Abstract
Background & objectives:
India has the third highest burden of HIV and highest number of cervical cancer in the world. A cross-sectional study was performed to determine the prevalence and types of human papillomavirus (HPV) infection, and the factors associated with HPV infection and abnormal cervical cytology in HIV-positive women attending the Antiretroviral Therapy (ART) Centre in a tertiary care hospital in eastern India.
Methods:
We screened 216 HIV- positive women with Papanicolau smear cytology and HPV testing. HPV DNA was detected by using consensus primers followed by sequencing.
Results:
Of the 216 HIV-positive women screened, 58 (26.85%) were HPV-positive; 56 (25.9%) were of high-risk (HR) HPV type. The most prevalent HPV type was HPV-16 (7.9%); non 16 and 18 HPV types were present in 17.6 per cent patients. Age ≤ 35 yr [(OR), 2.56 (1.26-5.19)], illiteracy [OR, 2.30 (1.19-4.46)], rural residence [OR, 3.99 (1.27-12.56)] and CD4 ≤350/μl [OR, 2.46 (1.26-4.83)] were associated with increased risk of acquisition of HPV. One hundred thirty nine (74.33%) patients had normal/ negative for intraepithelial lesions (NILM) cytology, three (1.60%) had atypical squamous cells of undetermined significance (ASCUS), 32 (17.11%) had low-grade squamous intraepithelial lesions (LSIL), 10 (5.35%) had high-grade squamous intraepithelial lesions (HSIL) and three (1.60%) had carcinoma cervix. WHO clinical Stage III and IV [OR, 2.83 (1.07-7.49)] and CD4 ≤350/μl [OR, 2.84 (1.30-6.20)] were risk factors for abnormal cytology.
Interpretation &conclusions:
Our study showed 26.85 per cent HPV positivity in HIV infected women in this region, with HPV-16 as the commonest genotype. Abnormal cervical cytology was seen in about 25 per cent women. Regular Pap smear screening as recommended by the National AIDS Control Organization will help in early detection of cervical abnormalities in HIV- positive women.
Keywords: Cervical cytology, human immunodeficiency virus, human papillomavirus, papanicolau smear cytology, polymerase chain reaction, sequencing
Human papillomavirus (HPV) is one of the most prevalent sexually transmitted infections in the world. High-risk (HR) genotypes of HPV have been implicated as a cause of cervical intraepithelial neoplasia and cervical cancer and possibly of other neoplasias of the lower genital tract in women1. Human immunodeficiency virus (HIV) - positive women have the highest risk for increased incidence and rapid progression of HPV-induced cervical precursor lesions, cervical intraepithelial neoplasia (CIN) and invasive cervical cancer (ICC)2,3. It has been observed in multiple studies4,5 including from India6 that HIV-infected women are two to five times more likely than HIV-uninfected women to manifest cervical intraepithelial neoplasia and cervical cancer. A large prospective cohort study observed that 20 per cent HIV-infected and 5 per cent HIV-uninfected women developed squamous intraepithelial lesions (SIL). HIV and HPV infection were significant risk factors for incident SIL7. Studies have shown that the prevalence of high-risk HPV is lower (20-40%) among HIV-infected women in countries having low level HIV epidemic as compared to countries with high level epidemic like Africa (45-90%)8,9,10,11,12.
India has the third largest number of people living with HIV/AIDS (acquired immunodeficiency syndrome) and accounts for nearly 1/4th of the global cervical cancer deaths13,14. Of the 2.09 million people living with HIV/ AIDS in India, 39 per cent are women13. There are only a few studies from the country regarding the prevalence and types of HPV and cervical abnormalities among HIV-positive women. A hospital based study from the eastern part of India observed a prevalence of oncogenic HPV among HIV-positive women to be 46.2 per cent15 whereas a study from northern India showed a prevalence of high-risk HPV in 20 per cent16. In a study from Pune, Pap smear abnormalities were seen in 6.3 per cent of HIV-positive women and were more common among women >30 yr and those with opportunistic infections17. In a recent study from Mumbai cervical abnormalities were observed in 19 per cent of HIV-positive women18. A population based study from eastern Uttar Pradesh observed the prevalence of HPV in clinically asymptomatic women as 9.9 per cent19. However, there are no data on the prevalence of cervical abnormalities and HPV infection among HIV-positive women in this region. Thus, this study was performed to estimate the prevalence of Pap smear abnormalities and HPV infection and the associated risk factors among HIV-infected women attending the Antiretroviral Therapy (ART) centre of a tertiary care hospital in eastern part of India.
Material & Methods
A cross-sectional study was conducted between December 2010 to June 2012 in the ART Centre of Centre of Excellence, department of Medicine, and department of Obstetrics and Gynaecology, Institute of Medical Sciences, Banaras Hindu University (BHU), Varanasi, India. The study was approved from the Ethics committee of Institute of Medical Sciences, BHU and written informed consent was obtained from all the participants.
In December 2010, there were 1540 females registered and were in active follow up. Of them, 585 were from in and around Varanasi. The sample size was 216, which was calculated assuming 35 per cent prevalence of HPV and population size of 585 at 5 per cent P value and 5 per cent absolute difference in the estimate. Of the 585 women we selected 216 patients through random numbers. If the selected HIV positive women did not give their consent, they were replaced by the next reporting patient similar to them. Similarity was considered by age and place of residence (rural/urban) of the patient.
The cervical scrapes were collected randomly from HIV-positive women aged 19-65 yr attending ART centre and were sent to the department of Pathology for Cytology. HPV detection was done in the Centre of Excellence. Exclusion criteria included a positive urine pregnancy test, prior hysterectomy and those who refused consent.
Data were extracted from white cards maintained in the ART centre for HIV-positive women which included age, date of HIV diagnosis, date of start of antiretroviral drugs, mode of HIV transmission, history of surgical intervention, WHO clinical stage, weight, haemoglobin, CD4 count and opportunistic infections at the time of Pap smear collection. CD4+ lymphocyte counts were determined using BD FACS Calibur (USA) and the values were expressed as cells/μl.
A conventional Papanicolau (Pap) smear with Ayre's spatula was done to look for cytological changes which were classified according to Bethesda system: normal i.e. no cell changes; NILM (negative for intraepithelial lesions and malignancy) which includes inflammatory changes, organisms, atrophic changes and reactive changes; ASCUS (atypical squamous cells of undetermined significance); ASC-H (atypical squamous cells cannot exclude a high-grade squamous intraepithelial lesion); LSIL (low-grade squamous intraepithelial lesions); and HSIL (high-grade squamous intraepithelial lesions)20. Women with Pap smear abnormality were referred to the department of Obstetrics & Gynaecology.
Scraped cervical cells were also obtained from the exocervix and were placed in 3-5 ml of phosphate buffered saline (pH 7.2) and frozen at -20°C until DNA was extracted.
DNA extraction from cervical scrapes: DNA was extracted from cervical cell suspensions using QIAamp DNA Blood Mini Kit (QIAGEN, Hilden, Germany) according to manufacturer's protocol and stored at -20° C until further processing. The quality of DNA and PCR product was checked on agarose gel. After ascertaining its quality and quantity by NanoDrop (Thermo Scientific, USA), the samples were sent for sequencing.
HPV detection and sequencing: Polymerase chain reaction (PCR) (amplification) was done for detection of HPV in all cervical samples by using consensus primers21: (F) 5’-TGTCAAAAACCGTTGTGTCC-3’; (R) 5’-GAGCTGTCGCTTAATTGCTC-3’. All HPV- positive samples were subjected to sequencing for confirmation of HPV types. DNA sequencing was performed on 3730XL DNA genetic analyzer (Applied Biosystem, USA) using the Big Dye Terminator Cycle Sequencing Ready Reaction Kit version 3.1 (Applied Biosystem, CA, USA) with the consensus primers by SciGenom, Labs Pvt. Ltd., Cochin, Kerala, India. The resulting sequences were compared with HPV sequences of known types using the basic local alignment search tool from the NCBI website (www.ncbi.nlm.nih.gov/blast/Blast.cgi). HPV types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68, 73 and 82 were considered as highly oncogenic [high-risk (HR)], while HPV types 26, 53 and 66 as probably oncogenic. HPV types 6, 11, 40, 42, 43, 44, 54, 61, 70, 72, 81 and CP6108 were considered as low oncogenic potential [low-risk (LR)]22.
Statistical analysis: Statistical analyses were performed using the Statistical Package for Social Sciences software, version 16 (SPSS, Inc., USA). For bivariate analysis, variables were compared between HPV-positive and negative and Pap smear cytology normal or abnormal HIV- positive women by performing chi square test, t test or the Mann-Whitney U test where appropriate. Binary logistic regression analysis was performed to analyze the associations between variables. Two tailed P values less than 0.05 were considered significant. For analysis patients with normal or NILM were considered as normal Pap smear and those with ASCUS, LSIL, HSIL and carcinoma cervix were considered as abnormal Pap smear.
Results
We screened 216 HIV-positive women in this study. Baseline characteristics of the HIV-positive women are given in Table I. The mean age was 35.27 yr (19-65 ± 10.23 yr). Median CD4+ cell counts were 368/μl (IQR 239.25-523.75) at the time of Pap smear collection. Mean weight and mean haemoglobin levels were 44.46 ±7.79 kg and 10.63 ± 1.76 g/dl, respectively. Twenty eight patients were treatment naive and 188 (87%) were on ART.
Table I.
Baseline characteristics and risk factor analysis of HPV-positive and negative HIV-positive women (n=216)
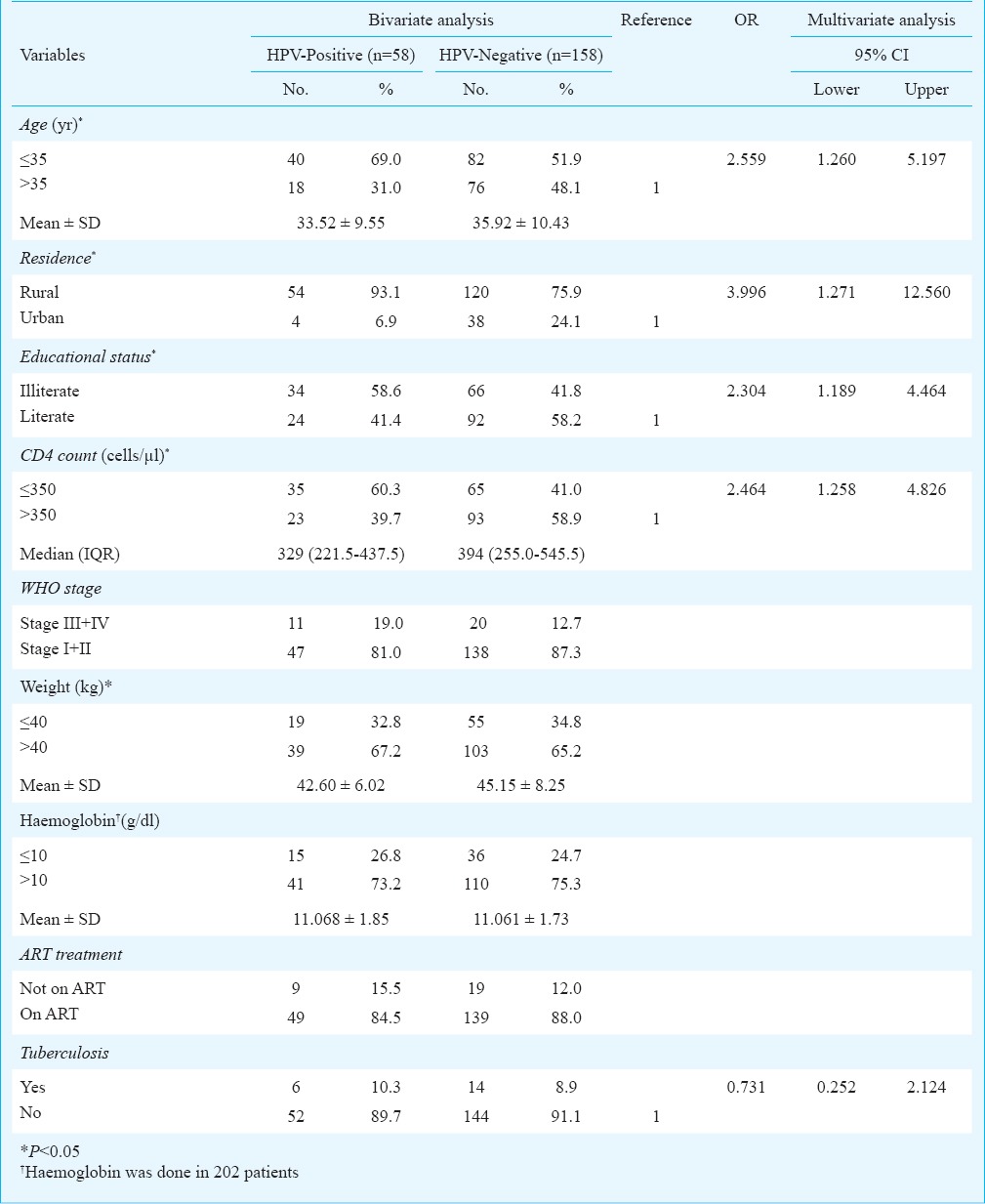
PCR & sequencing: HPV DNA was detected by PCR using consensus primers to generate a fragment of about 250 bp. HPV DNA was detected in 58 (26.85%) HIV-positive women. After sequencing, infection with high-risk HPV was found in 56 of 58 samples, i.e. 25.9 per cent of all HIV-positive women, probably high-risk HPV was found in two samples. The most prevalent HPV type in the study group was HPV-16, identified in 7.9 per cent (17/216) followed by HPV-31, HPV-35 and HPV-58 in 4.2 per cent (9/216) each, HPV-52 (2.3%, 5/216), HPV-18 (1.4%, 3/216), HPV-33 (0.93%, 2/216), HPV-56 and HPV-68 (0.5% each, 1/216). GenBank accession numbers for the 11 types of HPV reported in our study were from GenBank KJ869425 to GenBank KJ869435. Probably high-risk HPV types, HPV-66 and HPV-67 were identified in 0.93 per cent cases (2/216). Of the 58 HPV positive women, 54 were from rural background and 32 of 54 were illiterate. Age ≤35 yr [odds ratio (OR), 2.56; 95% CI, 1.26-5.19], illiteracy (OR, 2.30; 95% CI, 1.19-4.46), rural residence (OR, 3.99; 95% CI, 1.27-12.56) and CD4 count ≤ 350/μl (OR, 2.46; 95% CI, 1.26-4.83) were associated with increased risk of acquisition of HPV in HIV- positive women (Table I).
Cervical cytology: Cervical smear cytology reports were lost in 29 HIV-positive women. Among the 187 HIV- positive women cervical smear showed that 16.04 per cent (30) had normal cytology, 58.29 per cent (109) had NILM, 1.60 per cent (3) had ASCUS, 17.11 per cent (32) had LSIL, 5.35 per cent (10) had HSIL and 1.60 per cent (3) had carcinoma cervix. Patients with ASCUS and LSIL were called for repeat Pap smear after six months. Patients with HSIL were treated by loop electrosurgical excision procedure (LEEP) and specimen were send for histopathological examination.
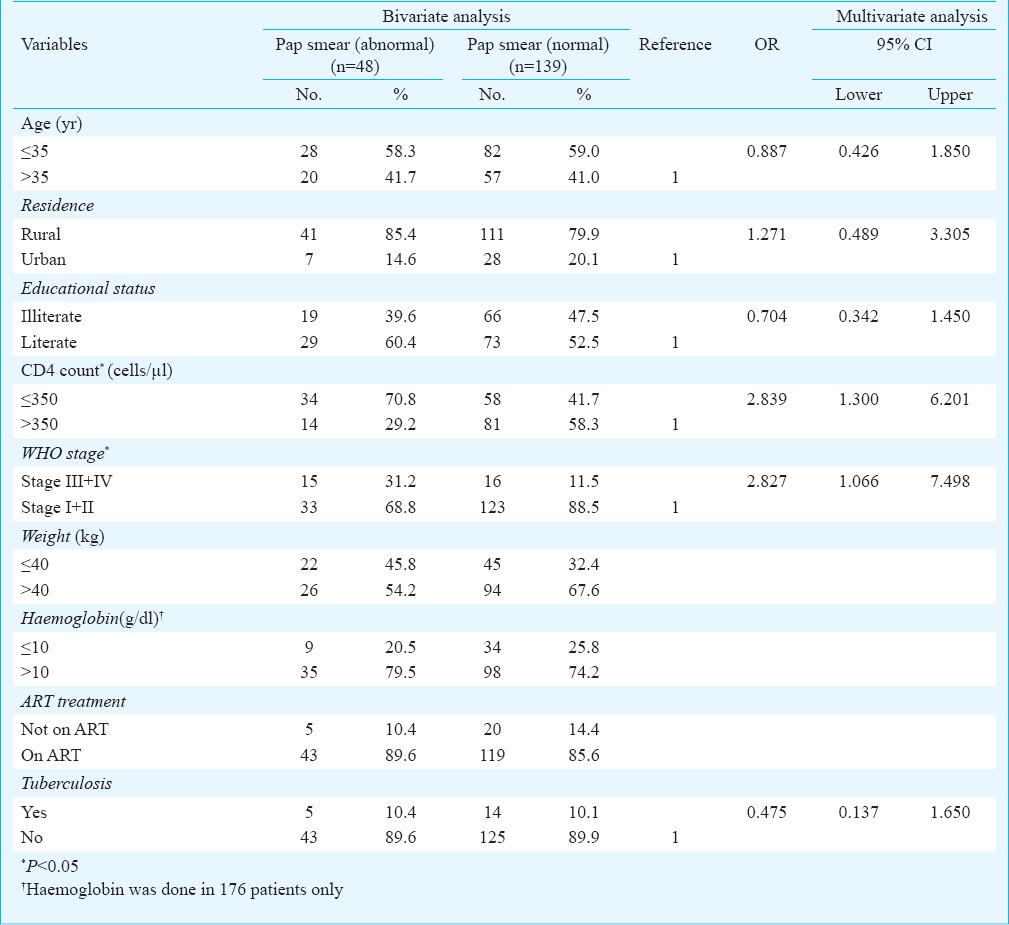
The risk factors for abnormal Pap smear in HIV-positive women were WHO clinical stage III and IV (OR, 2.83; 95% CI, 1.07-7.50) and CD4 count ≤350/μl (OR, 2.84; 95% CI, 1.30-6.20) (Table II).
Table II.
Characteristics of normal and abnormal Pap smear cytology among HIV-positive women (n=187)
HPV genotype distribution with cervical smear cytology: In patients with normal or NILM cytology (n=139), HPV-16 and 18 genotypes were present in nine (6.5%) each, HPV-35 in seven (5%), HPV-31 in six (4.3%), HPV-52 in two (1.4%) and HPV 33, 66, 67, 68 in one patient (0.7%) each. Thus, 25.18 per cent (35/139) women with normal or NILM cytology had high-risk HPV. None of the patient with ASCUS had HPV. In patient with LSIL (n=32), HPV-31 was present in three (9.4%), HPV-16 in two (6.3%) and HPV- 18, 33, 52, 56 in one (3.1%) patient each. In patient with HSIL (n=10), HPV-16 was present in two (20%), HPV-35 and 52 in one (10%) each. Of the three patients with carcinoma cervix one had HPV-16. Among the 29 patients in whom the cytology reports were lost, HPV-16 was present in three (10.3%), HPV-18 in two (6.9%), HPV-35 and 52 in one (3.4%) patient each.
Discussion
In this cross-sectional study, HPV infection was seen in 26.85 per cent HIV-positive women which was higher than that observed in general population in this region19. Most (56/58) of the HPV types present in our HIV-positive women were of high-risk. Prevalence of high-risk HPV in HIV-infected females in India have been reported 35.3 per cent from Pune (western India), 46.2 per cent from West Bengal, 20 per cent from Chandigarh (north India) and 37.3 per cent from Vellore (south India)10,15,16,23.
HPV-16 was the commonest genotype, identified in 7.9 per cent women in this study, however, 17.6 per cent were infected with non 16 and 18 HPV types. Prevalence of non HPV-16 and 18 high risk infection in HIV-positive women in India varies from 10.76-30.21 per cent15,16,24. Similar findings have been observed in a large meta-analysis of 5578 HIV-positive women from four continents25. Although there is no known reason why non-HPV 16 and 18 types are common in HIV positive women, it has been hypothesized that due to decrease immunity these patients cannot clear these non-HPV16 genotypes12,23. This suggests that the currently available bivalent (HPV16/18) or quadrivalent (HPV6/11/16/18) vaccines may not be effective in HIV-positive population.
In our study HIV-positive women with age ≤ 35 yr had higher risk of HPV infection. It has been observed that the prevalence of cervical HPV infection decreases in women after the age of 30 and those with persistent infection are at a highest risk for the development of high-grade squamous intraepithelial lesions or invasive cervical cancer26. Low CD4 count was found to be associated with increased risk of HPV infection in our study, similar to other studies27,28. Low CD4 count suggests a weakened immune system which could lead to persistence of HPV infection. Women residing in the rural areas were also at increased risk of HPV infection in our study similar to an earlier population based study from this region19. Illiteracy in women particularly in rural areas can lead to the lack of knowledge about their sexual health and prevent them from asserting themselves in matter related to sexual practices. This makes them vulnerable to unsafe sex leading to higher risk of acquiring HPV infection. It has been shown that the ART increased the clearance of oncogenic HPV types29. Thus, ART should be started in this vulnerable group of young, illiterate HIV positive women of rural background.
In a meta-analysis 57.9 per cent of HIV-positive females had normal cytology, 36.8 per cent had ASCUS/LSIL and 5.2 per cent had HSIL25. Similar findings were also observed in other studies from India18,24 as well as in the present study where we found 74.33 per cent. HIV-positive women with normal cytology or NILM. The risk factors for abnormal cervical cytology in HIV-positive women in our study were CD4 count ≤ 350/μl and WHO stage III and IV. Increased risk of cervical cytological abnormalities in patients with low CD4 count has been observed in other studies also30,31. Thus the current National AIDS Control Organization (NACO) guidelines of starting ART in all HIV positive individuals with CD4 count < 350/μl and in those with WHO stage III and IV irrespective of CD4 count will definitely decrease the number of women with SIL32.
The overall prevalence of HR-HPV was 25.18 per cent among the HIV-positive women without cytological abnormality in our study which was similar to the 36.3 per cent observed in a meta-analysis25. It has also been observed that oncogenic HPV infection predicts progression of cervical dysplasia from normal to abnormal SIL in HIV-positive women29. The American College of Obstetricians and Gynecologists recommends that women who are infected with HIV (or otherwise immunocompromised) should undergo cervical cytology for cancer screening twice in the first year after diagnosis of HIV infection and then annually, provided the test results are normal33. However, a study reported that adding HPV testing to the two cervical cytology smears obtained in the first year and then modifying subsequent screening based upon these results (cervical cytology screening every six months for women with detectable HPV DNA and annual screening for all others) was more beneficial and cost-effective than annual screening alone for HIV-infected women on antiretroviral therapy34. At present, there is no consensus as to whether HPV testing should be performed routinely on HIV-infected women. The only guidelines in India for cervical cancer screening in HIV-positive women are from NACO, which recommends annual Pap smear test for all HIV- positive women32. Efforts should be made to implement these guidelines in the ART centres where these patients come for regular follow up.
The limitations of our study were its cross-sectional nature, the inability to detect multiple HPV types, and inability to do colposcopy. Further, the results of our study cannot be generalized as the sample was only from eastern Uttar Pradesh.
Acknowledgment
Authors acknowledge the funding support provided by the COE, NACO (M-18017/72/2007/NACO (GF Rd 6), India, and thank Shriyut Neeraj Dwivedi and Saurabh Kumar Patel for their help in data analysis and sequence alignment, respectively. Authors also thank the staff of ART Centre and Centre of Excellence for their help and support.
Footnotes
Conflicts of Interest: None.
References
- 1.Parkin DM, Bray F. The burden of HPV-related cancers. Vaccine. 2006;24(Suppl 3):11–25. doi: 10.1016/j.vaccine.2006.05.111. [DOI] [PubMed] [Google Scholar]
- 2.Hawes SE, Critchlow CW, Faye Niang MA, Diouf MB, Diop A, Toure P, et al. Increased risk of high-grade cervical squamous intraepithelial lesions and invasive cervical cancer among African women with human immunodeficiency virus type 1 and 2 infections. J Infect Dis. 2003;188:555–63. doi: 10.1086/376996. [DOI] [PubMed] [Google Scholar]
- 3.Palefsky J. Human papillomavirus-related disease in people with HIV. Curr Opin HIV AIDS. 2009;4:52–6. doi: 10.1097/COH.0b013e32831a7246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Massad LS, Riester KA, Anastos KM, Fruchter RG, Palefsky JM, Burk RD, et al. Prevalence and predictors of squamous cell abnormalities in Papanicolaou smears from women infected with HIV-1. Women's Interagency HIV Study Group. J Acquir Immune Defic Syndr. 1999;21:33–41. doi: 10.1097/00126334-199905010-00005. [DOI] [PubMed] [Google Scholar]
- 5.Frisch M, Biggar RJ, Goedert JJ. Human papillomavirus-associated cancers in patients with human immunodeficiency virus infection and acquired immunodeficiency syndrome. J Natl Cancer Inst. 2000;92:1500–10. doi: 10.1093/jnci/92.18.1500. [DOI] [PubMed] [Google Scholar]
- 6.Joshi S, Chandorkar A, Krishnan G, Walimbe A, Gangakhedkar R, Risbud A, et al. Cervical intraepithelial changes & HIV infection in women attending sexually transmitted disease clinics in Pune, India. Indian J Med Res. 2001;113:161–9. [PubMed] [Google Scholar]
- 7.Ellerbrock TV, Chiasson MA, Bush TJ, Sun XW, Sawo D, Brudney K, et al. Incidence of cervical squamous intraepithelial lesions in HIV-infected women. JAMA. 2000;283:1031–7. doi: 10.1001/jama.283.8.1031. [DOI] [PubMed] [Google Scholar]
- 8.Coelho Lima BM, Golub JE, Tonani Mattos A, Freitas LB, Cruz Spano L, Espinosa Miranda A. Human papillomavirus in women with and without HIV-1 infection attending an STI clinic in Vitoria, Brazil. J Int Assoc Physicians AIDS Care (Chic) 2009;8:286–90. doi: 10.1177/1545109709341855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tornesello ML, Duraturo ML, Giorgi-Rossi P, Sansone M, Piccoli R, Buonaguro L, et al. Human papillomavirus (HPV) genotypes and HPV16 variants in human immunodeficiency virus-positive Italian women. J Gen Virol. 2008;89:1380–9. doi: 10.1099/vir.0.83553-0. [DOI] [PubMed] [Google Scholar]
- 10.Sahasrabuddhe VV, Bhosale RA, Joshi SN, Kavatkar AN, Nagwanshi CA, Kelkar RS, et al. Prevalence and predictors of colposcopic-histopathologically confirmed cervical intraepithelial neoplasia in HIV-infected women in India. PLoS One. 2010;5:e8634. doi: 10.1371/journal.pone.0008634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Singh DK, Anastos K, Hoover DR, Burk RD, Shi Q, Ngendahayo L, et al. Human papillomavirus infection and cervical cytology in HIV-infected and HIV-uninfected Rwandan women. J Infect Dis. 2009;199:1851–61. doi: 10.1086/599123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sahasrabuddhe VV, Mwanahamuntu MH, Vermund SH, Huh WK, Lyon MD, Stringer JS, et al. Prevalence and distribution of HPV genotypes among HIV-infected women in Zambia. Br J Cancer. 2007;96:1480–3. doi: 10.1038/sj.bjc.6603737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.New Delhi: Department of AIDS Control, National AIDS Control Organization, Ministry of Health and Family Welfare, Government of India; 2014. Annual Report 2013-14. [Google Scholar]
- 14.Bruni L, Barrionuevo-Rosas L, Albero G, Aldea M, Serrano B, Valencia S, et al. ICO Information Centre on HPV and Cancer (HPV Information Centre). Human papillomavirus and related diseases in India Summary report 2015-12-23. [accessed on January 21, 2016]. Available from: http://www.who.int/hpvcentre .
- 15.Sarkar K, Pal R, Bal B, Saha B, Bhattacharya S, Sengupta S, et al. Oncogenic HPV among HIV infected female population in West Bengal, India. BMC Infect Dis. 2011;11:72. doi: 10.1186/1471-2334-11-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aggarwal R, Sachdeva RK, Naru J, Suri V, Sharma A, Nijhawan R. HPV genotyping in north Indian women infected with HIV. Int J Gynecol Pathol. 2012;31:475–81. doi: 10.1097/PGP.0b013e31824a1d60. [DOI] [PubMed] [Google Scholar]
- 17.Joshi SN, Gopalkrishna V, Kumar BK, Dutta S, Nyaynirgune P, Thakar M, et al. Cervical squamous intra-epithelial changes and human papillomavirus infection in women infected with human immunodeficiency virus in Pune, India. J Med Virol. 2005;76:470–5. doi: 10.1002/jmv.20385. [DOI] [PubMed] [Google Scholar]
- 18.Isaakidis P, Pimple S, Varghese B, Khan S, Mansoor H, Ladomirska J, et al. HPV infection, cervical abnormalities, and cancer in HIV-infected women in Mumbai, India: 12-month follow-up. Int J Womens Health. 2013;5:487–94. doi: 10.2147/IJWH.S47710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Srivastava S, Gupta S, Roy JK. High prevalence of oncogenic HPV-16 in cervical smears of asymptomatic women of eastern Uttar Pradesh, India: a population-based study. J Biosci. 2012;37:63–72. doi: 10.1007/s12038-012-9181-y. [DOI] [PubMed] [Google Scholar]
- 20.Solomon D, Davey D, Kurman R, Moriarty A, O’Connor D, Prey M, et al. The 2001 Bethesda system: terminology for reporting results of cervical cytology. JAMA. 2002;287:2114. doi: 10.1001/jama.287.16.2114. [DOI] [PubMed] [Google Scholar]
- 21.Hwang T. Detection and typing of human papillomavirus DNA by PCR using consensus primers in various cervical lesions of Korean women. J Korean Med Sci. 1999;14:593–9. doi: 10.3346/jkms.1999.14.6.593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Munoz N, Bosch FX, de Sanjose S, Herrero R, Castellsague X, Shah KV, et al. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. 2003;348:518–27. doi: 10.1056/NEJMoa021641. [DOI] [PubMed] [Google Scholar]
- 23.Peedicayil A, Thiyagarajan K, Gnanamony M, Pulimood SA, Jeyaseelan V, Kannangai R, et al. Prevalence and risk factors for human papillomavirus and cervical intraepithelial neoplasia among HIV-positive women at a tertiary level hospital in India. J Low Genit Tract Dis. 2009;13:159–64. doi: 10.1097/LGT.0b013e31818fb40d. [DOI] [PubMed] [Google Scholar]
- 24.Mane A, Nirmalkar A, Risbud AR, Vermund SH, Mehendale SM, Sahasrabuddhe VV. HPV genotype distribution in cervical intraepithelial neoplasia among HIV-infected women in Pune, India. PLoS One. 2012;7(6):e38731. doi: 10.1371/journal.pone.0038731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Clifford GM, Goncalves MA, Franceschi S. Human papillomavirus types among women infected with HIV: a meta-analysis. AIDS. 2006;20:2337–44. doi: 10.1097/01.aids.0000253361.63578.14. [DOI] [PubMed] [Google Scholar]
- 26.Wright TC, Jr, Schiffman M. Adding a test for human papillomavirus DNA to cervical-cancer screening. N Engl J Med. 2003;348:489–90. doi: 10.1056/NEJMp020178. [DOI] [PubMed] [Google Scholar]
- 27.Zhang YX, Xiong Y, Gui XE, Chen SH, Rong YP, Cai HB. Epidemiologic risk profile of human papillomavirus infections in human immunodeficiency virus-positive Chinese women. Jpn J Infect Dis. 2011;64:411–6. [PubMed] [Google Scholar]
- 28.Rocha-Brischiliari SC, Gimenes F, de Abreu AL, Irie MM, Souza RP, Santana RG, et al. Risk factors for cervical HPV infection and genotypes distribution in HIV-infected South Brazilian women. Infect Agent Cancer. 2014;9:6. doi: 10.1186/1750-9378-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Blitz S, Baxter J, Raboud J, Walmsley S, Rachlis A, Smaill F, et al. Evaluation of HIV and highly active antiretroviral therapy on the natural history of human papillomavirus infection and cervical cytopathologic findings in HIV-positive and high-risk HIV-negative women. J Infect Dis. 2013;208:454–62. doi: 10.1093/infdis/jit181. [DOI] [PubMed] [Google Scholar]
- 30.Mangclaviraj S, Kerr SJ, Chaithongwongwatthana S, Ananworanich J, Hirschel B, Emery S, et al. Nadir CD4 count and monthly income predict cervical squamous cell abnormalities in HIV-positive women in a resource-limited setting. Int J STD AIDS. 2008;19:529–32. doi: 10.1258/ijsa.2007.007222. [DOI] [PubMed] [Google Scholar]
- 31.Massad LS, Ahdieh L, Benning L, Minkoff H, Greenblatt RM, Watts H, et al. Evolution of cervical abnormalities among women with HIV-1: evidence from surveillance cytology in the women's interagency HIV study. J Acquir Immune Defic Syndr. 2001;27:432–42. doi: 10.1097/00126334-200108150-00003. [DOI] [PubMed] [Google Scholar]
- 32.Department of AIDS control. National AIDS control Organization. Antiretroviral therapy guidelines for HIV infected Adults and Adolescents. May 2013. [December 21, 2014]. Available from: http://www.naco.gov.in/upload/Policies%20%20Guidelines/Antiretroviral%20Therapy%20Guidelines%20for%20HIV-Infected%20Adults%20and%20Adolescents.pdf .
- 33.ACOG Practice Bulletin No. 117: Gynecologic care for women with human immunodeficiency virus. ACOG Committee on Practice Bulletins-Gynecology. Obstet Gynecol. 2010;116:1492–509. doi: 10.1097/AOG.0b013e3182054cae. [DOI] [PubMed] [Google Scholar]
- 34.Goldie SJ, Freedberg KA, Weinstein MC, Wright TC, Kuntz KM. Cost effectiveness of human papillomavirus testing to augment cervical cancer screening in women infected with the human immunodeficiency virus. Am J Med. 2001;111:140–9. doi: 10.1016/s0002-9343(01)00780-x. [DOI] [PubMed] [Google Scholar]


