Highlights
-
•
In a prior case series, we noted a sign on CT associated with inguinoscrotal herniation of the ureter.
-
•
In this study, we analyzed all CT urograms performed at our institution over 1 year.
-
•
Deviation of the ureter from the psoas muscle at L4 by >1 cm should raise suspicion for a distal ureteral anomaly.
-
•
Morbid obesity and congenital anomalies may result in a similar imaging appearance.
-
•
Awareness of this anomaly can have significant operative implications.
Keywords: Ureteral herniation, Inguinal hernia, CT urogram, Inguinoscrotal herniation
Abstract
Introduction
An aberrant course of the distal ureter can pose a risk of ureteral injury during surgery for inguinal hernia repair and other groin operations. In a recent case series of inguinoscrotal hernation of the ureter, we found that each affected ureter was markedly anterior to the psoas muscle at its mid-point on abdominal CT. We hypothesized that this abnormality in the abdominal course of the ureter would predict the potentially hazardous aberrant course of the distal ureter.
Presentation of cases
We reviewed all evaluable CT urograms performed at St. Louis University Hospital from June 2012 to July 2013 and measured the ureteral course at several anatomically fixed points.
Discussion
93% (50/54) of ureters deviated by less than 1 cm from the psoas muscle in their mid-course (at the level of the L4 vertebra). Reasons for anterior deviation of the ureter in this study included morbid obesity with prominent retroperitoneal fat, congenital renal abnormality, and post-traumatic renal/retroperitoneal hematoma. We determined that the optimal level on abdominal CT to detect the displaced ureter was the mid-body of the L4 vertebra.
Conclusion
Anterior deviation of the ureter in its mid-course appears to predict inguinoscrotal herniation of the ureter. This finding is a sensitive predictor and should raise concern for this anomaly in the appropriate clinical setting. It is not entirely specific as morbid obesity and congenital anomalies may result in a similar imaging appearance. We believe that this association has not been reported previously. Awareness of this anomaly can have significant operative implications.
1. Introduction
Anomalous descent of the distal ureter into the inguinal canal or scrotum is a rare condition, with approximately 64 cases reported in the English language literature [1]. A recent case series suggests that this is under-reported [2]. Many reported cases were noted at the time of surgical exploration, often for inguinal hernia repair, or later as a result of an operative injury.
In each of our five recent cases, abdominal CT revealed an abnormal location of the affected ureter in its mid-course [2]. Unlike the normal contralateral ureter, which coursed immediately anterior to the psoas muscle at the level of the L4 vertebra, the ureter with the abnormal pelvic course also had an abnormal position at the L4 level, lying in retroperitoneal fat markedly anterior to the psoas muscle. In order to determine whether such deviation of the ureter anterior to the psoas muscle predicts an anomalous course of the distal ureter, we analyzed all CT urograms performed at St. Louis University Hospital over one year.
1.1. Presentation of cases
We obtained all CT urograms performed at St. Louis University Hospital in one year (June 2012–July 2013). These utilized a 3-phase protocol. At the minimum, this included 2 mm thick slices through the abdomen and pelvis prior to the administration of contrast, a nephrographic phase following the intravenous injection of 100 mL of Omnipaque contrast (350 mg of iodine per mL), and 10 min delayed images per the standard protocol at this institution. Studies were excluded from analysis if the ureters could not be identified due to poor opacification with contrast on delayed images, or if the patient had undergone surgery directly affecting the course of a ureter such as complete nephrectomy, cystectomy with urinary diversion, or any other ureteral surgery. After applying these exclusion criteria, the remaining 27 studies were selected for analysis. The ureter typically emerges from the renal hilum at the level of L2 and then courses almost straight downward towards the pelvic brim anterior to the psoas muscle, so this region of the abdominal ureter was felt to be least susceptible to variation. For all the studies, the anteroposterior distance between the ureter and the psoas muscle was measured at the L3-L4 level, the mid L4 level, and the L4-L5 level bilaterally by a radiologist. The greatest of these distances was recorded. The maximal measurements were classified into four categories: 0 mm (if there was no distinguishable fat plane between the mid ureter and psoas muscle), 0–5 mm, 5–10 mm, and greater than 10 mm. For the purposes of this study, the first non-rib-bearing vertebra was designated as L1. The patient’s chart was concurrently reviewed, and information including age, sex, weight, and the reason for the CT urogram was obtained. Of note, the patient’s weight was the weight entered in the patient’s chart at the time of data collection, and not necessarily the weight at the time that the CT urogram was performed; this time difference was up to 1 year in some cases. Body mass index (BMI) was not available for most patients and was therefore not included in the analysis.
2. Discussion
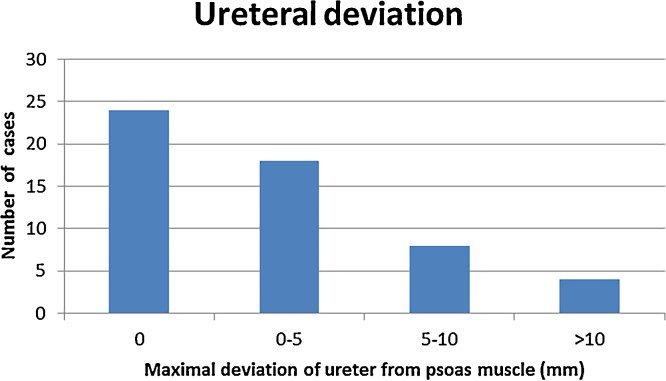
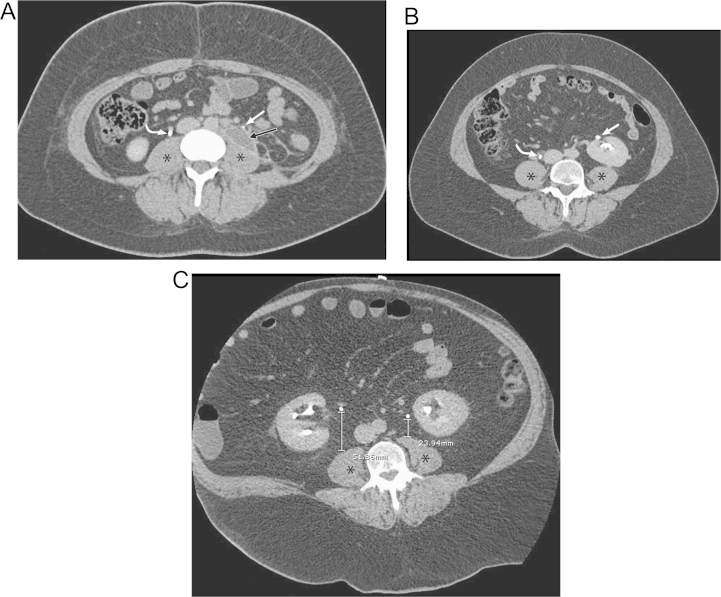
In this series, 93% (50/54) of ureters deviated by less than 1 cm from the psoas muscle in their mid-course, that is, near the level of L4 (Fig. 2 and Table 1, Table 2, Table 3). There was no significant difference in ureteral deviation at the levels of L3–L4, L4, and L4–L5 in these normal patients, so the midpoint of the L4 vertebral body was chosen for reproducibility. There were only 4 ureters (in 3 patients) that deviated by more than 1 cm from the psoas muscle. In the first such patient, the left ureter was separated from the psoas muscle by a 1.5 cm post-traumatic urinoma or hematoma (Fig. 1a). In the second patient, the left kidney was inferiorly located and anteriorly malrotated, likely a congenital ectopic pelvic kidney, with the short left ureter coursing rather abruptly medially into the bladder which resulted in a distance of 2.7 cm between the left ureter and psoas muscle when measured at L4–L5 (Fig. 1b). The third patient was extremely obese, weighing 173 kg (BMI of 48 kg/m2) at the time of data collection, and was the heaviest patient in this study. His right ureter was 5.2 cm anterior to the psoas muscle at L3–L4, although it subsequently traveled posteriorly, with a distance of 1.0 cm at L4–L5. His left ureter was 2.4 cm anterior to the psoas muscle at L3–L4 and 2.2 cm anterior the psoas at L4–L5 (Fig. 1c). Other than morbid obesity with extensive retroureteral fat, this patient had no other anatomic abnormality or genitourinary anomaly to account for the bilateral ureteral deviation. None of the ureters in these patients coursed into the inguinal or scrotal regions.
Fig. 2.
Frequency distribution depicting the maximal deviation of the mid ureter from the ipsilateral psoas muscle at the level of the midpoint of the L4 vertebral body.
Table 1.
Frequency of ureter deviation (right and left combined). Mean weight was also calculated for each category.
| Maximal deviation of ureter from psoas muscle (mm) | Number of cases | Percent | Mean weight (kg) |
|---|---|---|---|
| 0 | 24 | 44% | 78 |
| 0–5 | 18 | 33% | 83 |
| 5–10 | 8 | 15% | 75 |
| >10 | 4 | 7% | 135 |
| Total | 54 |
Table 2.
Frequency of ureter deviation on the right. Mean weight was also calculated for each category.
| Maximal deviation of right ureter from psoas muscle (mm) | Number of cases | Percent | Mean weight (kg) |
|---|---|---|---|
| 0 | 9 | 33% | 78 |
| 0–5 | 11 | 41% | 83 |
| 5–10 | 6 | 22% | 78 |
| >10 | 1 | 4% | 173 |
| Total | 27 |
Table 3.
Frequency of ureter deviation on the left. Mean weight was also calculated for each category.
| Maximal deviation of left ureter from psoas muscle (mm) | Number of cases | Percent | Mean weight (kg) |
|---|---|---|---|
| 0 | 15 | 56% | 78 |
| 0–5 | 7 | 26% | 85 |
| 5–10 | 2 | 7% | 66 |
| >10 | 3 | 11% | 122 |
| Total | 27 |
Fig. 1.
CT urograms showing separation of the ureter from the psoas muscle in patients without inguinal/scrotal hernias.
(a) Post-traumatic fluid collection, likely urinoma or hematoma (black arrow), separating the left ureter (straight white arrow) from the psoas muscle (*) as compared to the normal right ureter (curved white arrow).
(b) Malrotated left kidney resulting in an anteriorly displaced left ureter (straight arrow) as compared to the normal right ureter (curved arrow).
(c) Extreme obesity with abundant retroperitoneal fat resulting in anteroposterior displacement of the right ureter from the psoas muscle (*) by 5.2 cm and the left ureter from the psoas muscle (*) by 2.4 cm at the L4 level.
3. Conclusion
Descent of the ureter into the inguinal canal or scrotum may occur with an inguinal hernia, but is quite rare. Our literature search suggests that approximately 64 cases have been reported [1], although a recent case series of five patients suggests that the prevalence of this anomaly is underestimated [2]. While the “curlicue” sign of a looping ureter has been shown to be pathognomonic for ureteral herniation on X-ray urograms, it is not very sensitive [3]. Our recent case series noted the association between inguinoscrotal ureteral herniation and the finding on abdominal CT that we further describe here.
Our data indicate that deviation of the ureter from the psoas muscle at the level of midpoint of the L4 vertebral body by greater than 1 cm should raise suspicion for a distal ureteral anomaly. This is presumably because the affected ureter is pulled anteriorly starting from the level of the lumbar spine due to the inguinoscrotal hernia. However, this finding is not very specific as morbid obesity may also result in abundant retroperitoneal fat separating the ureter from the ipsilateral psoas muscle. It is reported that obesity is a major risk factor for ureteral herniation [4] and the anterior deviation of the ureters in the morbidly obese patient in our current study supports this radiologically. The occurrence is approximately three to four times more frequent on the right side than the left, probably due to differences in the morphology of the fascia of Toldt [3], [4]. Inguinal hernias containing a ureter have been associated with a large amount of retroperitoneal fat around the ureter, although this has not been quantitatively measured [4]. All inguinoscrotal ureteral herniations in our prior case series occurred in males, presumably because indirect inguinal hernias are much more common in males than females.
If an abdominal CT is available prior to hernia repair, the CT can be utilized to follow the course of the ureters. Marked anterior deviation of a ureter from the psoas muscle in its mid-course should raise concern for inguinoscrotal herniation of the ureter. A dedicated CT urogram is not justifiable before surgery in every patient with an inguinal hernia, but the surgeon should be aware of the possible aberrant course of the distal ureter during inguinal hernia dissection to prevent damage to the ureter, especially when the patient is very obese [5]. Methylene blue can be used intravenously or through a Foley catheter to identify all pertinent structures before complete dissection [6]. Immediate excision of the herniated ureteral loop with re-anastomosis and stenting is probably preferable to replacement in the retroperitoneum intact [7]. Ultrasound of the inguinal region has been proposed as a means to exclude incarcerated ureteral herniation in patients with renal transplant, oliguria, and possible inguinal hernia [8]. MR urography is also an option in patients who cannot receive iodinated contrast due to renal disease.
Conflict of interest
All authors declare that they have no conflict of interest.
Funding
No sources of funding.
Ethical Approval
Approved by St. Louis University School of Medicine IRB (Protocol ID 24463) on 3/11/2014.
Consent
Consent not required for this radiological research study. No patient identifiers were used.
Author contribution
Emad Allam: Study design, data collection, data analysis, manuscript composition.
David Johnson: Study design, manuscript composition.
Shaun Grewal: Study design, manuscript composition.
Frank Johnson: Study design, data collection, data analysis, manuscript composition.
Guarantor
Emad Allam, Frank Johnson.
Contributor Information
E.S. Allam, Email: eallam@gmail.com.
D.Y. Johnson, Email: dyjohnson@gmail.com.
S.G. Grewal, Email: shaungrewal@yahoo.com.
F.E. Johnson, Email: frankjohnsonmd@gmail.com.
References
- 1.Oruç M.T., Akbulut Z., Ozozan O., Coşkun F. Urological findings in inguinal hernias: a case report and review of the literature. Hernia. 2004;8(February 1):76–79. doi: 10.1007/s10029-003-0157-6. [DOI] [PubMed] [Google Scholar]
- 2.Allam E.S., Johnson D.Y., Grewal S.G., Johnson F.E. Inguinoscrotal hernation of the ureter: description of five cases. Int. J. Surg. Case Rep. 2015;14:160–163. doi: 10.1016/j.ijscr.2015.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pollack H.M., Popky G.L., Blumberg M.L. Hernias of the ureter—An anatomic-roentgenographic study. Radiology. 1975;117(November 2):275–281. doi: 10.1148/117.2.275. [DOI] [PubMed] [Google Scholar]
- 4.Giuly J., François G.F., Giuly D., Leroux C., Nguyen-Cat R.R. Intrascrotal hernia of the ureter and fatty hernia. Hernia. 2003;7(March 1):47–49. doi: 10.1007/s10029-002-0091-z. [DOI] [PubMed] [Google Scholar]
- 5.Sharma R.K., Murari K., Kumar V., Jain V.K. Inguinoscrotal extraperitoneal herniation of a ureter. Can. J. Surg. 2009;52(April 2):E29–30. [PMC free article] [PubMed] [Google Scholar]
- 6.Burstein J.D., Lipshitz S., Weinstein R.J., Boulinakis P., Seidman L., Fredland A. Ureteral herniation: case report and literature review. Mt. Sinai J. Med. 1986;53(February 2):134–136. [PubMed] [Google Scholar]
- 7.Mallouh C., Pellman C.M. Scrotal herniation of the ureter. J. Urol. 1971;106(July 1):38–41. doi: 10.1016/s0022-5347(17)61221-7. [DOI] [PubMed] [Google Scholar]
- 8.Otani L.H., Jayanthi S.K., Chiarantano R.S., Amaral A.M., Menezes M.R., Cerri G.G. Sonographic diagnosis of a ureteral inguinal hernia in a renal transplant. J. Ultrasound Med. 2008;27(December 12):1759–1765. doi: 10.7863/jum.2008.27.12.1759. [DOI] [PubMed] [Google Scholar]