Abstract
Objectives:
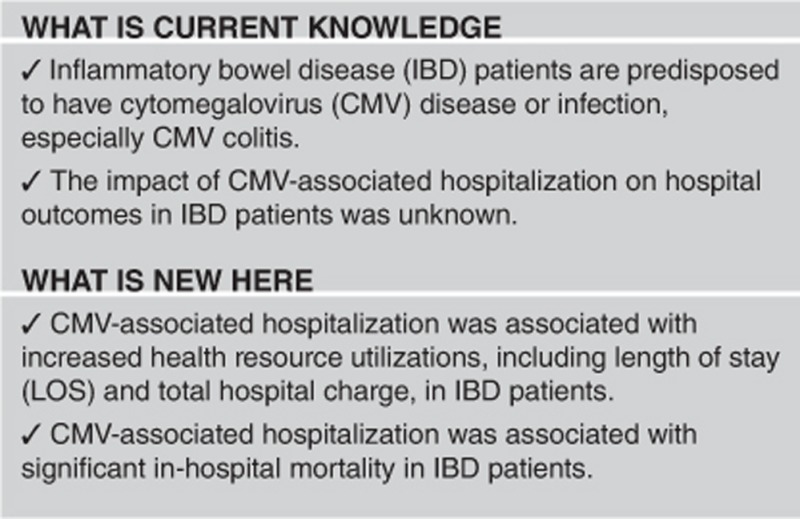
Impact of cytomegalovirus (CMV)-related hospitalization in inflammatory bowel disease (IBD) patients is unknown. The aim of this study was to determine hospital outcomes of CMV-related hospitalization in IBD patients in a large national in-patient administrative data set.
Methods:
This was a cross-sectional study using data from the Nationwide In-patient Sample database. IBD- and CMV-related hospitalizations between 2003 and 2011 were identified using appropriate ICD-9-CM (International Classification of Diseases, Ninth Revision, Clinical Modification) codes. Impact of CMV-related hospitalization on in-hospital mortality, length of stay (LOS), and hospital charges were quantified.
Results:
CMV-related hospitalization was associated with higher in-hospital mortality (odds ratio (OR) 7.09, 95% confidence interval (CI) 3.38–14.85), prolonged LOS (7.77 days, P<0.0001), and more hospital charge (US$66,495, P<0.0001) in IBD patients.
Conclusions:
CMV-related hospitalization in IBD is associated with high in-hospital mortality, prolonged LOS, and hospital care costs.
Introduction
The inflammatory bowel diseases (IBDs), comprising Crohn's disease (CD) and ulcerative colitis (UC), are chronic relapsing conditions that frequently require hospitalization.1 Patients with IBD, particularly those with severe, corticosteroid-refractory and -dependent states are often treated with immunosuppressive agents either alone or in combination. Therefore, patients with IBD are expected to be at an increased risk of infectious complications, such as cytomegalovirus (CMV)-related colitis.2 CMV, a member of the herpesviridae family, is responsible for a common viral infection in humans, with 30–100% of adults exhibiting evidence of past infection.3, 4 The primary infection in immunocompetent subjects is usually asymptomatic or limited to fever, mononucleosis-like illness or mild hepatitis, and followed by either chronic infection or viral latency from which virus may be reactivated.5 By contrast, CMV reactivation, which is common in situations favoring acquired defect of cellular immunity, including immunosuppressive therapy, malignancy, bone marrow or solid organ transplantation, and HIV/AIDS infection can induce high disease activity and mortality.3, 6
However, the outcomes of CMV-related hospitalization in IBD patients who have coexistent CMV disease or infection are not clear. Whether CMV disease or infection, especially CMV colitis, is associated with increased mortality is still debated. There are no studies that address the association between CMV-related hospitalization and health-care resource utilization, such as length of hospital stay (LOS) and total hospital charge. Because CMV disease or infection is an uncommon disease in IBD patients,7, 8 exploring large administrative data sets will help to determine the strength of association of CMV exposure and health-care outcomes. While individual patient's data is usually not available, results from large population data sets can be used to generate hypothesis for future prospective clinic studies.
In our study, we investigated the impact of CMV-related hospitalization on hospital mortality and health-care resource utilization for IBD patients from 2003 to 2011 at national and population-based levels by using the Nationwide In-patient Sample (NIS).
Methods
Data sources
All data were extracted from the NIS between 2003 and 2011. NIS is the largest all-payer in-patient care database in the United States.9 The database represents a 20% sample of nonfederal, acute-care hospitals in the United States and is stratified on hospital characteristics, e.g., location (urban vs. rural), teaching vs. non-teaching status, ownership (nonfederal, private, or public), and bed size (tertiles). The sampling frame includes community and general hospitals and academic medical centers comprising ~90% of all-hospital discharges in the United States. Each data entry includes a unique identifier, demographic variables (defined as age, gender, and race/ethnicity), type of admission, source of admission, principal (DX1) and secondary diagnoses (from DX2 to DX25), primary insurance payers, total hospital charges, and LOS.1 Comorbidity was assessed using Elixhauser score.10 The comorbidity burden was stratified based on Elixhauser score <3 (as reference) and ≥3.
Study population and definition of variables
The definitions of UC-, CD-, and CMV-related hospitalization
Our study population consisted of all adult discharges aged 19 years or older of IBD-related hospitalizations with or without CMV disease or infection (Appendix 1). It is important to note that because we used an administration database, CMV-related hospitalization in our study likely included both CMV disease and CMV infection. CMV infection refers to the detection of CMV antigens or antibodies in blood, whereas CMV disease is the presence of CMV infection and the presence of clinical signs and symptoms such as fever, leukopenia, or end-organ involvement. Some also consider the presence of typical CMV inclusions within cell preparations or end-organ tissue or positive viral cultures, crucial for the diagnosis of CMV disease.5, 6 In IBD patients, because CMV disease or infection most commonly involves the colon3, 4, 10, 11 and CMV activates and replicates more often in inflamed colonic mucosa,12 for the diagnosis of gastrointestinal CMV in IBD patients, detection of CMV inclusion bodies in biopsy specimens from the gastrointestinal mucosa either by hematoxylin and eosin or immunohistochemistry have been widely accepted.13 Therefore, in our study, we only included patients with IBD who had undergone either sigmoidoscopy or colonoscopy during the hospitalizations.
The discharges were considered to be IBD- and CMV-related if they met one of the following criteria: (a) principal diagnosis was UC or CD with a secondary diagnosis of CMV and they underwent either sigmoidoscopy or colonoscopy during the hospitalizations; or (b) a principal diagnosis of CMV and a secondary diagnosis of UC or CD and they underwent either sigmoidoscopy or colonoscopy during the hospitalizations.
Definition of hospital IBD admission volume
We calculated the number of discharges with a principal diagnosis of IBD (CD or UC) from each hospital during the study years. The hospitals were divided into low-volume (1–50 hospitalizations), medium-volume (50–150 hospitalizations), and high volume (more than 150 hospitalizations) hospitals depending on their annual volume of IBD-related hospitalizations as described and validated in a previous study.9
Definition of disease-specific severity
Disease-specific severity scores for CD14 and UC15 are quantified based on the presence of certain complications such as anemia, malnu;trition, requirement for blood transfusion, or total parenteral nutrition (Appendix 2).14, 15 The scores ranged from 0 to 7 for UC and 0 to 12 for CD, with higher scores representing greater severity of disease, and thus a higher likelihood of bowel resection (for CD) or colectomy (for UC). The disease-specific severity score has been shown to predict the outcome of interest in derivation and validation cohorts from the NIS and could be used to stratify hospitalizations into low, intermediate, and high-severity strata.14, 15, 16
Outcomes
Our interested outcomes were in-hospital mortality, LOS, and total hospital charges (Appendix 1).
Statistical analysis
SAS 9.3 (SAS Institute, Cary, NC) was used to perform all analyses, using appropriate survey estimation commands and strata weights. Data with missing information was excluded from statistical analysis for outcome analysis. Differences between patients with CMV disease or infection and those without were analyzed using χ2 tests or Student's t-tests, as appropriate. Multivariate linear regression was used to evaluate the effect of CMV disease or infection on LOS and total hospital charge and multivariate logistic regression was used to calculate adjusted odds ratios (ORs) and corresponding 95% confidence intervals (CIs) for in-hospital mortality. Each multivariate model adjusted for variables significantly associated with CMV disease or infection at P≤0.1 on univariate analysis.
Results
Demographic characteristics of CMV-related hospitalization among hospitalized IBD patients
After excluding patients (43,552) with missing data, a total of 145,282 IBD patients were identified from 2003 to 2011, among which there were a total of 144,484 hospitalizations with no CMV disease or infection (99.45%) and a total of 798 hospitalizations with CMV disease or infection (0.55%) (Table 1). A larger proportion of patients with CMV disease or infection, had more comorbidities (44.78% vs. 32.37%), and high disease-specific severity score (16.63% vs. 5.37%) were admitted to large hospitals (84.46% vs. 64.83%), hospitals with high IBD admission volume (23.36% vs. 8.47%), and urban teaching hospitals (71.47% vs. 44.97%) (Table 1).
Table 1. Univariate analysis of baseline characteristics among patients with IBD.
| No CMV disease or infection (n=144,484) | CMV disease or infection (n=798) | P-value | |||
|---|---|---|---|---|---|
| Age (mean, CI) | 48.45 (48.14, 48.77) | 50.59 (47.72, 53.45) | 0.1442 | ||
| Sex | 0.1339 | ||||
| Male | 62,122 | 43.00% | 388 | 48.65% | |
| Female | 82,362 | 57.00% | 410 | 51.35% | |
| Race | 0.0008 | ||||
| White | 107,732 | 74.56% | 567 | 71.00% | |
| Black | 17,661 | 12.22% | 73 | 9.17% | |
| Hispanic | 12,492 | 8.65% | 70 | 8.82% | |
| Other | 6,599 | 4.57% | 88 | 11.01% | |
| Hospital bed size | <0.0001 | ||||
| Small | 15,692 | 10.86% | 47 | 5.93% | |
| Medium | 35,127 | 24.31% | 77 | 9.61% | |
| Large | 93,664 | 64.83% | 674 | 84.46% | |
| Hospital type | <0.0001 | ||||
| Rural | 11,849 | 8.20% | 14 | 1.75% | |
| Urban non-teaching | 67,665 | 46.83% | 214 | 26.78% | |
| Urban teaching | 64,970 | 44.97% | 570 | 71.47% | |
| Insurance | 0.1038 | ||||
| Medicare | 40,832 | 28.26% | 240 | 30.12% | |
| Medicaid | 16,733 | 11.58% | 84 | 10.54% | |
| Privatea | 67,493 | 46.71% | 418 | 52.43% | |
| Otherb | 19,426 | 13.45% | 55 | 6.91% | |
| Elixhauser score | 0.0010 | ||||
| <3 | 97,721 | 67.63% | 441 | 55.22% | |
| ≥3 | 46,762 | 32.37% | 357 | 44.78% | |
| IBD admission volume | <0.0001 | ||||
| Low (0–50) | 90,705 | 62.78% | 289 | 36.19% | |
| Medium (51–150) | 41,535 | 28.75% | 323 | 40.45% | |
| High (>150) | 12,244 | 8.47% | 186 | 23.36% | |
| Admission day | 0.1765 | ||||
| Weekday | 112,318 | 77.74% | 655 | 82.05% | |
| Weekend | 32,165 | 22.26% | 143 | 17.95% | |
| Severity score | <0.0001 | ||||
| Low | 93,877 | 64.97% | 330 | 41.39% | |
| Intermediate | 42,846 | 29.65% | 335 | 41.98% | |
| High | 7,760 | 5.37% | 133 | 16.63% | |
CI, confidence interval; CMV, cytomegalovirus; HMO, Health Maintenance Organization; IBD, inflammatory bowel disease.
Private insurance includes HMO.
“Other” includes self-pay and with “no-charge”.
In-hospital mortality and health-care utilization of CMV-related hospitalization in IBD patients
On multivariate logistic regression analysis for in-hospital mortality, adjusting for patients' race, comorbidities, and disease-specific severity, hospital's size and type, and IBD admission volume, the odds of in-hospital mortality for an IBD patient with CMV disease or infection was 7.09 times higher (95% CI: 3.38–14.85) compared with an IBD patient without CMV (Table 2). Similarly, after adjusting for the above covariates, LOS, and the total hospital charge of an IBD patient with CMV disease or infection were 7.77 days longer (95% CI: 5.98–9.55, P<0.0001) and US$66,495 more (95% CI: 45,486–87,505, P<0.0001), respectively (Table 3).
Table 2. Multivariate logistic regression analysis of CMV disease or infection's impacts on hospital mortality in IBD patients.
| Odds ratio | 95% CI | P-value | |
|---|---|---|---|
| CMV disease or infection | <0.0001 | ||
| No | Reference | ||
| Yes | 7.09 | (3.38, 14.85) | |
| Race | 0.4162 | ||
| White | Reference | ||
| Black | 0.61 | (0.33, 1.12) | |
| Hispanic | 1.06 | (0.61, 1.83) | |
| Other | 0.79 | (0.35, 1.80) | |
| Hospital bed size | 0.7313 | ||
| Small | 0.81 | (0.47, 1.41) | |
| Medium | 1.01 | (0.69, 1.49) | |
| Large | Reference | ||
| Hospital type | 0.7391 | ||
| Rural | 1.24 | (0.67, 2.30) | |
| Urban non-teaching | 1.13 | (0.78, 1.62) | |
| Urban teaching | Reference | ||
| Elixhauser score | <0.0001 | ||
| <3 | Reference | ||
| ≥3 | 3.37 | (2.39, 4.77) | |
| IBD admission volume | 0.0785 | ||
| Low (0–50) | 2.71 | (1.13, 6.50) | |
| Medium (51–150) | 2.20 | (0.95, 5.11) | |
| High (>150) | Reference | ||
| Severity score | <0.0001 | ||
| Low | Reference | ||
| Intermediate | 2.84 | (1.95, 4.12) | |
| High | 6.44 | (4.05, 10.25) |
CI, confidence interval; CMV, cytomegalovirus; IBD, inflammatory bowel disease.
Table 3. Multivariate linear regression analysis of CMV disease or infection's impacts on LOS and total hospital charges in IBD patients.
|
LOS |
Total charges |
|||||
|---|---|---|---|---|---|---|
| Days | 95% CI | P-value | Dollars | 95% CI | P-value | |
| CMV disease or infection | <0.0001 | <0.0001 | ||||
| No | Reference | Reference | ||||
| Yes | 7.77 | (5.98, 9.55) | 66,495 | (45,486, 87,505) | ||
| Race | <0.0001 | <0.0001 | ||||
| White | Reference | Reference | ||||
| Black | −0.47 | (−0.70, −0.24) | −1,802 | (−3,516, −88) | ||
| Hispanic | −0.40 | (−0.61, −0.20) | 5,334 | (3,485, 7,184) | ||
| Other | −0.14 | (−0.50, 0.23) | 5,606 | (2,774, 8,439) | ||
| Hospital bed size | <0.0001 | <0.0001 | ||||
| Small | −0.83 | (−1.12, −0.54) | −8,336 | (−10,683, −5,988) | ||
| Medium | −0.53 | (−0.73, −0.32) | −4,157 | (−5,902, −2,412) | ||
| Large | Reference | Reference | ||||
| Hospital type | 0.0018 | <0.0001 | ||||
| Rural | −0.51 | (−0.80, −0.21) | −10,613 | (−12,735, −8,490) | ||
| Urban non-teaching | −0.13 | (−0.34, 0.07) | 2,506 | (724, 4,289) | ||
| Urban teaching | Reference | Reference | ||||
| Elixhauser score | <0.0001 | <0.0001 | ||||
| <3 | Reference | Reference | ||||
| ≥3 | 1.74 | (1.56, 1.92) | 11,588 | (10,354, 12,822) | ||
| IBD admission volume | 0.7647 | 0.0138 | ||||
| Low (0–50) | −0.18 | (−0.68, 0.32) | −6,096 | (−11,180, −1,011) | ||
| Medium (51–150) | −0.13 | (−0.62, 0.36) | −7,569 | (−12,747, −2,391) | ||
| High (>150) | Reference | Reference | ||||
| Severity score | <0.0001 | <0.0001 | ||||
| Low | Reference | Reference | ||||
| Intermediate | 2.48 | (2.31, 2.66) | 14,157 | (12,954, 15,359) | ||
| High | 9.63 | (9.01, 10.26) | 56,657 | (51,817, 61,496) | ||
CI, confidence interval; CMV, cytomegalovirus; IBD, inflammatory bowel disease; LOS, length of stay.
Other factors associated with increased mortality, prolonged LOS and more hospital charge (Tables 2 and 3) included more comorbidities and high disease-specific severity. Patients' race, hospital's size and type were associated with LOS and hospital charge (Table 3). High IBD admission volume was only associated with more hospital charge (Table 3).
Discussion
Our nationwide analysis of hospital discharges showed that CMV-related hospitalization in IBD patients who have coexistent CMV disease or infection was associated with significant mortality, prolonged LOS, and higher cost. To our knowledge, this is the first study to investigate in-hospital mortality and health-care resource utilization of CMV-related hospitalization among IBD patients in a large administrative data set.
In IBD patients, CMV is able to induce at least three types of disorders: (i) CMV infection without intestinal involvement; (ii) CMV infection involving the gastrointestinal tract, which most commonly presents as CMV colitis; and (iii) intestinal CMV infection limited to histologic stigmata of local CMV reactivation without systemic or local signs of disease.3 As the ICD-9-CM (International Classification of Diseases, Ninth Revision, Clinical Modification) code of CMV disease or infection has only one code, encompassing all types of CMV disease or infection, it was likely that we have included patients with CMV disease or infection without gastrointestinal involvement, such as CMV pneumonia, CMV retinitis, or hemophagocytic lymphohistiocytosis. However, in IBD patients, the colon is the most common site for CMV-related disease or infection.3, 4, 8, 11 Extracolonic manifestations of CMV disease or infection, such as CMV pneumonia or hemophagocytic lymphohistiocytosis, are exceedingly rare and only reported in case reports in IBD patients even if in the presence of immunosuppressant therapy.8, 17, 18 Furthermore, CMV disease or infection in active IBD patients seems to be a peculiar local process that could be facilitated by the tropism of CMV for granulation tissue, and triggered by local (proinflammatory cytokines) and systemic (medical-induced immunosuppression) conditions.8 In our study, we only included patients with IBD discharge codes who have received either sigmoidoscopy or colonoscopy during the hospitalization. Therefore, the CMV disease or infection in our study most likely represented CMV colitis in the majority of hospitalized IBD patients.
In our study, a significantly larger proportion of IBD patients with CMV disease or infection were admitted to urban teaching, large hospitals, and hospitals with high IBD admission volume, suggesting that more CMV disease or infection were managed in more specialized or experienced hospitals.
CMV disease or infection leads to high morbidity and mortality in patients with immunosuppressive drugs or corticosteroid, as well as in organ transplant and AIDS patients.19 CMV may cause severe colitis with significant morbidity and mortality in the immunocompetent host as well.20 However, the outcomes of CMV disease or infection, especially CMV colitis, in IBD patients are still debated. Coexistent CMV colitis in severe and refractory IBD patients has been associated with high rates of toxic megacolon, colectomy rates, and mortality.2, 5, 21 Anti-viral therapy can induce remission in IBD patients with concomitant CMV colitis.5, 6, 20, 22, 23, 24 Therefore, the American College of Gastroenterology guideline,25 European Crohn's and Colitis Organization consensus,26 and Canada consensus statements27 have stressed the importance of ruling out CMV disease or infection in all cases of severe colitis, especially in steroid-refractory patients. On the other hand, CMV was probably just an “innocent bystander” without an actual impact on remission rate, mortality, or requirement for surgery.7, 21, 23, 28, 29, 30, 31 A few case series studies found no benefit of anti-viral therapy with regard to the need for surgery,21, 27, 31, 32 which may support the role of CMV as an innocent bystander of intestinal inflammation, with no pathogenic activity by itself. Despite the above controversy, our study found that CMV-related hospitalization has been associated with significant mortality, prolonged LOS, and higher hospital costs among hospitalized IBD patients. However, we could not determine whether CMV disease or infection was a causative factor as this would require a prospective study. Based on these results, we suggest that the health provider should be vigilant about the coexistent CMV disease or infection in hospitalized IBD patients. In addition, the results also support that coexistent CMV disease or infection might be an indicator of severe inflammation in hospitalized IBD patients.6
There are some inherent limitations to our study. Although the current American College of Gastroenterology and European Crohn's and Colitis Organization guidelines emphasize the importance of awareness of coexistent CMV disease or infection in severe colitis patients, not every hospitalized IBD patient in our study has been tested for CMV. In addition, although the main target of CMV disease or infection is the gastrointestinal tract and CMV colitis is the most common type of CMV disease or infection in IBD patients,4 the single ICD-9-CM code of CMV might include all types of CMV disease or infection. Furthermore, the diagnostic modalities of CMV disease of infection in our study were unknown. There is a wide range of normal values for CMV diagnostic tests that are institution dependent. Several methods are currently used for detecting CMV disease or infection. For the diagnosis of gastrointestinal CMV, combined CMV antigenemia assay and detection of CMV inclusion bodies in biopsy specimens from the gastrointestinal mucosa either by hematoxylin and eosin or immunohistochemistry have been proposed. The real-time tissue PCR assay that allows more sensitive and rapid detection of CMV-DNA in clinical samples has also been widely used in clinical practice.13 This data type is not available in the NIS database. In our study, by only including the IBD patients who have received either sigmoidoscopy or colonoscopy, the patients with CMV disease or infection more likely had CMV colitis. Another limitation of the NIS database in our study was that the IBD severity could not be assessed based on patient's symptoms, signs, and test results. CMV colitis, however, is found to be more prevalent in severe or steroid-refractory IBD patients.7, 23, 24 The association between CMV disease or infection and adverse hospital outcomes may only reflect the IBD severity.6 In our study, we controlled for the disease-specific severity that is determeind by using the variables available in the NIS database, which has been validated by previous studies.14, 15, 16 In addition, NIS database analysis did not allow us to distinguish between CMV infection and disease. Therefore, the association between CMV-related hospitalization and adverse outcomes might be because of either CMV disease or CMV infection. Also, given the structure of the NIS, we could not determine the impact of CMV treatment on outcomes. The significance of CMV inclusions on colon biopsies in the absence of systemic features as well as anti-viral treatment in this context remains controversial. Some authors, including the current American College of Gastroenterology guideline along with consensus statements from European Crohn's and Colitis Organization and Canada, advocate the treatment of CMV disease or infection in IBD patients.22, 25, 26, 27 Other authors reported remission or improvement of IBD patients with coexistent CMV disease or infection without anti-viral therapy.21, 28, 29 To address this question, a randomized clinical trial is warranted.
Despite above limitations, our study also has strengths. The NIS database provides a large number of patients with discharge diagnosis of CMV disease or infection and IBD, which otherwise would not be possible from smaller single-center or multicenter studies because of the relatively uncommon CMV disease or infection in IBD patients.7, 8 In addition, by only focusing on patients with IBD who received either sigmoidoscopy or colonoscopy during the hospitalization, CMV disease or infection in our cohort is enriched to capture those patients more likely having CMV colitis. The benefit of using the NIS database is that the results represent the current national in-patient health-care utilization of IBD patients with CMV disease or infection.
In conclusion, IBD patients who have coexistent CMV disease or infection had significant in-hospital mortality, prolonged LOS, and higher total hospital charge. This strong association warrants prospective trials to determine the impact of anti-viral therapy in IBD patients with isolated colonic CMV disease or infection and/or systemic disease.
Study Highlights
Appendix 1
International Classification of Diseases, Ninth revision, Clinical modification code (ICD-9-CM) codes
Crohn's disease (CD) 555, 555.1, 555.2, and 555.9
Ulcerative colitis (UC) 556, 556.0, 556.1, 556.2, 556.3, 556.4, 556.5, 556.6, 556.8, and 556.9
CMV disease or infection 078.5
Procedures:
Flexible sigmoidoscopy 45.24
Rigid sigmoidoscopy 48.23
Colonoscopy 45.21, 45.22, 45.23, and 45.25
Severity score variables:
Anemia: 280, 280.1, 280.9, 285.1, and 285.9
Blood transfusion 99.0, 99.00, 99.03, and 99.04
Malnutrition: 263, 263.0, 263.1, 263.2, 263.8, and 263.9
Parental nutrition: 99.15
Obstructing: 560, 560.0, 560.1, 560.2, 560.3, 560.8, 560.9, 568.0, and 537.3
Fistulizing: 537.4, 567.2, 567.21, 567.22, 569.5, 569.8, 569.81, 569.82, 569.83, 569.89, 593.3, 593.82, 596.1, and 619.1
Volume depletion: 276.5
Clostridium difficile infection 008.45.
Appendix 2
|
CD |
UC |
||
|---|---|---|---|
| Characteristic | Points | Characteristic | Points |
| Inflammatory* | 0 | Anemia | 1 |
| Obstructing* | 2 | Requirement for blood transfusion | 1 |
| Fistulizing* | 4 | Malnutrition | 2 |
| No anemia | 0 | Total parental nutrition (TPN) | 2 |
| Anemia | 1 | Admission to teaching hospital | 1 |
| Requirement for blood transfusion | 1 | ||
| No malnutrition/TPN | 0 | ||
| Malnutrition | 2 | ||
| TPN | 1 | ||
| Volume depletion | 1 | ||
| Admission to teaching hospital | 1 | ||
| Clostridium diffcile Infection | 1 | ||
| Risk stratification for severity | CD | UC | |
| Low severity | 0–1 | Low severity | 0–1 |
| Intermediate severity | 2–4 | Intermediate severity | 2–3 |
| Severe severity | ≥5 | Severity | ≥4 |
*Only one disease behavior is assigned per hospitalization.
Risk score to predict sever hospitalization course among patients with either ulcerative colitis (UC) or Crohn' disease (CD).
Guarantor of the article: Cheng Zhang, MD, PhD.
Specific author contributions: Dr. Cheng Zhang had designed and conducted the research and written the manuscript. Dr. Alice Hinton had performed the statistical analysis. Dr. Somashekar Krishna, Razvan Arsenescu, Edward Levine and Darwin Conwell had participated in discussion the research project, interpretation of the results, and written the manuscript.
Financial support: None.
Potential competing interests: None.
References
- Nguyen GC, Kaplan GG, Harris ML et al. A national survey of the prevalence and impact of Clostridium difficile infection among hospitalized inflammatory bowel disease patients. Am J Gastroenterol 2008; 103: 1443–1450. [DOI] [PubMed] [Google Scholar]
- Kishore J, Ghoshal U, Ghoshal UC et al. Infection with cytomegalovirus in patients with inflammatory bowel disease: prevalence, clinical significance and outcome. J Med Microbiol 2004; 53: 1155–1160. [DOI] [PubMed] [Google Scholar]
- Pillet S, Pozzetto B, Jarlot C et al. Management of cytomegalovirus infection in inflammatory bowel diseases. Dig Liver Dis 2012; 44: 541–548. [DOI] [PubMed] [Google Scholar]
- Garrido E, Carrera E, Manzano R et al. Clinical significance of cytomegalovirus infection in patients with inflammatory bowel disease. World J Gastroenterol 2013; 19: 17–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandiel A, Lashner B. Cytomegalovirus colitis complicating inflammatory bowel disease. Am J Gastroenterol 2006; 101: 2857–2865. [DOI] [PubMed] [Google Scholar]
- Lawlor G, Moss AC. Cytomegalovirus in inflammatory bowel disease: pathogen or innocent bystander? Inflamm Bowel Dis 2010; 16: 1620–1627. [DOI] [PubMed] [Google Scholar]
- Dimitroulia E, Spanakis N, Konstantinidou AE et al. Frequent detection of cytomegalovirus in the intestine of patients with inflammatory bowel disease. Inflamm Bowel Dis 2006; 12: 879–884. [DOI] [PubMed] [Google Scholar]
- Domènech E, Vega R, Ojanguren I et al. Cytomegalovirus infection in ulcerative colitis: a prospective, comparative study on prevalence and diagnostic strategy. Inflamm Bowel Dis 2008; 14: 1373–1379. [DOI] [PubMed] [Google Scholar]
- Ananthakrishnan AN, McGinley EL, Binion DG. Does it matter where you are hospitalized for inflammatory bowel disease? A nationwide analysis of hospital volume. Am J Gastroenterol 2008; 103: 2789–2798. [DOI] [PubMed] [Google Scholar]
- Elixhauser A, Steiner C, Harris DR et al. Comorbidity measures for use with administrative date. Med Care 1998; 36: 8–27. [DOI] [PubMed] [Google Scholar]
- Hommes DW, Sterringa G, van Deventer SJ et al. The pathogenicity of cytomegalovirus in inflammatory bowel disease: a systematic review and evidence-based recommendations for future research. Inflamm Bowel Dis 2004; 10: 245–250. [DOI] [PubMed] [Google Scholar]
- Nakase H, Matsumura K, Yoshino T et al. Sytematic review: cytomegalovirus infection in inflammatory bowel disease. J Gastroenterol 2008; 4310: 735–40.21. [DOI] [PubMed] [Google Scholar]
- Köroğlu E, Çelik AF. Prevalence, predictive factors and ideal treatment of cytomegalovirus infection in IBD patients. Turk J Gastroenterol 2012; 23 ((Suppl 2)): 35–40. [DOI] [PubMed] [Google Scholar]
- Ananthakrishnan AN, McGinley EL, Binion DG et al. A novel risk score to stratify severity of Crohn's disease hospitalizations. Am J Gastroenterol 2010; 105: 1799–1807. [DOI] [PubMed] [Google Scholar]
- Ananthakrishnan AN, McGinley EL, Binion DG et al. Simple score to identify colectomy risk in ulcerative colitis hospitalizations. Inflamm Bowel Dis 2010; 16: 1532–1540. [DOI] [PubMed] [Google Scholar]
- Ananthakrishnan AN, McGinley EL, Binion DG et al. A nationwide analysis of changes in severity and outcomes of inflammatory bowel disease hospitalizations. J Gastrointest Surg 2011; 15: 267–276. [DOI] [PubMed] [Google Scholar]
- Cascio A, Iaria C, Ruggeri P et al. Cytomegalovirus pneumonia in patients with inflammatory bowel disease: a systematic review. Int J Infect Dis 2012; 16: e474–e479. [DOI] [PubMed] [Google Scholar]
- Hamlin PJ, Shah MN, Scott N et al. Systemic cytomegalovirus infection complicating ulcerative colitis: a case report and review of the literature. Postgrad Med J 2004; 80: 233–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Ovidio V, Vernia P, Gentile G et al. Cytomegalovirus infection in inflammatory bowel disease patients undergoing anti-TNFalpha therapy. J Clin Virol 2008; 43: 180–183. [DOI] [PubMed] [Google Scholar]
- Vega R, Bertrán X, Menacho M et al. Cytomegalovirus infection in patients with inflammatory bowel disease. Am J Gastroenterol 1999; 94: 1053–1056. [DOI] [PubMed] [Google Scholar]
- Matsuoka K, Iwao Y, Mori T et al. Cytomegalovirus is frequently reactivated and disappears without antiviral agents in ulcerative colitis patients. Am J Gastroenterol 2007; 102: 331–337. [DOI] [PubMed] [Google Scholar]
- Papadakis KA, Tung JK, Binder SW et al. Outcome of cytomegalovirus infections in patients with inflammatory bowel disease. Am J Gastroenterol 2001; 96: 2137–2142. [DOI] [PubMed] [Google Scholar]
- Criscuoli V, Casà A, Orlando A et al. Severe acute colitis associated with CMV: a prevalence study. Dig Liver Dis 2004; 36: 818–820. [DOI] [PubMed] [Google Scholar]
- Cottone M, Pietrosi G, Martorana G et al. Prevalence of cytomegalovirus infection in severe refractory ulcerative and Crohn's colitis. Am J Gastroenterol 2001; 96: 773–775. [DOI] [PubMed] [Google Scholar]
- Kornbluth A, Sachar DB, , Practice Parameters Committee of the American College of Gastroenterology. Ulcerative colitis practice guidelines in adults: American College of Gastroenterology, Practice Parameters Committee. Am J Gastroenterol 2010; 105: 501–523. [DOI] [PubMed] [Google Scholar]
- Rahier JF, Yazdanpanah Y, Colombel JF et al. The European (ECCO) Consensus on infection in IBD: what does it change for the clinician? Gut 2009; 58: 1313–1315. [DOI] [PubMed] [Google Scholar]
- Bitton A, Buie D, Enns R et alCanadian Association of Gastroenterology Severe Ulcerative Colitis Consensus Group. Treatment of hospitalized adult patients with severe ulcerative colitis: Toronto consensus statements. Am J Gastroenterol 2012;107:179–194. [DOI] [PubMed] [Google Scholar]
- Lévêque N, Brixi-Benmansour H, Reig T et al. Low frequency of cytomegalovirus infection during exacerbations of inflammatory bowel diseases. J Med Virol 2010; 82: 1694–1700. [DOI] [PubMed] [Google Scholar]
- Kim JJ, Simpson N, Klipfel N et al. Cytomegalovirus infection in patients with active inflammatory bowel disease. Dig Dis Sci 2010; 55: 1059–1065. [DOI] [PubMed] [Google Scholar]
- de Saussure P, Lavergne-Slove A, Mazeron MC et al. A prospective assessment of cytomegalovirus infection in active inflammatory bowel disease. Aliment Pharmacol Ther 2004; 20: 1323–1327. [DOI] [PubMed] [Google Scholar]
- Delvincourt M, Lopez A, Pillet S et al. The impact of cytomegalovirus reactivation and its treatment on the course of inflammatory bowel disease. Aliment Pharmacol Ther 2014; 39: 712–720. [DOI] [PubMed] [Google Scholar]
- Eyre-Brook IA, Dundas S. Incidence and clinical significance of colonic cytomegalovirus infection in idiopathic inflammatory bowel disease requiring colectomy. Gut 1986; 27: 1419–rt1425. [DOI] [PMC free article] [PubMed] [Google Scholar]


