Abstract
BACKGROUND
The aim of this study was to characterize patients readmitted following inpatient general surgery procedures. We hypothesized that a decreased length of stay would increase risk for readmission.
METHODS
We utilized our institutional National Surgical Quality Improvement Project database from 2006 to 2011. The main outcome of interest was 30-day readmission. Univariate and logistic regression analyses identified risk factors for readmission.
RESULTS
We identified 3,556 patients, with 322 (9%) readmitted within 30 days after discharge. Multivariable analysis demonstrated age, dyspnea, and American Society of Anesthesiologists class to be independent risk factors for readmission. In addition, patients who suffered multiple complications had a decreased risk for readmission as length of stay increased. Patients with <2 postoperative complications had an increased risk for readmission as length of stay increased.
CONCLUSIONS
Contributors to postoperative readmissions are multifactorial. Perioperative factors predict risk for readmission and may help determine a target length of stay. Prevention of postoperative complications may reduce readmission rates.
Keywords: Readmission, Postoperative, General surgery
Hospital readmission has recently become a focus of many hospital quality improvement programs. In 2008, the Medicare Payment Advisory Commission reported on a series of payment reforms to encourage coordination of patient care which included bundling of payments around an episode of care, gainsharing between hospitals and physicians, and a direct incentive to reduce readmissions.1 They found rates of readmission among patients diagnosed with an acute myocardial infarction, heart failure, or pneumonia to be upward of 17%. Using these numbers, the commission defined a number of preventable readmissions that could be avoided with improved index hospitalization patient care, discharge planning, or outpatient care coordination. Following this report, Congress enacted a hospital readmissions reduction program as part of the Patient Protection and Affordable Care Act of 2010. The hospital readmission reduction program was initiated by Centers for Medicare and Medicaid Services in 2012, which includes a penalty that results in the reduction of Medicare payments in 2013 to hospitals that had above-average rates of readmission among patients treated for acute myocardial infarction, heart failure, or pneumonia over the 3-year period from July 1, 2008 to June 30, 2011. In its most recent report, Medicare Payment Advisory Commission has recommended moving to a system whereby all-cause readmissions will be reported and penalties assessed based on a target rate of readmission.2 It is clear that surgical patients are different from medical patients and that causes of readmission are often related to underlying medical conditions rather than the initial admitting diagnosis.3 Therefore, it is critical that we clearly understand the problem of readmissions in the surgical patient population.
Multiple studies have attempted to define the patient factors that are associated with readmission. Patients of older age and of African-American race have been shown to be more likely to be readmitted.4,5 Other factors such as patient comorbidities, emergent surgery, transfusion requirements, and discharge to a skilled nursing facility have been associated with increased readmission rates.5 Hospital length of stay has also been studied as a possible predictor of readmission rates in the surgical patient population, but recent literature is conflicting. One study found that patients discharged 0 to 4 days after surgery had an increased risk for readmission (odds ratio, OR 5 1.45),6 while other studies identified an association between longer length of stay and an increased risk for readmission (OR 5 1.23 to 2.00).7–10
To decrease preventable, postoperative readmissions, we must first better understand the patient and perioperative variables which contribute to increased risk for readmission. The role of postoperative complications and risk for readmission cannot be downplayed.11 However, it is not clear if all complications carry the same risk for readmission. Furthermore, the effect of length of stay on risk for readmission in patients who have suffered complications needs to be clarified. To better understand these issues, we have undertaken this study with the following aims: (1) to characterize patients who were readmitted following inpatient general surgical procedures from 2006 to 2011; (2) to compare and contrast those patients readmitted with those who were not readmitted within 30 days after surgery; and (3) to correlate length of stay with rates of 30-day postoperative readmissions. We hypothesized that shorter length of stay would correlate with an increased risk for readmission.
Methods
Patients who were captured in the American College of Surgeons’ National Surgical Quality Improvement Project (NSQIP) database from August 1, 2006 to June 30, 2011 were evaluated. The University of Wisconsin Hospital and Clinics has participated in this project since August 1, 2006 and investigations using this database have been reviewed and approved by the University of Wisconsin-Madison Human Research Protection Program. Eligible patients included those who underwent an inpatient general surgery procedure. We excluded patients who underwent an emergency operation, an outpatient procedure, and any patient who underwent an operation not classified as general surgery as defined by the NSQIP program. Patients who died before 30 days post discharge were also excluded from the readmission risk analysis.
The NSQIP Surgical Clinical Reviewers (SCRs) prospectively collect over 20 preoperative morbidity variables and 30-day outcomes including complications, length of stay, and reoperation. In addition to preoperative variables, a number of intraoperative variables are also collected. Before 2012, readmissions were not formally collected by the NSQIP SCRs. Therefore, we linked the NSQIP database with our hospital discharge data and identified readmissions in the over 8,000 patients within our database. Readmissions occurring within 30 days of discharge from index hospitalization after a general surgery procedure were identified and studied. All readmitted patients were verified by independent review. Given that our hospital is a regional tertiary medical center, we acknowledge that some patients may be readmitted at their local hospitals and, therefore, not captured by our hospital database. To determine how frequently patients are not sent back to our hospital, we examined the discrepancy between our SCRs documentation in 2011 and our hospital database. This interrogation revealed that only 1 patient who was readmitted in 2011 was not captured in the hospital database indicating that most patients are sent back to our center for further care.
Explanatory variables included age, sex, and race. Race was identified according to the NSQIP classification system. The number of minority patients in this population was small; therefore race was categorized as Caucasian and non-Caucasian. We utilized age as a categorical variable in this study by classifying according to the following groups: <30, 30 to 49, 50 to 69, 70 to 89, and ≥90 years. Included in the explanatory variables were perioperative characteristics. Preoperative characteristics included the following 19 comorbid conditions: American Society of Anesthesiologists (ASA) class 1 to 5, body mass index ≥30, diabetes mellitus, smoking, dyspnea, preoperative functional status, chronic obstructive pulmonary disease, ascites within 30 days before surgery, congestive heart failure within 30 days before surgery, hypertension, acute renal failure, hemodialysis, disseminated cancer, open wound, steroid/immunosuppressive medication use, weight loss <10% within 6 months before surgery, bleeding disorder, transfusion of red blood cells within 72 hours before surgery, and sepsis within 48 hours before surgery. In addition, functional status was evaluated and patients were classified as independent, partially dependent, and totally dependent. Surgical specialty was also analyzed with subsets including advanced minimally invasive surgery, colorectal, endocrine, general surgery, and hepatopancreaticobiliary/soft tissue oncology. Medical home was categorized into UWHospital/Clinics, veterans administration Hospital/Clinics, and other. Payer was categorized into private insurance, Medicare/Medicaid, and uninsured.
Intraoperative characteristics included the following: preoperative diagnosis, procedures occurring at the time of index surgery, length of procedure, and operative approach (laparoscopic or open). We categorized preoperative diagnosis by International Statistical Classification of Disease 9 codes. Diagnoses with ≥100 cases were isolated and all other diagnoses with <100 cases were categorized as “all other diagnoses.” Procedures occurring at the time of index surgery were placed into 2 categories, “concurrent” meaning a second procedure being performed by the same surgeon or “other” meaning a second procedure being performed by a different team of surgeons. Length of procedure was clustered into <2, 2:00 to 3:59, 4:00 to 5:59, and ≥6 hours. Postoperative characteristics included the following: length of stay, ≥2 complications, reoperation, and postoperative complications as defined by NSQIP criteria. Patients were categorized into index length of stay groups as follows: ≤2, 3 to 5, 6 to 8, and >8 days.
Statistical analysis was performed using SPSS Version 20 (IBM Corp, Armonk, NY). Significance was defined as a 2-tailed P value of <.05. Descriptive analysis of categorical variables was performed with chi-square testing. In addition, ASA class and length of procedure were compared between patients with and without readmission using a Wilcoxon rank sums tests. Explanatory variables included demographics, preoperative, intraoperative, postoperative variables, medical home, and payer.
Multivariable logistic regression was used to identify factors that independently correlated with risk for readmission. Variables were removed from the multivariable analysis if they occurred fewer than 5 times in the dataset to achieve an acceptable order of power in the statistical analysis. These variables included the following: patients >90 years of age, on a ventilator, congestive heart failure, acute renal insufficiency, ASA class 5, and totally dependent functional status. We controlled for multicollinearity using a correlation statistic. We found no correlation between complications and reoperation; however, a strong relationship existed between complications and length of stay. Therefore, we created a category based on a combination of these 2 variables and evaluated the relationship of this combined category to readmission.
Results
We identified 3,632 patients who underwent an inpatient general surgery procedure from our database. Within 30 days post discharge, 76 patients died (2%) and were not included in the remainder of the analysis. Of the 3,556 patients remaining, 322 patients (9%) were readmitted within 30 days of discharge. Median length of stay for the index hospitalization was 6.0 days for all patients and 6.9 days for patients who were readmitted.
Preoperative predictors of readmission using univariate analysis are presented in Table 1. We found steroid/immunosuppressive medication use, weight loss .10% within 6 months of surgery, bleeding disorder, functional status, and ASA class to correlate significantly with risk for readmission (P < .05). Table 2 presents readmission rate as a function of preoperative diagnosis and demonstrates that some patient groups are at high risk for readmission (rates ranging from 4% for those patients with esophageal disease to 24% for patients with ulcerative colitis, P < .001). It is not clear if this is a reflection of the operation, the disease process, or a combination of the two. The only intraoperative factor found to correlate with increased risk for readmission was operation length. Patients who underwent operations >2 hours long were readmitted 7% of the time, while patients with operations R6 hours were readmitted 15% of the time (Table 3).
Table 1.
Patient characteristics and preoperative risk factors for readmission
| Risk factors | Total | No. of patients readmitted (%) |
No. of patients not readmitted (%) |
P value |
|---|---|---|---|---|
| No. of patients | 3,556 | 320 (9) | 3,236 (91) | |
| Sex (Male) | ||||
| Yes | 1,925 | 164 (9) | 1,761 (91) | |
| No | 1,631 | 151 (9) | 1,480 (91) | .238 |
| Race (White) | ||||
| Yes | 3,198 | 282 (9) | 2,907 (91) | |
| No | 335 | 31 (9) | 304 (91) | .432 |
| Functional status | ||||
| Independent | 3,243 | 292 (9) | 2,951 (91) | |
| Partially dependent | 230 | 30 (13) | 200 (87) | |
| Totally dependent | 83 | 3 (4) | 80 (96) | .021 |
| ASA class | ||||
| 1 | 260 | 10 (4) | 250 (96) | |
| 2 | 1,920 | 157 (8) | 1,763 (92) | |
| 3 | 1,217 | 129 (11) | 1,088 (89) | |
| 4 | 153 | 18 (12) | 135 (88) | <.001 |
| BMI ≥ 30 | ||||
| Yes | 1,381 | 119 (9) | 1,262 (91) | |
| No | 2,175 | 196 (9) | 1,979 (91) | .367 |
| Smoker | ||||
| Yes | 635 | 59 (9) | 576 (91) | |
| No | 2,921 | 256 (9) | 2,665 (91) | .360 |
| Dyspnea | ||||
| Yes | 283 | 19 (7) | 264 (93) | |
| No | 3,273 | 296 (9) | 2,977 (91) | .110 |
| COPD | ||||
| Yes | 147 | 16 (11) | 131 (89) | |
| No | 3,409 | 299 (9) | 3,110 (91) | .226 |
| Ascites | ||||
| Yes | 64 | 6 (9) | 58 (91) | |
| No | 3,492 | 309 (9) | 3,183 (91) | .506 |
| CHF | ||||
| Yes | 38 | 1 (3) | 37 (97) | |
| No | 3,518 | 314 (9) | 3,204 (91) | |
| Hypertension | ||||
| Yes | 1,538 | 138 (9) | 1,400 (91) | |
| No | 2,018 | 177 (9) | 1,841 (91) | .440 |
| Acute renal failure | ||||
| Yes | 14 | 0 (0) | 14 (100) | |
| No | 3,543 | 315 (9) | 3,227 (91) | .272 |
| Dialysis | ||||
| Yes | 36 | 5 (14) | 31 (86) | |
| No | 3,520 | 310 (9) | 3,210 (91) | .210 |
| Cancer | ||||
| Yes | 166 | 16 (10) | 150 (90) | |
| No | 3,390 | 299 (9) | 3,091 (91) | .399 |
| Open wound | ||||
| Yes | 203 | 22 (11) | 181 (89) | |
| No | 3,353 | 293 (9) | 3,060 (91) | .184 |
| Steroid use | ||||
| Yes | 274 | 47 (17) | 227 (83) | |
| No | 3,282 | 268 (8) | 3,014 (92) | <.001 |
| Weight loss | ||||
| Yes | 186 | 24 (13) | 162 (87) | |
| No | 3,370 | 291 (9) | 3,079 (91) | .036 |
| Bleeding | ||||
| Yes | 224 | 32 (14) | 192 (86) | |
| No | 3,332 | 283 (8) | 3,049 (92) | .004 |
| Transfusion | ||||
| Yes | 39 | 5 (13) | 34 (87) | |
| No | 3,517 | 310 (9) | 3,207 (91) | .260 |
| Sepsis | ||||
| Yes | 565 | 52 (9) | 513 (91) | |
| No | 2,991 | 263 (9) | 2,728 (91) | .402 |
| Comorbidities ≥2 | ||||
| Yes | 2,785 | 260 (9) | 2,525 (91) | |
| No | 771 | 55 (7) | 716 (93) | .031 |
| Diabetes | ||||
| Yes | 538 | 46 (9) | 492 (91) | |
| No | 3,018 | 269 (9) | 2,749 (91) | .792 |
| Age | ||||
| <30 | 366 | 44 (12) | 322 (88) | |
| 30–49 | 974 | 81 (8) | 893 (92) | |
| 50–69 | 1,526 | 138 (9) | 1,388 (91) | |
| 70–89 | 671 | 50 (7) | 621 (93) | |
| ≥90 | 19 | 2 (11) | 17 (89) | .155 |
ASA = American Society of Anesthesiologists; BMI = body mass index; CHF = congestive heart failure; COPD = chronic obstructive pulmonary disease.
Table 2.
Risk for readmission based on diagnostic ICD-9 codes
| Total | No. of patients readmitted (%) |
No. of patients not readmitted (%) |
P value | |
|---|---|---|---|---|
| Disease of the esophagus | 105 | 4 (4) | 101 (96) | |
| Malignant neoplasm of the colon | 145 | 9 (6) | 136 (94) | |
| Benign neoplasm of digestive | 125 | 7 (6) | 118 (94) | |
| Malignant neoplasm of the pancreas | 108 | 8 (7) | 100 (93) | |
| Obesity or hyperalimentation | 173 | 12 (7) | 161 (93) | |
| Cholelithiasis | 130 | 9 (7) | 121 (93) | |
| Hernia in the abdominal cavity with obstruction |
101 | 8 (8) | 93 (92) | |
| All other diagnoses | 1,583 | 127 (8) | 1,456 (92) | |
| Hernia in the abdominal cavity without obstruction |
192 | 17 (9) | 175 (91) | |
| Diverticula of the intestine | 123 | 11 (9) | 112 (91) | |
| Malignant neoplasm of the rectum, rectosigmoid junction, and anus |
150 | 15 (10) | 135 (90) | |
| Other disorders of the intestine | 134 | 15 (11) | 119 (89) | |
| Intestinal obstruction | 161 | 19 (12) | 142 (88) | |
| Attention to colostomy/ileostomy | 203 | 28 (14) | 175 (86) | |
| Ulcerative colitis | 123 | 30 (24) | 93 (76) | <.001 |
ICD = International Statistical Classification of Disease.
Table 3.
Intraoperative risk factors for readmission
| Risk factors | Total | No. of patients readmitted (%) |
No. of patients not readmitted (%) |
P value |
|---|---|---|---|---|
| Laparoscopic | ||||
| Yes | 1,315 | 104 (8) | 1,211 (92) | |
| No | 2,241 | 224 (10) | 2,017 (90) | .158 |
| Length of procedure (h) | ||||
| <2:00 | 1,787 | 131 (7) | 1,656 (93) | |
| 2:00–3:59 | 1,165 | 103 (9) | 1,062 (91) | |
| 4:00–5:59 | 363 | 45 (12) | 318 (88) | |
| ≥6:00 | 241 | 36 (15) | 205 (85) | <.001 |
| Concurrent procedure | ||||
| Yes | 216 | 22 (10) | 194 (90) | |
| No | 3,340 | 293 (9) | 3,047 (91) | .273 |
| Other procedures | ||||
| Yes | 1,927 | 175 (9) | 1,752 (91) | |
| No | 1,629 | 140 (9) | 1,489 (91) | .327 |
Postoperative risk factors for readmission are presented in Table 4 and included a return to the operating room (9% vs 25%) and the combination of postoperative complications with length of stay (P < .001). We found that patients with <2 complications had a higher risk for readmission as the length of stay increased (P < .001, Fig. 1). In these patients, readmission rates increased from 4% in patients who were hospitalized <3 days to 7% in patients hospitalized >8 days. Conversely, risk for readmission and length of stay were indirectly related to patients with >2 complications (P < .001, Fig. 1). Patients with complications and short hospital stay (<3 days) were readmitted 76% of the time as compared with a readmission rate of 16% in patients with prolonged length of stay (>8 days). We also found a linear correlation between readmission and number of complications (P < .001, Fig. 2). The majority of patients (67%) who were readmitted suffered from surgical site infections and wound dehiscence (data not shown). Neither payer nor medical home was a risk factor for readmission (Table 5).
Table 4.
Postoperative risk factors for readmission
| Risk factors | Total (n) | No. of patients readmitted (%) |
No. of patients not readmitted (%) |
P value |
|---|---|---|---|---|
| Return to OR | ||||
| Yes | 51 | 13 (25) | 38 (75) | |
| No | 3,504 | 302 (9) | 3,202 (91) | <.001 |
| Postoperative | ||||
| complications and LOS | ||||
| Complications <2 | ||||
| LOS 0–2 | 1,090 | 42 (4) | 1,048 (96) | |
| LOS 3–5 | 1,053 | 63 (6) | 990 (94) | |
| LOS 6–8 | 595 | 35 (6) | 590 (94) | |
| LOS >8 | 352 | 26 (7) | 326 (93) | |
| Complications ≥2 | ||||
| LOS 0–2 | 25 | 19 (76) | 6 (24) | |
| LOS 3–5 | 75 | 45 (60) | 30 (40) | |
| LOS 6–8 | 85 | 40 (47) | 45 (53) | |
| LOS >8 | 281 | 45 (16) | 236 (84) | <.001 |
LOS = length of stay; OR = operating room.
Figure 1.
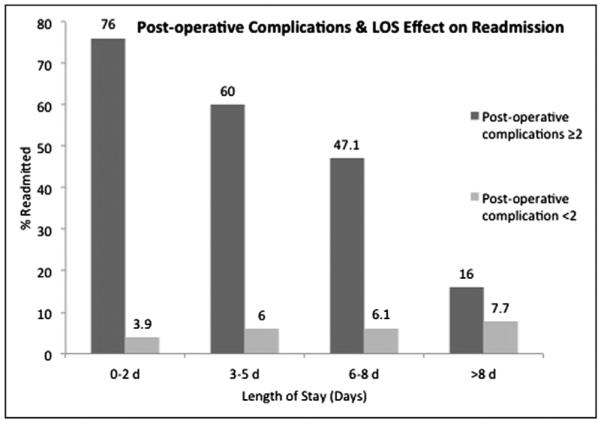
Patients who suffered R2 postoperative complications were found to have a decreased risk of readmission as length of stay increased. Conversely, those patients with <2 postoperative complications had an increased risk for readmission as length of stay increased.
Figure 2.
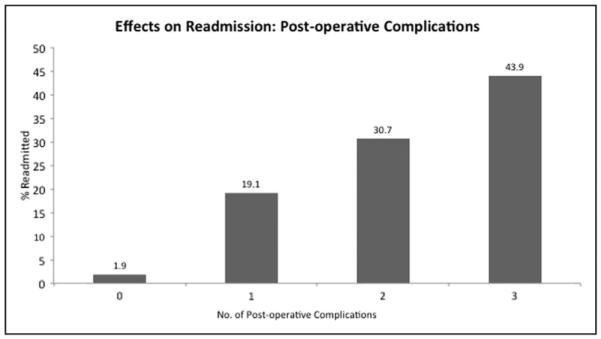
The impact of postoperative complications on readmission. As the number of postoperative complications increased, the percent of patients readmitted increased significantly.
Table 5.
Payer and medical home impact on readmission
| Risk factors | Total (n) | No. of patients readmitted (%) |
No. of patients not readmitted (%) |
P value |
|---|---|---|---|---|
| Payer | ||||
| Private | 2,023 | 182 (9) | 1,841 (91) | |
| Medicare/Medicaid | 1,367 | 109 (8) | 1,258 (92) | |
| Self | 105 | 5 (5) | 100 (95) | .187 |
| Medical home | ||||
| UW Health | 988 | 89 (9) | 899 (91) | |
| VA hospital/clinics | 16 | 0 (0) | 16 (100) | |
| Others | 2002 | 200 (10) | 1,802 (90) | .281 |
UW = University of Wisconsin; VA = veterans administration.
Table 6 illustrates surgeon specialty as a risk factor for readmission. For example, colorectal patients were readmitted at a rate of 10.9%, whereas endocrine patients had a readmission rate of 3.9% (P < .001).
Table 6.
Specialty impact on readmission rate
| Risk factors | Total (n) | No. of patients readmitted (%) |
No. of patients not readmitted (%) |
P value |
|---|---|---|---|---|
| Specialty | <.001 | |||
| Advanced MIS | 469 | 38 (8) | 431 (92) | |
| Colorectal | 1,306 | 142 (11) | 1,164 (89) | |
| Endocrine | 283 | 11 (4) | 272 (96) | |
| General surgery | 853 | 73 (9) | 780 (91) | |
| Hepatopancreaticobiliary and soft tissue oncology | 645 | 51 (8) | 594 (92) |
MIS = minimally invasive surgery.
Independent risk factors for readmission are presented in Table 7. Factors that are independently correlated with a high risk for readmission included the following: steroid use, bleeding disorder, ASA class 2, length of procedure <2 hours, a return to the operating room, preoperative diagnosis of hernia in the abdominal cavity without obstruction and surgeon specialty. Finally, because of multicollinearity, we created a new variable that controlled length of stay for >2 complications and included this in the multivariable analysis. We found that patients who suffered ≥2 complications and a length of stay <2 days were significantly more likely to be readmitted (OR 90.900, 95% confidence interval 32.950 to 250.765) than patients without complications (Table 7).
Table 7.
Multivariable analysis: significant independent risk factors for readmission
| Risk factors | Adjusted OR |
95% CI | |
|---|---|---|---|
| Age | |||
| 30–49 | .601 | .382 | .976 |
| 50–69 | .556 | .344 | .898 |
| 70–89 | .336 | .186 | .608 |
| Sex (Male) | 1.036 | .791 | 1.356 |
| Race (White) | 1.209 | .771 | 1.895 |
| BMI .30 | 1.022 | .732 | 1.427 |
| Diabetes | .939 | .559 | 1.579 |
| Smoking | .965 | .667 | 1.396 |
| Dyspnea | 1.796 | 1.024 | 3.150 |
| COPD | 1.417 | .736 | 2.728 |
| Ascites | .546 | .188 | 1.590 |
| Hypertension | .967 | .688 | 1.360 |
| Dialysis | 1.254 | .396 | 3.976 |
| Cancer | .801 | .413 | 1.554 |
| Open wound | .891 | .495 | 1.604 |
| Steroids | 1.425 | .892 | 2.277 |
| Weight loss | 1.137 | .662 | 1.950 |
| Bleeding | 1.541 | .947 | 2.508 |
| Transfusion | .733 | .231 | 2.324 |
| Sepsis | .821 | .534 | 1.263 |
| Comorbidities ≥2 | 1.059 | .669 | 1.679 |
| ASA class | |||
| 1 | 1.902 | .923 | 3.918 |
| 2 | 2.638 | 1.227 | 5.671 |
| 3 | 3.143 | 1.174 | 8.416 |
| Functional status | .865 | .507 | 1.476 |
| Laparoscopic | 1.151 | .810 | 1.634 |
| Length of procedure (h) | |||
| 0–2 | 1.145 | .811 | 1.616 |
| 2–4 | 1.337 | .815 | 2.194 |
| 4–6 | 1.272 | .691 | 2.343 |
| Concurrent procedure | 1.131 | .662 | 1.933 |
| Other procedures | .845 | .611 | 1.169 |
| Return to operating room | 2.218 | 1.000 | 4.922 |
| Patients | |||
| with complications ≥2 (d) | |||
| LOS 0–2 | 90.900 | 32.950 | 250.765 |
| LOS 3–5 | 32.783 | 17.295 | 62.142 |
| LOS 6–8 | 23.710 | 12.638 | 44.484 |
| LOS ≥8 | 4.584 | 2.535 | 8.289 |
| Surgeon specialty | 1.298 | .904 | 1.863 |
| Hernia without obstruction | 1.619 | .777 | 3.371 |
ASA = American Society of Anesthesiologists; BMI = body mass index; CI = confidence interval; COPD = chronic obstructive pulmonary disease; LOS = length of stay; OR = odds ratio.
Conclusions
The aim of this study was to identify risk factors for 30-day readmission in patients who underwent general surgical procedures. Not surprisingly, we found that patients were more likely to be readmitted if they had postoperative complications or required reoperation within 30 days. Interestingly, we also identified an increased risk of readmission in patients with multiple complications and shorter (<2 days) length of stay.
Other authors have similarly identified shorter length of stay as a risk factor for readmission independent of postoperative complication.5 However, an association between longer length of stay and readmissions has also been described.8,10 We may have identified an explanation for this discrepancy in the literature by taking into account the number of postoperative complications. We found that patients with 0 or 1 complication had readmission rates that correlated with longer length of stay where patients with multiple complications were more likely to be readmitted after shorter lengths of stay. McAleese and Odling-Smee12 found that 41% of patients who had complications and were subsequently readmitted had been discharged before the average length of stay for that procedure. These results may imply that patients are being discharged too soon postoperatively before complications have been diagnosed or without timely follow-up.
We found that comorbidities such as bleeding disorder, worse functional status, and preoperative weight loss were predictive of postoperative readmission. We also found that postoperative complications strongly correlated with risk for readmission. Others have found that postoperative complications were strongly associated with risk for readmission.11 Although we did not find an association between older age and sex with risk for readmission, we did find an interesting relationship among postoperative complications, length of stay, and readmission. In fact, we found that patients with multiple complications had a decrease in their risk for readmission as length of stay increased. Conversely, patients with a single complication had an increased risk for readmission as their length of stay increased. In future studies, we plan on differentiating the timing of these complications and determining which complications occur after specific procedures.
Our study has limitations inherent to retrospective database analysis where unmeasured differences could contribute to confounding. A large, prospective, randomized study of the effects of postoperative complications and length of stay on readmissions is not feasible. Therefore, we performed a multivariable analysis to attempt to control for known variables that impact the risk for readmission. With these statistical controls, the relationship among postoperative complications, length of stay, and readmissions remained significant.
We recognize that this study reflects our institution’s experience and only represents about 20% of all general surgery procedures performed in our hospital over the study time period. Sampling error may limit the generalizability. However, others have shown the validity of the NSQIP data collection process.13 An additional limitation to this study is that patients who undergo surgery at the University of Wisconsin Hospital are referred from a large geographic region beyond the borders of the state. Some patients may have been readmitted to the local hospitals without our knowledge, in which case the readmission rate in this study would be an underestimate. We have tried to control for this limitation as described in the “Methods” section, but recognize that our sampling may have significant limitations. Finally, we acknowledge that a potential weakness of this study is our lack of insight into readmission rates in specific patient groups. Although we are not able to evaluate readmission rates with respect to operative complexity, we have evaluated readmission rate by diagnosis code and by surgical specialty in an attempt to identify groups of patients at high risk for readmission. However, the goal of this study was to examine the relationship between complications and readmission. Thus, we have been able to devise interventions for patients who have suffered complications in an attempt to decrease readmissions.
In summary, we have identified risk factors for 30-day readmission in general surgery patients. We also uncovered an interesting relationship among multiple complications, length of stay, and readmission rates. Our future studies will focus on elucidating a relationship between diagnosis groups and readmission as well as further clarifying the timing of complications and risk for readmission.
Acknowledgment
We would like to acknowledge Glen Leverson who offered statistical advice on this project.
Supported by the University of Wisconsin Department of Surgery and the Shapiro Research Program.
Footnotes
The authors declare no conflicts of interest and have not received support from industry or organizations that might have influenced this work.
References
- 1.MedPAC . Report to the Congress: Reforming the Delivery System. M.P.A. Commission; Washington, DC: 2008. pp. 83–101. [Google Scholar]
- 2.MedPAC . Report to the Congress: Medicare and the Health Care Delivery System. M.P.A. Commission; Washington, DC: 2013. pp. 91–110. [Google Scholar]
- 3.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 4.Schneider EB, Haider AH, Hyder O, et al. Assessing short-and long-term outcomes among black vs white Medicare patients undergoing resection of colorectal cancer. Am J Surg. 2013;205:402–8. doi: 10.1016/j.amjsurg.2012.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Greenblatt DY, Weber SM, O’Connor ES, et al. Readmission after colectomy for cancer predicts one-year mortality. Ann Surg. 2010;251:659–69. doi: 10.1097/SLA.0b013e3181d3d27c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hendren S, Morris AM, Zhang W, et al. Early discharge and hospital readmission after colectomy for cancer. Dis Colon Rectum. 2011;54:1362–7. doi: 10.1097/DCR.0b013e31822b72d3. [DOI] [PubMed] [Google Scholar]
- 7.Wick EC, Shore AD, Hirose K, et al. Readmission rates and cost following colorectal surgery. Dis Colon Rectum. 2011;54:1475–9. doi: 10.1097/DCR.0b013e31822ff8f0. [DOI] [PubMed] [Google Scholar]
- 8.Kelly M, Sharp L, Dwane F, et al. Factors predicting hospital length-of-stay and readmission after colorectal resection: a population-based study of elective and emergency admissions. BMC Health Serv Res. 2012;12:77. doi: 10.1186/1472-6963-12-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dorman RB, Miller CJ, Leslie DB, et al. Risk for hospital readmission following bariatric surgery. PLoS One. 2012;7:e32506. doi: 10.1371/journal.pone.0032506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barbas AS, Turley RS, Mallipeddi MK, et al. Examining reoperation and readmission after hepatic surgery. J Am Coll Surg. 2013;216:915–23. doi: 10.1016/j.jamcollsurg.2013.01.008. [DOI] [PubMed] [Google Scholar]
- 11.Kassin MT, Owen RM, Perez SD, et al. Risk factors for 30-day hospital readmission among general surgery patients. J Am Coll Surg. 2012;215:322–30. doi: 10.1016/j.jamcollsurg.2012.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McAleese P, Odling-Smee W. The effect of complications on length of stay. Ann Surg. 1994;220:740–4. doi: 10.1097/00000658-199412000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shiloach M, Frencher SK, Steeger JE, et al. Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2010;210:6–16. doi: 10.1016/j.jamcollsurg.2009.09.031. [DOI] [PubMed] [Google Scholar]


