Abstract
Deep brain stimulation (DBS) of the globus pallidus internus (GPi) is an established procedure to improve generalised, segmental craniofacial dystonia. However, no studies have addressed the applicability of DBS for blepharospasm as a focal craniofacial dystonia. A 52-year-old man developed medically intractable involuntary eye closure. Because the abnormal movement was observed exclusively in the eyelids, he was diagnosed not with Meige's syndrome but with blepharospasm as a focal craniofacial dystonia. He underwent stereotactic surgery under general anaesthesia for bilateral GPi-DBS. Continuous GPi stimulation almost completely abolished the blepharospasm. 15 months after the operation, his preoperative scores on the Burke-Fahn-Marsden Dystonia Rating Scale (=8 points) decreased to 1 (87.5% improvement). The present study demonstrates the applicability of GPi-DBS for treating blepharospasm presenting as focal dystonia. Further studies with accumulated case series are needed to confirm the effect of DBS on blepharospasm and other focal craniofacial dystonias.
Background
Dystonia is classified according to distribution into focal, segmental, multifocal, hemidystonia or generalised.1 2
Deep brain stimulation (DBS) of the globus pallidus internus (GPi) is an established procedure to improve generalised1 2 or segmental craniofacial dystonias,1 3–8 and is even effective for certain focal dystonias, especially primary cervical and hand dystonia.1 2–9 Within this context, DBS might be applicable to focal craniofacial dystonias; however, no studies to date have addressed this possibility.
Case presentation
A 52-year-old man developed bilateral, involuntary, right-side dominant eye closure in 2008. Despite the administration of oral medications, including clonazepam 2.0 mg/day and etizolam 1.5 mg/day, the symptom gradually progressed, and eventually affected his ability to drive. The patient underwent botulinum toxin A injection in the orbicularis (Botox 50U) at another hospital every 3 months between 2010 and 2013. This treatment was moderately effective initially, but lost its efficacy over time. At the first visit to our clinic in November 2013, persistent eye closure for ≥50% of waking hours severely impaired his daily activities and work, resulting in depression. He sought surgical treatment to improve this medically intractable symptom.
He had no history of the known aetiologies of dystonia, such as neurological disorders and neuroleptic treatments.
Investigations
The patient's brain anatomy was normal on MRI.
Differential diagnosis
Because the abnormal movement was observed exclusively in the eyelids, the patient was diagnosed not with Meige's syndrome but with blepharospasm as a focal dystonia (video 1, segment 1). He could open the left eye slightly for a short time, allowing him to recognise his surroundings (video 1, segment 2).
Treatment
We informed the patient and his family that although DBS is useful for treating Meige's syndrome and generalised dystonia, its effects on blepharospasm are unknown. With their prior informed consent, we performed the procedure.
In April 2014, the patient underwent stereotactic surgery under general anaesthesia, for bilateral DBS of the GPi (model 3387 electrodes and Activa RC; Medtronic, Minneapolis, MN).9 The tentative target site, determined at a coordinate setting, was 2 mm anterior to the midpoint of a line drawn between the anterior and posterior commissures (AC–PC line), and 20 mm lateral and 3 mm ventral to the AC–PC line. The tentative target coordinates were confirmed to be optimal based on direct visualisation in MRI. Intraoperative microelectrode recordings confirmed the multiunit activities in the GPi and decreased amplitude at the ansa lenticularis, or optic tract, indicating the ventral border of the GPi. The tip of the DBS electrode (contact 0) was placed at the ventral border of the GPi.
We evaluated various stimulation parameters to determine the most effective values, and found that unipolar stimulation was optimal at the following contact, frequency, pulse width (PW) and amplitude settings: 0 -, 130 Hz, 450 µs and 1.1 V on the right side, and 1-, 130 Hz, 450 µs and 1.3 V on the left side, respectively.
Outcome and follow-up
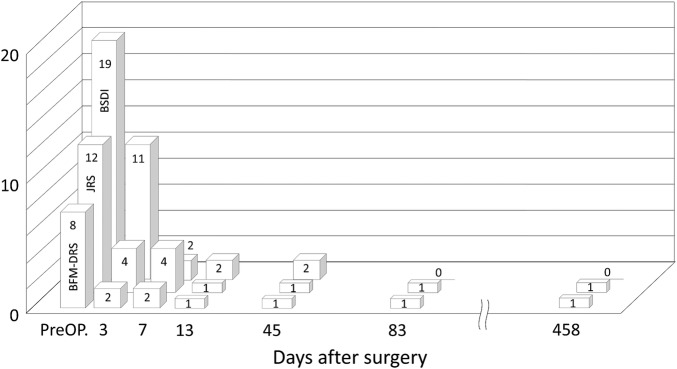
Continuous GPi stimulation almost completely abolished the blepharospasm 7 days after the surgery (video 1 segment 3). The patient returned to work 1 month after the operation. Fifteen months after the operation, his preoperative scores on the Burke-Fahn-Marsden Dystonia Rating Scale (BFM-DRS) (=8 points), the Jankovic Rating Scale (=12 points)10 and the Blepharospasm Disability Index (=19) decreased to 1 (87.5% improvement), 1 (91.7% improvement) and 0 (100% improvement), respectively (figure 1).
Figure 1.
Changes in the Burke-Fahn-Marsden Dystonia Rating Scale (BFM-DRS) score, Jankovic Rating Scale (JRS) score and Blepharospasm Disability Index (BSDI). Fifteen months after the operation, the patient's preoperative BFM-DRS score (8), JRS score (12) and BSDI (19) decreased to 1 (87.5% improvement), 1 (91.7%improvement) and 0 (100% improvement), respectively.
Video 1.
Segment 1—Before the operation, the patient exhibits persistent eye closure for more than 50% of his waking hours. Because the abnormal movement is exclusively observed in the eyelids, he was not diagnosed with Meige's syndrome, but with blepharospasm as a focal craniofacial dystonia. Segment 2—Preoperatively, he is told to open his eyes. He can only open his left eye for a short time. Segment 3–Seven days after the surgery, the blepharospasm is almost completely abolished by the continuous GPi stimulation. GPi, globus pallidus internus.
Discussion
Evidence supporting the efficacy of oral medication for blepharospasm is lacking, although some authors recommend the use of clonazepam.2 Currently, the main treatment option available for blepharospasm is botulinum neurotoxin.2
Although no study has assessed the usefulness of DBS in isolated blepharospasm,2 GPi-DBS has been shown to be beneficial in a blepharospasm trial for craniofacial dystonia (Meige's syndrome). The reported improvement rates in BFM-DRS for the eye were 57%,4 92%3 and 92%5 in single-case studies. Sako et al8 described five patients with Meige's syndrome who experienced 88% improvement in their eyes. Similarly, in their study on six cases, Osterm et al6 reported 86% improvement in BFM-DRS for the eye. However, Reese et al7 showed less effective results (<50% improvement) in 12 patients; the reports of overall good response of blepharospasm in the subset of patients with Meige's syndrome strongly suggests the applicability of DBS to isolated blepharospasm.
The long PW (450 µs) we used in our patient was the consequence of the frequent postoperative parameter adjustments that were made to identify the optimal DBS settings. Even though some studies11 12 have suggested that the PW in GPi-DBS has no effect on the postoperative improvement of patients with cervical or generalised dystonia, the optimal setting for the DBS parameters may differ depending on the pathophysiological characteristics and precise anatomic location of the DBS electrodes in individual patients.
The present study demonstrates the applicability of GPi-DBS for treating blepharospasm presenting as focal dystonia. Further studies with accumulated case series are needed to confirm the effect of DBS on blepharospasm and other focal craniofacial dystonias.
Patient 's perspective.
The patient and his family are very pleased that he is freed from the symptom that he suffered from for 6 years. He says, “I am very happy to have come across this effective therapy.”
Learning points.
Deep brain stimulation (DBS) of the globus pallidus internus (GPi) is an established procedure to improve generalised or segmental craniofacial dystonias, and is even viable for certain focal dystonias.
DBS might be applicable for focal craniofacial dystonias; however, no studies to date have addressed this possibility.
We offer a single case with medically intractable isolated blepharospasm that was almost completely abolished by continuous GPi stimulation.
The present study demonstrates the applicability of GPi-DBS for treating blepharospasm presenting as focal dystonia. Further studies with accumulated case series are needed to confirm the effect of DBS on blepharospasm and other focal craniofacial dystonias.
Footnotes
Contributors: KY designed and conducted the study, including patient recruitment, data collection and data analysis (conception, organisation and execution of research project, and design of statistical analysis). TH and NS contributed to the entire surgical process including planning and targeting, and to the postoperative data analysis (execution of statistical analysis). KY prepared the manuscript draft (writing of the first draft) with important intellectual input from J-iK (review and critique of statistical analysis and of manuscript preparation). All the authors approved the final manuscript.
Funding: A foundation subscribed by Hokuto Hospital, Obihiro, Hokkaido, Japan; a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan (grant number 25462271).
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Albanese A, Asmus F, Bhatia KP et al. EFNS guidelines on diagnosis and treatment of primary dystonias. Eur J Neurol 2011;18:5–18. 10.1111/j.1468-1331.2010.03042.x [DOI] [PubMed] [Google Scholar]
- 2.Batla A, Stamelou M, Bhatia KP. Treatment of focal dystonia. Curr Treat Options Neurol 2012;14:213–29. 10.1007/s11940-012-0169-6 [DOI] [PubMed] [Google Scholar]
- 3.Caplelle H-H, Wigel R, Krauss JK. Bilateral pallidal stimulation for blepharospasm-oromandibular dystonia (Meige sydrome). Neurology 2003;60:2017–18. 10.1212/01.WNL.0000068527.25191.78 [DOI] [PubMed] [Google Scholar]
- 4.Foote KD, Canchez JC, Okun MS. Staged deep brain stimulation for refractory craniofacial dystonia with blepharospasm: case report and physiology. Neurosurgery 2005;56:E415 10.1227/01.NEU.0000147978.67424.42 [DOI] [PubMed] [Google Scholar]
- 5.Loher TJ, Capelle HH, Kaelin-Lang A et al. Deep brain stimulation for dystonia: outcome at long-term follow-up. J Neurol 2008;255:881–4. 10.1007/s00415-008-0798-6 [DOI] [PubMed] [Google Scholar]
- 6.Ostrem JL, Marks WJ Jr, Volz MM et al. Pallidal deep brain stimulation in patients with cranial-cervical dystonia (Meige syndrome). Mov Disord 2007;22:1885–91. 10.1002/mds.21580 [DOI] [PubMed] [Google Scholar]
- 7.Reese R, Gruber D, Schoenecker T et al. Long-term clinical outcome in Meige syndrome treated with internal pallidum deep brain stimulation. Mov Diord 2011;26:691–8. 10.1002/mds.23549 [DOI] [PubMed] [Google Scholar]
- 8.Sako W, Morigaki R, Mizobuchi Y et al. Bilateral pallidal deep brain stimulation in primary Meige syndrome. Parkinsonism Relat Disord 2011;17:123–5. 10.1016/j.parkreldis.2010.11.013 [DOI] [PubMed] [Google Scholar]
- 9.Yamada K, Hamasaki T, Hasegawa Y et al. Long disease duration interferes with therapeutic effect of globuls pallidus interuns pallidal stimulaiton in primary cervical dystonia. Neuromodulaiton 2013;16:219–25. 10.1111/j.1525-1403.2012.00464.x [DOI] [PubMed] [Google Scholar]
- 10.Jankovic J, Kenney C, Grafe S et al. Relationship between various clinical outcome assessments in patients with blepharospasm. Mov Diord 2009;24:407–13. 10.1002/mds.22368 [DOI] [PubMed] [Google Scholar]
- 11.Moro E, Piboolnurak P, Arenovich T et al. Pallidal stimulation in cervical dystonia: clinical implications of acute changes in stimulation parameters. Eur J Neurol 2009;16:506–12. 10.1111/j.1468-1331.2008.02520.x [DOI] [PubMed] [Google Scholar]
- 12.Vercueil L, Houeto JL, Krystkowiak P et al. Effects of pulse width variation in pallidal stimulation for primary generalized dystonia. J Neurol 2007;254:1533–7. 10.1007/s00415-007-0578-8 [DOI] [PubMed] [Google Scholar]