Abstract
Background and objectives
Masked hypertension and elevated nighttime BP are associated with increased risk of hypertensive target organ damage and adverse cardiovascular and renal outcomes in patients with normal kidney function. The significance of masked hypertension for these risks in patients with CKD is less well defined. The objective of this study was to evaluate the association between masked hypertension and kidney function and markers of cardiovascular target organ damage, and to determine whether this relationship was consistent among those with and without elevated nighttime BP.
Design, setting, participants, & measurements
This was a cross-sectional study. We performed 24-hour ambulatory BP in 1492 men and women with CKD enrolled in the Chronic Renal Insufficiency Cohort Study. We categorized participants into controlled BP, white-coat, masked, and sustained hypertension on the basis of clinic and 24-hour ambulatory BP. We obtained echocardiograms and measured pulse wave velocity in 1278 and 1394 participants, respectively.
Results
The percentages of participants with controlled BP, white-coat, masked, and sustained hypertension were 49.3%, 4.1%, 27.8%, and 18.8%, respectively. Compared with controlled BP, masked hypertension independently associated with low eGFR (−3.2 ml/min per 1.73 m2; 95% confidence interval, −5.5 to −0.9), higher proteinuria (+0.9 unit higher in log2 urine protein; 95% confidence interval, 0.7 to 1.1), and higher left ventricular mass index (+2.52 g/m2.7; 95% confidence interval, 0.9 to 4.1), and pulse wave velocity (+0.92 m/s; 95% confidence interval, 0.5 to 1.3). Participants with masked hypertension had lower eGFR only in the presence of elevated nighttime BP (−3.6 ml/min per 1.73 m2; 95% confidence interval, −6.1 to −1.1; versus −1.4 ml/min per 1.73 m2; 95% confidence interval, −6.9 to 4.0, among those with nighttime BP <120/70 mmHg; P value for interaction with nighttime systolic BP 0.002).
Conclusions
Masked hypertension is common in patients with CKD and associated with lower eGFR, proteinuria, and cardiovascular target organ damage. In patients with CKD, ambulatory BP characterizes the relationship between BP and target organ damage better than BP measured in the clinic alone.
Keywords: chronic kidney disease, cardiovascular disease, left ventricular hypertrophy, ambulatory blood pressure monitoring, pulse wave analysis, nighttime, blood pressure, humans, hypertension, masked hypertension
Introduction
Measurement of BP in the clinic is the most common setting to evaluate hypertension in clinical practice and in research studies. However, ambulatory BP monitoring (ABPM) may offer additional prognostic value for patients with hypertension (1). In addition, ABPM provides an assessment of nighttime BP and diurnal variation in BP.
Among persons whose kidney function is considered normal, masked hypertension—which is defined by normal clinic BP and elevated ambulatory BP (ABP)—is associated with increased risk for target organ damage and cardiovascular events (2–6). In contrast, patients with elevated clinic but normal ABP, known as white-coat hypertension, are at similar risk for cardiovascular outcomes as persons whose BP is controlled on the basis of both clinic and ABP (7). A better estimate of the burden of hypertension and improved risk stratification from out-of-office BP measurements is well recognized in the general population; consequently, ABPM is being advanced as an integral part of the evaluation of hypertension, including a recent analysis by the US Preventive Services Task Force (7,8). Less is known about masked and white-coat hypertension in patients with CKD because the majority of studies evaluating ABP have been conducted in the general population. Small studies in participants with CKD have reported that masked and sustained hypertension are associated with increased rates of left ventricular hypertrophy (LVH), proteinuria, and cardiovascular and renal events (9–11).
Nighttime BP and diurnal variation in BP are also important factors associated with hypertensive target organ damage. Cross-sectional analyses in patients with normal renal function show that elevated nighttime BP is associated with both greater pulse wave velocity (PWV) and LVH (3,12,13). A few small studies of patients with CKD have shown that both decreased eGFR and proteinuria are associated with elevated nighttime BP (14–16). The mechanism by which CKD leads to elevated nighttime BP is not well understood but is likely multifactorial, and includes volume-dependent hypertension exacerbated by recumbent posture, abnormal sodium handling, and comorbidities such as diabetes and autonomic insufficiency. Additionally, whether nighttime BP modifies the relationship between masked hypertension and adverse renal and cardiovascular outcomes is unknown.
ABPM was performed in a subset of the participants of the Chronic Renal Insufficiency Cohort (CRIC) Study, a prospective study of men and women with CKD. This afforded the opportunity to (1) evaluate the cross-sectional association between white-coat, masked, and sustained hypertension and renal function (eGFR and proteinuria), and subclinical measures of cardiovascular damage (left ventricular mass index [LVMI] and PWV); (2) characterize the clinical and demographic characteristics associated with nighttime systolic BP; and (3) evaluate whether the relationship between masked hypertension and renal and cardiovascular target organ damage is modified by the presence of elevated nighttime BP.
Materials and Methods
The CRIC Study is an ongoing multicenter observational cohort study that enrolled 3939 participants aged 21–74 years with an eGFR between 20 and 70 ml/min per 1.73 m2. The study design and baseline characteristics of participants have been described previously (17,18). The study protocol was approved by the institutional review board of each participating site; written informed consent was obtained from all participants. The following information and measures were obtained at study entry (baseline) and annually: demographic characteristics, medical history, medication use, height, weight, electrocardiogram, and serum and urine for laboratory assessments. An estimating equation developed from CRIC Study data was used to calculate eGFR (19).
Clinic and ABP Measurements
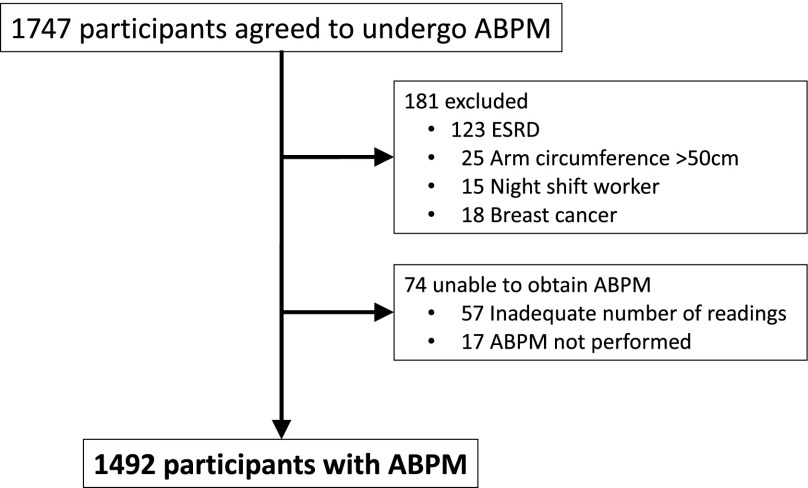
BP was measured three times during a clinic visit by trained study staff after a 5-minute rest period, following guideline-recommended protocols using aneroid sphygmomanometers with appropriately sized cuffs; the average of these measurements was used to define clinic BP (20). ABP was obtained in 1492 out of 1747 CRIC participants who agreed to undergo ABPM (Figure 1, Supplemental Table 1). Participants with any of the following were not eligible for ABPM: arm circumference greater than 50 cm, night-shift workers, breast cancer requiring mastectomy or radiation, and ESRD. ABPM was conducted between 2008 and 2012 with a SpaceLabs 90207 or 90217 ABP monitor. ABPM was conducted during the second phase of CRIC; the average time from the CRIC baseline visit to ABPM was 5.1 years. For the purposes of this manuscript, baseline was defined as the measurements and visit closest to the measurement of ABP.
Figure 1.
A totalof 255 Chronic Renal Insufficiency Cohort participants were excluded from ambulatory BP monitoring (ABPM).
The ABP protocol was designed on the basis of the recommendations of the British Hypertension Society (21,22). The ABPM cuff was placed on the nondominant arm unless an arteriovenous graft or fistula was present, in which case, the dominant arm was used. The monitor recorded BP every 30 minutes throughout the day and night; readings were not displayed to the participants. A recording was considered valid if there were at least 14 readings between 06:00 a.m. and midnight and at least six readings between midnight and 06:00 a.m. Participants were asked to undergo repeat ABPM if the minimum number of readings was not obtained. Nighttime ABP was defined by the average of readings between midnight and 06:00 a.m. Dipping status was defined by the night/day systolic BP ratio: extreme dippers (<0.8), dippers (≥0.8 and ≤0.9), nondippers (>0.9 and ≤1), and reverse dippers (>1). Participants were categorized as follows:
• Controlled BP: clinic BP <140/90 mmHg and 24-hour ABP <130/80 mmHg
• White-coat hypertension: clinic BP ≥140/90 mmHg and 24-hour ABP <130/80 mmHg
• Masked hypertension: clinic BP <140/90 mmHg and 24-hour ABP ≥130/80 mmHg
• Sustained hypertension: clinic BP ≥140/90 mmHg and 24-hour ABP ≥130/80 mmHg.
Study Outcomes—Target Organ Damage
Echocardiograms were obtained in CRIC participants at the year-1 and year-4 study visits and at the time of progression to advanced CKD and/or ESRD. The protocol for obtaining echocardiograms has been described previously (23,24). LVMI was calculated on the basis of the area-length formula and indexed to height2.7 (25). The measurement of LVMI closest to ABPM was selected for these analyses. Aortic PWV was measured in CRIC participants at the year-2 follow-up visit and then every other year thereafter. The protocol for measuring PWV has been described previously (26). For the purposes of these analyses, PWV measurements were selected on the basis of the following priority: (1) within 30 days of the ABPM, (2) next PWV measurement after ABPM, and (3) most recent PWV measurement before ABPM.
Statistical Analyses
For measurements unavailable at the time of ABPM, such as those only measured at the time of enrollment into the observational cohort or missing at the visit concurrent with ABPM, the most recent values were used. Baseline characteristics are reported by BP categories as mean and SD or median and interquartile range (IQR) for continuous variables, and frequency and percentage for categorical variables. ANOVA, Kruskal–Wallis rank sum test, and Pearson chi-squared test were used to evaluate differences between BP categories.
Separate linear regression models were used to investigate the cross-sectional association between white-coat, masked, and sustained hypertension and eGFR, proteinuria, LVMI, and PWV. Multivariable models were adjusted for age, sex, race, clinical center, tobacco use, antihypertensive medications, coronary artery disease, congestive heart failure, diabetes, body mass index, eGFR, urine protein, LDL cholesterol, serum phosphorus, serum calcium, serum uric acid, C-reactive protein, and 24-hour urine sodium. Nonlinearity was assessed using restricted cubic splines. An interaction term was used to assess whether the relationship between BP category and LVMI and PWV was modified by nighttime BP. Finally, linear regression models were used to evaluate the relationship between renal function (eGFR and proteinuria) and nighttime BP. Multivariable models were sequentially adjusted for age, sex, race, clinical center, and clinical characteristics. Careful attention was given to model assumptions by examining residual versus fitted plots, normal Q-Q plots of standardized residuals, scale-location plots, and plots of standardized residuals versus leverage.
Results
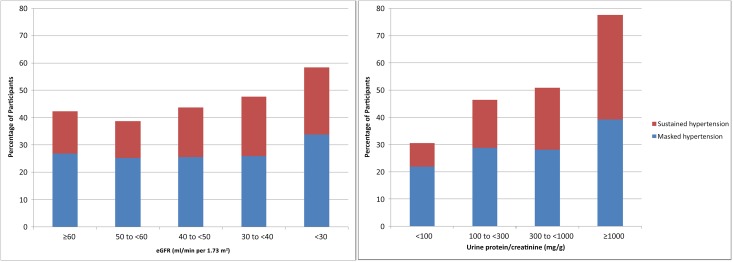
Analyzable ABP measurements were obtained in 1492 CRIC participants (Figure 1). Baseline characteristics for participants who underwent ABPM by BP category are shown in Table 1. The mean age of the study population was 63.1 years, 55.8% were male, and 38.9% were non-Hispanic black. The percentage of participants with controlled BP was 49.3%, white-coat hypertension 4.1%, masked hypertension 27.8%, and sustained hypertension 18.8%. Reverse dippers and nondippers accounted for 54.8% of participants. A total of 91.8% of participants were taking at least one antihypertensive medication. There were several differences in clinical and biochemical profiles of participants with white-coat, masked, and sustained hypertension (Table 1). Median urine protein/creatinine ratio was lowest among patients with controlled BP and highest among those with uncontrolled hypertension. Mean eGFR was lowest in the sustained hypertension group and highest in the controlled BP group. At lower eGFR and higher levels of proteinuria, there was a greater proportion of participants with masked and sustained hypertension (Figure 2).
Table 1.
Baseline characteristics by BP category
| Variable | All Participants (N=1492) | Controlled Clinic and ABP (n=735), 49.3% | White-Coat Hypertension (n=61), 4.1% | Masked Hypertension (n=415), 27.8% | Sustained Hypertension (n=281), 18.8% | P Value |
|---|---|---|---|---|---|---|
| Clinic BP definition | <140/90 | ≥140/90 | <140/90 | ≥140/90 | ||
| 24-h ABP definition | <130/80 | <130/80 | ≥130/80 | ≥130/80 | ||
| Age, yr | 63.1 (10.3) | 62.5 (10.8) | 66.1 (8.8) | 62.6 (10.1) | 64.7 (9.1) | 0.002 |
| Sex, n (%) male | 833 (55.8) | 392 (53.3) | 23 (37.7) | 262 (63.1) | 156 (55.5) | <0.001 |
| Race, n (%) | ||||||
| Non-Hispanic white | 672 (45.0) | 415 (56.5) | 21 (34.4) | 175 (42.2) | 61 (21.7) | <0.001 |
| Non-Hispanic black | 581 (38.9) | 226 (30.7) | 23 (37.7) | 181 (43.6) | 151 (53.7) | |
| Hispanic | 183 (12.3) | 73 (9.9) | 14 (23.0) | 37 (8.9) | 59 (21.0) | |
| Other | 56 (3.8) | 21 (2.9) | 3 (4.9) | 22 (5.3) | 10 (3.6) | |
| Education, n (%) | ||||||
| Less than high school | 251 (16.8) | 92 (12.5) | 13 (21.3) | 67 (16.2) | 79 (28.1) | <0.001 |
| High school graduate | 257 (17.2) | 110 (15.0) | 13 (21.3) | 71 (17.1) | 63 (22.4) | |
| Posthigh school education | 463 (31.1) | 246 (33.5) | 17 (27.9) | 129 (31.2) | 71 (25.3) | |
| ≥College graduate | 520 (34.9) | 287 (39.0) | 18 (29.5) | 147 (35.5) | 68 (24.2) | |
| Tobacco use, n (%) | ||||||
| >100 cigarettes during lifetime | 642 (43.0) | 317 (43.1) | 29 (47.5) | 183 (44.1) | 113 (40.2) | 0.02 |
| Current smoker | 130 (8.7) | 46 (6.3) | 4 (6.6) | 46 (11.1) | 34 (12.1) | |
| Exercise,a n (%) yes | 578 (69.9) | 295 (72.7) | 23 (63.9) | 155 (68.6) | 105 (66.0) | 0.33 |
| Medical history, n (%) | ||||||
| Hypertension | 1389 (93.1) | 651 (88.6) | 61 (100) | 396 (95.4) | 281 (100) | <0.001 |
| Coronary artery disease | 412 (27.6) | 193 (26.3) | 14 (23.0) | 113 (27.2) | 92 (32.7) | 0.17 |
| Chronic heart failure | 147 (9.9) | 71 (9.7) | 2 (3.3) | 45 (10.8) | 29 (10.3) | 0.32 |
| Diabetes | 626 (42.0) | 261 (35.5) | 31 (50.8) | 185 (44.6) | 149 (53.0) | <0.001 |
| Number of antihypertensive medications | 2.6 (1.5) | 2.3 (1.5) | 2.5 (1.2) | 2.8 (1.5) | 2.9 (1.4) | <0.001 |
| BP variables | ||||||
| Clinic SBP (mmHg) | 126.4 (20.4) | 114.7 (12.5) | 148.3 (12.9) | 124.7 (10.0) | 154.6 (18.8) | <0.001 |
| Clinic DBP (mmHg) | 69.3 (12.2) | 65.9 (10.1) | 76.1 (12.9) | 69.0 (10.8) | 76.9 (14.5) | <0.001 |
| 24-h SBP (mmHg) | 128.4 (15.9) | 116.7 (8.4) | 122.5 (6.4) | 137.3 (9.5) | 147.2 (13.5) | <0.001 |
| 24-h DBP (mmHg) | 72.5 (9.5) | 67.8 (6.9) | 68.2 (7.2) | 77.0 (8.3) | 78.9 (10.6) | <0.001 |
| Daytime SBP (mmHg) | 132.3 (15.6) | 121.2 (9.0) | 128.0 (7.6) | 140.3 (9.5) | 150.6 (13.5) | <0.001 |
| Daytime DBP (mmHg) | 75.7 (9.9) | 71.5 (7.7) | 72.5 (8.0) | 79.8 (9.1) | 81.6 (11.1) | <0.001 |
| Nighttime SBP (mmHg) | 121.2 (18.9) | 108.7 (11.2) | 112.9 (10.1) | 131.4 (14.0) | 140.6 (17.3) | <0.001 |
| Nighttime DBP (mmHg) | 66.7 (10.7) | 61.4 (7.6) | 60.8 (8.2) | 72.0 (9.3) | 73.9 (11.8) | <0.001 |
| Dipping status (SBP), n (%) | ||||||
| Reverse dipper (night/day >1) | 239 (16.0) | 83 (11.3) | 6 (9.8) | 91 (21.9) | 59 (21.0) | <0.001 |
| Nondipper (1≥ night/day >0.9) | 579 (38.8) | 253 (34.4) | 16 (26.2) | 181 (43.6) | 129 (45.9) | |
| Dipper (0.9≥ night/day ≥0.8) | 553 (37.1) | 323 (43.9) | 29 (47.5) | 120 (28.9) | 81 (28.8) | |
| Extreme dipper (night/day <0.8) | 121 (8.1) | 76 (10.3) | 10 (16.4) | 23 (5.5) | 12 (4.3) | |
| BMI (kg/m2) | 31.5 (7.2) | 31.3 (7.2) | 33.4 (10.6) | 31.5 (6.5) | 31.9 (7.3) | 0.10 |
| Kidney function measures | ||||||
| eGFR (ml/min per 1.73 m2) | 46.1 (20.7) | 49.2 (20.1) | 42.4 (18.0) | 43.9 (20.1) | 42.2 (22.2) | <0.001 |
| Urine protein/Cr (mg/mg) | 0.16 (0.07–0.60) | 0.10 (0.06–0.27) | 0.19 (0.10–0.41) | 0.22 (0.09–1.0) | 0.49 (0.13–1.8) | <0.001 |
| ACEI or ARB therapy, n (%) | 982 (66.0) | 500 (68.1) | 40 (66.7) | 272 (65.7) | 170 (60.5) | 0.15 |
| LDL cholesterol (mg/dl) | 102.8 (33.7) | 101.7 (33.9) | 97.7 (33.7) | 103.8 (33.6) | 105.3 (33.5) | 0.26 |
| HDL cholesterol (mg/dl) | 48.0 (15.6) | 49.5 (16.1) | 48.2 (14.2) | 46.0 (15.4) | 47.1 (14.7) | 0.002 |
| Triglycerides (mg/dl) | 148.5 (98) | 148.0 (98) | 136.0 (73) | 151.8 (110) | 147.7 (86) | 0.68 |
| Hemoglobin (g/dl) | 12.8 (1.7) | 13.0 (1.6) | 12.3 (1.9) | 12.9 (1.7) | 12.3 (1.8) | <0.001 |
| Serum calcium (mg/dl) | 9.33 (0.5) | 9.38 (0.4) | 9.37 (0.6) | 9.32 (0.5) | 9.20 (0.6) | <0.001 |
| Serum phosphorus (mg/dl) | 3.60 (0.6) | 3.56 (0.6) | 3.64 (0.6) | 3.65 (0.6) | 3.66 (0.6) | 0.03 |
| Serum albumin (g/dl) | 3.88 (0.4) | 3.96 (0.3) | 3.86 (0.3) | 3.85 (0.4) | 3.75 (0.4) | <0.001 |
| Total iPTH (pg/ml) | 46 (32–71) | 42 (31–61) | 42 (29–68) | 51 (34–79) | 54 (37–83) | <0.001 |
| FGF23 (RU/ml) | 121 (86–182) | 114 (84–172) | 114 (80–169) | 134 (89–201) | 129 (90–187) | 0.004 |
| Hemoglobin A1c (%) | 6.46 (1.4) | 6.23 (1.2) | 6.49 (1.4) | 6.58 (1.4) | 6.87 (1.6) | <0.001 |
| Serum uric acid (mg/dl) | 7.21 (1.9) | 7.06 (1.9) | 6.76 (1.7) | 7.34 (1.8) | 7.52 (1.8) | <0.001 |
| C-reactive protein (mg/L) | 2.3 (1.0–5.7) | 2.1 (0.9–5.2) | 2.2 (1.0–5.4) | 2.5 (1.0–6.4) | 2.7 (1.1–6.6) | 0.05 |
Baseline characteristics are reported by BP category as mean (SD) or continuous variables, as median (interquartile range) for skewed variables, and n (%) for categorical variables. ABP, ambulatory BP; SBP, systolic BP; DBP, diastolic BP; BMI, body mass index; Cr, creatinine; ACEI, angiotensin converting enzyme inhibitor; ARB, angiotensin receptor blocker; iPTH, intact parathyroid hormone; FGF23, fibroblast growth factor 23.
Exercise was defined as any intentional exercise. Exercise was missing for 665 out of 1492 participants.
Figure 2.
Percentage of participants with masked and sustained hypertension by eGFR and urine protein/creatinine ratio categories.
Association between BP Category and eGFR and Proteinuria
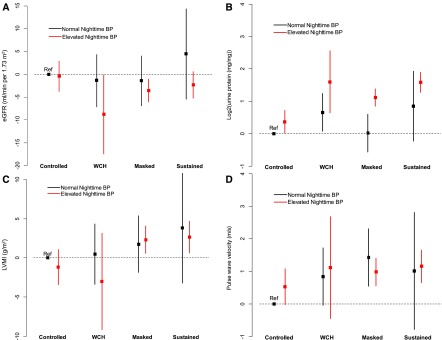
Masked and sustained hypertension were associated with low eGFR and elevated proteinuria (Table 2). In fully adjusted linear regression models, masked hypertension was associated with low eGFR (−3.2 ml/min per 1.73 m2; 95% confidence interval [95% CI], −5.5 to −0.9). To account for a non-normal distribution, urine protein was log transformed with base 2 (log2). Masked and sustained hypertension were associated with a nearly twofold higher urine protein (masked: +0.9 units higher log2 urine protein; 95% CI, 0.7 to 1.1; sustained: +1.44 units higher log2 urine protein; 95% CI, 1.1 to 1.7). The association between masked and sustained hypertension and low eGFR and elevated proteinuria was more pronounced in patients with elevated nighttime BP (P interaction =0.002 for eGFR and 0.10 for proteinuria; Figure 3, A and B).
Table 2.
Relationship between BP category and eGFR and proteinuria
| BP Category | eGFR (ml/min per 1.73 m2) | Proteinuria (log2 mg/mg) | ||
|---|---|---|---|---|
| Unadjusted (95% CI) | Adjusteda (95% CI) | Unadjusted (95% CI) | Adjusteda (95% CI) | |
| Controlled clinic and ambulatory BP | Reference | Reference | Reference | Reference |
| White-coat hypertension | −6.8 (−12.3 to −1.4)b | −3.4 (−8.3 to 1.4) | 0.82 (0.3 to 1.4)b | 0.81 (0.3 to 1.3)b |
| Masked hypertension | −5.3 (−7.9 to −2.8)b | −3.2 (−5.5 to −0.9)b | 1.11 (0.9 to 1.4)b | 0.90 (0.7 to 1.1)b |
| Sustained hypertension | −7.0 (−9.9 to −4.2)b | −1.8 (−4.6 to 0.9) | 1.85 (1.6 to 2.1)b | 1.44 (1.1 to 1.7)b |
log2, log base 2; 95% CI, 95% confidence interval.
Adjusted for age, sex, race, clinical center, tobacco use, angiotensin converting enzyme inhibitors/angiotensin receptor blockers, diuretics, beta blockers, calcium channel blockers, total number of antihypertensives, coronary artery disease, congestive heart failure, diabetes, body mass index, LDL cholesterol, serum phosphorus, serum calcium, serum uric acid, C-reactive protein, and 24-hour urine sodium.
P<0.05.
Figure 3.
Relationship between BP categories, nighttime BP, and target organ damage (eGFR, proteinuria, left ventricular mass index [LVMI], and pulse wave velocity). Squares represent point estimate (β) from linear regression models and lines represent 95% confidence interval with controlled BP with normal nighttime BP as the reference category. WCH, white-coat hypertension.
Association between BP Category and Cardiovascular Target Organ Damage
Among the 1492 CRIC participants with ABP data, LVMI was obtained in 1278 participants. The median (IQR) time between ABPM and echocardiography was 327 (0–404) days. The average (SD) LVMI-Cornell for all participants was 48.5 (13.0) g/m2.7. In fully adjusted linear regression models, both masked hypertension and sustained hypertension were associated with higher LVMI (Table 3). In participants with masked hypertension, LVMI was 2.52 g/m2.7 (95% CI, 0.9 to 4.1) higher compared with those with controlled clinic BP and ABP. There was a significant interaction between BP category and nighttime BP (P=0.05); the greater LVMI associated with masked and sustained hypertension may be limited to those with elevated nighttime BP (Figure 3C).
Table 3.
Relationship between BP category and left ventricular mass and pulse wave velocity
| BP Category | Left Ventricular Mass Index (g/m2.7) | Pulse Wave Velocity (m/s) | ||
|---|---|---|---|---|
| Unadjusted (95% CI) | Adjusteda (95% CI) | Unadjusted (95% CI) | Adjusteda (95% CI) | |
| Controlled clinic and ambulatory BP | Reference | Reference | Reference | Reference |
| White-coat hypertension | 4.24 (0.6 to 7.9)b | −0.21 (−3.5 to 3.1) | 1.36 (0.6 to 2.2)b | 0.80 (0.02 to 1.6)b |
| Masked hypertension | 4.34 (2.7 to 6.0)b | 2.52 (0.9 to 4.1)b | 1.09 (0.7 to 1.5)b | 0.92 (0.5 to 1.3)b |
| Sustained hypertension | 8.37 (6.5 to 10.2)b | 2.99 (1.1 to 4.9)b | 1.77 (1.3 to 2.2)b | 1.03 (0.6 to 1.5)b |
95% CI, 95% confidence interval.
Adjusted for age, sex, race, clinical center, tobacco use, angiotensin converting enzyme inhibitors/angiotensin receptor blockers, diuretics, beta blockers, calcium channel blockers, total number of antihypertensives, coronary artery disease, congestive heart failure, diabetes, body mass index, eGFR, urine protein, LDL cholesterol, serum phosphorus, serum calcium, serum uric acid, C-reactive protein, and 24-hour urine sodium.
P<0.05.
PWV and ABPM were obtained in 1394 participants; average (SD) PWV among these participants was 9.8 (3.1) m/s. The median (IQR) time between ABPM and PWV measurement was 343 (0–552) days. In adjusted analyses, white-coat, masked, and sustained hypertension were associated with higher PWV compared with controlled clinic BP and ABP (Table 3). The interaction between BP category and nighttime BP was not significant (P=0.14); the higher PWV associated with masked and sustained hypertension was consistent regardless of nighttime BP (Figure 3D). The association between BP control and hypertension categories and target organ damage did not differ significantly among those with measures within 6 months and those whose measures were more distal (P value for interaction 0.16 for LVMI and 0.20 for PWV; Supplemental Table 2).
Associations between Clinical and Demographic Characteristics and Nighttime BP
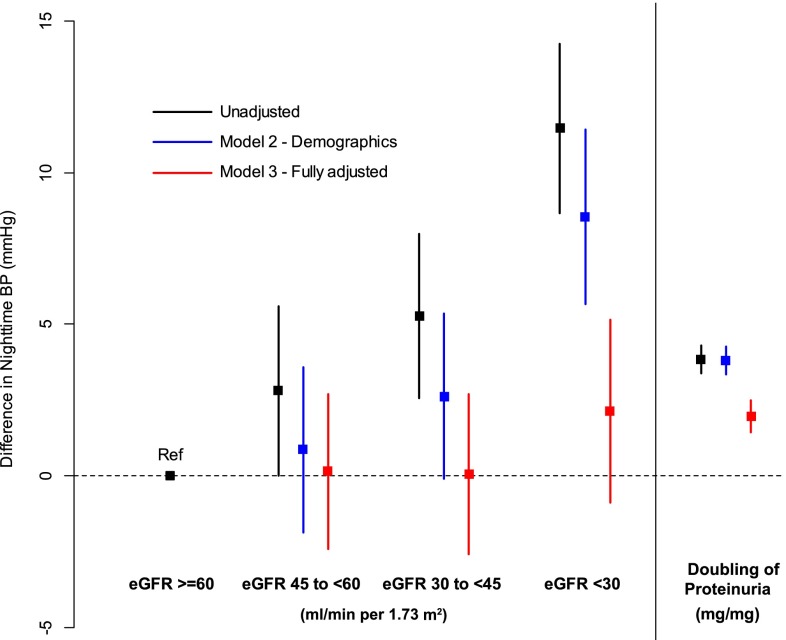
Factors independently associated with elevated nighttime BP were low eGFR, proteinuria, older age, black race, diabetes, and low HDL (Table 4). The relationship between eGFR and nighttime BP was found to be nonlinear. Although in unadjusted models mild and moderate CKD are associated with elevated nighttime BP, in fully adjusted models, nighttime BP is elevated only at an eGFR less than approximately 30 ml/min per 1.73 m2 (Figure 4, Table 4). The association between proteinuria and elevated nighttime BP was attenuated but still significant after adjustment (Figure 4).
Table 4.
Multivariable associations between clinical and demographic characteristics and nighttime systolic BP
| Variable | Difference in Nighttime BP | 95% Confidence Interval |
|---|---|---|
| Age (per 5 yr) | 1.03 | 0.51 to 1.56 |
| Sex (female versus male) | −1.09 | −3.34 to 1.15 |
| Race (versus non-Hispanic white) | ||
| Non-Hispanic black | 5.84 | 3.43 to 8.25 |
| Hispanic | 0.35 | −3.48 to 4.17 |
| Other | −0.22 | −5.15 to 4.71 |
| Education (versus college degree or higher) | ||
| Less than high school | −1.66 | −5.01 to 1.68 |
| High school graduate | 0.79 | −2.14 to 3.72 |
| Some college | −1.62 | −3.97 to 0.73 |
| Smoking status (versus nonsmoker) | ||
| Current smoker | 2.48 | −1.21 to 6.16 |
| >100 cigarettes during lifetime | −0.93 | −2.93 to 1.06 |
| Alcohol use (yes versus no) | 0.90 | −1.17 to 2.97 |
| Medical history | ||
| Hypertension | 4.17 | −0.16 to 8.50 |
| MI or coronary revascularization | 1.97 | −0.34 to 4.28 |
| Chronic heart failure | 0.08 | −3.42 to 3.57 |
| Diabetes | 3.85 | 1.72 to 5.98 |
| Clinic systolic BP (per 5 mmHg) | 1.78 | 1.52 to 2.05 |
| Body mass index (kg/m2) | −0.05 | −1.29 to 1.20 |
| Heart rate variability, SDNNa | −0.98a | −1.86 to −0.09a |
| eGFR (25 versus 30 ml/min per 1.73 m2) | 1.37 | 0.53 to 2.22 |
| Urine protein/creatininea | 2.04a | 1.43 to 2.66a |
| Medications | ||
| ACEI or ARB therapy | −6.10 | −8.75 to −3.45 |
| Diuretics | −4.27 | −6.94 to −1.59 |
| Beta-blockers | −2.89 | −5.81 to 0.03 |
| Calcium channel blockers | −0.80 | −3.37 to 1.77 |
| Number of antihypertensive medications (per one medication) | 2.91 | 1.30 to 4.53 |
| Serum calcium (mg/dl) | −0.07 | −1.14 to 1.00 |
| Serum phosphorus (mg/dl) | 0.57 | −0.82 to 1.96 |
| Total iPTH (pg/ml) | 0.76 | −0.21 to 1.73 |
| Serum uric acid (mg/dl) | −0.97 | −2.40 to 0.46 |
| C-reactive protein (mg/L) | −0.24 | −0.82 to 0.33 |
| HDL cholesterol (mg/dl) | −1.88 | −3.06 to −0.70 |
All variables were included in the model simultaneously. Increase in continuous variables from 25th to 75th percentile unless otherwise noted. MI, myocardial infarction; SDNN, standard deviation of all R-R intervals; ACEI, angiotensin converting enzyme inhibitor; ARB, angiotensin receptor blocker; iPTH, intact parathyroid hormone.
Per doubling.
Figure 4.
Relationship between eGFR and proteinuria and nighttime BP.
Discussion
The current study is the largest ABPM cohort of patients with CKD with concurrent measurement of LVMI and PWV. In this large cohort, the prevalence of masked hypertension was high, and masked hypertension was associated with low eGFR, proteinuria, and elevated LVMI and PWV. The association between masked hypertension and target organ damage may be more pronounced in patients with elevated nighttime BP. We demonstrate, for the first time in CKD patients, that masked hypertension is associated with higher PWV, a marker of vascular stiffness. Finally, a number of clinical and demographic characteristics—including lower eGFR, proteinuria, diabetes, and black race—were associated with elevated nighttime BP, and diuretics, angiotensin converting enzyme inhibitors, and angiotensin receptor blockers were associated with lower nighttime BP.
The prevalence of masked hypertension was similar in CRIC participants when compared with other cohorts of patients with CKD, such as in the African American Study of Kidney Disease and Hypertension Cohort Study and the CKD Japan Cohort, at 43% and 31% respectively (9,27–29). However, in a meta-analysis by Agarwal et al. and a cross-sectional study from Spain, masked hypertension was present in less than 10% of CKD patients (30,31). Although differences in prevalence are likely attributable to underlying interstudy variability in race, ethnicity, and renal function, these differences may also relate to the definitions and diagnostic thresholds used (e.g., daytime versus 24-hour ABPM). The high prevalence of masked hypertension in patients with CKD reinforces the need to measure out-of-office BP for a full characterization of the burden of hypertension. Among all CRIC participants, clinic BP was controlled at the initial visit in approximately 72% of participants, with a higher rate observed in those who went on to undergo ABPM (32). At the time of ABPM, clinic BP was controlled in 77% of participants. In contrast, only 49% of ABPM participants had controlled clinic BP and ABP. These discrepancies between clinic BP and ABP control rates are relevant to the interpretation and application of clinical trial evidence of effectiveness of antihypertensive medications and BP targets, which is based entirely on BP measured in the clinical setting.
Earlier studies of CKD cohorts have shown an increased risk for masked and sustained hypertension with elevated urine protein, but analyses were unadjusted or obtained from small cohorts (9,27,33). In CRIC, masked hypertension was associated with low eGFR, and masked and sustained hypertension were associated with elevated urine protein, independent of other risk factors. It is possible that ABP is affected more than clinic BP by endothelial function, for which elevated urine protein is a surrogate marker (34–36). In summary, our data indicate that patients with masked hypertension are more likely to have low eGFR and proteinuria. Therefore, further studies are needed to understand the mechanisms by which these high-risk BP profiles develop in patients with CKD, and pave the way for therapeutic strategies targeting ABP.
In patients with normal renal function, masked and sustained hypertension are well established risk factors for target organ damage, such as LVH and elevated PWV, and cardiovascular events (37–39). Among black Americans, masked hypertension was associated with proteinuria and LVH, and elevated ABP was associated with increased risk for cardiovascular events overall and renal events in those with controlled clinic BP (9,10). In a study of 217 veterans with CKD, ABP was a stronger predictor of ESRD and death than clinic BP; similarly, among 436 Italian patients with CKD, elevated ambulatory daytime and nighttime BP but not clinic BP were associated with increased risk for renal and cardiovascular events (40,41). Only one study has evaluated the risk for adverse events associated with white-coat, masked, and sustained hypertension in patients with CKD. Minutolo et al. reported that masked hypertension is associated with increased risk for cardiovascular and renal events in a cohort of 489 consecutive hypertensive patients with CKD seen in nephrology clinics in Italy (11). We found that masked and sustained hypertension increased risk for elevated LVMI. We report, for the first time to our knowledge, that this relationship is dependent, albeit marginally, on nighttime BP. This is also the first report of an association between masked hypertension and increased PWV in patients with CKD. LVMI and PWV are both more than just biomarkers of cardiovascular risk, they are direct measures of target organ damage. Both LVH and elevated PWV are associated with significantly increased risk for cardiovascular and all-cause mortality, particularly in patients with ESRD (42–44). The optimal therapeutic approach to masked hypertension remains poorly defined. It is unknown whether the increased risk for adverse outcomes associated with masked hypertension is modifiable. Our findings emphasize the need to evaluate whether traditional therapeutic strategies to treat hypertension lower the increased cardiovascular and renal risk associated with masked hypertension.
Finally, in order to better understand the epidemiology and potential mechanisms underlying elevated nighttime BP, we evaluated the clinical and demographic characteristics associated with nighttime BP. Low eGFR and proteinuria were associated with elevated nighttime BP. These results are consistent with earlier studies in cohorts of patients with CKD, and highlight the importance of ABP rather than home BP in assessing the potential effect of hypertension in patients with CKD (14–16). Additionally, use of diuretics and angiotensin converting enzyme inhibitors and/or angiotensin receptor blockers was associated with lower nighttime BP. This effect may be due to decreased sodium retention and therefore less nocturnal pressure natriuresis. However, estimation of differences between drugs is limited in observational analyses such as CRIC and may be susceptible to indication biases. Prospectively designed interventional studies comparing drugs are needed to address this important question.
A number of limitations to the current study need to be considered. The study is cross-sectional and observational in nature, which limits assessment of causality. However, CRIC participants are well characterized, which allows for adjustment for multiple potential confounders and covariates, and therefore enhances the robustness of observed associations. Although echocardiography and PWV measurements were available in most ABPM participants, they were not necessarily obtained concurrently, and the sequence of ABPM and these measures was not uniform across all participants; this further limits our ability to assess causality. We did not distinguish between masked hypertension and masked uncontrolled hypertension, although >90% of participants received antihypertensive medications (45). Additionally, the outcomes assessed in this paper, although clearly important, are still surrogates for clinical cardiovascular disease. Longitudinal follow-up of CRIC participants will determine whether masked hypertension is associated with increased risk for cardiovascular events and kidney disease progression. Finally, only one measurement of ABP was obtained; classification of patients on the basis of clinic BP and ABP may differ over time in up to 25% of patients (29,46).
In conclusion, this study demonstrates that masked hypertension is associated with low eGFR, proteinuria, and target organ damage as assessed by LVMI and PWV. Low eGFR and proteinuria are also associated with elevated nighttime BP. ABP may better characterize the relationship between BP and adverse outcomes in patients with CKD. Further studies are needed to determine whether targeting patients for treatment on the basis of ABPM results reduces the incidence of adverse clinical events.
Disclosures
None.
Supplementary Material
Acknowledgments
The study was supported in part through a Career Development Award K23DK087919 (P.E.D.) from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Funding for the CRIC Study was obtained under a cooperative agreement from the NIDDK (U01DK060990, U01DK060984, U01DK061022, U01DK061021, U01DK061028, U01DK060980, U01DK060963, and U01DK060902). In addition, this work was supported in part by: the Perelman School of Medicine at the University of Pennsylvania Clinical and Translational Science Award National Institutes of Health (NIH)/National Center for Advancing Translational Sciences (NCATS) UL1TR000003, Johns Hopkins University UL1 TR-000424, University of Maryland General Clinical Research Center M01 RR-16500, Clinical and Translational Science Collaborative of Cleveland, UL1TR000439 from the NCATS component of the NIH and NIH roadmap for Medical Research, Michigan Institute for Clinical and Health Research UL1TR000433, University of Illinois at Chicago Clinical and Translational Science Award UL1RR029879, Tulane University Translational Research in Hypertension and Renal Biology P30GM103337, Kaiser Permanente NIH/National Center for Research Resources University of California San Francisco-Clinical and Translational Science Institute UL1 RR-024131, and K01DK092353. PWV measurements were funded through NIH/NIDDK DK-067390.
This work was presented at the American Society of Nephrology Kidney Week Annual Meeting, November 7–10, 2013, in Atlanta, Georgia.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIDDK or the NIH.
The CRIC Study Investigators are Lawrence J. Appel, MD, MPH (Departments of Medicine and Epidemiology, Johns Hopkins University, Baltimore, MD); Harold I. Feldman, MD, MSCE (Department of Biostatistics and Epidemiology, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA); Alan S. Go, MD (Kaiser Permanente Northern California Division of Research, Oakland, CA); J.H.; J.W.K.; James P. Lash, MD (University of Illinois at Chicago, College of Medicine, Chicago, IL); Akinlolu Ojo, MD, PhD (Division of Nephrology, University of Michigan, Ann Arbor, MI); M.R.; and R.R.T.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.08530815/-/DCSupplemental.
References
- 1.Drawz PE, Abdalla M, Rahman M: Blood pressure measurement: clinic, home, ambulatory, and beyond. Am J Kidney Dis 60: 449–462, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu JE, Roman MJ, Pini R, Schwartz JE, Pickering TG, Devereux RB: Cardiac and arterial target organ damage in adults with elevated ambulatory and normal office blood pressure. Ann Intern Med 131: 564–572, 1999 [DOI] [PubMed] [Google Scholar]
- 3.Wijkman M, Länne T, Engvall J, Lindström T, Ostgren CJ, Nystrom FH: Masked nocturnal hypertension--a novel marker of risk in type 2 diabetes. Diabetologia 52: 1258–1264, 2009 [DOI] [PubMed] [Google Scholar]
- 4.Matsui Y, Eguchi K, Ishikawa J, Hoshide S, Shimada K, Kario K: Subclinical arterial damage in untreated masked hypertensive subjects detected by home blood pressure measurement. Am J Hypertens 20: 385–391, 2007 [DOI] [PubMed] [Google Scholar]
- 5.Bobrie G, Chatellier G, Genes N, Clerson P, Vaur L, Vaisse B, Menard J, Mallion JM: Cardiovascular prognosis of “masked hypertension” detected by blood pressure self-measurement in elderly treated hypertensive patients. JAMA 291: 1342–1349, 2004 [DOI] [PubMed] [Google Scholar]
- 6.Fagard RH, Cornelissen VA: Incidence of cardiovascular events in white-coat, masked and sustained hypertension versus true normotension: a meta-analysis. J Hypertens 25: 2193–2198, 2007 [DOI] [PubMed] [Google Scholar]
- 7.Piper MA, Evans CV, Burda BU, Margolis KL, O’Connor E, Whitlock EP: Diagnostic and predictive accuracy of blood pressure screening methods with consideration of rescreening intervals: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med 162: 192–204, 2015 [DOI] [PubMed] [Google Scholar]
- 8.Krause T, Lovibond K, Caulfield M, McCormack T, Williams B, Guideline Development Group : Management of hypertension: summary of NICE guidance. BMJ 343: d4891, 2011 [DOI] [PubMed] [Google Scholar]
- 9.Pogue V, Rahman M, Lipkowitz M, Toto R, Miller E, Faulkner M, Rostand S, Hiremath L, Sika M, Kendrick C, Hu B, Greene T, Appel L, Phillips RA, African American Study of Kidney Disease and Hypertension Collaborative Research Group : Disparate estimates of hypertension control from ambulatory and clinic blood pressure measurements in hypertensive kidney disease. Hypertension 53: 20–27, 2009 [DOI] [PubMed] [Google Scholar]
- 10.Gabbai FB, Rahman M, Hu B, Appel LJ, Charleston J, Contreras G, Faulkner ML, Hiremath L, Jamerson KA, Lea JP, Lipkowitz MS, Pogue VA, Rostand SG, Smogorzewski MJ, Wright JT, Greene T, Gassman J, Wang X, Phillips RA, African American Study of Kidney Disease and Hypertension (AASK) Study Group : Relationship between ambulatory BP and clinical outcomes in patients with hypertensive CKD. Clin J Am Soc Nephrol 7: 1770–1776, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Minutolo R, Gabbai FB, Agarwal R, Chiodini P, Borrelli S, Bellizzi V, Nappi F, Stanzione G, Conte G, De Nicola L: Assessment of achieved clinic and ambulatory blood pressure recordings and outcomes during treatment in hypertensive patients with CKD: a multicenter prospective cohort study. Am J Kidney Dis 64: 744–752, 2014 [DOI] [PubMed] [Google Scholar]
- 12.Cuspidi C, Michev I, Meani S, Severgnini B, Fusi V, Corti C, Salerno M, Valerio C, Magrini F, Zanchetti A: Reduced nocturnal fall in blood pressure, assessed by two ambulatory blood pressure monitorings and cardiac alterations in early phases of untreated essential hypertension. J Hum Hypertens 17: 245–251, 2003 [DOI] [PubMed] [Google Scholar]
- 13.Cuspidi C, Meani S, Salerno M, Valerio C, Fusi V, Severgnini B, Lonati L, Magrini F, Zanchetti A: Cardiovascular target organ damage in essential hypertensives with or without reproducible nocturnal fall in blood pressure. J Hypertens 22: 273–280, 2004 [DOI] [PubMed] [Google Scholar]
- 14.Farmer CK, Goldsmith DJ, Cox J, Dallyn P, Kingswood JC, Sharpstone P: An investigation of the effect of advancing uraemia, renal replacement therapy and renal transplantation on blood pressure diurnal variability. Nephrol Dial Transplant 12: 2301–2307, 1997 [DOI] [PubMed] [Google Scholar]
- 15.Fukuda M, Munemura M, Usami T, Nakao N, Takeuchi O, Kamiya Y, Yoshida A, Kimura G: Nocturnal blood pressure is elevated with natriuresis and proteinuria as renal function deteriorates in nephropathy. Kidney Int 65: 621–625, 2004 [DOI] [PubMed] [Google Scholar]
- 16.Paoletti E, Bellino D, Amidone M, Rolla D, Cannella G: Relationship between arterial hypertension and renal damage in chronic kidney disease: insights from ABPM. J Nephrol 19: 778–782, 2006 [PubMed] [Google Scholar]
- 17.Feldman HI, Appel LJ, Chertow GM, Cifelli D, Cizman B, Daugirdas J, Fink JC, Franklin-Becker ED, Go AS, Hamm LL, He J, Hostetter T, Hsu CY, Jamerson K, Joffe M, Kusek JW, Landis JR, Lash JP, Miller ER, Mohler ER, 3rd, Muntner P, Ojo AO, Rahman M, Townsend RR, Wright JT, Chronic Renal Insufficiency Cohort (CRIC) Study Investigators : The Chronic Renal Insufficiency Cohort (CRIC) Study: Design and Methods. J Am Soc Nephrol 14[Suppl 2]: S148–S153, 2003 [DOI] [PubMed] [Google Scholar]
- 18.Lash JP, Go AS, Appel LJ, He J, Ojo A, Rahman M, Townsend RR, Xie D, Cifelli D, Cohan J, Fink JC, Fischer MJ, Gadegbeku C, Hamm LL, Kusek JW, Landis JR, Narva A, Robinson N, Teal V, Feldman HI, Chronic Renal Insufficiency Cohort (CRIC) Study Group : Chronic Renal Insufficiency Cohort (CRIC) Study: baseline characteristics and associations with kidney function. Clin J Am Soc Nephrol 4: 1302–1311, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anderson AH, Yang W, Hsu CY, Joffe MM, Leonard MB, Xie D, Chen J, Greene T, Jaar BG, Kao P, Kusek JW, Landis JR, Lash JP, Townsend RR, Weir MR, Feldman HI, CRIC Study Investigators : Estimating GFR among participants in the Chronic Renal Insufficiency Cohort (CRIC) Study. Am J Kidney Dis 60: 250–261, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ, Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute. National High Blood Pressure Education Program Coordinating Committee : Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 42: 1206–1252, 2003 [DOI] [PubMed] [Google Scholar]
- 21.O’Brien E, Asmar R, Beilin L, Imai Y, Mallion JM, Mancia G, Mengden T, Myers M, Padfield P, Palatini P, Parati G, Pickering T, Redon J, Staessen J, Stergiou G, Verdecchia P, European Society of Hypertension Working Group on Blood Pressure Monitoring : European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens 21: 821–848, 2003 [DOI] [PubMed] [Google Scholar]
- 22.O’Brien E, Coats A, Owens P, Petrie J, Padfield PL, Littler WA, de Swiet M, Mee F: Use and interpretation of ambulatory blood pressure monitoring: recommendations of the British hypertension society. BMJ 320: 1128–1134, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bansal N, Keane M, Delafontaine P, Dries D, Foster E, Gadegbeku CA, Go AS, Hamm LL, Kusek JW, Ojo AO, Rahman M, Tao K, Wright JT, Xie D, Hsu CY, CRIC Study Investigators : A longitudinal study of left ventricular function and structure from CKD to ESRD: the CRIC study. Clin J Am Soc Nephrol 8: 355–362, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mishra RK, Li Y, DeFilippi C, Fischer MJ, Yang W, Keane M, Chen J, He J, Kallem R, Horwitz EJ, Rafey M, Raj DS, Go AS, Shlipak MG, CRIC Study Investigators : Association of cardiac troponin T with left ventricular structure and function in CKD. Am J Kidney Dis 61: 701–709, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ, Chamber Quantification Writing Group. American Society of Echocardiography’s Guidelines and Standards Committee. European Association of Echocardiography : Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 18: 1440–1463, 2005 [DOI] [PubMed] [Google Scholar]
- 26.Townsend RR, Wimmer NJ, Chirinos JA, Parsa A, Weir M, Perumal K, Lash JP, Chen J, Steigerwalt SP, Flack J, Go AS, Rafey M, Rahman M, Sheridan A, Gadegbeku CA, Robinson NA, Joffe M: Aortic PWV in chronic kidney disease: a CRIC ancillary study. Am J Hypertens 23: 282–289, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Iimuro S, Imai E, Watanabe T, Nitta K, Akizawa T, Matsuo S, Makino H, Ohashi Y, Hishida A, Chronic Kidney Disease Japan Cohort Study Group : Clinical correlates of ambulatory BP monitoring among patients with CKD. Clin J Am Soc Nephrol 8: 721–730, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang C, Gong WY, Zhang J, Peng H, Tang H, Liu X, Ye ZC, Lou T: Disparate assessment of clinic blood pressure and ambulatory blood pressure in differently aged patients with chronic kidney disease. Int J Cardiol 183: 54–62, 2015 [DOI] [PubMed] [Google Scholar]
- 29.Agarwal R, Pappas MK, Sinha AD: Masked Uncontrolled Hypertension in CKD [published online ahead of print July 10, 2015]. J Am Soc Nephrol 10.1681/ASN.2015030243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bangash F, Agarwal R: Masked hypertension and white-coat hypertension in chronic kidney disease: a meta-analysis. Clin J Am Soc Nephrol 4: 656–664, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gorostidi M, Sarafidis PA, de la Sierra A, Segura J, de la Cruz JJ, Banegas JR, Ruilope LM, Spanish ABPM Registry Investigators : Differences between office and 24-hour blood pressure control in hypertensive patients with CKD: A 5,693-patient cross-sectional analysis from Spain. Am J Kidney Dis 62: 285–294, 2013 [DOI] [PubMed] [Google Scholar]
- 32.Muntner P, Anderson A, Charleston J, Chen Z, Ford V, Makos G, O’Connor A, Perumal K, Rahman M, Steigerwalt S, Teal V, Townsend R, Weir M, Wright JT, Jr, Chronic Renal Insufficiency Cohort (CRIC) Study Investigators : Hypertension awareness, treatment, and control in adults with CKD: results from the Chronic Renal Insufficiency Cohort (CRIC) Study. Am J Kidney Dis 55: 441–451, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Minutolo R, Borrelli S, Scigliano R, Bellizzi V, Chiodini P, Cianciaruso B, Nappi F, Zamboli P, Conte G, De Nicola L: Prevalence and clinical correlates of white coat hypertension in chronic kidney disease. Nephrol Dial Transplant 22: 2217–2223, 2007 [DOI] [PubMed] [Google Scholar]
- 34.Stehouwer CD, Henry RM, Dekker JM, Nijpels G, Heine RJ, Bouter LM: Microalbuminuria is associated with impaired brachial artery, flow-mediated vasodilation in elderly individuals without and with diabetes: further evidence for a link between microalbuminuria and endothelial dysfunction--the Hoorn Study. Kidney Int Suppl 92: S42–S44, 2004 [DOI] [PubMed] [Google Scholar]
- 35.Suliman ME, Yilmaz MI, Carrero JJ, Qureshi AR, Saglam M, Ipcioglu OM, Yenicesu M, Tong M, Heimbürger O, Barany P, Alvestrand A, Lindholm B, Stenvinkel P: Novel links between the long pentraxin 3, endothelial dysfunction, and albuminuria in early and advanced chronic kidney disease. Clin J Am Soc Nephrol 3: 976–985, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Veerabhadrappa P, Diaz KM, Feairheller DL, Sturgeon KM, Williamson ST, Crabbe DL, Kashem AM, Brown MD: Endothelial-dependent flow-mediated dilation in African Americans with masked-hypertension. Am J Hypertens 24: 1102–1107, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pierdomenico SD, Cuccurullo F: Prognostic value of white-coat and masked hypertension diagnosed by ambulatory monitoring in initially untreated subjects: an updated meta analysis. Am J Hypertens 24: 52–58, 2011 [DOI] [PubMed] [Google Scholar]
- 38.Franklin SS, Thijs L, Hansen TW, Li Y, Boggia J, Kikuya M, Björklund-Bodegård K, Ohkubo T, Jeppesen J, Torp-Pedersen C, Dolan E, Kuznetsova T, Stolarz-Skrzypek K, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Lind L, Sandoya E, Kawecka-Jaszcz K, Imai Y, Wang J, Ibsen H, O’Brien E, Staessen JA, International Database on Ambulatory Blood Pressure in Relation to Cardiovascular Outcomes Investigators : Significance of white-coat hypertension in older persons with isolated systolic hypertension: a meta-analysis using the International Database on Ambulatory Blood Pressure Monitoring in Relation to Cardiovascular Outcomes population. Hypertension 59: 564–571, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hänninen MR, Niiranen TJ, Puukka PJ, Kesäniemi YA, Kähönen M, Jula AM: Target organ damage and masked hypertension in the general population: the Finn-Home study. J Hypertens 31: 1136–1143, 2013 [DOI] [PubMed] [Google Scholar]
- 40.Agarwal R, Andersen MJ: Prognostic importance of ambulatory blood pressure recordings in patients with chronic kidney disease. Kidney Int 69: 1175–1180, 2006 [DOI] [PubMed] [Google Scholar]
- 41.Minutolo R, Agarwal R, Borrelli S, Chiodini P, Bellizzi V, Nappi F, Cianciaruso B, Zamboli P, Conte G, Gabbai FB, De Nicola L: Prognostic role of ambulatory blood pressure measurement in patients with nondialysis chronic kidney disease. Arch Intern Med 171: 1090–1098, 2011 [DOI] [PubMed] [Google Scholar]
- 42.Vlachopoulos C, Aznaouridis K, O’Rourke MF, Safar ME, Baou K, Stefanadis C: Prediction of cardiovascular events and all-cause mortality with central haemodynamics: a systematic review and meta-analysis. Eur Heart J 31: 1865–1871, 2010 [DOI] [PubMed] [Google Scholar]
- 43.Blacher J, Safar ME, Guerin AP, Pannier B, Marchais SJ, London GM: Aortic pulse wave velocity index and mortality in end-stage renal disease. Kidney Int 63: 1852–1860, 2003 [DOI] [PubMed] [Google Scholar]
- 44.Silberberg JS, Barre PE, Prichard SS, Sniderman AD: Impact of left ventricular hypertrophy on survival in end-stage renal disease. Kidney Int 36: 286–290, 1989 [DOI] [PubMed] [Google Scholar]
- 45.Banegas JR, Ruilope LM, de la Sierra A, de la Cruz JJ, Gorostidi M, Segura J, Martell N, García-Puig J, Deanfield J, Williams B: High prevalence of masked uncontrolled hypertension in people with treated hypertension. Eur Heart J 35: 3304–3312, 2014 [DOI] [PubMed] [Google Scholar]
- 46.Muxfeldt ES, Fiszman R, de Souza F, Viegas B, Oliveira FC, Salles GF: Appropriate time interval to repeat ambulatory blood pressure monitoring in patients with white-coat resistant hypertension. Hypertension 59: 384–389, 2012 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.