Abstract
Objective
The objectives of this study were to describe residents' experiences with end-of-life (EOL) education during a rotation in the intensive care unit (ICU), and to understand the possible influence of the 3 Wishes Project.
Design
We enrolled dying patients, their families and 1–3 of their clinicians in the 3 Wishes Project, eliciting and honouring a set of 3 wishes to bring peace to the final days of a critically ill patient's life, and ease the grieving process for families. We conducted semistructured interviews with 33 residents who had cared for 50 dying patients to understand their experiences with the project. Interviews were recorded, transcribed verbatim, then analysed using a qualitative descriptive approach.
Setting
21-bed medical surgical ICU in a tertiary care, university-affiliated hospital.
Results
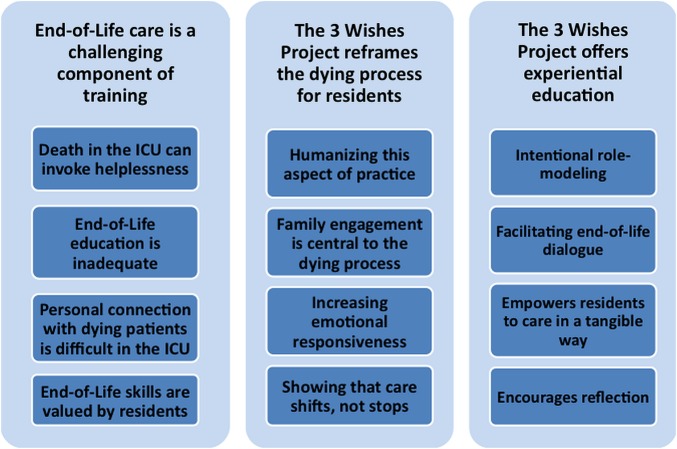
33 residents participated from internal medicine (24, 72.7%), anaesthesia (8, 24.2%) and laboratory medicine (1, 3.0%) programmes in postgraduate years 1–3. 3 categories and associated themes emerged. (1) EOL care is a challenging component of training in that (a) death in the ICU can invoke helplessness, (b) EOL education is inadequate, (c) personal connections with dying patients is difficult in the ICU and (d) EOL skills are valued by residents. (2) The project reframes the dying process for residents by (a) humanising this aspect of practice, (b) identifying that family engagement is central to the dying process, (c) increasing emotional responsiveness and (d) showing that care shifts, not stops. (3) The project offers experiential education by (a) intentional role modelling, (b) facilitating EOL dialogue, (c) empowering residents to care in a tangible way and (d) encouraging reflection.
Conclusions
For residents, the 3 Wishes Project integrated many forms of active learning for residents. Practice-based rather than classroom-based programmes may engage trainees to develop EOL skills transferable to other settings.
Keywords: MEDICAL ETHICS
Strengths and limitations of this study.
This mixed-methods study of resident interviews about an end-of-life project in the intensive care unit used investigator and methodological triangulation.
Residents reported how eliciting and implementing a set of three wishes for dying critically ill patients helped to honour the dying patients.
The 3 Wishes Project helped to reframe the dying process for residents, offering experiential education in end-of-life care.
Residents were mainly from internal medicine and anaesthesia training programmes in one intensive care unit in Canada, so results may not be generalisable to other trainees working in different settings.
Introduction
Residents in training can play an important role providing end-of-life (EOL) care to patients dying in hospital. Although EOL curricula have begun to address the holistic needs of patients and their families, it has also been plagued by a prevailing view that dying patients ‘are not good teaching cases’.1
The intensive care unit (ICU) may be an excellent venue to teach EOL care to residents.2 3
Owing to the high mortality of critical illness, basic and advanced life support is often employed, necessitating discussion about whether, when and how to administer, withhold or withdraw life support in anticipation of death. There are frequent family meetings about the goals of care in the ICU; residents are often participating actively or at least observing such meetings. Residents also tend to care for fewer patients in the ICU than they would on other wards, and do so more consistently, so they come to know the families of critically ill patients, with whom they are more commonly conversing than typically comatose or semicomatose critically ill patients. Nevertheless, a systematic review of residents’ experiences with EOL decision-making suggested the need for more structured teaching and supervision of delivering EOL care to critically ill patients.4 A recent US survey reported that residents wanted to learn more palliative care in the ICU.5
Objectives of this study were to describe residents' experiences with EOL education prior to and during their ICU rotation, and understand the possible influence of a project designed to personalise the dying process for critically ill patients, their families and clinicians. The 3 Wishes Project was developed in January 2013 to bring peace to the final days of a patient's life and ease the grieving process.6
Methods
Design
We conducted this mixed-methods study in a 21-bed closed medical surgical ICU in a tertiary care hospital. When patients or their family members made the decision to withdraw life support in anticipation of death, or if the probability of dying in the ICU as judged by the physician was >95%, patients and families were invited to participate in the 3 Wishes Project. Patients were excluded if they were admitted to ICU for <6 h. We elicited and implemented three wishes from the patient, families or clinicians, to help dignify the patients' death, celebrate a patient's life and foster humanism in practice.6 We documented what the wishes were and whose wishes they were. When introducing the project, our focus was how best to honour the patient; all wishes were for the patient and/or family. We documented when and by whom the wishes were implemented. The wishes focused on ways to honour the patient and were classified into five categories: humanising the environment (eg, favourite flowers, bringing cherished mementos into the room), personal tributes (eg, tea party, tree planting in the patient's name), family reconnections (eg, locating a lost relative, sponsoring a memorial meal), rituals and observances (eg, blessing, renewal of wedding vows, firework display) and ‘paying it forward’ (eg, organ donation, contribution to a charity of significance, unsolicited family donation to this project).
From patients, we collected age, admitting diagnosis, illness severity, process-of-care variables (administration, withdrawal and/or withholding of advanced life support (mechanical ventilation, inotropes/vasopressors, renal replacement therapy, cardiopulmonary resuscitation)) and time of death. We collected basic demographic data on the interview participants.
Aligned with the objectives of this study, this analysis focused on the experiences and perspectives of residents in the 3 Wishes Project with respect to EOL education; residents had completed their medical doctorate degree and were in their first to third postgraduate year of training. This work was performed in the context of conducting semistructured interviews with 1–3 clinicians and at least one family member/patient to understand the impact of the 3 Wishes Project on the experience of the dying process, and their overall perceptions about the project (see online supplementary appendix). Verbal informed consent was obtained from the family (and the patient when possible) for participating in the wishes; written consent was obtained for participating in the interviews.
bmjopen-2015-010626supp_appendix.pdf (87.2KB, pdf)
Analysis
Interviews were digitally recorded, transcribed verbatim and anonymised. Qualitative data were analysed from transcripts using a descriptive approach to generate a summary of study findings, which were then organised and presented using the language of the participants with minimal theoretical interpretation.7 Data were analysed using qualitative content analysis, whereby codes were derived directly from the data rather than preconceived categories.8 Two investigators independently coded 10 initial transcripts, developing a list of codes, which included a general code for all data related to resident education.9 An experienced qualitative researcher coded remaining transcripts. Three investigators reviewed the coding reports of resident interviews on resident education and the impact of the 3 Wishes Project, then three investigators developed more detailed codes. The team met monthly to review the data, organise the codes into meaningful categories and discuss potential relationships among them, referred to as axial coding.9 Coding framework changes were documented in an audit trail.10 Categories of codes were organised into three higher level themes.11 Exemplars from the data were identified for each code and category. N'Vivo (V.10.0; QSR International, Melbourne, Australia) was used for data management and analysis.
Investigator triangulation was achieved through our research team (residents, physicians (critical care and palliative care), a qualitative researcher and a medical student). Methodological triangulation was achieved using a mixed-methods design.12–14 Member checking occurred at a meeting with eight residents who had participated in interviews.
Quantitative data were analysed using descriptive statistics.
Results
Participant characteristics
Overall, 33 (100%) residents agreed to participate. All interviews were conducted in person. Residents were 28.6 (3.4) years old in three core residency programmes: internal medicine (24, 72.7%), anaesthesia (8, 24.2%) and laboratory medicine (1, 3.0%). Baseline characteristics of 50 patients enrolled in the 3 Wishes Project who were cared for by participating residents are in table 1.
Table 1.
Patient characteristics
| Baseline characteristics | |
| Age in years at death, mean (SD) | 67.1 (15.9) |
| Female, n (%) | 23 (46.0) |
| Race, n (%) | |
| White | 44 (88.0) |
| Non-white | 6 (12.0) |
| APACHE II score, mean (SD) | 29.6 (9.3) |
| Location prior to ICU, n (%) | |
| Hospital ward | 21 (42.0) |
| Emergency room | 16 (32.0) |
| Operating room | 1 (2.0) |
| Other hospital—any ward | 11 (22.0) |
| Other (dialysis unit) | 1 (2.0) |
| ICU admitting diagnosis, n (%) | |
| Cardiovascular/vascular | 19 (38.0) |
| Respiratory | 14 (28.00 |
| GI | 6 (12.0) |
| Neurological | 4 (8.0) |
| Sepsis | 6 (12.0) |
| Renal | 1 (2.0) |
| Admission type, n (%) | |
| Medical | 49 (98.0) |
| Surgical | 1 (2.0) |
| On dialysis pre-ICU, n (%) | 10 (20.0) |
| Spiritual belief, n (%) | |
| Catholic | 15 (30.0) |
| Muslim | 2 (4.0) |
| Lutheran | 1 (2.0) |
| Baptist | 4 (8.0) |
| Anglican | 5 (10.0) |
| Agnostic | 7 (14.0) |
| Greek Orthodox | 1 (2.0) |
| Protestant | 2 (4.0) |
| United | 1 (2.0) |
| None | 7 (14.0) |
| Unknown | 5 (10.0) |
| ICU stay | |
| Code status documented on ICU admission, n (%) | |
| Full code | 40 (80.0) |
| No code | 10 (20.0) |
| Advanced life supports administered at any time in ICU, n (%) | |
| Mechanical ventilation | 50 (100.0) |
| Inotropes | 34 (68.0) |
| Dialysis | 21 (42.0) |
| Advanced life supports withdrawn just before death, n (%) | |
| Mechanical ventilation | 33 (66.0) |
| Inotropes | 10 (20.0) |
| Dialysis | 3 (6.0) |
| Advanced life supports withheld, n (%) | |
| Mechanical ventilation | 5 (10.0) |
| Inotropes | 2 (4.0) |
| Dialysis | 10 (20.0) |
| Patient had an explicit wish to die, n (%) | 4 (8.0) |
| Spiritual care consult in ICU, n (%) | 38 (76.0) |
| Palliative care consult in ICU, n (%) | 17 (34.0) |
| Location of death | |
| ICU | 48 (96.0) |
| Emergency room | 1 (2.0) |
| Ward | 1 (2.0) |
| Length of stay | |
| Days from hospital admission to ICU admission, median (IQR) | 0 (0–7) Total range 0–201 |
| Days from ICU admission to death, median (IQR) | 6 (4–13) Total range 0–66 |
| Days from hospital admission to death, median (IQR) | 8 (4–28) Total range 0–209 |
| Days from ICU admission to enrolment in 3 Wishes Program, median (IQR) | 4.5 (2–8) Total range 0–61 |
| Days from enrolment in 3 Wishes Program to death, median (IQR) | 1 (0–2) Total range 0–23 |
| Advanced life support | |
| On mechanical ventilation at any time in ICU, n (%) | 50 (100.0) |
| Duration of mechanical ventilation, median days (IQR) | 6 (5–14) n=50 |
| Received inotropes at any time in ICU, n (%) | 34 (68.0) |
| Duration of receipt of inotropes, median days (IQR) | 4 (2–6) n=34 |
| Patients newly receiving dialysis in ICU (of those who did not receive it prior to ICU), n (%) | 11/40 (27.5) |
| Duration of dialysis in ICU in those newly receiving dialysis in ICU, median days (IQR) | 5 (1–23) n=11 |
In this table, we describe the characteristics of 50 patients enrolled in the 3 Wishes Project cared for by the 33 residents we interviewed.
n=50 patients.
GI, gastrointestinal; ICU, intensive care unit.
Resident characteristics are reported in table 2.
Table 2.
Resident demographics
| Resident demographics (n=33) | |
|---|---|
| Age, mean (SD) | 28.6 (3.4) Total range: 24–40 |
| Sex, n (%) | |
| Female | 16 (48.5) |
| Male | 17 (51.5) |
| Postgraduate year, n (%) | |
| One | 8 (24.2) |
| Two | 7 (21.2) |
| Three | 18 (54.5) |
| Residency training programme, n (%) | |
| Internal medicine | 24 (72.7) |
| Anaesthesia | 8 (24.2) |
| Laboratory medicine | 1 (3.0) |
| Days from patient death to interview, median (IQR) | 6 (4–13) Total range: 1–63 |
| Spiritual affiliation, n (%) | |
| Agnostic | 5 (15.2) |
| Anglican | 1 (3.0) |
| Atheist | 2 (6.1) |
| Catholic | 7 (21.2) |
| Christian | 3 (9.1) |
| Hindu | 1 (3.0) |
| Liberal Buddhist | 1 (3.0) |
| Muslim | 7 (21.2) |
| Spiritual | 1 (3.0) |
| None | 5 (15.2) |
We describe the characteristics of the 33 residents interviewed for the 3 Wishes Project who cared for 50 patients included in this project.
Interviews
Three main themes emerged from resident interviews (figure 1). (1) EOL care is a challenging component of training, (2) the 3 Wishes Project reframes the dying process for residents and (3) the 3 Wishes Project offers experiential education.
Figure 1.
Study findings. In this figure, we present the three themes and categories that emerged from the resident interviews.
EOL care is a challenging component of training
For residents, caring for dying patients is difficult. Optimal encounters require sophisticated, compassionate patient and family communication skills. While trained to be well versed in aetiology, diagnosis, prognosis, treatment and prevention, palliation may not be on equal footing. Residents felt that they lack the requisite knowledge, skills and experience. They explained how EOL care is challenging in that (1) death in the ICU can invoke helplessness, (2) EOL education is inadequate, (3) personal connections with patients dying in the ICU is difficult and (4) EOL skills are valued by residents.
Death in the ICU can invoke helplessness
Residents rotating in the ICU typically use basic and advanced life support to care for patients. Dying patients can induce a sense of inadequacy and despondent feelings about the care being provided.
You don't know if you're doing enough and when you're not sleeping very much, and there's really sick people in all the time, and a lot of the people aren't making it out, it's hard.
I think, sometimes when we're palliating patients, we feel at a loss of what else to do. Like, we can manage their pain but that doesn't address…the soul aching…getting them to that state where…nothing is left unfulfilled…
EOL education is inadequate
Residents felt ill prepared to approach sensitive EOL of issues despite their role as front-line providers.
I don't think residents get much teaching or training in addressing non-medical aspects of end of life care…about the basic things the patient would want, like, who they want to be with…I don't think we're ever reminded…to look beyond those very basic things.
Really, there's not much formal teaching which is really unfortunate because really, we're not prepared for it…I'm an R1, I've been doing it for maybe 7 months and there have been times when I have been the only person there to have these important conversations…it's difficult because you don't really feel you're doing it justice.
Personal connections with dying patients is difficult in the ICU
Traditional demands of critical care can overshadow authentic connections with dying patients, especially given their frequent incapacity. Together, these factors can inhibit therapeutic relationships during the dying process.
ICU is very different from my other rotations because it's the first time that I don't have a connection with the patient… most of the time they're sedated or, you know, on the ventilator. So you don't get to know them as much as a person…
They have all these tubes and lines. It's really hard to actually see them as a human being.
EOL skills are valued by residents
Even though EOL care is so challenging for residents, they declared a desire to develop their own approach to EOL care.
You end up just following other people's…footsteps and…this [project] kind of made me…step back and think, you know, I have to have my own personalized approach.
Residents acknowledged how cultivating palliative care skills matures them as physicians.
It's very important to emphasize earlier on,… at the end of the day, these are the things that mature me … and help me become better day by day…
The 3 Wishes Project reframes the dying process for residents
When focus is turned away from life-saving treatments in the ICU, trainees may assume that opportunities for learning and caring are over. The 3 Wishes Project helped to illustrate that patient centredness remained paramount, and that opportunities for personal and professional development abound when patients are dying. Residents found that an active approach to EOL care via the 3 Wishes Project reframes the dying process by (1) humanising this aspect of practice, (2) identifying the central role of family engagement, (3) increasing emotional awareness and (4) showing how care for patients shifts, not stops.
Humanising this aspect of practice
The 3 Wishes Project provided an opportunity to understand who patients are while formally introducing individualised EOL care. The programme brought patient values to the forefront. It allowed residents to identify with their patients as individuals, understanding their personal and social history.
It just serves to highlight or remind us to take a step back and think about why we're doing what we're doing, and think about the family and the patient as people, and not as sort of ‘the clinical problem’ or the collection of symptoms and treatment.
The project really highlighted the patient as a human being and a person first, which was very different from the way that I, unfortunately, approach ICU patients.
As Francis Peabody commented, “One of the essential qualities of the clinician is interest in humanity, for the secret of the care of the patient is in caring for the patient.”15 The project helped residents recognise the patient's life journey—people, events and personal endeavours that should be acknowledged.
I hopefully will be reminded of, next time I'm dealing with a patient that's dying is to take a step back and remember that outside of the clinical context they have, a very complex, rich life that I'm not really appreciating.
We're so medicalized that, you know, you kind of dehumanize the whole process but this kind of brought that all into perspective that this person- he lived a life, he enjoyed something—music, and that music's playing at his bedside, and it kind of put a different twist on things altogether.
Family engagement is central to the dying process
The 3 Wishes Project helped to give families a voice and underscored the importance of family-centred care.
It showed me how interaction with the family, getting to know what the patient would want, making patients as comfortable as they can be and the family as comfortable as they can be, can really make a difference when people do pass away.
They [the family] came out with such appreciation for what we had done for their father at time of death…I thought that was a huge impact for such a small amount of effort from our part, [that it] could make such a big impact on them and also on us…
Increasing emotional responsiveness
Concerns arise that residents' ability to empathise may decrease over time due to insufficient EOL training, inadequate feedback and psychic defences.16 After experiencing this project, residents wondered if they may be more able to respond to emotional cues, avoiding detachment in difficult encounters.
You take these things forward and you hope to be a better clinician…a more empathetic, more sympathetic clinician, from dealing with these situations.
I think, as part of our training, maybe we kind of put up barriers just to protect ourselves from becoming too involved in…that sort of thing and, I mean, it's always good to get a reminder that, you know, maybe don't build those walls too high.
Showing that care shifts, not stops
The project symbolised a transition from the traditional orientation of critical care towards the palliative approach.
It almost becomes a shift of focus in the medical care that we're providing and focusing on the spiritual or psycho-social component of things rather then medicalizing the process of dying.
I think that it really does do a good job outlining that transition between provision of intensive care to the palliation and support during that end-of-life period, whenever that decision is made….we never actually stop caring for people. We just maybe refocus on what the goals are, and emphasize different things.
The project shifted the mindset of residents towards a more holistic approach to EOL care.
We're always so focused on saving the patient and I think that as a physician…we think that we failed if that didn't happen…Maybe that's why end of life is hard or difficult…[the 3 Wishes Project] bridges it for the physician to realize that you haven't failed. There are different types of care and things that you can provide that are still important to patients.
Sometimes we treat those numbers whereas maybe if we…focused more on what the end game is in terms of ensuring that the patients are comfortable…and ensuring that their dignity is kept intact…And I think in Mrs. X's instance, that was really something that we were able to accomplish because of early identification of her wishes and really striving to make sure that we were respecting them…
The 3 Wishes Project offers experiential education
Experiential education in this context is active and interactive rather than passive. It was designed to engage learners in practical aspects of care, with deliberate personal introspection to process what has occurred. Medical training incorporates formal, didactic, knowledge-based teaching, combined with experiential learning. The 3 Wishes Project offers experiential education consistent with the apprenticeship model of postgraduate training, by (1) intentional role modelling, (2) facilitating EOL dialogue, (3) empowering residents to care in a tangible way and (4) encouraging reflection.
Intentional role modelling
Residents often learn communication skills by the ‘watch and then do’ approach rather than through constructive faculty feedback.17 Observing experienced physicians using refined communication techniques to navigate difficult discussions was useful.
You kind of just try to absorb as much as you can and learn from the body language that you see other people use, and the words that other people use.
The 3 Wishes Project provided residents with intentional role modelling and hands-on EOL care.
This was different than..lectures and having little group sessions…those were artificial…you have to sit around every Tuesday morning and discuss, you know, patient emotions and things like that…it was forced and nobody liked it. It didn't really hit home at any point.
Participation provided tangible examples of the ‘hidden curriculum’—fundamentals of caring for patients which cannot be learnt by reading.18
These are important aspects for caring for critically ill patients that you wouldn't learn if the staff didn't take the time to teach you…by getting involved in this project.
Facilitating EOL dialogue
Standardised tools and tactics have been developed to help physicians in training deliver bad news, or review advanced directives.19 The 3 Wishes Project provided an opportunity to initiate EOL conversations and develop a personal approach to difficult discussions.
Having the program facilitated the kind of conversations that I felt I wasn't really equipped to have or to naturally bring up, but through saying, you know, ‘We have this program and we'd like to help you’ and then having them bring things in the room and having certain other things happen …So, the program actually kind of facilitates that discussion, in some ways makes it more normal, makes it easier to do it.
I think, as a junior clinician, our focus right now is getting better at the medical expert role, and a lot of the other stuff falls by the wayside. I think the 3 Wishes program could…sort of segue to the larger topic of what to say to patients at the end, how to say it, how to interact with the family.
Empowers residents to care in a tangible way
Engagement in the project exposed residents to various strategies that may ease the dying process.
Hey, there's a lot more that you can do for a patient. If…a patient's family really wants coffee, why can't I just go downstairs and get them coffee…I had to line up [to get the coffee for a family] for the 3 Wishes program for, like 20 minutes, and damn it, it felt good lining up for 20 minutes because I felt like I made a difference.
This realisation empowered and encouraged residents to think outside the box, and learn some practical, simple approaches to help patients and families.
This allows you to maybe actually be able to do something positive in a sad situation. It gives you a little power back in the sense that you can help in some way, even if it's small…try and help the family and patient cope with kind of what's happening….just seeing Dr. X give [the flowers] to the family, it felt like we were…seeing, something tangible that you're giving and doing.
Encourages reflection
The interview process allowed residents to reflect on their experience, identifying how their care may have benefited not only patients, but families as well.
I feel like there's a recorder here and you're interviewing me and you're hearing me out just the same way we are hearing out patients, and I feel good just talking about my experience. I can't imagine how a patient or a family who's going through a lot feels when a physician who they know has a lot of duties to fulfill is spending the time with them, so, the fact that we're listened to makes us feel better and I feel better by just talking and reflecting about all of this.
As is used in the operating room, the value of a debriefing process was identified as providing closure and an opportunity for cathartic reflections.
I mean it's nice, this actually kind of helps you get a little bit more closure in a sense because you get to talk about going through something like that, which we don't normally [do].
Discussion
This study of resident perspectives in the ICU setting highlighted that EOL care is a challenging yet crucial component of training. Residents reported that EOL education is inadequate, consistent with Sullivan's national US survey documenting that the majority of internal medicine, family medicine and surgery residents report no formal training in EOL care.20 Residents reported that the format of some EOL education is similar to teaching about disease processes, whereas gaining experience may be as important as gaining knowledge when it comes to palliative care.
Practical exposure to EOL care in the 3 Wishes Project was perceived as a way to develop and display positive attitudes about palliation. This ‘hidden curriculum’ can influence trainees—a phenomenon whereby students learn a great deal through experiential learning that is not part of the official curriculum,18 creating physicians who value EOL knowledge and skills3 in their practice. In one study, involvement of residents in family meetings was the only variable affecting resident confidence with EOL care.21 Observing expert role models and proceeding towards supervised responsibility, leading family discussions and receiving feedback may be as or more effective than didactic teaching. Recommendations for EOL education in a recent consensus statement included case-based, patient-centred education and opportunities to observe more senior physicians, then lead family discussions.22 During our member checking exercise more than 1 year after exposure to this project, residents reported how their involvement made them more comfortable in subsequent rotations in other settings, as they had developed transferable skills.
Educational approaches incorporating storytelling, such as the reflective interview component of this project, allow expressions of feelings, doubts and opinions, and may foster personal and emotional learning in critical care.23 The opportunity for trainees to engage emotionally with patients is especially important; indeed, others have highlighted compassion as the top attribute among excellent critical care physicians.24 Stimulating self-awareness and a deeper understanding of suffering and the human condition are a hallmark of the experiential learning promoted by this project. Residents also witnessed or facilitated wishes that were culturally sensitive such as family chanting of African tribal music on a patient's deathbed and traditional faith healer rituals, while avoiding assumptions about ‘Western’ healthcare practices.
Research in EOL education is emerging. A communication workshop featuring a short didactic session, and simulated family meetings, was evaluated by 51 subspecialty trainees. Their ethical and legal knowledge, and comfort scores improved significantly, and communication scores tended to improve over the workshop. A year later, participants believed it had prepared them for communication challenges in training and practice.25 Hope et al described a communication skills programme for 31 ICU fellows exposed to a 1 month didactic curriculum, with topics related to palliative care, communication and bioethics, combined with four simulation communication cases. Fellows improved with verbalising an agenda for the meeting, summarising for patients and providing a follow-up plan. More than 95% reported feeling more comfortable discussing foregoing life-sustaining treatments and leading family discussions.26 Similarly, McCallister et al27 demonstrated that fellows exposed to a 1-year communication programme versus those who did not have improved communication skills and more self-confidence with family meetings. However, in a randomised trial of internal medicine residents and nurse practitioners allocated to an eight simulation-based communication skills intervention versus ‘usual education’, the former did not improve communication about EOL care, but was associated with a small increase in patients' depressive symptoms.28 Interestingly, in a study of narrative storytelling about level-of-care decision making by 19 ICU fellows, the most common sentiment was a desire to respect patients' wishes23—a fundamental goal of the 3 Wishes Project.6
When the limits of medical interventions for critically ill patients are reached, or when care delivered is inconsistent with patient values, we should ensure that patients' wishes, goals and dignity are respected. Traditional educational focus in the ICU is understanding pathophysiology, resuscitation and technical skills. However, for dying patients it is the art of engaging with our patients and families, understanding their wishes and showing compassion and empathy that require heightened attention. The 3 Wishes Project demonstrates how expert ICU physicians who incorporate these tenets into EOL care could enhance the training of young physicians to develop these essential skills and attributes.
Strengths of our study include the concrete example of an EOL intervention embedded in an ICU rotation. Reflecting real-life practice, rotating residents had a range of critical care experience, variable knowledge of the programme and patient (some attended family meetings while all attended rounds on the patients). After being interviewed, three residents became investigators, involved in analysing and interpreting data. The project exposed residents to an interprofessional collaboration29 with non-hierarchical leadership borne of a shared clinical purpose, and valuing shared learnings.
Limitations of our study include the dominant representation of internal medicine and anaesthesia residency programmes. By design, we excluded ICU fellows, medical students, other clinicians and families from this analysis. There was no formal didactic educational component to our study, or follow-up interviews or audits to evaluate the project's long-term impact. This ICU uses periodic ethics debriefing30 but does not use death rounds,31 a family information pamphlet,32 bereavement brochure,32 withdrawal-of-life-support protocol33 or comfort measure order sets34 all of which may influence trainees in the short and long terms. Although EOL demonstration projects fostering patient dignity may change the values and vernacular on a ward, we did not measure this directly. Our results may not be generalisable to other disciplines or centres.
In summary, in this mixed-methods project, we found that residents working in the ICU desire more effective EOL education. The 3 Wishes Project allowed reframing of the dying process, and created opportunity for experiential education. Practice-based rather than classroom-based programmes such as the 3 Wishes Program may facilitate learning and engage residents in developing EOL skills transferable to other settings.
Acknowledgments
The authors are grateful for the compassion of clinicians in the St. Joseph's Healthcare ICU every day. They thank all the residents and others who participated in this project. They appreciate France Clarke for her project management, and Nicole Zytaruk, Feli Toledo, Trudy Rose, Tracey Hand-Breckenridge and Lois Saunders for their help realising several wishes. The authors thank Diana Clancy and Laurel Grainger for transcription assistance. They also thank Dr Robert Sheppard, Dr Graeme Rocker, Dr Daren Heyland and Dr Randy Curtis for helpful comments on this project. They are moved by the family members and friends who donated to the 3 Wishes Project to help other dying patients and grieving families. This work was inspired by the work of the Sisters of St. Joseph in Hamilton.
Footnotes
Twitter: Follow Ahmed Barefah at @barefah
Contributors: JC conceived of the idea, coded some of the data, analysed the qualitative data and drafted the manuscript. MS conceived of the idea, conducted the interviews, coded all of the data, analysed the qualitative data and drafted the manuscript. JD coded some of the data, analysed the qualitative data and edited the manuscript. AB coded some of the data, analysed the qualitative data and edited the manuscript. AB, AW and MS analysed the qualitative data and edited the manuscript. DH-A conducted the quantitative analysis and edited the manuscript. DC conceived of the idea, obtained funding, supervised the project, analysed the qualitative data and drafted the manuscript. All authors approved of the final manuscript.
Funding: This study was peer-review funded by the Hamilton Chapter of the Canadian Intensive Care Foundation, the Canadian Tire Foundation (Hamilton Branch) and the Hamilton Academy of Health Sciences research Organization and several physicians.
Competing interests: None declared.
Ethics approval: Hamilton Integrated Research Ethics Board.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Shalev D. A piece of my mind. A final course. JAMA 2016;315:263–4. 10.1001/jama.2015.17057 [DOI] [PubMed] [Google Scholar]
- 2.Danis M, Federman D, Fins JJ et al. . Incorporating palliative care into critical care education: principles, challenges, and opportunities. Crit Care Med 1999;27:2005–13. 10.1097/00003246-199909000-00047 [DOI] [PubMed] [Google Scholar]
- 3.Curtis JR, Levy MM. Our responsibility for training physicians to understand the effect patient death has on them: the role of the intensivist. Chest 2014;145:932–3. 10.1378/chest.13-2600 [DOI] [PubMed] [Google Scholar]
- 4.Gorman T, Ahern S, Wiseman J et al. . Residents' end-of-life decision making with adult hospitalized patients: a review of the literature. Acad Med 2005;80:622–33. 10.1097/00001888-200507000-00004 [DOI] [PubMed] [Google Scholar]
- 5.Chen E, McCann JJ, Lateef OB. Attitudes toward and experiences in end-of-life care education in the intensive care unit: a survey of resident physicians. Am J Hosp Palliat Med 2015;32:738–44. 10.1177/1049909114539038 [DOI] [PubMed] [Google Scholar]
- 6.Cook DJ, Swinton M, Toledo F et al. . Personalizing death in the intensive care unit: the 3 Wishes Project: a mixed-methods study. Ann Intern Med 2015;163:271–9. 10.7326/M15-0502 [DOI] [PubMed] [Google Scholar]
- 7.Sandelowski M. Whatever happened to qualitative description? Res Nurs Health 2000;23:334–40. [DOI] [PubMed] [Google Scholar]
- 8.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277–88. 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- 9.Strauss A, Corbin J. Basics of qualitative research: grounded theory procedures and techniques. Newbury Park, CA: Sage, 1990:23–32. [Google Scholar]
- 10.Rodgers BL, Cowles KV. The qualitative research audit trail: a complex collection of documentation. Res Nurs Health 1993;16:219–26. 10.1002/nur.4770160309 [DOI] [PubMed] [Google Scholar]
- 11.Patton MQ. Qualitative research and evaluation methods. 3rd edn Thousand Oaks, CA: Sage Publications, 2002. [Google Scholar]
- 12.Mays N, Pope C. Qualitative research in health care: assessing quality in qualitative research. BMJ 2000;320:50–2. 10.1136/bmj.320.7226.50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thurmond VA. The point of triangulation. J Nurs Scholarsh 2001;33:253–8. 10.1111/j.1547-5069.2001.00253.x [DOI] [PubMed] [Google Scholar]
- 14.Giacomini MK, Cook DJ. Users' guides to the medical literature. XXIII. Qualitative research in health care A. Are the results of the study valid? JAMA 2000;284:357–62. 10.1001/jama.284.3.357 [DOI] [PubMed] [Google Scholar]
- 15.Peabody FW. The care of the patient. JAMA 1927;88:877–82. 10.1001/jama.1927.02680380001001 [DOI] [PubMed] [Google Scholar]
- 16.Szmuilowicz E, el-Jawahri A, Chiappetta L et al. . Improving residents' end-of-life communication skills with a short retreat: a randomized controlled trial. J Palliat Med 2010;13:439–52. 10.1089/jpm.2009.0262 [DOI] [PubMed] [Google Scholar]
- 17.Siddiqui MF, Holley JL. Residents' practices and perceptions about do not resuscitate orders and pronouncing death: an opportunity for clinical training. Am J Hosp Palliat Care 2011;28:94–7. 10.1177/1049909110374599 [DOI] [PubMed] [Google Scholar]
- 18.Hafferty FW. Beyond curriculum reform: confronting medicine's hidden curriculum. Acad Med 1998;73:403–7. 10.1097/00001888-199804000-00013 [DOI] [PubMed] [Google Scholar]
- 19.Buckman R. Breaking bad news: the S-P-I-K-E-S strategy. Community Oncol 2005;2:138–42. 10.1016/S1548-5315(11)70867-1 [DOI] [Google Scholar]
- 20.Sullivan AM, Lakoma MD, Block SD. The status of medical education in end-of-life care: a national report. J Gen Intern Med 2003;18:685–95. 10.1046/j.1525-1497.2003.21215.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stevens L, Cook DJ, Guyatt G et al. . Education, ethics and end-of-life decisions in the intensive care unit. Crit Care Med 2002;30:290–6. 10.1097/00003246-200202000-00004 [DOI] [PubMed] [Google Scholar]
- 22.Truog RD, Campbell ML, Curtis JR et al. . American Academy of Critical Care Medicine. Recommendations for end-of-life care in the intensive care unit: a consensus statement by the American College [corrected] of Critical Care Medicine. Crit Care Med 2008;36:953–63. 10.1097/CCM.0B013E3181659096 [DOI] [PubMed] [Google Scholar]
- 23.Ahern SP, Doyle TK, Marqui F et al. . Critically ill patients and end-of-life decision-making: the senior medical resident experience. Adv In Health Sci Educ 2012;17:121–36. 10.1007/s10459-011-9306-3 [DOI] [PubMed] [Google Scholar]
- 24.Sprung CL, Cohen R, Marini JJ. The top attributes of excellence of intensive care physicians. Intensive Care Med 2015;41:312–14. 10.1007/s00134-014-3561-8 [DOI] [PubMed] [Google Scholar]
- 25.Downar J, Knickle K, Granton JT et al. . Using standardized family members to teach communication skills and ethical principles to critical care trainees. Crit Care Med 2012;40:1814–9. 10.1097/CCM.0b013e31824e0fb7 [DOI] [PubMed] [Google Scholar]
- 26.Hope AA, Hsieh AJ, Howes JM et al. . Let's talk critical. Development and evaluation of a communication skills training program for critical care fellows. Ann Am Thorac Soc 2015;12:505–11. 10.1513/AnnalsATS.201501-040OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McCallister JW, Gustin JL, Wells-Di Gregorio S et al. . Communication skills training curriculum for pulmonary and critical care fellows. Ann Am Thorac Soc 2015;12:520–5. 10.1513/AnnalsATS.201501-039OC [DOI] [PubMed] [Google Scholar]
- 28.Curtis JR, Back AL, Ford DW et al. . Effect of communication skills training for residents and nurse practitioners on quality of communication with patients with serious illness: a randomized trial. JAMA 2013;310:2271–81. 10.1001/jama.2013.282081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Swinton M, Rose T, Toledo F et al. . Interprofessional collaboration in the ICU: determinants of success in the 3 Wishes Project. Can Crit Care Forum Abstract Book 2015. [Google Scholar]
- 30.Santiago C, Abdool S. Conversations about challenging end-of-life-cases: ethics debriefing in the medical-surgical intensive care unit. Dynamics 2011;22:26–30. [PubMed] [Google Scholar]
- 31.Hough CL, Hudson LD, Salud A et al. . Death rounds: end-of-life discussion among medical residents in the intensive care unit. J Crit Care 2005;20:20–5. 10.1016/j.jcrc.2004.09.006 [DOI] [PubMed] [Google Scholar]
- 32.Lautrette A, Darmon M, Megarbane B et al. . A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med 2007;356:469–78. 10.1056/NEJMoa063446 [DOI] [PubMed] [Google Scholar]
- 33.Treece PD, Engelberg RA, Crowley L et al. . Evaluation of a standardized order form for the withdrawal of life support in the intensive care unit. Crit Care Med 2004;32:1141–8. 10.1097/01.CCM.0000125509.34805.0C [DOI] [PubMed] [Google Scholar]
- 34.Walling AM, Ettner SL, Barry T et al. . Missed opportunities: use of an end-of-life symptom management order protocol among inpatients dying expected deaths. J Palliat Med 2011;14:407–12. 10.1089/jpm.2010.0328 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2015-010626supp_appendix.pdf (87.2KB, pdf)