Abstract
Background
Positive Focused Assessment with Sonography in Trauma (FAST) and hypotension often indicates urgent surgery. An abdomen/pelvis CT (apCT) may allow less invasive management but the delay may be associated with adverse outcomes.
Methods
Patients in the Prospective Observational Multicenter Major Trauma Transfusion study with hypotension and a positive FAST (HF+) who underwent a CT (apCT+) were compared to those who did not.
Results
Of the 92 HF+ identified, 32(35%) underwent apCT during initial evaluation and apCT was associated with decreased odds of an emergency operation, OR 0.11 95% CI (0.001–0.116) and increased odds of angiographic intervention, OR 14.3 95% CI (1.5–135). There was no significant difference in 30 day mortality or need for dialysis.
Conclusion
An apCt in HF+ patients is associated with reduced odds of emergency surgery, but not mortality. Select HF+ patients can safely undergo apCT to obtain clinically useful information.
Keywords: FAST exam, Trauma, Computed Tomography Scan
Introduction
Expeditious control of hemorrhage is an imperative in high quality trauma care and is associated with improved mortality1,2. This imperative to control hemorrhage places a critical emphasis on rapid and accurate diagnosis of injuries. An optimal diagnostic algorithm for abdominal trauma, however, remains in evolution3–5.
Traditional diagnosis of intra-abdominal injuries relied upon physical exam and diagnostic peritoneal lavage (DPL), techniques hampered, respectively, by low sensitivity and low specificity6–10. Helical computed tomography (CT) has evolved to become a standard evaluation tool for the diagnostic imaging of abdominal trauma but is limited by concerns over radiation and contrast exposure as well as the logistical challenges of transporting an unstable patient to the radiology suite5,11,12. The Focused Assessment with Sonography in Trauma (FAST) exam was developed to provide a rapid, inexpensive and repeatable bedside tool to evaluate abdominal injuries. Despite concerns over a low sensitivity and operator dependence, a positive FAST exam is specific for intra-peritoneal fluid and in the setting of hemodynamic instability, has been considered an indication for an immediate laparotomy5,10,13–18. Despite this sensitivity for hemoperitoneum, FAST may not correlate well with need for an emergent operation2.
The advent of angiography and non-operative management (NOM) of select blunt intra-abdominal injuries along with an evolving understanding of the implications of a non-therapeutic trauma laparotomy has highlighted the importance of balancing speed and accuracy of diagnosis19–21. It is no longer necessary to rush every patient with hemoperitoneum to the operating room and it has been suggested that patients who can be transiently stabilized are candidates for CT evaluation22. It is unclear if this delay in definitive care is associated with adverse outcomes and if the information obtained from a CT scan alters clinical decision making.
We therefore sought to determine if patients who were initially hypotensive who undergo an abdomen and pelvis CT (CT) scan following a positive FAST exam have similar long term outcomes and less urgent operations than patients who do not undergo a CT.
Materials and Methods
Data were obtained from a database created by the Prospective Observational Multicenter Major Trauma Transfusion (PROMMTT) study Data Coordinating Center at the University of Texas Health Science Center at Houston. PROMMTT enrolled 1,245 injured patients who required the highest level activation at one of 10 Level I trauma centers and who subsequently received one or more units of red blood cells (RBCs) within 6 hours of hospital admission. Exclusion criteria included age younger than 16 years, transfer from another hospital, pregnancy, more than 20% burn injury, inhalation injury, incarceration, cardiopulmonary resuscitation lasting more than 5 minutes occurring prehospital or in the first 30 minutes after admission, and death within 30 minutes of hospital admission. Data were collected in real time on a wide variety of patient characteristics, including fluid and blood product infusions, diagnostic studies, and surgical interventions. The time of mortality or hospital discharge was recorded. Approval was obtained from the institutional review board at each center and from the US Army Human Research Protections Office23,24.
Patients who had a positive FAST along with hypotension, defined as an admission systolic blood pressure (SBP) ≤90mmHg were identified. An urgent operation was defined as direct admission to the operating room less than 3 hours from presentation. This longer time was chosen to allow for the inherent delay in obtaining a CT scan during trauma workup. Patients who went to CT were compared to those who did not. Data are presented as medians with 25th and 75th percentile. Univariable comparisons were made with Fischer’s exact test and a Mann-Whitney U test, for categorical and continuous variables, respectively.
Multivariable comparisons were made with binary logistic regression. Variables were selected for inclusion based on clinical feasibility and selected for inclusion in the multivariable model using backwards stepwise elimination to select relevant variables.
In order to control for the fact that this study did not prescribe the management of hypotensive patients with a positive FAST exam and the likely fact that patients who went to CT differed from patients who did not go to CT, we derived a propensity score to undergo CT. This was doing by constructing a binary logistic regression model with backwards stepwise elimination to select variables that were independently associated with undergoing CT. The propensity score was a conditional probability, between 0 and 1, that a patient would undergo CT based upon these variables. This allowed collection of confounding variables into a single propensity that was then used as an independent predictor in binary logistic modeling25. These propensity scores for CT and splenectomy were then used as independent variables in binary logistic models to determine independent associations with either operative or angiographic intervention. Results are presented with odds ratio (OR) and 95% confidence intervals. Statistical analysis was performed using SPSS (IBM Corporation) v22.0. Significance was set at p<0.05.
Results
We identified 255 patients with a positive FAST exam, of whom 46% subsequently went to CT, demographics of this group are presented in TABLE 1. We subsequently identified 92 patients, 7% of the total population, with admission hypotension and a positive FAST exam. In this group, 32 (35%) underwent CT during their initial trauma evaluation a median of 43 (25–51) minutes after admission to the trauma bay. Importantly, despite setting inclusion criteria for urgent operation at 3 hours, patients taken immediately to the operating room arrived there very rapidly, a median of 25 (17–36) minutes after admission. Initially hypotensive patients who underwent CT following a positive FAST exam were more likely to have a blunt injury, had a higher head Abbreviated Injury Severity (AIS) score and a higher admission platelet count than patients who did not have a CT. There were no significant differences between groups with respect to age, gender, admission hemodynamics, Glasgow Coma Score (GCS), Injury Severity Score (ISS), other AIS regions or admission hematocrit (TABLE 2A).
Table 1.
Demongraphics of patients with a positive FAST.
| Patients with a Positive FAST | |||
|---|---|---|---|
| No CT (n=138) | Yes CT (n=117) | p | |
| Age | 33(22,48) | 33(23,47) | 0.66 |
| SBP | 98(76,118) | 103(88,127) | <0.05 |
| GCS | 14(3,15) | 11(3,15) | <0.05 |
| ISS | 25(16,37) | 34(22,41) | <0.01 |
| Urgent Operation | 93% | 54% | <0.01 |
| Minutes to Operation | 25(17,36) | 88(57,151) | <0.01 |
| 30 Day Mortality | 26% | 19% | 0.18 |
CT: Abdominal/Pelvis CT scan, SBP: Systolic Blood Pressure, GCS: Glasgow Coma Scale
Table 2.
(A) Admission Data and (B) Outcomes of initiallly unstable patients with a postitive FAST exam.
| Table 2A | |||
|---|---|---|---|
| Patients with a Positive FAST and Hypotension on Admission | |||
| No CT (n=60) | Yes CT (n=32) | p | |
| Age in Years | 41(24,54) | 34(24,45) | 0.15 |
| sBP | 82% | 63% | 0.08 |
| Blunt Injury | 63% | 91% | <0.01 |
| SBP | 74(65,83) | 80(66,86) | 0.21 |
| Heart Rate | 107(88,128) | 118(88,125) | 0.62 |
| GCS | 13(3,5) | 9(4,14) | 0.15 |
| ISS | 27(16,35) | 34(23,41) | 0.12 |
| Head AIS | 0(0,0.8) | 0.5(0,4) | <0.05 |
| Face AIS | 0(0,0) | 0(0,1) | 0.05 |
| Chest AIS | 3(1,4) | 3(3,4) | 0.19 |
| Abdomen AIS | 3(2,4) | 3(3,4) | 0.8 |
| Extremity AIS | 2(0,3) | 2(0,3) | 0.82 |
| External AIS | 1(0,1) | 1(0,1) | 0.62 |
| Admission Plt Count (thousand) | 200(164–255) | 253(176–327) | <0.05 |
| Admission Hematocrit | 34(28,37) | 35(31,40) | 0.26 |
| 2B | |||
|---|---|---|---|
| Patients with a Positive FAST and Hypotension on Admission | |||
| No CT (n=60) | Yes CT (n=32) | p | |
| Urgent Operation | 93% | 22% | <0.01 |
| Urgent Angiography | 2% | 22% | <0.01 |
| Minute to Operation | 26(19–35) | 93(41,121) | <0.01 |
| 24 Hour PRBC Volume (Units) | 10(6,27) | 7(4,11) | <0.05 |
| 30 Day PRBC Volume (Units) | 8(4,23) | 5(3,1) | <0.05 |
| 24 Hour FFP Volume (Units) | 9(4,20) | 6(2,14) | <0.05 |
| 30 Day FFP Volume (Units) | 7(4,17) | 4(2,10) | <0.05 |
| 24 Hour Plt Volume (Units) | 6(6,12) | 0(0,6) | <0.05 |
| 30 Day Plt Volume (UnitS) | 6(6,12) | 0(0,6) | <0.01 |
| Length of Stay | 17(11,30) | 20(14,37) | 0.49 |
| 24 Hour Mortality | 20% | 6% | <0.01 |
| 30 Day Mortality | 30% | 19% | 0.32 |
| 30 Day Dialysis | 6% | 8% | 1 |
AIS: Abbreviated Injury Scale score, PRBC: Packed Red Blood Cells, FFP: Fresh Frozen Plasma, Plt: Platelet
On univariable comparison of outcomes, patients who underwent CT during their initial trauma evaluation were less likely to undergo an urgent operation though they were more likely to undergo an urgent angiographic intervention. Only one patient who underwent CT proceeded to the OR after 3 hours, and they were in the operating room 3.5 hours after admission. Transfusion volumes of red blood cells, plasma and platelets were lower for patients who underwent CT and while mortality at 24 hours was lower in the CT group, there was no difference in 30 day mortality. Additionally, there was no difference in length of hospital stay for patients who survived and no difference in 30 day need for dialysis (Table 2B).
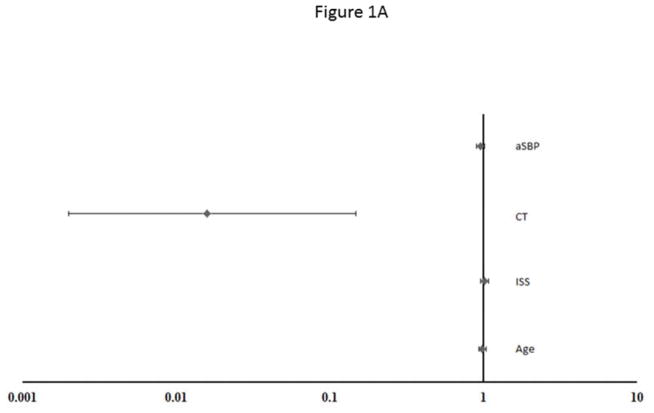
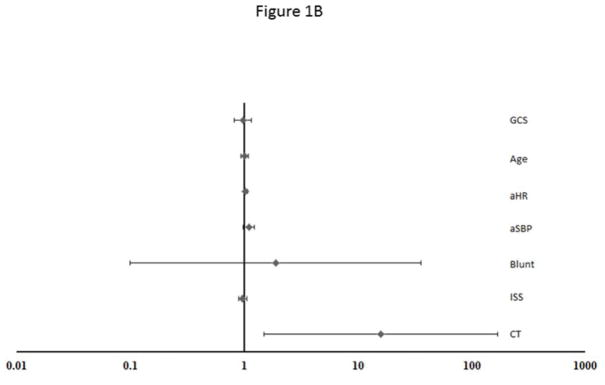
On multivariable analysis of hypotensive patients with a positive FAST, after controlling for 24 hour red blood cell and plasma transfusion volume, patient age, ISS, admission systolic blood pressure and incidence of urgent operation, there was no independent association between CT and 24 hour or 30 day mortality OR 0.41 95% CI (0.05–3.6) and 1.4 95% CI (0.24–7.7) respectively. In a multivariable model of initially hypotensive patients with a positive FAST exam, controlling for patient age, ISS and admission systolic blood pressure, CT was associated with reduced odds of an urgent operation, OR 0.02 95% CI (<0.01–0.15). In a similar model controlling for admission GCS, ISS, systolic blood pressure, heart rate, patient age and mechanism of injury, a CT scan was associated with increased odds of proceeding to interventional radiology, OR 15.8 95% CI (1.5–133.2). (FIGURE 1A&B)
Figure 1.
Figure 1A: Multivariable model predicting odds of proceeding to an urgent operation in initially hypotensive patients with a positive FAST. CT: abdominal pelvis CT scan, ISS: Injury Severity Score, aSBP: admission systolic blood pressure. R2 = 0.
Figure 1B: Multivariable model predicting odds of proceeding to an urgent angiographic intervention in initially hypotensive patients with a positive FAST. GCS: Glasgow Coma Score, aHR: admission hear rate, aSBP: admission systolic blood pressure, Blunt: blunt mechanism of injury, ISS: Injury Severity Score, CT: abdomen pelvis CT scan. R2 = 0.304.
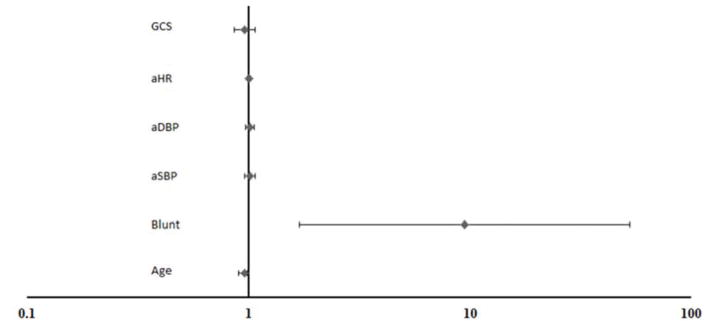
On binary logistic regression, blunt injury, OR 9.7 95% CI (1.8–51.8), and increasing age, OR 0.95 95% CI (0.92–0.99) were independently associated with propensity to undergo CT in initially hypotensive patients with a positive FAST. (FIGURE 2). Among patients with a similar propensity to undergo CT, actually undergoing a CT was associated with reduced odds of an emergency operation, OR 0.11 95% CI (<0.01–0.12) and an increased odds of proceeding to an angiographic intervention OR 14.3 95% CI (1.5–135).
Figure 2.
Multivariable model predicting propensity for initially hypotensive patients with a positive FAST exam to undergo a CT scan during initial trauma evaluation. GCS: Glasgow Coma Score, aHR: admission hear rate, aDBP: admission diastolic blood pressure, aSBP: admission systolic blood pressure, Blunt: blunt mechanism of injury. R2 = 0.185.
Discussion
Hypotensive patients with a positive FAST exam present a management dilemma for the provider. While consensus opinions suggest that this constellation of findings is an indication for an urgent operation10,18, this must be balanced against recent findings suggesting that FAST may not correlate well with need for an emergent operation2 and our evolving understanding of the long term morbidity of a non-therapeutic trauma laparotomy19–21. In this study, we demonstrate that initially hypotensive trauma patients with a positive FAST exam who undergo CT have a 30 day mortality that is no different than patients managed without CT. Additionally, we found that undergoing a CT during initial trauma evaluation is associated with increased odds of angiographic intervention and reduced the odds of an urgent operation.
When considering this finding, it is critical to remember that given the limitations of this study design, we cannot infer causation and likely the patients taken to CT are different from patients who are not taken to CT as evidenced by their rapid transport to the operating room, the difference in their mechanism of injury and head AIS as well as by their need for blood product resuscitation. As anticipated, blunt trauma was independently associated with increasing propensity to undergo CT – suggesting that hypotensive patients with penetrating injury are taken directly to the operating room. Interestingly, while not independently associated with CT, HF+ who underwent CT had a higher head and face AIS. This suggests that hypotensive patients who suffered blunt trauma and have some degree of intracranial injury are the population most likely to go to CT following a positive FAST. In addition to these injury factors, it seems likely that some degree of management variation may be related to attending surgeon preference (and thus not captured within this data set) it is also likely that patients found to be responders or transient responders to resuscitation are the ones taken to CT26,27. This is one of the most important limitations of this data set and must be kept in mind when applying these results to clinical practice. In order to retrospectively control for this variation in patients, we stratified patients by propensity to undergo CT and found, even within groups of patients with similar propensity to undergo CT, that CT was still independently associated with increased odds of an angiographic intervention and reduced odds of an urgent operation. This finding suggests that the clinical information obtained from CT is altering management decisions and diverting some bluntly injured patients away from operative intervention and to angiography or non-operative management.
Non-operative management of select intra-abdominal solid organ injuries is well established in the trauma literature. The angiographic management of selected injuries is gaining traction28–30. While delays in definitive hemorrhage control have been associated with higher mortality in trauma patients, it may be that the additional anatomic information obtained from CT allows for selection of patients that are appropriate for non-operative management or angiographic intervention2,31. The findings of this study suggest that an CT in select patients may allow for treatment of appropriate injuries in the angiography suite. This study demonstrates that the time delay inherent in obtaining an CT, at least in some patients, does not result in increased mortality and thus may be a safe decision that yields important information.
These findings must be interpreted carefully as this study is limited by the inclusion criteria of PROMMTT. The database contains only patients who received at least one unit of red blood cells and therefore our findings may not be applicable to all trauma patients. It seems likely, however, that the majority of initially hypotensive trauma patients with a positive FAST exam will receive at least one unit of blood. We are additionally limited by significant missing data in the nature of the operative intervention. While it seems likely that patients with a positive FAST and hypotension on admission who proceed urgently to the operating room are undergoing a thoraco-abdominal operation, this cannot definitely be shown in this data set. In addition, many of the factors that may contribute to variations in trauma bay decision making are not captured in the original PROMMTT database. While propensity score matching attempts to control for this variation in decision making and we hypothesize responders or transient responders are primarily taken to CT, proving this will require additional studies. There is also significant variation in FAST ordering criteria between centers despite its acceptance as a standard diagnostic imaging test and this may introduce variation in patients included within the initially hypotensive, positive FAST cohort32,33. Our relatively small numbers as well as the limited data on the specific nature of injuries limited our ability to directly test the hypothesis that patients with injuries not amenable to angiographic intervention might be disproportionately harmed by the delay necessary to obtain a CT, as compared to patients with injuries amenable to angiographic intervention.
We additionally defined initially hypotensive patients as those patients with an admission SBP of ≤90mmHg. We did not limit to patients with tachycardia or base deficit abnormalities in order to simulate the clinical situation of an initially hypotensive patient with a positive FAST and admission hypotension in which the trauma surgeon is deciding between immediate operations or further imaging prior to the availability of additional laboratory values.
Conclusion
In conclusion, we find that some patients with initial hypotension and a positive FAST may be taken to CT without a significant difference in 30 day mortality. We additionally find that undergoing an CT is independently associated with reduced odds of an urgent operation and increased odds of angiographic intervention. This suggests that the information obtained from the CT may impact clinical decisions and that admission hypotension and a positive FAST exam does not mandate laparotomy.
PRospective Observational Multicenter Major Trauma Transfusion (PROMMTT) Study Group
University of Texas Health Science Center at Houston, Houston, TX: Data Coordinating Center: Mohammad H. Rahbar, PhD (principal investigator); John B. Holcomb, MD (co-investigator); Erin E. Fox, PhD (co-investigator and project coordinator); Deborah J. del Junco, PhD (co-investigator); Bryan A. Cotton, MD, MPH (co-investigator); Charles E. Wade, PhD (co-investigator); Jiajie Zhang, PhD (co-investigator); Nena Matijevic, PhD (co-investigator); Yu Bai, MD, PhD (co-investigator); Weiwei Wang, PhD (co-investigator); Jeanette Podbielski, RN (study coordinator); Sarah J. Duran, MSCIS (data manager); Ruby Benjamin-Garner, PhD (data manager); Robert J. Reynolds, MPH (data manager); Xuan Zhang, MS (data analyst); Aisha Dickerson, MSPH (graduate assistant); Elizabeth S. Camp, MSPH (data analyst). Clinical Site: John B. Holcomb, MD (co-principal investigator); Bryan A. Cotton, MD, MPH (co-principal investigator); Marily Elopre, RN (study coordinator); Quinton M. Hatch, MD (research associate); Michelle Scerbo (research associate); Zerremi Caga-Anan, MD (research associate).
Other Clinical Sites
Brooke Army Medical Center, San Antonio, TX: Christopher E. White, MD (principal investigator); Kimberly L. Franzen, MD (co-investigator); Elsa C. Coates, MS, RN (study coordinator). Medical College of Wisconsin, Milwaukee, WI: Karen J. Brasel, MD, MPH (principal investigator); Pamela Walsh (study coordinator).
Oregon Health and Sciences University, Portland, OR: Martin A. Schreiber, MD (principal investigator); Samantha J. Underwood, MS (study coordinator); Jodie Curren (study coordinator).
University of California, San Francisco, San Francisco, CA: Mitchell J. Cohen, MD (principal investigator); M. Margaret Knudson, MD (co-investigator); Mary Nelson, RN, MPA (study coordinator); Mariah S. Call, BS (study coordinator).
University of Cincinnati, Cincinnati, OH: Peter Muskat, MD (principal investigator); Jay A. Johannigman, MD (co-investigator); Bryce RH Robinson, MD (co-investigator); Richard Branson (co-investigator); Dina Gomaa, BS, RRT (study coordinator); Cendi Dahl (study coordinator).
University of Pittsburgh Medical Center, Pittsburgh, PA: Louis H. Alarcon, MD (principal investigator); Andrew B. Peitzman, MD (co-investigator); Stacy D. Stull, MS, CCRC (study coordinator); Mitch Kampmeyer MPAS, CCRC, PA-C, (study coordinator); Barbara J. Early, RN, BSN, CCRC (study coordinator); Helen L. Shnol, BS, CRC (study coordinator); Samuel J. Zolin, BS (research associate); Sarah B. Sears, BS (research associate).
University of Texas Health Science Center at San Antonio, San Antonio, TX: John G. Myers, MD (co-principal investigator); Ronald M. Stewart, MD (co-principal investigator); Rick L. Sambucini, RN, BS (study coordinator); Marianne Gildea, RN, BSN, MS (study coordinator); Mark DeRosa CRT (study coordinator); Rachelle Jonas, RN, BSN (study coordinator); Janet McCarthy, RN (study coordinator).
University of Texas Southwestern Medical Center, Dallas, TX: Herbert A. Phelan, MD, MSCS (principal investigator); Joseph P. Minei, MD (co-investigator); Elizabeth Carroll, MD (study coordinator).
University of Washington, Seattle, WA: Eileen M. Bulger, MD (principal investigator); Patricia Klotz, RN (study coordinator); Keir J. Warner, BS (research coordinator).
Footnotes
The views and opinions expressed in this article are those of the authors and do not reflect the official policy or position of the Army Medical Department, Department of the Army, the Department of Defense, or the US Government.
This work was presented at the 2014 meeting of the North Pacific Surgical Association.
Disclosures:
This project was funded by the U.S. Army Medical Research and Materiel Command subcontract W81XWH-08-C-0712. Infrastructure for the Data Coordinating Center was supported by CTSA funds from NIH grant UL1 RR024148. All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. J.B.H. reported serving on the board for Tenaxis, the Regional Advisory Council for Trauma, and the National Trauma Institute; providing expert testimony for the Department of Justice; grants funded by the Haemonetics Corporation, and KCI USA, Inc. and consultant fees from the Winkenwerder Company. C.E.W. reported serving on the Science Board for Resuscitation Products, Inc. and the Advisory Board for Astrazeneca.
No other disclosures were reported.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Mackenzie R. Cook, Oregon Health & Science University, Portland, Oregon.
John B. Holcomb, University of Texas Health Science Center at Houston, Houston, Texas.
Mohammad H. Rahbar, University of Texas Health Science Center at Houston, Houston, Texas.
Louis H. Alarcon, University of Pittsburgh, Pittsburgh, Pennsylvania.
Eileen M. Bulger, University of Washington, Seattle, Washington.
Karen J. Brasel, Oregon Health & Science Univeristy, Portland, Oregon.
Martin A. Schreiber, Oregon Health & Science University, Portland, Oregon.
References
- 1.MacLeod JB, Lynn M, McKenney MG, Cohn SM, Murtha M. Early coagulopathy predicts mortality in trauma. Journal of Trauma-Injury Infection & Critical Care. 2003;55(1):39–44. doi: 10.1097/01.TA.0000075338.21177.EF. [DOI] [PubMed] [Google Scholar]
- 2.Barbosa RR, Rowell SE, Fox EE, et al. Increasing time to operation is associated with decreased survival in patients with a positive FAST examination requiring emergent laparotomy. J Trauma Acute Care Surg. 2013;75(1 Suppl 1):S48–52. doi: 10.1097/TA.0b013e31828fa54e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stengel D, Bauwens K, Sehouli J, et al. Systematic review and meta-analysis of emergency ultrasonography for blunt abdominal trauma. Br J Surg. 2001;88(7):901–912. doi: 10.1046/j.0007-1323.2001.01777.x. [DOI] [PubMed] [Google Scholar]
- 4.Bardenheuer M, Obertacke U, Waydhas C, Nast-Kolb D. Epidemiology of the severely injured patient. A prospective assessment of preclinical and clinical management. AG polytrauma of DGU. Unfallchirurg. 2000;103(5):355–363. doi: 10.1007/s001130050550. [DOI] [PubMed] [Google Scholar]
- 5.Stengel D, Bauwens K, Rademacher G, Ekkernkamp A, Guthoff C. Emergency ultrasound-based algorithms for diagnosing blunt abdominal trauma. Cochrane Database Syst Rev. 2013;7:CD004446. doi: 10.1002/14651858.CD004446.pub3. [DOI] [PubMed] [Google Scholar]
- 6.Prall JA, Nichols JS, Brennan R, Moore EE. Early definitive abdominal evaluation in the triage of unconscious normotensive blunt trauma patients. J Trauma. 1994;37(5):792–797. doi: 10.1097/00005373-199411000-00014. [DOI] [PubMed] [Google Scholar]
- 7.Hodgson NF, Stewart TC, Girotti MJ. Autopsies and death certification in deaths due to blunt trauma: What are we missing? Can J Surg. 2000;43(2):130–136. [PMC free article] [PubMed] [Google Scholar]
- 8.Amoroso TA. Evaluation of the patient with blunt abdominal trauma: An evidence based approach. Emerg Med Clin North Am. 1999;17(1):63–75. viii. doi: 10.1016/s0733-8627(05)70047-x. [DOI] [PubMed] [Google Scholar]
- 9.Hodgson NF, Stewart TC, Girotti MJ. Open or closed diagnostic peritoneal lavage for abdominal trauma? A meta-analysis. J Trauma. 2000;48(6):1091–1095. doi: 10.1097/00005373-200006000-00015. [DOI] [PubMed] [Google Scholar]
- 10.Hoff WS, Holevar M, Nagy KK, et al. Practice management guidelines for the evaluation of blunt abdominal trauma: The east practice management guidelines work group. J Trauma. 2002;53(3):602–615. doi: 10.1097/00005373-200209000-00038. [DOI] [PubMed] [Google Scholar]
- 11.Linsenmaier U, Krotz M, Hauser H, et al. Whole-body computed tomography in polytrauma: Techniques and management. Eur Radiol. 2002;12(7):1728–1740. doi: 10.1007/s00330-001-1225-x. [DOI] [PubMed] [Google Scholar]
- 12.Livingston DH, Lavery RF, Passannante MR, et al. Admission or observation is not necessary after a negative abdominal computed tomographic scan in patients with suspected blunt abdominal trauma: Results of a prospective, multi-institutional trial. J Trauma. 1998;44(2):273–80. doi: 10.1097/00005373-199802000-00005. discussion 280–2. [DOI] [PubMed] [Google Scholar]
- 13.Baka AG, Delgado CA, Simon HK. Current use and perceived utility of ultrasound for evaluation of pediatric compared with adult trauma patients. Pediatr Emerg Care. 2002;18(3):163–167. doi: 10.1097/00006565-200206000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Boulanger BR, Kearney PA, Brenneman FD, Tsuei B, Ochoa J. Utilization of FAST (focused assessment with sonography for trauma) in 1999: Results of a survey of north american trauma centers. Am Surg. 2000;66(11):1049–1055. [PubMed] [Google Scholar]
- 15.Scalea TM, Rodriguez A, Chiu WC, et al. Focused assessment with sonography for trauma (FAST): Results from an international consensus conference. J Trauma. 1999;46(3):466–472. doi: 10.1097/00005373-199903000-00022. [DOI] [PubMed] [Google Scholar]
- 16.Yoshii H, Sato M, Yamamoto S, et al. Usefulness and limitations of ultrasonography in the initial evaluation of blunt abdominal trauma. J Trauma. 1998;45(1):45–50. doi: 10.1097/00005373-199807000-00009. discussion 50–1. [DOI] [PubMed] [Google Scholar]
- 17.Miller MT, Pasquale MD, Bromberg WJ, Wasser TE, Cox J. Not so FAST. J Trauma. 2003;54(1):52–9. doi: 10.1097/00005373-200301000-00007. discussion 59–60. [DOI] [PubMed] [Google Scholar]
- 18.Olthof DC, van der Vlies CH, Joosse P, et al. Consensus strategies for the nonoperative management of patients with blunt splenic injury: A delphi study. J Trauma Acute Care Surg. 2013;74(6):1567–1574. doi: 10.1097/TA.0b013e3182921627. [DOI] [PubMed] [Google Scholar]
- 19.Renz BMFD. Unnecessary laparotomies for trauma: A prospective study of morbidity. J Trauma. 1995;38:350–356. doi: 10.1097/00005373-199503000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Morrison JE, Wisner DH, Bodai BI. Complications after negative laparotomy for trauma: Long-term follow-up in a health maintenance organization. J Trauma. 1996;41:509–513. doi: 10.1097/00005373-199609000-00021. [DOI] [PubMed] [Google Scholar]
- 21.Ross SE, Dragon M, O’Malley KF, et al. Morbidity of negative coeliotomy in trauma. Injury. 1995;26:393–394. doi: 10.1016/0020-1383(95)00058-h. [DOI] [PubMed] [Google Scholar]
- 22.Wallis A, Kelly MD, Jones L. Angiography and embolisation for solid abdominal organ injury in adults - a current perspective. World J Emerg Surg. 2010;5:18-7922-5-18. doi: 10.1186/1749-7922-5-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rahbar MH, Fox EE, del Junco DJ, et al. Coordination and management of multicenter clinical studies in trauma: Experience from the PRospective observational multicenter major trauma transfusion (PROMMTT) study. Resuscitation. 2012;83(4):459–464. doi: 10.1016/j.resuscitation.2011.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Holcomb JB, del Junco DJ, Fox EE, et al. The prospective, observational, multicenter, major trauma transfusion (PROMMTT) study: Comparative effectiveness of a time-varying treatment with competing risks. JAMA Surg. 2013;148(2):127–136. doi: 10.1001/2013.jamasurg.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Newgard CD, Hedges JR, Arthur M, Mullins RJ. Advanced statistics: The propensity score--a method for estimating treatment effect in observational research. Acad Emerg Med. 2004;11(9):953–961. doi: 10.1197/j.aem.2004.02.530. [DOI] [PubMed] [Google Scholar]
- 26.American College of Surgeons. ATLS: Advanced trauma life support for doctors (student course manual) 9 2012. [Google Scholar]
- 27.ATLS: Advanced trauma life support for doctors (student course manual) 8. American College of Surgeons; 2008. [Google Scholar]
- 28.Dasgupta N, Matsumoto AH, Arslan B, Turba UC, Sabri S, Angle JF. Embolization therapy for traumatic splenic lacerations. Cardiovasc Intervent Radiol. 2012;35(4):795–806. doi: 10.1007/s00270-011-0186-y. [DOI] [PubMed] [Google Scholar]
- 29.Bhullar IS, Frykberg ER, Siragusa D, et al. Selective angiographic embolization of blunt splenic traumatic injuries in adults decreases failure rate of nonoperative management. J Trauma Acute Care Surg. 2012;72(5):1127–1134. doi: 10.1097/TA.0b013e3182569849. [DOI] [PubMed] [Google Scholar]
- 30.van der Wilden GM, Velmahos GC, Emhoff T, et al. Successful nonoperative management of the most severe blunt liver injuries: A multicenter study of the research consortium of new england centers for trauma. Arch Surg. 2012;147(5):423–428. doi: 10.1001/archsurg.2012.147. [DOI] [PubMed] [Google Scholar]
- 31.Crookes BA, Shackford SR, Gratton J, Khaleel M, Ratliff J, Osler T. “Never be wrong”: The morbidity of negative and delayed laparotomies after blunt trauma. J Trauma. 2010;69(6):1386–91. doi: 10.1097/TA.0b013e3181fd6977. discussion 1391–2. [DOI] [PubMed] [Google Scholar]
- 32.Fuchs PA, del Junco DJ, Fox EE, et al. Purposeful variable selection and stratification to impute missing focused assessment with sonography for trauma data in trauma research. J Trauma Acute Care Surg. 2013;75(1 Suppl 1):S75–81. doi: 10.1097/TA.0b013e31828fa51c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Galvan DA, Matsushima K, Frankel HL. Ultrasound in the surgical intensive care unit. Isr Med Assoc J. 2011;13(9):566–570. [PubMed] [Google Scholar]