Introduction
Pituitary adenomas, Rathke’s cysts, craniopharyngiomas, and other sellar lesions are often resected through a transsphenoidal corridor. Surgical access to this corridor can be achieved either microscopically, using a standard operating microscope and peering into the transsphenoidal space, or endoscopically, with the help of an endoscopic camera and light source. Microscopic transsphenoidal surgery predates endoscopic surgery, and was historically the more common technique [1]. This is perhaps because the microscope is familiar to neurosurgeons and used in many other neurosurgical approaches. Endoscopy, on the other hand, requires the acquisition of a novel skillset for most neurosurgeons, but provides wider and more flexible viewing angles which can be critical during the resection of extrasellar tumors.
While both approaches are useful and important for pituitary surgeons, the frequency at which both techniques are used is unknown. The Centers for Medicare and Medicaid Services (CMS) Part B National Summary Data File lists the number of procedures billed to CMS by Current Procedural Terminology (CPT) code, which specifically differentiates endoscopic from microscopic pituitary surgery. These data were supplemented by the CMS Part B Carrier Summary Data File, which provides state-level data. International Classification of Disease (ICD-9), like those used in the Nationwide Inpatient Sample (NIS), do not specify whether a pituitary surgery was microscopic or endoscopic, so such databases cannot determine the relative proportion of the two techniques.
Methods
Using the CMS National Summary Data File and the CMS Carrier Summary Data File, we extracted all procedures with codes 61548 (microscopic hypophysectomy, transnasal or transseptal) and 62165 (neuroendoscopy for excision of pituitary tumor, transnasal or transsphenoidal), spanning the years 2003 to 2013. When the CMS provides state-level data in the Carrier file, procedure counts between 1 and 10 are censored and replaced with “n/a” to protect patient anonymity. We therefore conservatively replaced these “n/a” values with values of 1 during our analyses, so as not to overestimate endoscopic procedures. When constructing national maps, the average number of cases per year was ploted for two time periods, at the beginning (2005-7) of the available data, and the end of the available data (2009-11). Data were unavailable for Indiana and unavailable for 2005-7 for Pennsylvania. Figures and analysis were conducted with Matlab R2015a (MathWorks; Natick, MA, USA) and SPSS version 23 (IBM Corp.; Armonk, NY, USA).
Results
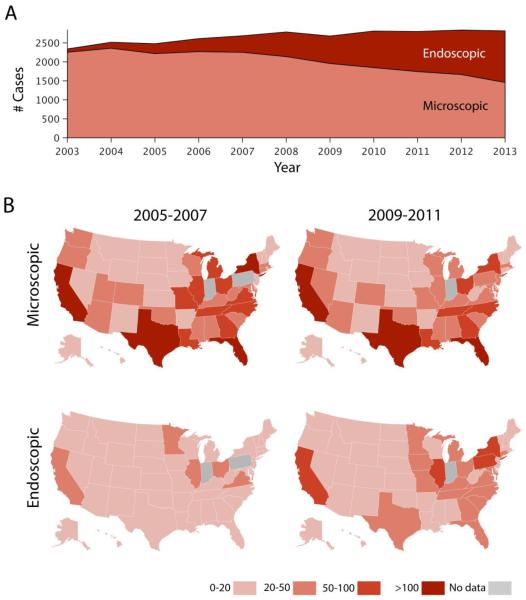
From 2003 to 2013, there was a strong and consistent increase in endoscopic transsphenoidal procedures and a gradual decline in microscopic procedures for pituitary tumors (Figure 1A). These trends were statistically significant, with linear regression showing a decline of 84.6 cases per year (95% confidence interval [CI] 107.5, 67.7) for microscopic pituitary surgery (F = 69.8, p < 0.001, ANOVA) and a gain of 130.2 cases per year (95% CI 118.4, 142.1) for endoscopic pituitary surgery (F = 615.7, p < 0.001, ANOVA).
Figure 1. Trends in pituitary surgery in the United States.
A) National data from CMS show that microscopic transsphenoidal cases (light red) decreased from 2003 to 2013, while endoscopic cases increased (dark red). B) State-level data are shown as the average number of cases per year during the periods 2005-2007 and 2009-2011. Data for Indiana were unavailable, as were data from 2005-7 from Pennsylvania.
State-level data was available from 2005 to 2011, a subset of the national data. The trends of decreasing microscopic surgery and increasing endoscopic surgery were also present in this data (Figure 1B). When years 2009-2011 were compared to the earlier years 2005-2008, 38 of 48 states decreased their rate of microscopic surgery, as compared to 38 of 48 states where rates endoscopic surgery increased (p < 0.001, Chi-Square test). The 10 states that increased their microscopy rates were Alaska, Arizona, Arkansas, Delaware, Hawaii, Idaho, Nevada, New Jersey, Washington, and Wyoming. The 10 states the did not increase their endoscopy rates were Idaho, Maine, Minnesota, Montana, Nevada, North Dakota, Ohio, South Dakota, West Virginia, and Wyoming.
Discussion
There is currently a lack of high-level evidence supporting one pituitary surgery technique over another, with some studies showing a benefit to endoscopic approaches [2] and others showing a higher rate of complications [1, 3]. Yet national data show a clear and rapid increase in the use of endoscopic surgery over the past decade, coupled to a decline in microscopic transsphenoidal surgery (Figure 1). Both techniques likely have specific advantages and disadvantages that might even be surgeon-specific, and there are often cases more suited to one modality as compared to the other (e.g., when a surgeon needs to “peer around a corner” with an endoscope). Despite the gradual decline of microscopic approaches in favor of endoscopic approaches, the microscopic skillset should continue to be cultivated and practiced, since endoscopic equipment is not always available in all hospitals or in all situations (e.g., some weekends or emergencies). Further studies are certainly indicated to provide a better understanding of any differences in outcomes, costs, and complications between the two strategies, and also to understand what is driving this trends in endoscopy.
Acknowledgments
Funding: No sponsor funding was used to support this study.
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
References
- 1.Pietro Mortini. Cons: endoscopic endonasal transsphenoidal pituitary surgery is not superior to microscopic transsphenoidal surgery for pituitary adenomas. Endocrine. 2014;47:415–420. doi: 10.1007/s12020-014-0365-0. doi: 10.1007/s12020-014-0365-0. [DOI] [PubMed] [Google Scholar]
- 2.Gao Y, Zhong C, Wang Y, et al. Endoscopic versus microscopic transsphenoidal pituitary adenoma surgery: a meta-analysis. World Journal of Surgical Oncology. 2014;12:94. doi: 10.1186/1477-7819-12-94. doi: 10.1186/1477-7819-12-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ammirati M, Wei L, Ciric I. Short-term outcome of endoscopic versus microscopic pituitary adenoma surgery: a systematic review and meta-analysis. J Neurol Neurosurg Psychiatr. 2013;84:843–849. doi: 10.1136/jnnp-2012-303194. doi: 10.1136/jnnp-2012-303194. [DOI] [PMC free article] [PubMed] [Google Scholar]