Abstract
Acute pulmonary embolism (PE) is a frequent life-threatening condition in emergency departments. Careful diagnosis is important, and different diagnostic tests such as electrocardiogram (ECG), biochemical markers, echocardiogram, and computed tomography are required. Although ECG is a cheap and rapid diagnostic test for pulmonary embolism, it has some limitations in the differential diagnosis of acute coronary syndrome and acute PE. Herein, we report ECG results of a patient diagnosed with acute PE mimicking acute coronary syndrome.
Keywords: Acute pulmonary embolism, Acute coronary syndrome, ECG
1. Case presentation
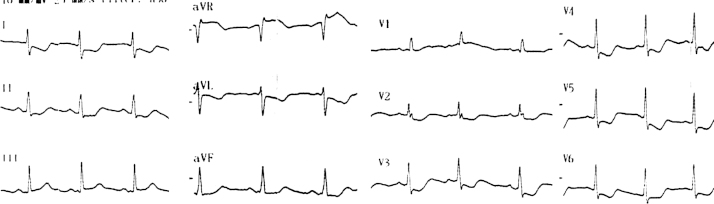
A 72-year-old woman was admitted to the emergency department because of chest pain. She was on valsartan 160 mg daily for hypertension. Physical examination on admission was unremarkable. Twelve-lead electrocardiogram (ECG) revealed sinus rhythm (92 bpm) with diffuse ST-segment depression (involving eight leads) associated with ST-segment elevation in lead aVR (Fig. 1). In addition, ECG showed rightward mean frontal plane QRS-axis and R-wave dominance with pure R waves in leads V1–V3 suggesting right ventricular pressure or volume overload. The patient had no history of chronic obstructive pulmonary disease, rheumatic valvular disease, or other conditions indicating right ventricular pathology. Cardiac enzyme levels were elevated: Creatine kinase (CK)-MB at 7.9 ng/ml (0.6–6.3 ng/ml) and troponin I at 0.79 ng/ml (0–0.04 ng/ml). Since the elevated levels of the cardiac enzymes and ECG changes indicated left main coronary artery or three‐vessel disease, coronary angiography was performed. Surprisingly, it was normal. Bedside echocardiography showed right ventricular enlargement with a normal left ventricular ejection fraction (60%). Computed tomography of the chest was performed because of suspicion of acute pulmonary embolism (APE), and it revealed a thrombus in the right pulmonary artery (Fig. 2). Therefore, thrombolytic therapy (alteplase) was started, and the patient was discharged six days after admission.
Fig. 1.
Twelve-lead ECG shows normal sinus rhythm with diffuse ST-segment depression and ST-segment elevation in aVR lead.
Fig. 2.
Pulmonary CT angiography shows pulmonary embolism being more prominent in the right pulmonary artery (arrow).
Clinical symptoms may be similar in patients with acute coronary syndrome (ACS) and APE, and biochemical markers of myocardial necrosis may be elevated in both diseases. In addition to the medical history and clinical and laboratory findings, 12-lead ECG is important, but has some limitations in the differential diagnosis of ACS and PE. ECG changes suggestive of myocardial ischemia were observed in 70% of patients with APE, and predicted worse progression and 30-day mortality [1], [2]. Diffuse ST-segment depressions in more than six leads associated with ST-segment elevation in aVR lead has been associated with left main, left main equivalent, or severe three‐vessel disease [3]. ST-segment elevation in lead aVR may also occur in APE patients, probably as an expression of right ventricular overload or right ventricular ischemia. It is associated with poor prognosis [4], [5]. A similar case of APE with diffuse ST-segment depressions in more than six leads associated with ST-segment elevation in aVR lead was reported before [6]. To the best of our knowledge, our case is the second one in the literature related to this issue. Emergency physicians, cardiologists, and internists should be aware of the ECG findings of APE mimicking ACS.
Conflict of interest
All authors declare no conflict of interest related to this study. The authors have no commercial associations or sources of support that might pose a conflict of interest.
All authors have made substantive contributions to the study, and all authors endorse the data and conclusions. Nevertheless, confirmation of informed patient consent for publication was obtained
References
- 1.Kukla P., Dlugopolski R., Krupa E. How often pulmonary embolism mimics acute coronary syndrome? Kardiol. Pol. 2011;69(3):235–240. [PubMed] [Google Scholar]
- 2.Zhan Z.Q., Wang C.Q., Wang Z.X. Significance of ST-segment deviation in patients with acute pulmonary embolism and negative T waves. Cardiol. J. 2015;22:583–589. doi: 10.5603/CJ.a2015.0023. [DOI] [PubMed] [Google Scholar]
- 3.Nikus K., Pahlm O., Wagner G. Electrocardiographic classification of acute coronary syndromes: a review by a committee of the International Society for Holter and Non-Invasive Electrocardiology. J. Electrocardiol. 2010;43(2):91–103. doi: 10.1016/j.jelectrocard.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 4.Kukla P., Dlugopolski R., Krupa E. The prognostic value of ST-segment elevation in the lead aVR in patients with acute pulmonary embolism. Kardiol. Pol. 2011;69(7):649–654. [PubMed] [Google Scholar]
- 5.Janata K., Höchtl T., Wenzel C. The role of ST-segment elevation in lead aVR in the risk assessment of patients with acute pulmonary embolism. Clin. Res. Cardiol. 2011;101:329–337. doi: 10.1007/s00392-011-0395-z. [DOI] [PubMed] [Google Scholar]
- 6.Ciliberti P., Rapezzi C., Villani C. Massive pulmonary embolism with acute coronary syndrome-like electrocardiogram mimicking acute left main coronary artery obstruction. J. Emerg. Med. 2011;16:325–331. doi: 10.1016/j.jemermed.2011.03.037. [DOI] [PubMed] [Google Scholar]