Abstract
Background
Consistent detection of rotor(s) and/or focal impulse(s) of atrial fibrillation can using a 64-pole basket catheter remain unclear.
Methods and results
Intracardiac left atrial electrograms were recorded, prior to ablation, in 20 patients with atrial fibrillation. Unipolar electrograms, filtered at 0.1–300 Hz, were recorded and exported for an offline phase analysis. From the cohort, 8 of the 20 patients had analyzable data. Localized rotors were identified in 3 of these patients, with focal impulses detected in 4 patients.
Conclusion
Localized rotors and focal impulses can be identified on phase maps of atrial fibrillation in a small number of patients.
Keywords: Atrial fibrillation, Rotor, Focal impulse, Phase mapping
1. Background
The existence of localized rotors and focal impulses has been reported in human atrial fibrillation (AF) [1]. Phase mapping has been used to characterize the spatiotemporal variability of electrical activities, thereby providing insight into the mechanisms of AF [1], [2]. Although the existence of a rotor, along with fibrillatory conduction, has been reported to contribute to maintenance of AF [3], the prevalence and specific role of stable rotors and/or focal impulses in human AF remain unclear. Therefore, we investigated whether rotors and focal impulses can be identified in human AF by analyzing intracardiac electrograms recorded from a multi-electrode catheter.
2. Methods
2.1. Study patients
This study included 20 consecutive patients undergoing initial catheter ablation for drug-refractory AF: 9 for paroxysmal AF (spontaneous termination within 7 days), and 11 for persistent AF (AF lasting more than 7 days). The study protocol was approved by the Institutional Review Board of Nihon University Itabashi Hospital (December 7, 2012, RK-121109-5), and all patients provided written informed consent for participation in the study, which was conducted under ethics committee approval. All antiarrhythmic drugs were discontinued for at least 5 half-lives before ablation, and all patients underwent multidetector-row computed tomography for construction of 3-dimensional maps of the left atrium (LA) (NavX system; St. Jude Medical, Inc., St. Paul, MN, USA).
2.2. Electrophysiological study and unipole signal recordings
Electrophysiological study was performed with patients under conscious sedation that was achieved with propofol and fentanyl [4], [5]. After 2 long sheaths (1 SL0 sheath and 1 Agilis sheath; St. Jude Medical, Inc.) were inserted into the LA via transseptal puncture; the 3-dimensional geometry of the LA and the 4 pulmonary veins (PVs) were reconstructed by using the EnSite NavX navigation system (v8.0; St. Jude Medical, Inc.), and a 20-pole circular mapping catheter with 1.5-mm interelectrode spacing (Livewire Spiral HP catheter, St. Jude Medical, Inc.). Thereafter, a 64-pole basket catheter (BC), consisting of 8 splines with 8 electrodes each (Boston Scientific, Natick, MA, USA), was placed in the LA and labeled on the EnSite NavX system, and simultaneous 60-s unipolar signals were recorded with a filter setting of 0.1–300 Hz. The BC was deployed in the LA, with the distal end placed at the superior left pulmonary vein antrum (Fig. 1). A BC of adequate size (38 mm, 48 mm, or 60 mm with an interelectrode spacing of 3 mm, 4 mm, or 5 mm, respectively) was selected for consistent contact with the LA endocardium. If the patient was in sinus rhythm, AF was induced via rapid atrial pacing from the coronary sinus ostium. Each 10-s data segment was exported for offline phase mapping analysis, which was performed with CEPAS software (Cuoretech Pty. Ltd., Sydney, Australia).
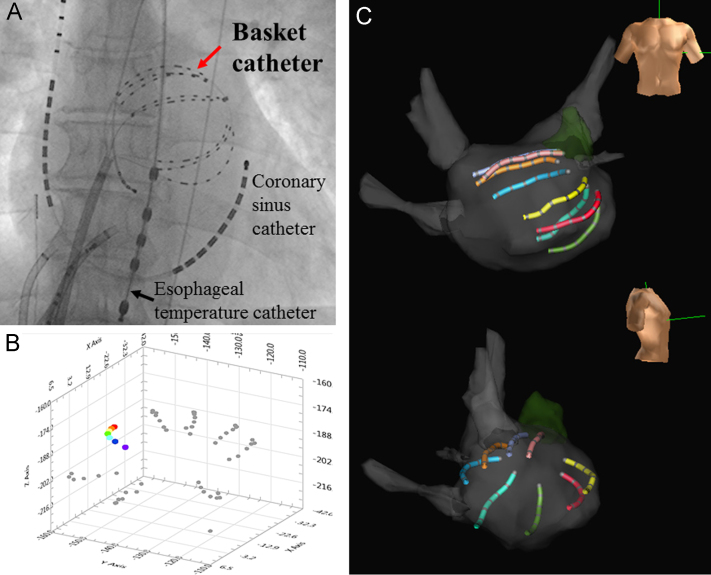
Fig. 1.
Data acquisition from a basket catheter (BC). (A) Fluoroscopic image (anteroposterior view) of the BC (red arrow). The catheter is placed in the posterolateral left atrium (LA). (B) Panoramic diagram of the BC in the LA chamber, as depicted by the CEPAS. The proximal electrodes are indicated by red dots and the distal electrodes by purple dots. (C) Three-dimensional electroanatomic shell of the LA showing the BC. Anteroposterior view (upper image) and right lateral view (lower image). The distal electrodes are seen on the right side, and the proximal electrodes on the left side, of the upper image.
2.3. Phase mapping analysis
CEPAS™ incorporates user-defined characteristics to identify electrogram activations on each unipole of the mapping catheter. These characteristics include (i) baseline noise threshold, (ii) electrogram width criterion, to avoid detection of broad far-field activation, (iii) electrogram slope, and (iv) electrogram refractory periods, to avoid multiple detections within the same activation. For analysis, the noise threshold was set at 0.1 mV, width criterion at 10 ms, and the refractory period at 50 ms. Activation timing was then used to compute the phase [6]. Prior to activation detection and phase mapping, the signals were filtered, using the CEPAS system, with a 50 Hz alternating current removal filter (only if required), low pass filter with a cutoff frequency of 100 Hz to remove high frequency noise, and a wavelet filter as a wandering baseline removal filter. Any ventricular activation picked up, typically on the splines closest to the mitral annulus, was removed using a V wave removal algorithm. The activation detection algorithm automatically detects activations for all channels (Fig. 2). If the automatic detection algorithm did not work accurately, based on an expert user׳s opinion, either by missing activations or by falsely including activations, manual adjustments were possible to add, remove, or adjust the location of activations on individual channels. The phase map was oriented to give a 2-dimensional representation of the LA.
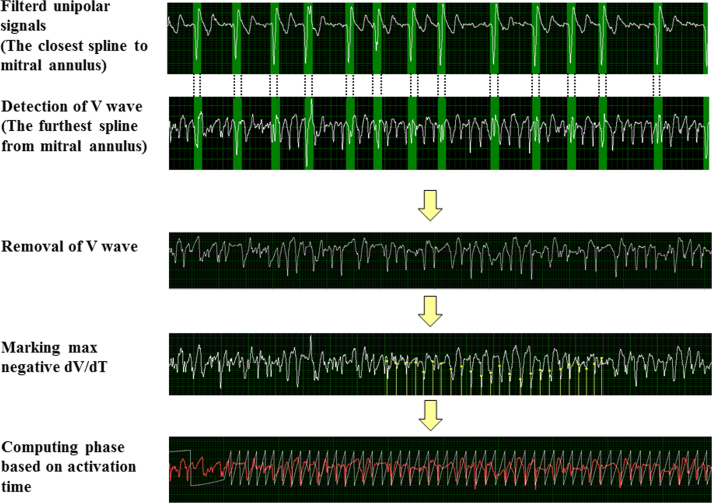
Fig. 2.
Schematic representation of the phase analysis process for detection of the wavefront activation. Fibrillatory unipolar signals are recorded and pre-processed by a 50 Hz alternate current filter, low-pass filter designed with a 100 Hz cut-off, and a baseline wander removal based on the wavelets. The complex wave is canceled by a template subtraction algorithm. First, a distinct V wave complex from the spline closest to mitral annulus is identified (first row), with an ambiguous V wave from the furthest spline (second row) coupled. Second, the fibrillatory signals are marked with the negative dV/dt max to directly compute the phase. The signals are then subjected to fast Fourier transform analysis, and finally the frequency spectrum is determined.
2.4. Fast Fourier transform (FFT) analysis
Frequency domain analysis with FFT, to estimate the power spectra of the signals [4], [5], was performed simultaneously with phase mapping [7]. For this analysis, the exported signals were filtered using the same filters as used for phase mapping. The atrial fibrillatory signals were full wave rectified, and the FFT window was set to flat-top. The spectrum was computed by means of the FFT. The dominant frequency (DF) was defined as the frequency with the maximum power in the frequency range of 3–15 Hz [8]. The regularity index, defined as the ratio of the area under the curve of the spectrum, within the 0.75-Hz band around the DF, to the area under the spectrum curve over the whole 3–15-Hz band, was computed simultaneously to quantify the sharpness of the dominant peak [9]. The rotor was defined as a stable rotating pattern of 360° observed on the phase map.
3. Results
Patient mean age was 54±12 years, and all were men. The median AF duration was 60 (17–109) months, and mean transthoracic echocardiography-derived LA diameter was 38±5 mm. The BCs were 38 mm (4 patients), 48 mm (9 patients), or 60 mm (7 patients) in diameter.
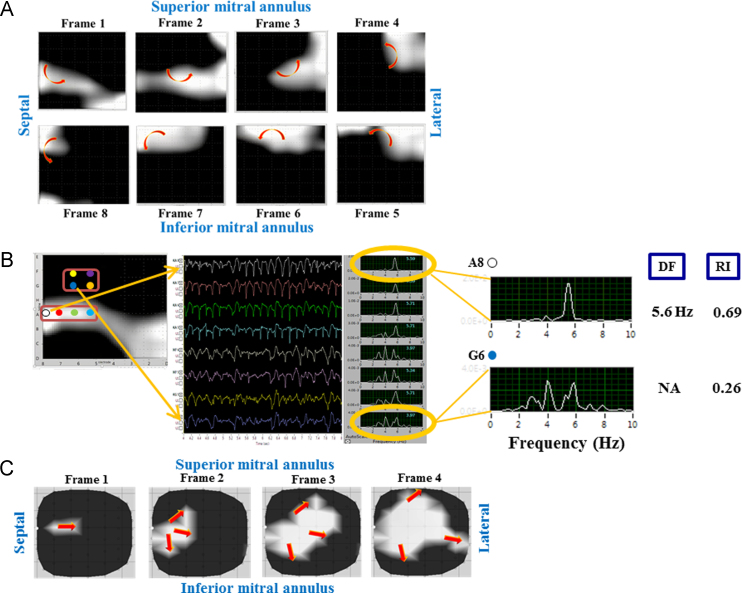
High-quality left atrial intracardiac electrogram recordings were obtained for 8 patients (40%). Intracardiac electrogram signals for the remaining 12 patients were of reduced quality due to insufficient contact between some of the BC electrodes and the LA wall, and thus did not furnish global maps. One or more localized rotors were detected in 3 (37.5%) of the 8 patients (Fig. 3A). Localized rotors lasted 1.9–6.8 s. Regions in the rotor path were characterized by a distinct DF, whereas the region at the center of the rotor exhibited a fragmented, irregular, low-amplitude wavefront, resulting in no distinct DF (Fig. 3B). Of the remaining 5 patients, 4 were shown to have focal impulses (Fig. 3C), and 1 exhibited neither a rotor nor focal impulse. The regions at the focus exhibited a sharp DF.
Fig. 3.
Representative phase maps. (A) Representative sequential phase maps of the left atrium (LA), indicating a localized rotor. Frames 1–8 (1 cycle) are at 20 ms intervals. During atrial fibrillation (AF), a single counter clockwise rotor is seen in the anterior LA; AF cycle length is 170 ms. (B) Intracardiac electrograms and frequency spectrums from the same patient as in panel (A). The wavefront at the rotor path indicates a distinct dominant frequency (DF), while that at the center region of the rotor does not exhibit any distinct DF. RI=regularity index. (C) Representative sequential phase maps of the LA, indicating a focal impulse. Frames 1–4 are at 5 ms intervals.
4. Discussion
The existence of rotor(s) during AF has been demonstrated in an isolated sheep heart [3], and subsequently demonstrated in human AF via BC recordings, epicardial mapping, and body surface mapping [6], [10], [11]. These procedures aimed to identify atrial sites that exhibited multiphasic and rapid activation, and ablation at those sites effectively terminated the AF [10], [11]. However, the number of rotors and results of rotor ablation remain poorly defined [12]. Stable LA activation was recorded from the BC in 8 of the 20 study patients, and in 3 of these 8 patients, rotors localized to the LA were observed. Although limited, the present results suggest that BC-based phase mapping can be used to visualize the LA wavefront dynamics underlying AF. We found that the power spectra along the rotor path typically exhibited a single peak frequency, but the region at the center of the rotor did not show a single, clear DF. This finding is consistent with a previous report that the widespread frequency power distribution during the meandering of a rotor reflects the power spectra of signals outside its immediate vicinity, and thus explains the irregular and fragmented local electrograms [13]. Identification of the rotating wavefronts or focal impulses from multi-electrode catheter recordings is difficult because of low signal quality and/or low spatial sampling density. In 12 of the 20 patients, a number of BC electrodes did not adequately contact the LA wall, and thus the BC coverage posed a major methodological limitation in the assessment of global LA activation, as also reported previously [12].
5. Conclusions
In some patients, localized rotors and focal impulses can be identified during AF via phase mapping from BC electrograms. Such phase maps provide dynamic visualization of electrical activation during AF, but improvement in signal quality and wide-area coverage of the LA surface is required before this method can be used in all patients.
Source of funding
This work was supported by a Japan Heart Foundation Memorial Research Grant, awarded to Dr. Hiroshi Irisawa and Dr. Aya Irisawa.
Conflict of interest
All authors declare no conflict of interest related to this study.
Acknowledgments
We would like to thank Mr. John Martin for assistance with the English text.
Footnotes
Supplementary data associated with this article can be found in the online version at http://dx.doi.org/10.1016/j.joa.2015.11.010.
Appendix A. Supplementary material
Supplemental Video 1 Representative phase map of the left atrium (LA) indicating 2 localized rotors at the LA posterior and anterior.
Supplemental Video 2 Representative phase map of the left atrium (LA) indicating a focal impulse on the LA roof.
References
- 1.Lalani G.G., Trikha R., Krummen D.E., Narayan S.M. Rotors and focal sources for human atrial fibrillation: mechanistic paradigm with direct clinical relevance. Circ J. 2014;78:2357–2366. doi: 10.1253/circj.cj-14-0478. [DOI] [PubMed] [Google Scholar]
- 2.Cuculich P.S., Wang Y., Lindsay B.D. Noninvasive characterization of epicardial activation in humans with diverse atrial fibrillation patterns. Circulation. 2010;22:1364–1372. doi: 10.1161/CIRCULATIONAHA.110.945709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jalife J., Berenfeld O., Mansour M. Mother rotors and fibrillatory conduction: a mechanism of atrial fibrillation. Cardiovasc Res. 2002;54:204–216. doi: 10.1016/s0008-6363(02)00223-7. [DOI] [PubMed] [Google Scholar]
- 4.Kogawa R., Okumura Y., Watanabe I. Spatial and temporal variability of the complex fractionated atrial electrogram activity and dominant frequency in human atrial fibrillation. J Arrhythmia. 2015;31:101–107. doi: 10.1016/j.joa.2014.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Okumura Y., Watanabe I., Kofune M. Characteristics and distribution of complex fractionated atrial electrograms and the dominant frequency during atrial fibrillation: relationship to the response and outcome of circumferential pulmonary vein isolation. J Interv Card Electrophysiol. 2012;34:267–275. doi: 10.1007/s10840-011-9637-2. [DOI] [PubMed] [Google Scholar]
- 6.Lee G., Kumar S., Teh A. Epicardial wave mapping in human long-lasting persistent atrial fibrillation: transient rotational circuits, complex wavefronts, and disorganized activity. Eur Heart J. 2014;35:86–97. doi: 10.1093/eurheartj/eht267. [DOI] [PubMed] [Google Scholar]
- 7.Sasaki N., Okumura Y., Watanabe I. Frequency analysis of atrial fibrillation from the specific ECG leads V7–V9: A lower DF in lead V9 is a marker of potential atrial remodeling. J Cardiol. 2015;66:388–394. doi: 10.1016/j.jjcc.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 8.Husser D., Stridh M., Sörnmo L. Frequency analysis of atrial fibrillation from the surface electrocardiogram. Indian Pacing Electrophysiol J. 2004;4:122–136. [PMC free article] [PubMed] [Google Scholar]
- 9.Bencsik G., Martinek M., Hassanein S. Acute effects of complex fractionated atrial electrogram ablation on dominant frequency and regulatory index for the fibrillatory process. Europace. 2009;11:1011–1017. doi: 10.1093/europace/eup113. [DOI] [PubMed] [Google Scholar]
- 10.Narayan S.M., Krummen D.E., Shivkumar K. Treatment of atrial fibrillation by the ablation of localized sources: CONFIRM (Conventional Ablation for Atrial Fibrillation With or Without Focal Impulse and Rotor Modulation) trial. J Am Coll Cardiol. 2012;60:628–636. doi: 10.1016/j.jacc.2012.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haissaguerre M., Hocini M., Denis A. Driver domains in persistent atrial fibrillation. Circulation. 2014;130:530–538. doi: 10.1161/CIRCULATIONAHA.113.005421. [DOI] [PubMed] [Google Scholar]
- 12.Benharash P., Buch E., Frank P. Quantitative analysis of localized sources identified by focal impulse and rotor modulation in atrial fibrillation. Circ Arrhythm Electrophysiol. 2015;8:554–561. doi: 10.1161/CIRCEP.115.002721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zlochiver S., Yamazaki M., Kalifa J., Berenfeld O. Rotor meandering contributes to irregularity in electrograms during atrial fibrillation. Heart Rhythm. 2008;5:846–854. doi: 10.1016/j.hrthm.2008.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Video 1 Representative phase map of the left atrium (LA) indicating 2 localized rotors at the LA posterior and anterior.
Supplemental Video 2 Representative phase map of the left atrium (LA) indicating a focal impulse on the LA roof.