Abstract
Objectives
Systematic review and meta-analysis on the diagnostic accuracy of temporal artery thermometers (TAT).
Design
Systematic review and meta-analysis. The index test consisted of temperature measurement with TAT. The reference test consisted of an estimation of core temperature.
Participants
Clinical patients as well as healthy participants, with or without fever.
Interventions
Literature search in PubMed, Embase, Cinahl and Web of Science. Three reviewers selected articles for full-text reading after which a further selection was made. Risk of bias was assessed with QUADAS-2. Pooled difference and limits of agreement (LoA) were estimated with an inverse variance weighted approach. Subgroup and sensitivity analyses were performed. Sensitivity and specificity were estimated using hierarchical models. Quality of evidence was assessed according to the GRADE system.
Primary and secondary outcome measures
The primary outcome was measurement accuracy expressed as mean difference ±95% LoA. A secondary outcome was sensitivity and specificity to detect fever. If tympanic thermometers were assessed in the same population as TAT, these results were recorded as well.
Results
37 articles comprising 5026 participants were selected. Pooled difference was -0.19°C (95% LoA −1.16 to 0.77°C), with moderate quality of evidence. Pooled sensitivity was 0.72 (95% CI 0.61 to 0.81) with a specificity of 0.94 (95% CI 0.87 to 0.97). The subgroup analysis revealed a trend towards underestimation of the temperature for febrile patients. There was a large heterogeneity among included studies with wide LoA which reduced the quality of evidence.
Conclusions
TAT is not sufficiently accurate to replace one of the reference methods such as rectal, bladder or more invasive temperature measurement methods. The results are, however, similar to those with tympanic thermometers, both in our meta-analysis and when compared with others. Thus, it seems that TAT could replace tympanic thermometers with the caveat that both methods are inaccurate.
Trial registration number
CRD42014008832.
Keywords: INFECTIOUS DISEASES, INTERNAL MEDICINE, PRIMARY CARE
Strengths and limitations of this study.
With 37 studies and 5026 study participants, this is the largest summary of the evidence for temperature measurements at the temporal artery.
The sensitivity analysis did not change the overall result notably.
A weakness is the large heterogeneity among included studies.
Introduction
Body temperature is one of the most commonly used parameters in healthcare. For this, reliable equipment must be used. There is no universal agreement on how accurate a thermometer must be, but the method is generally considered accurate and reliable if the mean difference is less than 0.2 to 0.5°C and the limits of agreement (LoA) are less than ±0.5°C.1–3 Reference methods for temperature measurement have traditionally been rather invasive with measurements taken from the nasopharynx, oesophagus, pulmonary artery, brain or urinary bladder. There is thus a need to find a less invasive method for body temperature measurement as a replacement for the ‘reference’ methods.
Temperature measurement over the temporal artery (TAT, temporal artery thermometry) is a method for temperature measurement that uses infrared technology to detect the heat that is radiated from the skin surface over the temporal artery.
For many years, rectal measurements have been used as the clinical reference method with an acceptable balance between accuracy and degree of invasiveness. Recently, it has to a large degree been replaced by infrared ear thermometry, measuring at the tympanic membrane. However, this method is regarded as suboptimal, mainly because of poor repeatability and a tendency to show false low results compared with core temperature.4–6
Previous literature reports have given mixed results of the value of TAT, and there are no recent systematic reviews of the method. The purpose was thus to perform a systematic literature review and meta-analysis of the measurement accuracy of TAT compared with reference temperature. A secondary aim was to compare the accuracy of TAT and tympanic temperature measurement when both temperatures were measured on the same samples.
The study was designed as a systematic review.
Method and materials
This systematic review has been registered in the PROSPERO International prospective register of systematic reviews (http://www.crd.york.ac.uk/PROSPERO), CRD42014008832.
Study identification
A literature search was performed by a librarian in the electronic databases PubMed/MEDLINE (search string “(temporal artery) AND (((temperature) OR thermometer) OR fever)”), Embase, Cinahl, Web of Science, The Cochrane Library, Trip, International Network of Agencies for Health Technology Assessment (INAHTA) and Centre for Reviews and Dissemination (CRD). Ongoing studies were searched via ClinicalTrials.gov. Reference lists of included studies were checked. The paper is based on the systematic search of literature published up to 29 September 2015.
Study selection and quality assessment
Three reviewers read all titles and abstracts independently. Obviously irrelevant articles were removed, whereas the full text of the potentially relevant articles was retrieved and assessed on the basis of the eligibility criteria for the inclusion in the current review. Disagreements were solved in consensus.
For selecting a study, all of these inclusion criteria should be fulfilled: (A) primary study; (B) temperature measurement at the temporal artery; (C) comparison with core temperature; (D) study performed in a healthcare setting. Exclusion criteria were (A) non-human studies; (B) review articles, editorials, letter or congress abstracts; (C) insufficient data to report or calculate bias or sensitivity/specificity; (D) language other than English, French, German or one of the Nordic languages.
The subject matter was delimited according to PICO7 (population—intervention (index test)—comparison (reference test)—outcome) to clinical patients as well as healthy participants, with or without fever. The index test consisted of temperature measurement with TAT. The reference test consisted of an estimation of reference temperature, expressed as measurement in the nasopharynx, oesophagus, pulmonary artery, rectum, brain and urinary bladder. However, participants received verification with the same reference standard within each study.
All included studies were assessed for methodological quality by three independent reviewers according to QUADAS-2.8 Disagreements were solved in consensus. Most focus was laid on the domain Flow and Timing since the timing between temperature measurements was deemed to be the most crucial part. The process of recording the temperature consisted simply of recording a figure, so blinding was not deemed to be as important.
Outcomes
The primary outcome was measurement accuracy of the index test compared to a reference standard, expressed as pooled estimates of mean temperature difference (systematic error) and 95% LoA (random error). The secondary outcome was average summary estimates of test sensitivity (SE) and specificity (SP) at a chosen test threshold. If tympanic thermometers had been assessed in the same population as the TAT, these results were recorded as well.
Data extraction
Two reviewers independently extracted the relevant data and resolved disagreements through discussion with other reviewers.
From each included study, we retrieved information on study and patient characteristics, type of the index test thermometer, reference standard and information on comparator test, if available, and relevant statistics: mean difference (TAT—reference) and SD of the differences in temperature readings. Mean differences and SD reported in Fahrenheit were converted into Celsius. When mean differences and/or SD of the differences were not directly reported, we computed them from other reported data using standard formulae. Thus, SD of the mean difference was computed from CIs, range of differences, SD for each thermometer and the correlation coefficient, or mean difference and t-statistic. In one study, the mean difference and SD were estimated after extracting individual values from the figures. When possible, we also extracted paired estimates of sensitivity and specificity.
Data analysis
Mean difference in temperature readings
To obtain pooled estimates of systematic error (bias) and random error (LoA), we used the inverse variance weighted approach to combine individual study estimates of the mean difference and SD. More details on the techniques used in this meta-analysis can be found in Williamson et al.9
Pooled estimates of the differences and limits of agreement were calculated using a random-effects approach.10
To explore possible reasons for heterogeneity, we performed subgroup analyses. We hypothesised a priori that age, type of thermometer, presence/absence of fever and reference standard may be sources of heterogeneity across studies, and performed subgroup meta-analyses according to these characteristics where sufficient data were available.
Several sensitivity analyses were performed in various combinations excluding studies with a high risk of bias (in the domain Flow and Timing); studies that used replicated data in pairs using differences for each pair of measurements and did not provide information on how they accounted for within-person correlation of observations11; or studies lacking information on whether SD of the difference was corrected,11 12 when means of repeated measurements by each of the two methods on the same participant were used to evaluate the agreement between the two methods (see online supplementary appendix for details).
bmjopen-2015-009509supp_appendix.pdf (77.2KB, pdf)
Sensitivity and specificity
We used coupled forest plots and a summary receiver operating characteristics (sROC) plot to display SE and SP estimates from individual studies, and obtained average summary estimates of SE and SP from studies that reported results at selected common positivity thresholds (t≥38.0°C) using bivariate random-effects meta-analysis.13 The bivariate model jointly analyses pairs of SE and SP to account for the patterns of correlation between the two measures. To check the robustness of the results, we performed sensitivity analysis by excluding influential studies and outliers. We used Cook's distance to identify influential studies and standardised level-2 residuals to identify outliers.14 15 We did not investigate publication bias, since standard tests for publication bias are not recommended in meta-analysis of diagnostic accuracy studies.16
Statistical analysis was performed using Stata 12/SE, including the user written programmes.14 15 A Stata programme, has been written incorporating formulae described in Williamson et al9 to obtain the pooled estimate of systematic error and LoA utilising random-effects methods.
Quality of evidence (GRADE)
We assessed the quality of evidence for the estimation of pooled difference and LoA according to the GRADE system taking into account risk of bias, consistency, directness, precision and publication bias.17
Health economy
A simplified health economic assessment was performed, comparing TAT and tympanic measurements. The time for performing measurements was assumed to be equal for the two thermometers.3
Results
The literature search resulted in 626 hits. Another 27 articles were added after a manual search of reference lists. After duplicate removal, 558 articles remained. Of these, 97 articles were selected for full-text reading. Thirty-seven of these fulfilled the inclusion and exclusion criteria and were selected for final analysis. Of these, the decision was unanimous in 34 cases. Two reviewers agreed on two cases, and in the final included case only one reviewer initially advocated inclusion. The selection process is shown in figure 1. Study characteristics are shown in table 1.
Figure 1.

Study flow diagram.
Table 1.
Study characteristics of the 37 included studies
| Author, year, country | Inclusion criteria | Population | Febrile status | Maximum time between measurements | Temporal artery device* | Reference standard | Other comparison |
|---|---|---|---|---|---|---|---|
| Allegaert 2014, Belgium18 | Children admitted to paediatric wards | 294, median age 3.2 years, range 0–17 years | Febrile and afebrile | 5 min | TAT-5000 | Rectal temperature (Filac 3000, Covidien, Mechelen, Belgium) | Tympanic (AccuSystem Genius2 Tympanic Infrared Ear Thermometer, Covidien, Mechelen, Belgium) |
| Al-Mukhaizeem 2004, Canada19 | Children undergoing elective dental surgery requiring endotracheal tube placement | 80, mean age 45 months (SD 35) | 2 febrile | Unclear | LXTA Temporal scanner (Exergen, Watertown, Massachusetts, USA) | Oesophageal temperature probe (TeleThermometer, YSI Incorporated, USA) | |
| Bahorski 2012, USA20 | Infants and children presenting in emergency centre, ICU and outpatient unit | 47, 43% male, age 3 to 36 months | Febrile (47%) and afebrile | Rapid sequential manner | TAT-5000 | Rectal temperature (Welch-Allyn) | |
| Batra 2013, India21 | Children 2–12 years, emergency room setting | 50 febrile, mean age 6.1 years, 48% male. 50 afebrile, mean age 6.15 years, 60% male | 50 febrile and 50 afebrile | Unclear | Exergen TAT-2000C (Exergen) | Rectal temperature, mercury thermometer (Hicks Thermometers, Aligarh, India) | Axillary, tympanic (EQ ET 99, Equinox Overseas Private, New Delhi, India) |
| Callanan 2003, USA22 | Infants under 3 months in emergency department | 187 measured with both methods | Afebrile and 23 febrile | Unclear | SensorTouch TA (Exergen) | Rectal temperature (SureTemp, WelchAllyn) | |
| Calonder 2010, USA23 | Adults undergoing surgery | 23, mean age 55.7 years (SD 13.4), 26% male. Two measurements each | Afebrile | 2 min | TAT-5000 | Oesophageal probe (Smiths Medical, Dublin, Ohio, USA) | Oral |
| Carr 2011, USA24 | Inpatients 0–24 months | 40, mean age 10.9 months, 55% male | Febrile | Unclear | TAT-5000 | Rectal temperature (Sure Temp, Welch Allyn Instruments) | |
| Drake-Brockman 2014, Australia25 | Children undergoing general anaesthesia for routine elective non-cardiac surgery | 200, mean age 8.44 years (SD 0.17), 59% male | Unclear | Concurrently | TAT-5000 | Nasopharyngeal temperature (IntelliVue MP800, Philips, Amsterdam, Netherlands) | Skin temperature, tympanic (TermoScan 6021, Braun, Melsungen, Germany) |
| Dybwik 2003, Norway26 | Adult patients in intensive care | 164 | Afebrile and febrile | Unclear | Exergen TAT-4000 (Exergen) | Rectal temperature (Terumo C402) | |
| Furlong 2015, USA27 | Adult patients in cardiac surgical intensive care | 60, mean age 60.8 years (SD 15.2), 68% male | Febrile | Simultaneously | TAT-5000 | Pulmonary artery catheter (Swan-Ganz VIP; Edwards Lifesciences, Irvine, California) | |
| Greenes 2001, USA28 | Infants in emergency department, younger than 1 year | 304 | 36% febrile | Unclear | LXTA Temporal scanner (Exergen) | Rectal temperature (Diatek, Welch Allyn, Skaneateles Falls, New York, USA) | Tympanic (FirstTemp Genius, Sherwood Medical, St Louis, Missouri, USA) |
| Greenes 2004, USA29 | Infants under 1 year in emergency department given an antipyretic drug | 45, mean age 210 days (range 11–335) | All febrile | Unclear | LXTA Temporal scanner (Exergen) | Rectal temperature (Diatek, Welch Allyn, Skaneateles Falls, New York, USA) | |
| Gunawan 2010, Indonesia30 | Neonates more than 24 h old | 134, mean age 36 h (SD 13 h), 52% male | Maximum 37.8°C | Unclear | TAT-5000 | Rectal temperature (Clinical thermometer-CE 0197, China) | |
| Hamilton 2013, Argentina31 | Paediatric inpatients or outpatients | 212, 205 completed study, 58% male | 46% febrile | 5 min | TAT-5000 | Under 5 years rectal, over 5 years oral temperature (SureTemp Plus, Welch Allyn, Skaneateles Falls, New York, USA) | Tympanic (ThermoScan PRO 4000 IR, Braun, Kronberg, Germany) |
| Hebbar 2005, USA1 | Patients in paediatric ICU | 44, mean age 11.5 months (25th–75th percentile 2–34 months) | Afebrile and febrile | Unclear | LXTA Temporal scanner (Exergen) | Pulmonary or rectal temperature (Allegiance Healthcare Corporation, McGaw Park, Illinois, USA) | |
| Holzhauer 2009, USA32 | Children 3–36 months presenting at emergency department | 474 enrolled, 201 febrile included | Afebrile and febrile (42%) | Unclear | Exergen TAT (Exergen) | Rectal temperature (Welch Allyn, New York, USA) | |
| Kimberger 2007, Austria2 | Adult neurosurgical patients | 35 in surgery, mean age 49 years (SD 25), 34% male; 35 in ICU, mean age 58 years (SD 19), 51% male | Afebrile and febrile | Simultaneously | TAT-5000 | Bladder temperature sensor (SmithsMedical, London, UK) | |
| Kirk 2009, UK33 | 16 years or older within 24 h of severe traumatic brain injury | 20, median age 33 years, 80% male | Unclear | Unclear | TAT-5000 | Brain temperature (ICP/temperature probe, Neurovent-PTemp, Raumedic AG, Münchberg, Germany) | Tympanic (Core-Check model 2090, IVAC, San Diego, California, USA) |
| Langham 2009, USA34 | Adult surgical patients | 50, mean age 57 years (SD 14), 48% male | Afebrile and febrile | 5 min | TAT-5000 | Bladder temperature (Foley catheter with thermistor, Mon-a-therm FoleyTemp, Mallinckrodt Anesthesiology, St. Louis, Missouri, USA) | Tympanic (FirstTemp Genius 3000A, Kendall, Mansfield, Massachusetts, USA) |
| Lawson 2007, USA35 | Adult patients in intensive care with pulmonary artery catheter | 60, mean age 57 years (SD 15), 67% male | Afebrile and febrile | 1 min | TAT-5000 | Pulmonary artery Swan-Ganz catheter (Edwards Lifesciences, Irvine, California, USA) | Tympanic (Genius Infrared Tympanic Thermometer 3000A, Sherwood Medical, St Louis, Missouri, USA) |
| Lee 2011, USA36 | Neonatals in intensive care | 34, mean age 35.7 weeks (SD 1.8), 53% male | Afebrile | 2 min | TAT-5000 | Indwelling rectal probe (oesophageal/rectal temperature probe, Smiths Medical ASD, Rockland, Massachusetts, USA) | Axillary |
| Mangat 2010, UK37 | Adult surgical patients | 61, mean age 66 years (SD 14), 75% male | Afebrile | Unclear | TAT-5000 | Nasopharyngeal (Thermistor 400 series 9 Fr, Mallinckrodt, USA) | Tympanic (Genius 2 in core mode, Covidien, Hampshire, USA and PRO4000, Braun, Germany) |
| Moore 2015, USA38 | Children 3 months to 4 years | 239, mean age 1.5 years (SD 0.77), 53% male | 41% febrile | ‘Immediately following’ | Temporal scanner (Exergen) | Rectal (Alaris Medical Sciences, San Diego, California, USA) | |
| Myny 2005, Belgium39 | Orally intubated patients in ICU | 57, mean age 60 years (SD 14.9), 60% male | Afebrile and febrile | 3 min | LXTA Temporal scanner (Exergen) | Pulmonal artery catheter (Baxter Health Care, Irvine, USA) | |
| Nimah 2006, USA40 | Children under 7 years in intensive care | 36, mean age 20.0 months (SD 18.6 months), 58% male | 51% febrile | In a rapid manner (unclear) | SensorTouch HF370 (Philips, Chicago, Illinois, USA) | Bladder temperature (RSP Foley Catheter with 400 Series thermistor, Respiratory Support Products Inc, San Diego, California, USA) | Tympanic (Thermoscan IRT 3020 and IRT 3520, Braun, Kronberg, Germany) |
| Odinaka 2014, Nigeria41 | Children under 5 years in emergency department | 156, mean age 10.8 months (SD 13.6), 52% male | Afebrile and febrile (51%) | Simultaneously | Exergen TAT-2000C (Exergen) | Rectal (mercury in glass) | |
| Penning 2011, Netherlands42 | Children 0–18 years | 198, mean age 5.1 years (SD 4.7), 61% male | Afebrile and febrile (41%) | Max 15 min after rectal | TAT-5000 | Rectal temperature (Terumo C402/C202, Terumo, Tokyo, Japan) | |
| Reynolds 2014, USA43 | Children under 4 years admitted to emergency department | 52, mean age 13.5 months (SD 8.0), 60% male. | Febrile (15%) and afebrile | Unclear | TAT-5000 | Rectal temperature (Sure Temp Plus 690, Welch Allyn, Skaneateles Falls, New York, USA) | Axillary temperature |
| Rubia-Rubia 2011, Spain44 | Patients over 18 years old admitted to intensive care | 201, mean age 59 years (SD 11), 74% male | Afebrile and febrile | Simultaneously | ThermoTouch Baby (Chicco, Grandate, Italy) | Pulmonary artery catheter | Infrared ear thermometer |
| Sahin 2012, Turkey45 | Children who underwent elective lower abdominal surgery | 60, mean age 1.84 years (SD 1.17), 45% male | Afebrile | 5 min | PlusMRD Infrared Temporal Artery Thermometer (pM 1–802, PlusMED, Istanbul, Turkey) | Nasopharyngeal temperature (GE Datex-Ohmeda S/5, Datex-Ohmeda, Madison, Wisconsin, USA) | Axillary mercury-glass thermometer |
| Schuh 2004, Canada46 | Children under 24 months in emergency department | 327, mean age 9.2 months (SD 6.8) | Afebrile and febrile | Unclear | LXTA Temporal scanner (Exergen) | Rectal temperature (IVAC 2000, ALARIS Medical Systems, San Diego, California, USA) | |
| Siberry 2002, USA47 | Children up to 2 years presenting for acute care visit | 275, mean age 11.2 months (range 0–24), 49% male | Afebrile and febrile | Unclear | LXTA Temporal scanner (Exergen) | Rectal temperature (SureTemp, WelchAllyn) | |
| Singler 2013, Germany48 | Patients ≥75 years in an emergency department | 427 patients, mean age 82.7±5.1 years, 159 (37%) male | 67 (15.7%) febrile | Unclear | TAT-5000 | Rectal temperature (IVAC TEMP PLUS II Model 2080) | Tympanic (Braun Thermoscan ear thermometer) |
| Stelfox 2010, Canada49 | Adults in intensive care | 14, mean age 51 years (SD 18), 36% male | Afebrile and febrile | Rapid sequential manner | TAT-5000 | Bladder temperature (Foley Catheter temperature Sensor, Smiths Group, Rockland, USA) | |
| Suleman 2002, USA50 | Adult and paediatric patients recovering from cardiopulmonary bypass | 56, 30 adults (56±15 years old) and 26 children (3±4 years old). 15+16 febrile of these selected | Febrile | Simultaneously | SensorTouch (Philips) | Pulmonary catheter in adults and bladder catheter in children | |
| Teran 2012, Bolivia51 | Children in ER and inpatient unit, 1 to 48 months | 434, mean age 14.6 months, SD 10.7. 48% male | 167 (38%) febrile | 15 s | Exergen TAT-2000C | Rectal temperature (glass mercury thermometer) | |
| Winslow 2012, USA52 | Convenience sample with scheduled surgery over 18 years | 64, mean age 57 years (33% male) | Afebrile | – | TAT-5000 | Bladder temperature (Bardex Lubricath 400-Series and Lubri-Sil Foley Catheter, Bard, Covington, Georgia, USA) |
*TAT-5000: Exergen TemporalScanner TAT-5000 (Exergen, Watertown, Massachusetts, USA).
TAT, temporal artery thermometers.
A literature search in The Cochrane Library resulted in six hits, including two primary studies, of which one was included via the primary search.1 The search of ClinicalTrials.gov resulted in nine studies, of which seven were completed, one cancelled and one awaiting start of recruitment. One of the completed studies has been published.48 The search of the Trip database contributed nothing new while CRD gave three reviews but no new primary studies.
Risk of bias
The risk of bias and applicability concerns are summarised in figure 2. In general, the patient selection consisted of convenience samples that were not consecutive or randomised. Financial support was regarded as a possible source of publication bias. Seven articles reported support by grants from manufacturers.19 28 29 31 40 46 50 Another five studies were supported with instruments from the manufacturers.1 20 22 42 47
Figure 2.

Risk of bias and applicability concerns summary.
Pooled mean difference in temperature readings
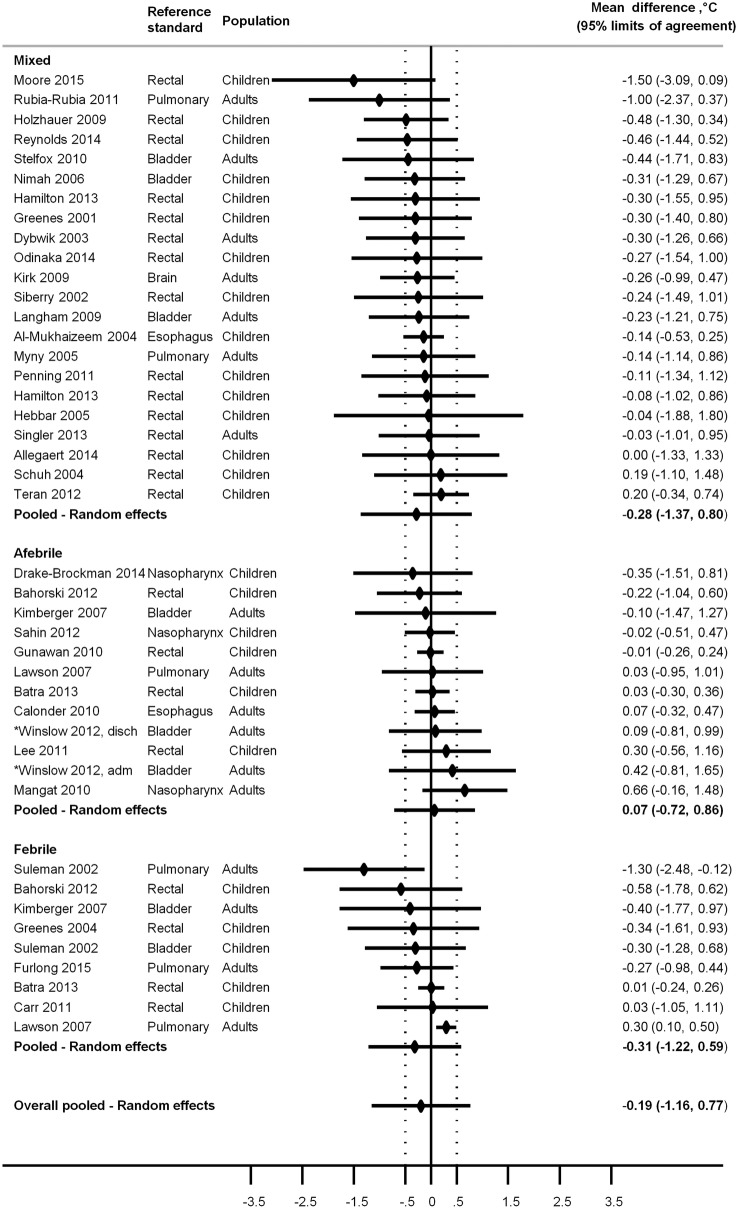
The 37 included articles comprise altogether 5026 study participants, 1301 adults and 3725 children. Thirty-six articles reported mean differences from the reference method, and some provided estimates for different subgroups resulting in 43 comparisons. The overall random-effects pooled mean difference in temperature readings from these 43 comparisons was −0.19°C (95% LoA −1.16 to 0.77°C) (figure 3).
Figure 3.
Mean temperature difference (temporal artery thermometer –reference standard) and 95% limits of agreement by febrile status.
Subgroup and sensitivity analyses
There was a trend towards larger differences from the reference for febrile patients, with an underestimation of the temperature, mean difference −0.31°C (95% LoA −1.22 to 0.59°C), while the afebrile group was closer to the reference, mean difference 0.07°C (95% LoA −0.72 to 0.86°C) (figure 3). The results for adult and children subgroups were almost identical, mean difference −0.20°C (95% LoA −1.17 to 0.76°C) for children and −0.17°C (95% LoA −1.14 to 0.79°C) for adults (table 2). Grouping by reference standard did not show any differences. When grouping by type of TAT, the TAT-5000 thermometer (22 comparisons) had a result similar to all others.
Table 2.
Estimates of the pooled mean difference and 95% LoA between the temporal artery thermometer and reference standard. Random-effects meta-analysis*
| Pooled mean difference, °C (95% limits of agreement) |
Number of comparisons | |
|---|---|---|
| Overall | −0.19 (−1.16 to 0.77) | 43 |
| Subgroup analysis | ||
| Reference standards† | ||
| Rectal | −0.19 (−1.21 to 0.81) | 23 |
| Oesophagus | −0.03 (−0.43 to 0.36) | 2 |
| Bladder | −0.17 (−1.30 to 0.95) | 8 |
| Nasopharynx | 0.09 (−0.73 to 0.91) | 3 |
| Pulmonary artery | −0.40 (−1.30 to 0.51) | 6 |
| Patient factors | ||
| Children | −0.20 (−1.17 to 0.76) | 26 |
| Adults | −0.17 (−1.14 to 0.79) | 17 |
| Febrile status | ||
| Febrile | −0.31 (−1.22 to 0.59) | 9 |
| Afebrile | 0.07 (−0.72 to 0.86) | 12 |
| Mixed | −0.28 (−1.37 to 0.79) | 22 |
| Thermometer factors‡ | ||
| TAT-5000 | −0.10 (−1.09 to 0.89) | 22 |
| Other | −0.27 (−1.23 to 0.67) | 20 |
*Random-effects pooled estimates are calculated according to Williamson et al.9
†One study used the brain.
‡Thermometer type was unclear in one study.
LoA, limits of agreement; TAT, temporal artery thermometers.
Excluding studies with an ‘Unclear’ or ‘High’ risk of bias in the domain Flow and Timing, or studies lacking information on how they dealt with multiple measurements on the same participant, did not change results notably (pooled differences ranging from −0.09 to −0.19°C; see online supplementary appendix for details).
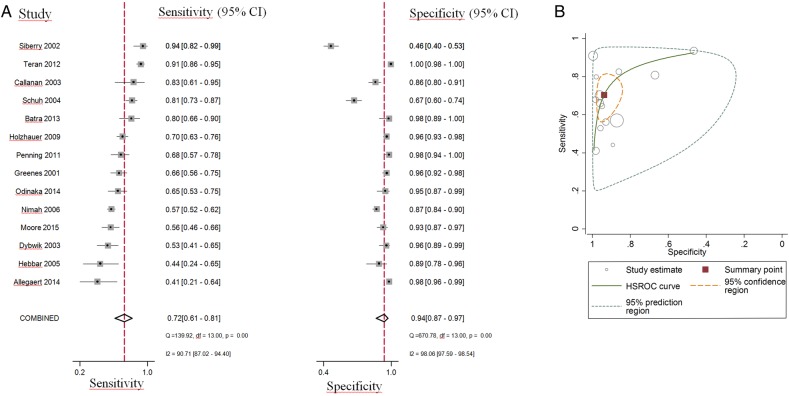
Average summary estimates of SE and SP at the t≥38.0°C cut-off value
Sixteen articles reported data on SE and SP. The SE varied between 0.26 and 0.94 while the SP varied between 0.46 and 1.00. The cut-off for test positivity ranged from t>37.8 to t≥39.0°C.
We pooled the results from 14 studies (1 adult and 13 paediatric) including 1568 participants with fever, and 2566 participants without fever to estimate summary estimates of SE and SP at the t≥38.0°C threshold. The reference test was rectal temperature in 13 studies, and bladder temperature in 1 study. SE and SP estimates and their 95% CI from each of these studies are displayed using coupled forest plots (figure 4A). The sROC plot (figure 4B) shows the 95% confidence and prediction regions. There was substantial heterogeneity for both SE and SP with greater variability in estimated SP than SE across studies. Bivariate random-effects meta-analysis produced the following summary estimates: SE 0.721 (95% CI 0.610 to 0.810), SP 0.939 (95% CI 0.865 to 0.973), positive likelihood ratio 11.8 (95% CI 5.3 to 26.1), and negative likelihood ratio 0.30 (95% CI 0.21 to 0.42). Since most studies had fewer participants with fever than without fever, estimates of SP are more precise than those of SE.
Figure 4.
Accuracy of temperature measurement with a temporal artery thermometer measured through sensitivity and specificity. Pooled estimates obtained by a bivariate random-effects model (A) Coupled forest plot, (B) Summary receiver operating characteristics plot of sensitivity and specificity at t≥38.0°C cut-off value. Each circle shows individual study estimates; inner ellipse represents 95% confidence region, and outer ellipse represents 95% prediction region for a future study.
On the basis of Cook's distance, we found the studies by Teran et al51 and Siberry et al47 to be the most influential in the meta-analysis (in descending order) (figure 5). Of these, Teran et al was identified as an outlier having the highest standardised residuals for SP (figure 5). After refitting the model and leaving this study out, bivariate random-effects meta-analysis produced the following summary estimates: SE 0.690 (95% CI 0.590 to 0.780) and SP 0.92 (95% CI 0.84 to 0.96).
Figure 5.
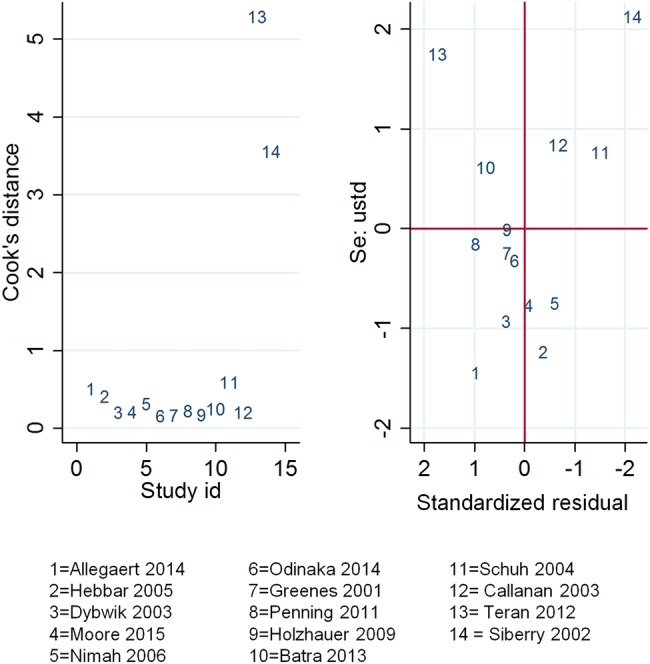
Influential and outlying studies.
Comparison with tympanic thermometers
Eleven articles included comparison with tympanic thermometers in the same population, comprising 1764 participants. In these articles, the mean difference from the reference method for TAT was −0.06°C (95% LoA −0.92 to 0.79°C) and for tympanic thermometers it was −0.29°C (95% LoA −1.15 to 0.57°C).
Four articles reported SE and SP for TAT and tympanic thermometers at the t≥38.0°C threshold in the same population, 734 participants.18 21 28 40 The results were similar with SE 0.70 (95% CI 0.28 to 0.93) and SP 0.99 (95% CI 0.85 to 1.00) for tympanic thermometers.
Quality of evidence (GRADE)
The quality of evidence was graded for the overall result of pooled difference from the reference method with LoA. The quality level was rated down by one point due to inconsistency between the trials (point estimates ranging from −1.50 to 0.66°C). We considered that having support from manufacturers was not enough risk to downgrade on publication bias. This resulted in a moderate evidence quality (⊕⊕⊕O) for a 95% LoA of −1.16 to 0.77°C (table 3).
Table 3.
GRADE evidence profile
| Factors that may decrease quality of evidence |
Test property (95% limits of agreement) | Quality of evidence (GRADE) | ||||||
|---|---|---|---|---|---|---|---|---|
| Test result | Study design | Risk of bias | Directness | Consistency | Precision | Publication bias | ||
| Point estimate with LoA, overall | Cross-sectional design, 37 studies, 5026 participants (⊕⊕⊕⊕) | 0 | 0 | −1 | 0 | 0 | Pooled difference −0.19°C (−1.16°C to 0.77°C) |
⊕⊕⊕O |
LoA, limits of agreement.
Economic analysis
The local procurement price for the TAT is SEK 4200, and for a tympanic instrument it is SEK 895. For the tympanic instrument, a single-use protective cover is needed. With an interest rate of 2% and an assumed depreciation time of 6 years for the TAT and 4 years for the tympanic instrument, the cost per measurement would be equal at about 1100 measurements per year. For fewer measurements per instrument, the tympanic instrument would be cheaper.
Discussion
The present meta-analysis indicates that TAT has a pooled difference from the reference of −0.19°C with 95% LoA −1.16 to 0.77°C or about ±1.0°C. Common criteria for what is a clinically acceptable deviation from the reference temperature have been reported as LoA less than±0.5°C.1 2 TAT exceeds this level considerably, and it cannot be recommended as a replacement for one of the reference methods. The diagnostic accuracy was, however, very similar when compared with tympanic thermometers in the same participants. The subgroup analysis showed a trend towards lower temperature estimates in febrile patients, which in part may explain the rather low sensitivity of 0.72 and specificity of 0.94. In the literature, the minimum sensitivity acceptable to clinicians has been stated to be 0.9.32 46 47 Except for this, the performance was rather similar regardless of the reference method, adults versus children or type of instrument. The sensitivity analysis did not show any significant influence when we adjusted for study quality or statistical methods in the articles. The risk of bias analysis showed that the study populations were in general highly selected with convenience samples most common. Blinding was almost non-existent but was not judged to be a problem since most instruments give a digital figure that simply has to be recorded without interpretation. The timing between index and reference methods was, however, judged to be important since various parts of the body react differently when temperature is rising or falling.29 The quality of evidence was rated as moderate due to inconsistency between the included studies. Publication bias was difficult to evaluate, which is common in studies on diagnostic accuracy. The annual cost for temperature measurements is not high compared to other aspects of healthcare. The largest influence on cost is probably personnel cost, so an instrument with a long measurement process is probably more expensive than instruments with rapid measurements such as the TAT.
It has been shown that TAT gives less discomfort and pain to children compared with rectal and axillary instruments.24 28 32 36 The rectal thermometer has also been reported to be frightening and psychologically harmful for children and there is always a risk of perforation and infection.53 54 Long-term risks are not known, but rectal temperature measurements could together with other painful, stressful and integrity insulting procedures add to psychological suffering for the child. Another fact in favour of TAT is that the patient does not need to be awake for temperature measurement. If the most important issue is to have high accuracy and repeatability but the method is uncomfortable and integrity insulting, the frequency of temperature measurements should be reduced as much as possible.
The present systematic review is with 37 studies and 5026 study participants the largest summary of the evidence for temperature measurements at the temporal artery. Its strength is that the sensitivity analysis did not change the overall result notably. A weakness is the large heterogeneity among included studies.
Temperature measurements with TAT have been evaluated in a health technology assessment report from Scotland55 where it was considered as not exact enough when compared with a reference standard. A recent meta-analysis by Niven et al56 came to the same conclusion; they, however, included only 12 articles. When comparing with tympanic measurements, the results point in various directions. Barnason et al57 show evidence supporting the use in non-febrile adults and children 3 years and older, with clearer evidence supporting oral temperature measurements. Other reviews found no evidence supporting the use of TAT.58 59 Tympanic thermometer measurements in children have been evaluated in a systematic review and meta-analysis by Zhen et al.6 A pooled difference of 0.22°C (95% LoA −0.44 to 1.30°C) was found compared with reference. They concluded that tympanic measurements cannot replace rectal temperature measurements in these patients. Tympanic measurements have been reported as acceptable in critically ill patients in a systematic review by Jefferies et al,60 but had low sensitivity and high specificity in other systematic reviews.4 61
Our results indicate that TAT is not sufficiently accurate to replace one of the reference methods such as rectal, bladder or more invasive temperature measurement methods. Although inaccurate, the results are similar to those with tympanic thermometers, both in our meta-analysis and when compared with others. Thus, it seems that TAT could replace tympanic thermometers with the caveat that both methods are inaccurate. It is unlikely that further research would alter these conclusions. However, there is a need to find a refined non-invasive thermometer with high accuracy.
Acknowledgments
The authors thank Margareta Landin at the Medical Library at Örebro University who performed the literature search. Lars Hagberg, PhD, performed the health economic analysis. Ronny Carlsson assisted with technical information. Mia Svantesson-Sandberg, PhD, performed the ethical analysis. Monica Hultcrantz, Agneta Pettersson and Pernilla Östlund from the Swedish Council on Health Technology Assessment (SBU) participated in the assessment of methodological quality and in rating the quality of evidence.
Footnotes
Contributors: HG performed the literature search together with a librarian. HG, GL and YN selected articles and assessed the methodological quality. RU performed the statistical analysis. This report was mainly written by HG and was critically reviewed, revised and subsequently approved by all authors.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Hebbar K, Fortenberry JD, Rogers K et al. Comparison of temporal artery thermometer to standard temperature measurements in pediatric intensive care unit patients. Pediatr Crit Care Med 2005;6:557–61. 10.1097/01.PCC.0000163671.69197.16 [DOI] [PubMed] [Google Scholar]
- 2.Kimberger O, Cohen D, Illievich U et al. Temporal artery versus bladder thermometry during perioperative and intensive care unit monitoring. Anesth Analg 2007;105:1042–7. 10.1213/01.ane.0000281927.88935.e0 [DOI] [PubMed] [Google Scholar]
- 3.Ng KPM, FR, Heng BH. An evaluation of non-invasive temperature measurement for inpatients: a review of the literature. Health Technology Assessment. Singapore: National Healthcare Group, 2007:1–15. [Google Scholar]
- 4.Dodd SR, Lancaster GA, Craig JV et al. In a systematic review, infrared ear thermometry for fever diagnosis in children finds poor sensitivity. J Clin Epidemiol 2006;59:354–7. 10.1016/j.jclinepi.2005.10.004 [DOI] [PubMed] [Google Scholar]
- 5.Huggins R, Glaviano N, Negishi N et al. Comparison of rectal and aural core body temperature thermometry in hyperthermic, exercising individuals: a meta-analysis. J Athl Train 2012;47:329–38. 10.4085/1062-6050-47.3.09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhen C, Xia Z, Long L et al. Accuracy of infrared ear thermometry in children: a meta-analysis and systematic review. Clin Pediatr (Phila) 2014;53:1158–65. 10.1177/0009922814536774 [DOI] [PubMed] [Google Scholar]
- 7.Higgins J, Green S, eds. Cochrane handbook for systematic reviews of interventions version 5.1.0. The Cochrane Collaboration, 2011. [Google Scholar]
- 8.Whiting PF, Rutjes AW, Westwood ME et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 2011;155:529–36. 10.7326/0003-4819-155-8-201110180-00009 [DOI] [PubMed] [Google Scholar]
- 9.Williamson PR, Lancaster GA, Craig JV et al. Meta-analysis of method comparison studies. Stat Med 2002;21:2013–25. 10.1002/sim.1158 [DOI] [PubMed] [Google Scholar]
- 10.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177–88. 10.1016/0197-2456(86)90046-2 [DOI] [PubMed] [Google Scholar]
- 11.Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res 1999;8:135–60. 10.1191/096228099673819272 [DOI] [PubMed] [Google Scholar]
- 12.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;1:307–10. 10.1016/S0140-6736(86)90837-8 [DOI] [PubMed] [Google Scholar]
- 13.Reitsma JB, Glas AS, Rutjes AW et al. Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol 2005;58:982–90. 10.1016/j.jclinepi.2005.02.022 [DOI] [PubMed] [Google Scholar]
- 14.Dwamena BA. midas: A program for meta-analytical integration of diagnostic accuracy studies in Stata. Division of Nuclear Medicine, Department of Radiology, University of Michigan Medical School, Ann Arbor, Michigan 2007.
- 15.Harbord RM, Whiting P. metandi: Meta-analysis of diagnostic accuracy using hierarchical logistic regression. Stata J 2009;9:211–29. [Google Scholar]
- 16.Macaskill P, Gatsonis C, Deeks JJ et al. Chapter 10: analysing and presenting results. In: Deeks JJ, Bossuyt PM, Gatsonis C, eds. Cochrane handbook for systematic reviews of diagnostic test accuracy version 1.0. The Cochrane Collaboration, 2010. http://srdta.cochrane.org/ [Google Scholar]
- 17.Guyatt GH, Oxman AD, Kunz R et al. What is “quality of evidence” and why is it important to clinicians? BMJ 2008;336:995–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Allegaert K, Casteels K, van Gorp I et al. Tympanic, infrared skin, and temporal artery scan thermometers compared with rectal measurement in children: a real-life assessment. Curr Ther Res Clin Exp 2014;76:34–8. 10.1016/j.curtheres.2013.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Al-Mukhaizeem F, Allen U, Komar L et al. Comparison of temporal artery, rectal and esophageal core temperatures in children: Results of a pilot study. Paediatr Child Health 2004;9:461–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bahorski J, Repasky T, Ranner D et al. Temperature measurement in pediatrics: a comparison of the rectal method versus the temporal artery method. J Pediatr Nurs 2012;27:243–7. [DOI] [PubMed] [Google Scholar]
- 21.Batra P, Goyal S. Comparison of rectal, axillary, tympanic, and temporal artery thermometry in the pediatric emergency room. Pediatr Emerg Care 2013;29:63–6. 10.1097/PEC.0b013e31827b5427 [DOI] [PubMed] [Google Scholar]
- 22.Callanan D. Detecting fever in young infants: reliability of perceived, pacifier, and temporal artery temperatures in infants younger than 3 months of age. Pediatr Emerg Care 2003;19:240–3. 10.1097/01.pec.0000086231.54586.15 [DOI] [PubMed] [Google Scholar]
- 23.Calonder EM, Sendelbach S, Hodges JS et al. Temperature measurement in patients undergoing colorectal surgery and gynecology surgery: a comparison of esophageal core, temporal artery, and oral methods. J Perianesth Nurs 2010;25:71–8. 10.1016/j.jopan.2010.01.006 [DOI] [PubMed] [Google Scholar]
- 24.Carr EA, Wilmoth ML, Eliades AB et al. Comparison of temporal artery to rectal temperature measurements in children up to 24 months. J Pediatr Nurs 2011;26:179–85. [DOI] [PubMed] [Google Scholar]
- 25.Drake-Brockman TF, Hegarty M, Chambers NA et al. Monitoring temperature in children undergoing anaesthesia: a comparison of methods. Anaesth Intensive Care 2014;42:315–20. [DOI] [PubMed] [Google Scholar]
- 26.Dybwik K, Nielsen EW. [Infrared temporal thermometry]. Tidsskr Nor Laegeforen 2003;123:3025–6. [PubMed] [Google Scholar]
- 27.Furlong D, Carroll DL, Finn C et al. Comparison of temporal to pulmonary artery temperature in febrile patients. Dimens Crit Care Nurs 2015;34:47–52. 10.1097/DCC.0000000000000090 [DOI] [PubMed] [Google Scholar]
- 28.Greenes DS, Fleisher GR. Accuracy of a noninvasive temporal artery thermometer for use in infants. Arch Pediatr Adolesc Med 2001;155:376–81. 10.1001/archpedi.155.3.376 [DOI] [PubMed] [Google Scholar]
- 29.Greenes DS, Fleisher GR. When body temperature changes, does rectal temperature lag? J Pediatr 2004;144:824–6. 10.1016/j.jpeds.2004.02.037 [DOI] [PubMed] [Google Scholar]
- 30.Gunawan M, Soetjiningsih I, Kardana M. Comparison of the accuracy of body temperature measurements with temporal artery thermometer and axillary mercury thermometer in term newborns. Paediatr Indones 2010;50:67–72. [Google Scholar]
- 31.Hamilton PA, Marcos LS, Secic M. Performance of infrared ear and forehead thermometers: a comparative study in 205 febrile and afebrile children. J Clin Nurs 2013;22:2509–18. 10.1111/jocn.12060 [DOI] [PubMed] [Google Scholar]
- 32.Holzhauer JK, Reith V, Sawin KJ et al. Evaluation of temporal artery thermometry in children 3–36 months old. J Spec Pediatr Nurs 2009;14:239–44. 10.1111/j.1744-6155.2009.00204.x [DOI] [PubMed] [Google Scholar]
- 33.Kirk D, Rainey T, Vail A et al. Infra-red thermometry: the reliability of tympanic and temporal artery readings for predicting brain temperature after severe traumatic brain injury. Crit Care 2009;13:R81 10.1186/cc7898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Langham GE, Maheshwari A, Contrera K et al. Noninvasive temperature monitoring in postanesthesia care units. Anesthesiology 2009;111:90–6. 10.1097/ALN.0b013e3181a864ca [DOI] [PubMed] [Google Scholar]
- 35.Lawson L, Bridges EJ, Ballou I et al. Accuracy and precision of noninvasive temperature measurement in adult intensive care patients. Am J Crit Care 2007;16:485–96. [PubMed] [Google Scholar]
- 36.Lee G, Flannery-Bergey D, Randall-Rollins K et al. Accuracy of temporal artery thermometry in neonatal intensive care infants. Adv Neonatal Care 2011;11:62–70. 10.1097/ANC.0b013e3182087d2b [DOI] [PubMed] [Google Scholar]
- 37.Mangat J, Standley T, Prevost A et al. A comparison of technologies used for estimation of body temperature. Physiol Meas 2010;31:1105–18. 10.1088/0967-3334/31/9/003 [DOI] [PubMed] [Google Scholar]
- 38.Moore AH, Carrigan JD, Solomon DM et al. Temporal artery thermometry to detect pediatric fever. Clin Nurs Res 2015;24:556–63. 10.1177/1054773814557481 [DOI] [PubMed] [Google Scholar]
- 39.Myny D, De Waele J, Defloor T et al. Temporal scanner thermometry: a new method of core temperature estimation in ICU patients. Scott Med J 2005;50:15–18. [DOI] [PubMed] [Google Scholar]
- 40.Nimah MM, Bshesh K, Callahan JD et al. Infrared tympanic thermometry in comparison with other temperature measurement techniques in febrile children. Pediatr Crit Care Med 2006;7:48–55. 10.1097/01.PCC.0000185476.35550.B2 [DOI] [PubMed] [Google Scholar]
- 41.Odinaka KK, Edelu BO, Nwolisa CE et al. Temporal artery thermometry in children younger than 5 years: a comparison with rectal thermometry. Pediatr Emerg Care 2014;30:867–70. 10.1097/PEC.0000000000000289 [DOI] [PubMed] [Google Scholar]
- 42.Penning C, van der Linden JH, Tibboel D et al. Is the temporal artery thermometer a reliable instrument for detecting fever in children? J Clin Nurs 2011;20:1632–9. 10.1111/j.1365-2702.2010.03568.x [DOI] [PubMed] [Google Scholar]
- 43.Reynolds M, Bonham L, Gueck M et al. Are temporal artery temperatures accurate enough to replace rectal temperature measurement in pediatric ED patients? J Emerg Nurs 2014;40:46–50. 10.1016/j.jen.2012.07.007 [DOI] [PubMed] [Google Scholar]
- 44.Rubia-Rubia J, Arias A, Sierra A et al. Measurement of body temperature in adult patients: Comparative study of accuracy, reliability and validity of different devices. Int J Nurs Stud 2011;48:872–80. 10.1016/j.ijnurstu.2010.11.003 [DOI] [PubMed] [Google Scholar]
- 45.Sahin SH, Duran R, Sut N et al. Comparison of temporal artery, nasopharyngeal, and axillary temperature measurement during anesthesia in children. J Clin Anesth 2012;24:647–51. 10.1016/j.jclinane.2012.05.003 [DOI] [PubMed] [Google Scholar]
- 46.Schuh S, Komar L, Stephens D et al. Comparison of the temporal artery and rectal thermometry in children in the emergency department. Pediatr Emerg Care 2004;20:736–41. 10.1097/01.pec.0000144915.78124.26 [DOI] [PubMed] [Google Scholar]
- 47.Siberry GK, Diener-West M, Schappell E et al. Comparison of temple temperatures with rectal temperatures in children under two years of age. Clin Pediatr (Phila) 2002;41:405–14. 10.1177/000992280204100605 [DOI] [PubMed] [Google Scholar]
- 48.Singler K, Bertsch T, Heppner HJ et al. Diagnostic accuracy of three different methods of temperature measurement in acutely ill geriatric patients. Age Ageing 2013;42:740–6. 10.1093/ageing/aft121 [DOI] [PubMed] [Google Scholar]
- 49.Stelfox HT, Straus SE, Ghali WA et al. Temporal artery versus bladder thermometry during adult medical-surgical intensive care monitoring: an observational study. BMC Anesthesiol 2010;10:13 10.1186/1471-2253-10-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Suleman MI, Doufas AG, Akça O et al. Insufficiency in a new temporal-artery thermometer for adult and pediatric patients. Anesth Analg 2002;95:67–71. 10.1097/00000539-200207000-00012 [DOI] [PubMed] [Google Scholar]
- 51.Teran CG, Torrez-Llanos J, Teran-Miranda TE et al. Clinical accuracy of a non-contact infrared skin thermometer in paediatric practice. Child Care Health Dev 2012;38:471–6. 10.1111/j.1365-2214.2011.01264.x [DOI] [PubMed] [Google Scholar]
- 52.Winslow EH, Cooper SK, Haws DM et al. Unplanned perioperative hypothermia and agreement between oral, temporal artery, and bladder temperatures in adult major surgery patients. J Perianesth Nurs 2012;27:165–80. 10.1016/j.jopan.2012.01.012 [DOI] [PubMed] [Google Scholar]
- 53.El-Radhi AS, Barry W. Thermometry in paediatric practice. Arch Dis Child 2006;91:351–6. 10.1136/adc.2005.088831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Maxton FJ, Justin L, Gillies D. Estimating core temperature in infants and children after cardiac surgery: a comparison of six methods. J Adv Nurs 2004;45:214–22. 10.1046/j.1365-2648.2003.02883.x [DOI] [PubMed] [Google Scholar]
- 55.Thompson L. What is the clinical and cost effectiveness of temporal artery thermometers compared with infrared in-ear thermometers for temperature measurement in routine clinical practice? Glasgow: Healthcare Improvement Scotland. Technologies scoping report 11. 2012. [Google Scholar]
- 56.Niven DJ, Gaudet JE, Laupland KB et al. Accuracy of peripheral thermometers for estimating temperature: a systematic review and meta-analysis. Ann Intern Med 2015;163:768–77. 10.7326/M15-1150 [DOI] [PubMed] [Google Scholar]
- 57.Barnason S, Williams J, Proehl J et al. Emergency nursing resource: non-invasive temperature measurement in the emergency department. J Emerg Nurs 2012;38:523–30. 10.1016/j.jen.2012.05.012 [DOI] [PubMed] [Google Scholar]
- 58.Bahr SJ, Senica A, Gingras L et al. Clinical nurse specialist-led evaluation of temporal artery thermometers in acute care. Clin Nurse Spec 2010;24:238–44. 10.1097/NUR.0b013e3181ecda4b [DOI] [PubMed] [Google Scholar]
- 59.Hooper VD, Andrews JO. Accuracy of noninvasive core temperature measurement in acutely ill adults: the state of the science. Biol Res Nurs 2006;8:24–34. 10.1177/1099800406289151 [DOI] [PubMed] [Google Scholar]
- 60.Jefferies S, Weatherall M, Young P et al. A systematic review of the accuracy of peripheral thermometry in estimating core temperatures among febrile critically ill patients. Crit Care Resusc 2011;13:194–9. [PubMed] [Google Scholar]
- 61.Holte TO, Vandvik PO, Elvsaas IKÖ et al. Diagnostisk nøyaktighet av øre-, munnhule-, armhule- og pannetermometer sammenliknet med rektaltermometer for å identifisere feber hos voksne pasienter innlagt i sykehus eller sykehjem. Rapport fra Kunnskapssenteret. Oslo: Nasjonalt kunnskapssenter for helsetjenesten, 2009:1–49. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2015-009509supp_appendix.pdf (77.2KB, pdf)