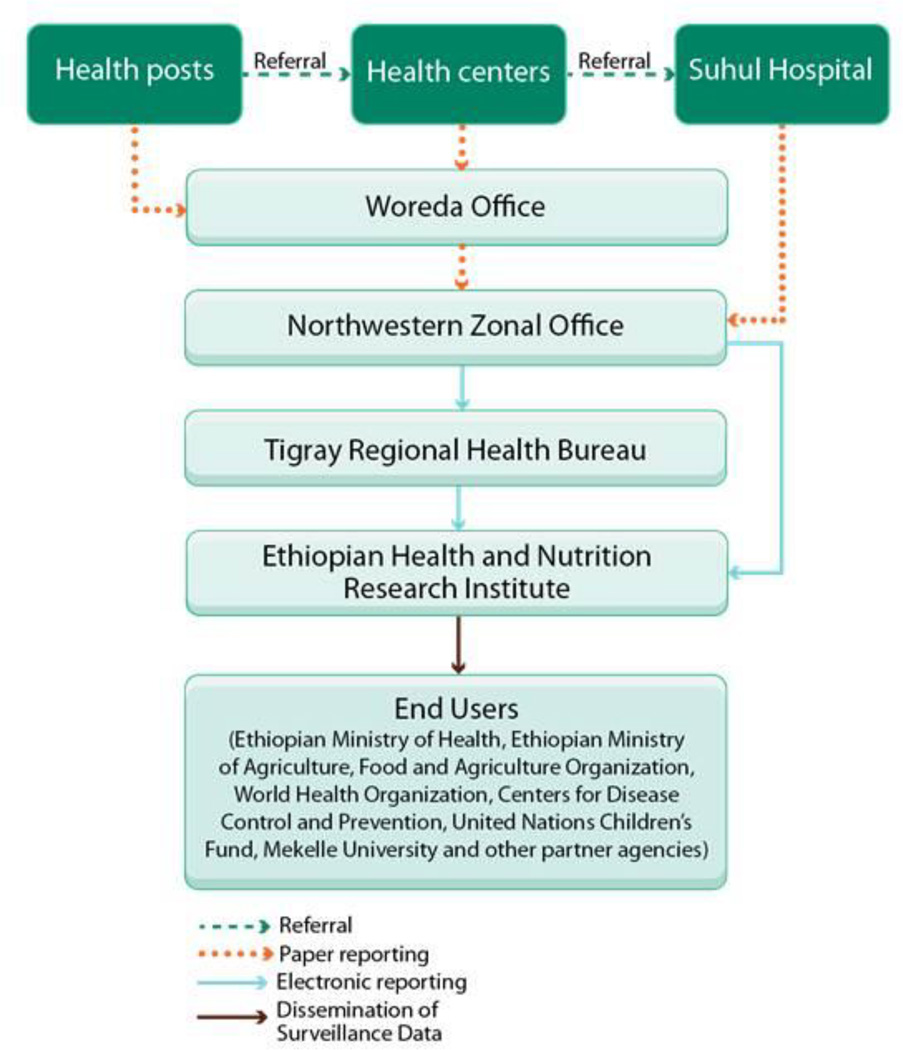
A strong partnership and collaboration between EHNRI, WHO, CDC, and TRHB jointly implemented the ULD surveillance system. EHNRI was the central coordinating body overseeing the ULD surveillance system. Other stakeholders included health facilities, district health offices, Northwestern Zonal office, and funding and partner agencies (Figure 1).
Figure 1.
Information Flow in the Unidentified Liver Disease Active Surveillance System in Tigray, Ethiopia
Case definitions
Simple sign and symptom-based case definitions that did not require laboratory capacity were designed to detect cases. Suspect cases were 1) individuals with abdominal distension identified by history or on physical exam; and 2) either a household member with similar symptoms and/or abdominal pain/cramps for at least two weeks. Possible cases met the suspect case definition and also had a palpable liver below the right costal margin (hepatomegaly) and/or palpable spleen below the left costal margin (splenomegaly) on physical exam. Because there was no confirmatory laboratory test, there was no “confirmed” case definition. A standardized surveillance form was used to capture case demographics, disease history, signs and symptoms, and laboratory parameters.
Reporting
As of September 2011, 13 districts were under active surveillance in the Northwestern, Central and Western Zones in the Tigray region. Typically, each district health office oversaw four to six health centers and over 20 health posts. Cases were identified when they self-presented at local health facilities. In order to actively detect cases, health extension workers (HEWs) from health posts who were already performing household visits for other public health purposes such as malaria prevention were trained on ULD and the simple case definition. They referred cases for care at local health centers, which then referred the more complex and severe cases to the hospitals. Health facilities sent surveillance reporting forms to the district health offices, which were compiled and sent to the zonal and regional health offices; there the data were converted to electronic format and were sent to EHNRI and shared with ULD investigation partners. Due to limited transportation capability to deliver paper reports, EHNRI placed a surveillance team in the NW Zonal office in Shire, the town in closest proximity to the outbreak region, which actively collected missing reports from the health facilities when passive reporting failed.
Monitoring and Evaluation
Health centers, where the majority of the patients were managed, communicated regularly with the district offices via weekly phone calls and quarterly meetings. The district offices also conducted quarterly monitoring visits with health centers, health posts, and communities for quality control and to ensure that the information collected was consistent, accurate, and complete.
In September 2011, CDC conducted a qualitative assessment of the implementation of the surveillance system two years after its establishment. We interviewed 20 staff in all levels of the surveillance system, visited 9 sites (2 health posts, 3 health centers, 1 hospital, and district, zonal and regional health offices), and reviewed the documentation and processes used for surveillance activities. Interviews covered training, case identification and management, data collection and reporting, supervision and feedback, and suggestions for system improvement. Health facilities and offices were visited based on availability; therefore, the findings represent the views of the sites visited and individuals interviewed only.
Results
The ULD surveillance system overcame a number of challenges and successfully achieved its objectives (Table 1). As of September 2011, the system identified a total of 1033 cases, including 314 deaths. Case fatality rates were calculated to monitor the effect of treatment and follow-up on patient prognosis. Data from the surveillance system were also used to allocate medications to health facilities to treat patients. When several health facilities reported medication shortages, TRHB reviewed its operations to more effectively guide medication management and distribution.
Table 1.
Challenges and Strategies Employed in Implementing the Unidentified Liver Disease Active Surveillance System in Tigray, Ethiopia
| Challenges | Strategies | Outcomes | Lessons Learned |
|---|---|---|---|
| Unknown etiology and absence of diagnostic test | |||
|
|
|
|
| Implementation of traditional paper-reporting system | |||
|
|
|
|
| Staff shortage and turnover | |||
|
|
|
|
Lessons Learned
There were many challenges and lessons learned in establishing and ensuring sustainable implementation of this surveillance system (Table 1). We outline three major ones here that may be applicable for other surveillance systems in similar settings (Box 1).
Box 1. Summary of main lessons learned.
Dedicated frontline staff willing to perform active case finding and reporting under difficult conditions was critical for the success of this surveillance system.
Official training conducted in 2010 was highly effective; however regular training will be necessary to address high staff turnover as well as train back-up staff at all reporting sites.
Active collection of missing reports from health facilities and district health offices was instrumental in maintaining the high level of operation of this surveillance system.
The importance of dedicated frontline staff
This surveillance system used traditional paper reporting, which posed significant logistical challenges for frontline staff. Surveillance staff were dependent on the district offices to provide paper forms and photocopied forms at their own expense or hand-wrote the reports when forms ran out. Frontline staff travelled by foot or caught available rides in order to carry paper reports up to 40 km. In addition, roads between health posts and health centers become impassable during the rainy season. Dedicated frontline staff were critical to the success of the surveillance system, overcoming these challenges in order to conduct active case finding and reporting. However, they were often not provided timely updates including surveillance reports. During our interviews, 70% (7 out of 10) of the frontline staff (health facility and district office staff) said they would like to receive reports as one form of feedback.
Overcoming staff shortages and need for regular official training
In a typical health post, staff included a nurse and a HEW who visited six to eight households every day. A health center typically had a medical director, surveillance focal person, and multiple nurses. Forty-three percent (3 out of 7 health facilities and district offices visited) reported that as soon as the surveillance focal person was away, the reporting stopped due to lack of trained back-up personnel. In addition, two out of seven (29%) health facilities and district offices we visited had staff turnover during the past year. A large-scale official training on the ULD surveillance system was conducted in 2010; however, among interviewed staff at health facilities and district office, only 60% (6 out of 10) had received the official training, and 80% (8 out of 10) requested additional official training.
Active collection of reports
Due to staff shortage, EHNRI and TRHB were resourceful and in March 2011 asked the agricultural team temporarily assigned in Shire to conduct animal and plant studies to also oversee the surveillance activities; during this time there was a general impression among the staff that surveillance was functioning optimally. The team visited district offices and health facilities to monitor progress and collect missing reports. However, this temporary assignment ended in Dec 2011, which left no surveillance staff in Shire to perform this function.
Conclusions
Surveillance plays an integral role in monitoring a disease outbreak. For optimal functioning in a rural, resource-limited setting where a paper-based system is the only option, it is critical to ensure there are adequate transportation, communication, training, record keeping, and staff incentives (9, 10, 11). Conducting surveillance for a chronic disease of unknown etiology with no diagnostic test presented additional challenges that were addressed by using simple case definitions to identify cases and ensuring detected cases received treatment and were monitored for long-term disease prognosis. To ensure sustainability of this surveillance system, the following recommendations could be considered: 1) provide regular official trainings; 2) utilize common resources from other programs to maximize resource support for collecting and delivering reports; 3) provide feedback by sharing surveillance reports to engage and motivate frontline staff; and 4) regular evaluation to continually monitor and address the immediate challenges in the system.
In 2011, with evidence from multiple studies, the investigation group concluded the cause of illness to be contamination of locally produced grains with several pyrrolizidine alkaloid (PA) producing plants, and ULD was renamed to PA-induced liver disease (PAILD) (1, 3, 4, 6, 12). Ongoing support of the surveillance system will be critical to ensure continual disease monitoring as interventions to disrupt PA exposure are implemented in the community.
References
- 1.Bane A, Seboxa T, Mesfin G, Ali A, Tsegaye Y, M WT, et al. An outbreak of veno-occlusive liver disease in northern Ethiopia, clinical findings. Ethiopian medical journal. 2012 Apr;50(Suppl 2):9–16. PubMed PMID: 22946291. Epub 2012/09/06. eng. [PubMed] [Google Scholar]
- 2.Mesfin G, Ali A, Seboxa T, Bane A, Tensae MW, Gebressilassie S, et al. An epidemiological study into the investigation of liver disease of unknown origin in a rural community of northern Ethiopia, 2005. Ethiopian medical journal. 2012 Apr;50(Suppl 2):1–8. PubMed PMID: 22946290. [PubMed] [Google Scholar]
- 3.Schneider J, Tsegaye Y, M WT, S GS, Haile T, Bane A, et al. Veno-occlusive liver disease: a case report. Ethiopian medical journal. 2012 Apr;50(Suppl 2):47–51. PubMed PMID: 22946295. [PubMed] [Google Scholar]
- 4.Debella A, Abebe D, Tekabe F, Mamo H, Abebe A, Tsegaye B, et al. Toxicity study and evaluation of biochemical markers towards the identification of the causative agent for an outbreak of liver disease in Tahtay Koraro Woreda, Tigray. Ethiopian medical journal. 2012 Apr;50(Suppl 2):27–35. PubMed PMID: 22946293. [PubMed] [Google Scholar]
- 5.Abebe D, Debella A, Tekabe F, Mekonnen Y, Degefa A, Mekonnen A, et al. An outbreak of liver disease in Tahtay Koraro Woreda, Tigray region of Ethiopia: a case-control study for the identification of the etiologic agent. Ethiopian medical journal. 2012 Apr;50(Suppl 2):17–25. PubMed PMID: 22946292. [PubMed] [Google Scholar]
- 6.Debella A, Abebe D, Tekabe F, Degefa A, Desta A, Tefera A, et al. Physico-chemical investigation of consumables and environmental samples to determine the causative agent of liver disease outbreak in Tahitay Koraro Woreda, Tigray. Ethiopian medical journal. 2012 Apr;50(Suppl 2):37–45. PubMed PMID: 22946294. [PubMed] [Google Scholar]
- 7.Yazew E, Depeweg H, Haile M. Earthen dam irrigation schemes in Tigray, Ethiopia: development opportunities versus sustainability challenges. 2008 Available from: www.ethiopianreview.com/archive/0838102811008030307.doc.
- 8.Ethiopian Demography and Health. [cited 2012 Oct 27];Tigray. Available from: http://www.ethiodemographyandhealth.org/Tigray.html.
- 9.Ndiaye SM, Quick L, Sanda O, Niandou S. The value of community participation in disease surveillance: a case study from Niger. Health Promot Int. 2003 Jun;18(2):89–98. doi: 10.1093/heapro/18.2.89. PubMed PMID: 12746380. Epub 2003/05/15. eng. [DOI] [PubMed] [Google Scholar]
- 10.Rumisha SF, Mboera LE, Senkoro KP, Gueye D, Mmbuji PK. Monitoring and evaluation of integrated disease surveillance and response in selected districts in Tanzania. Tanzania health research bulletin. 2007 Jan;9(1):1–11. doi: 10.4314/thrb.v9i1.14285. PubMed PMID: 17547094. Epub 2007/06/06. eng. [DOI] [PubMed] [Google Scholar]
- 11.Oum S, Chandramohan D, Cairncross S. Community-based surveillance: a pilot study from rural Cambodia. Tropical medicine & international health : TM & IH. 2005 Jul;10(7):689–697. doi: 10.1111/j.1365-3156.2005.01445.x. PubMed PMID: 15960708. Epub 2005/06/18. eng. [DOI] [PubMed] [Google Scholar]
- 12.Buttke DE, Martin C, Na L, Rentz D, Luce R, Bayleyegn T, et al. Serum evidence of exposure to pyrrolizidine alkaloids in the setting of a widespread outbreak of liver disease of unknown etiology—Tigray, Ethiopia 2008–2011. Unpublished. [Google Scholar]