Abstract
An 85-year-old man was referred to our hospital with a pacemaker pocket infection. A permanent pacemaker had been implanted via the right subclavian vein. The pacemaker and pacing leads were removed and a temporary pacemaker was implanted. After vancomycin treatment for 4 weeks, pacemaker implantation via the right external iliac vein was performed under local anesthesia because of left subclavian vein occlusion, infection of the right pocket, and difficulty with epicardial lead insertion. The iliac vein approach is an effective alternative in patients in whom the pectoral approach cannot be used.
Learning objective: Permanent pacemaker implantation using the conventional pectoral approach is impossible or contraindicated in 1–6% of patients. In such patients, implantation via the iliac vein is considered an effective alternative. The advantages of this approach are that the wound size and bleeding amount are very small and that it can be performed under local anesthesia. Therefore, this approach can be used in patients with a poor general condition, including elderly patients.
Keywords: Permanent pacemaker implantation, Iliac vein, Pocket infection, Subclavian vein occlusion, Local anesthesia
1. Introduction
The number of permanent pacemaker implantations (PMIs) being performed is increasing due to population aging. The insertion of transvenous pacing leads via the superior vena cava is occasionally impossible; in such situations, a thoracotomy is performed for the placement of epicardial leads. However, the epicardial approach cannot be used in patients at high operative risk because it requires general anesthesia and a thoracotomy. Here we present the case of a patient who successfully underwent permanent PMI via the iliac vein.
2. Case report
An 85-year-old man was referred to our hospital with a persistent fever and swelling in the right chest. In August 2010, a permanent pacemaker was implanted for sick sinus syndrome via the right subclavian vein since the left subclavian vein was occluded. He had a history of thoracic aorta replacement and chronic renal failure on hemodialysis and was hospitalized for dementia and declining mobility. In August 2011, a catheter was inserted in the right internal jugular vein for dialysis shunt occlusion. However, at the start of September, he experienced fever as well as redness and swelling of the pacemaker pocket. Antibiotics were administered for 4 weeks; however, his condition did not improve, so he was referred to our hospital. Immediately after he arrived at our hospital, his pacemaker and pacing leads were removed and a temporary pacemaker was implanted via the right femoral vein. Methicillin-resistant Staphylococcus aureus was detected in his wound and blood samples for which vancomycin was administered for 4 weeks. Negative blood cultures were confirmed over 2 weeks after the completion of vancomycin therapy.
Re-implantation of a permanent pacemaker was considered. However, the subclavian vein approach was impossible because of occlusion and an infection of the right pocket and jugular vein. Epicardial lead insertion from below the xiphoid process was considered difficult because of the high risk of general anesthesia and adhesions from past aortic replacement surgery. Therefore, PMI via the right external iliac vein was considered. Under local anesthesia, a skin incision was made two finger breadths above the right inguinal ligament. The subcutaneous tissue was peeled back to expose the external iliac vein (Fig. 1). The external iliac vein was punctured under direct vision and a 55-cm-long sheath was inserted. A 75-cm-long active fixation lead (CapSureFix NOVUS 5076®; Medtronic) was screwed to the right ventricular septum (Fig. 2). A subcutaneous pocket was created by hand for the device in the external oblique fascia from the incision site. The incision site was closed using absorbable suture (2-0 PDS™; Ethicon) and skin staplers (Appose™; Covidien). The procedure lasted for approximately 2 h and a small amount of bleeding was noted. He was discharged from the hospital 3 days after the procedure without any complications.
Fig. 1.
An image showing the skin incision and exposure of the external iliac vein. The skin incision is made two finger breadths above the right inguinal ligament. Under local anesthesia, the subcutaneous tissue is peeled back and the external iliac vein is exposed.
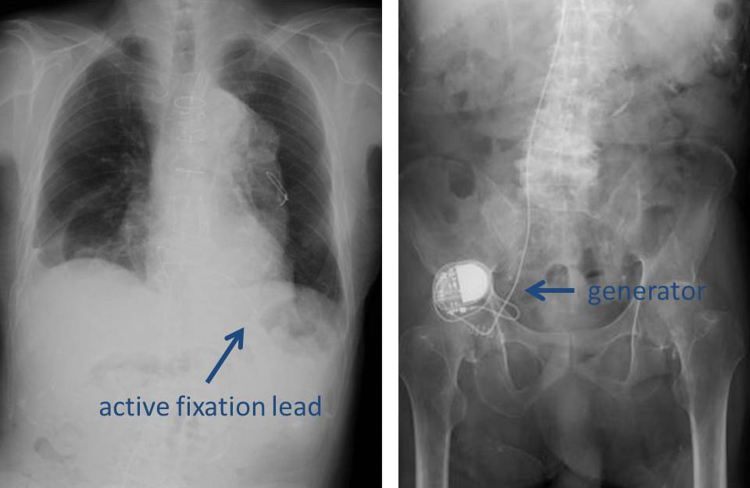
Fig. 2.
An image showing insertion of the lead and generator. A 55-cm-long sheath is inserted into the external iliac vein and a 75-cm-long active fixation lead (CapSureFix NOVUS 5076®; Medtronic) is screwed to the right ventricular septum. A subcutaneous pocket for the device is created by hand in the external oblique fascia from the incision site.
3. Discussion
Here we presented a case of a patient who successfully underwent permanent PMI via the iliac vein.
Studies have reported that permanent PMI using the conventional pectoral approach is impossible or contraindicated in 1–6% of patients [1], [2], [3], [4], [5]. In such patients, PMI via the iliac vein is considered an effective alternative. The advantages of this approach are that the wound size and bleeding amount are very small and that it can be performed under local anesthesia [5]. Therefore, this approach can be used in patients with a poor general condition. Another advantage is the low possibility of late threshold increases in the epicardial leads. However, this procedure has several limitations, including retroperitoneal hematoma due to erroneous arterial puncture, a high rate of atrial lead dislodgement, and lead fracture with hip joint movement [1], [2], [3], [4], [5]. Retroperitoneal hematoma can be avoided with puncture under visual guidance as in the present case. The atrial lead dislodgement rate is reportedly 7–21% [1], [2], [3], [4], and the anatomical morphology and gravitational forces acting upon the implanted generator are the main causes [2], [3], [4], [5]. Our primary aim in the current study was to save the patient’s life; therefore, atrial leads were not used and the procedure could be completed in little time without any complications. Lead fracture induced by hip joint movement was reported previously [1], [3]. However, no study has reported that lead fracture occurs more frequently after the iliac vein approach than after the conventional pectoral approach. To monitor for lead fracture, our patient has been followed up intensively. More than 3 years have passed since the procedure, lead fracture has not occurred, and the patient remains in good condition.
The iliac vein approach is an effective complication-free alternative for patients in whom the pectoral approach cannot be used. For this approach, patients should be appropriately selected, the need for atrial leads should be assessed, and puncture should be performed under visual guidance.
Conflict of interest
All authors declare no conflict of interest related to this study.
Acknowledgments
This case was presented at the 4th Implantable Cardiac Device Winter Conference on February 10, 2012.
References
- 1.Ellestad M.H., Caso R., Greenberg P.S. Permanent pacemaker implantation using the femoral vein: a preliminary report. Pacing Clin Electrophysiol. 1980;3:418–423. doi: 10.1111/j.1540-8159.1980.tb05250.x. [DOI] [PubMed] [Google Scholar]
- 2.Ellestad M.H., French J. Iliac vein approach to permanent pacemaker implantation. Pacing Clin Electrophysiol. 1989;12:1030–1033. doi: 10.1111/j.1540-8159.1989.tb01921.x. [DOI] [PubMed] [Google Scholar]
- 3.Mathur G., Stabels R.H., Heaven D., Ingram A., Sutton R. Permanent pacemaker implantation via the femoral vein: an alternative in cases with contraindications to the pectoral approach. Europace. 2001;3:56–59. doi: 10.1053/eupc.2000.0135. [DOI] [PubMed] [Google Scholar]
- 4.Barakat K., Hill J., Kelly P. Permanent transfemoral pacemaker implantation is the technique of choice for patients in whom the superior vena cava is inaccessible. Pacing Clin Electrophysiol. 2000;23:446–449. doi: 10.1111/j.1540-8159.2000.tb00825.x. [DOI] [PubMed] [Google Scholar]
- 5.Tsutsumi K., Hashizume K., Kimura N. Permanent pacemaker implantation via the iliac vein: an alternative in 4 cases with contraindications to the pectoral approach. J Arrhythmia. 2010;26:55–61. [Google Scholar]