Abstract
Injection drug users (IDUs) are at high risk of acquiring HIV infection through preventable drug- and sex-related HIV risk behaviors. In recent decade, there has been a growing evidence that methadone maintenance treatment (MMT) is associated with a significant decrease in both drug- and sex-related risk behaviors among this high-risk population. The better understanding of the relationship between MMT and HIV-related risk behaviors will help to better inform future HIV prevention strategies, which may have policy implications as well. In this systematic review, we therefore aimed to explore the relevant literature to more clearly examine the possible impact of MMT on HIV risks behaviors among high-risk IDUs. The findings thus far suggest that MMT is associated with a significant decrease in injecting drug use and sharing of injecting equipment. Evidence on sex-related risk behavior is limited, but suggest that MMT is associated with a lower incidence of multiple sex partners and unprotected sex. The literature also suggests that the most significant factor in reducing HIV risks was treatment adherence. As such, more attention needs to be given in future studies to ensure the higher rates of access to MMT as well as to improve the adherence to MMT.
Keywords: Methadone maintenance treatment, HIV risk reduction, injection drug users, HIV/AIDS, behavioral interventions, opioid-dependence, systematic review
Introduction
Globally, approximately 78 million people have been infected with the HIV and about 39 million people have died of HIV, since the beginning of the HIV/AIDS epidemic.[1] In the United States alone, approximately 600,000 people have died of AIDS-related illnesses. Despite a wide array of primary and secondary HIV prevention approaches, the US is still facing a major ongoing HIV epidemic with around 50,000 new infections per year.[2] Although new HIV infections attributed to drug injection have been decreasing in the United States since the late 1980s, rates continue to be high among specific sub-populations of IDUs, including racial/ethnic minority groups.[2]
Injection drug use has been inextricably linked with HIV/AIDS since the beginning of the epidemic.[3, 4] Behaviors related with drug use that are specific for HIV transmission include shared use of injection equipment and other paraphernalia and unprotected sexual intercourse with injecting drug users (IDU),[5–9] both of which are influenced by wider structural and environmental factors such as patterns of drug use, commercial sex work, and the availability and nature of interventions aimed at reducing harm.
Despite advances in scientific understanding of HIV, its prevention and treatment, previous research has found that drug users engage in high-risk sexual behaviors and most people living with HIV or at risk for HIV do not have access to prevention and treatment. However, effective treatment with antiretroviral drugs can control the virus so that people with HIV can enjoy healthy lives and reduce the risk of transmitting the virus to others.[10–12]
In a recent decade, treatment programs, such as methadone maintenance treatment (MMT), have been shown to be effective in reducing drug use and injection related risk behaviors.[13–15] Studies have indicated that MMT is associated with a significant decrease in both drug-related and sex-related risk behaviors and emphasize the benefits of methadone programs for public health and HIV prevention.[13–15] Indeed, the studies have shown that the higher rate of retaining IDUs in MMT is positively associated to their treatment success rate and can affect many aspects of the participant’s life in a positive way, including reduction of HIV risk.[16, 17] Likewise, studies have found that low-threshold MMT programs can reduce the risk of HIV without the enforcement of abstinence–based policies.[18] Understanding the effectiveness of MMT on high-risk population, some studies points to the need for further study of MMT access in this setting as a means of informing efforts aimed at maximizing initiation of MMT among the target population.
The better understanding of the relationship between MMT and HIV-related risk behaviors will help to better inform future HIV prevention strategies, which may also have policy implications as well. Thus, understanding the relationship between injection drug use, methadone maintenance program, and HIV risk factors is crucial to successfully intervening against a range of risk behaviors among IDUs. This systematic review is aimed at exploring the relevant research literature to more clearly examine the possible impact of MMT on HIV risks behaviors among high-risk IDUs. The outcome of this study could potentially provide general evidence about the influence of methadone maintenance treatment on HIV related risk behaviors among high-risk injection drug users.
Methods
Search methods for identification of studies
The literature review for this review paper was restricted to peer-reviewed research articles and dissertations on the effects of MMT on HIV risk behaviors among high-risk IDUs. To build the systemic review, we searched for relevant English-language papers published between 2005 through November 2015 (present date). Studies were identified using PubMed database with the following search terms: [(Methadone maintenance program) OR (MMP) OR (methadone maintenance treatment) OR (MMT) OR (opiate replacement therapy) OR (ORT)] AND [(HIV risk behaviors) OR (sexual risk behavior) OR (substance abuse risk behavior) OR (condom use) OR (injection drug use) OR (IDU) OR (multiple sex partner)] AND [(high-risk injection drug users) OR (injection drug users) OR (IDU)]. A secondary search was conducted, which involved checking the reference sections of relevant review papers for articles that may have missed in the initial computerized search.
Study selection and inclusion/exclusion criteria
In conducting the systematic review, we included peer-reviewed studies that met all of the following criteria: (1) participants were high-risk injection drug users; (2) participants enrolled in MMT; (3) assessed substance- or sexual-related HIV risk behavior outcome(s); and (d) were published in English. The search was not limited to any particular geographic area or region and there were no restrictions imposed on the age of subject populations. Studies were excluded if they focused on sexual and drug use transmission risk but not on impacts of MMT on HIV risk behaviors. We also excluded the studies with medically and psychologically unstable participants and pharmaceutical studies.
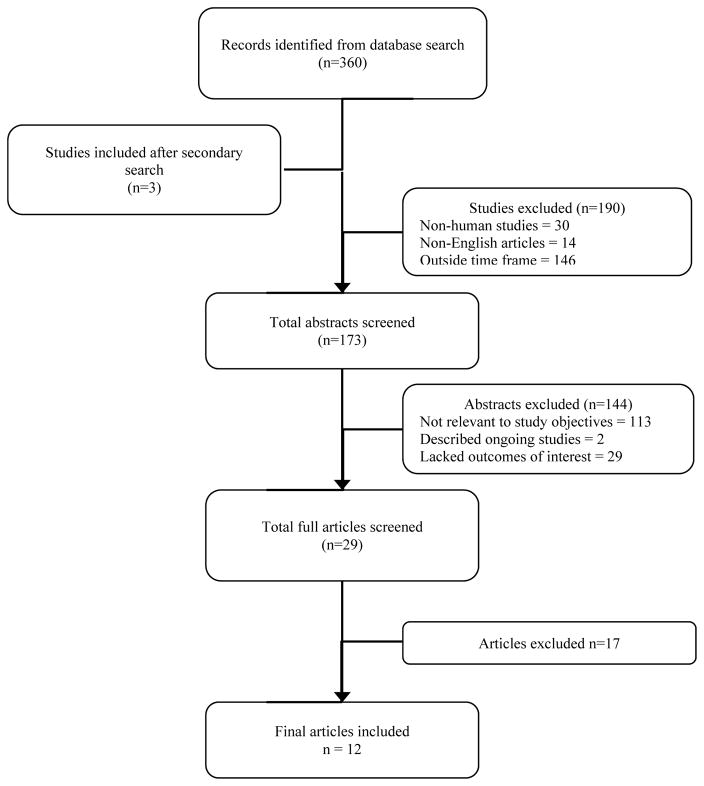
A total of 360 articles were retrieved as of October 25, 2015. After 3 additional articles were found in the reference section of the relevant journal articles, we had 363 articles for preliminary review. Of these, 190 were subsequently excluded because they were non-human studies (30), non-English articles (14), and outside time frame (146), thus leaving 173 records for further review. After inspecting study titles and abstracts, we found that 113 records were not directly relevant to the study objectives, 2 described ongoing studies with no data published, and 29 lacked the stated outcomes of interest, leaving 29 records for further, more detailed, review. A full-text copy of these subset of studies were obtained and assessed for inclusion. Seventeen full-text records were excluded because they did not investigate an association between the variables of interest and behavioral outcomes that constitute HIV risk behaviors. Finally, a total of 12 studies were included for this review. A flowchart of the study population selection process is shown in Figure 1.
Figure 1.
Summary of study selection process
Data extraction and management
Studies found relevant and rigorous were eligible for the review. Data concerning study characteristics, participant characteristics, study design characteristics, and outcome characteristics were independently abstracted from relevant studies by two reviewers (PK and RS). Any discrepancies were resolved by discussion or by contacting additional authors (THM and MC).
A standardized form was utilized for data extraction process. Article characteristics included such information as (1) authors, (2) publication year, (3) study duration, (4) location of study, (5) sample size, and (6) a theoretical framework guiding the intervention. Participant characteristics included (1) age, (2) gender distribution, and (3) sample type. Study design characteristics included (1) type of study design, (2) methadone dose, and (3) years in methadone treatment program. Outcome characteristics included influence of MMT on HIV risk behaviors, including (1) self-reported condom use (male or female condoms), (2) self-reported number of sexual partners, (3) self-reported injection drug use pattern, and (4) self-efficacy (assessing self-confidence related to condom application skills, sexual practices, and needle cleaning skills after intervention).
Results
Description of studies
A total of 12 studies met the review inclusion criteria (Table 1). Studies were conducted between 2005 and 2015, with almost two-forth (41%; k = 5) of the studies taking place within the last 5 years. Study locations included 4 countries: China (41.7%), Canada (33.3%), the United States (16.7%) and Iran (8.3%). In terms of methods, over half of the studies (58.3%) were longitudinal, 33.3% cross-sectional, and 8.3% were randomized controlled trial. Studies collected data through face-to-face interviews (66.6%), self-administered surveys (33.3%). Sex-related risk behaviors among samples were assessed in 8 studies (66.7%), whereas, drug-related risk behaviors were assessed in all the studies (k = 12). However, no studies looked at the self-efficacy related to HIV risk reduction skills.
Table 1.
Summary of studies included in the review
| Study (first author, date) | Study location | Study site | Sample size (N) | Age (Years) | Study design | Incentive | Sex-related Outcome | Drug-related Outcome | Summary of findings |
|---|---|---|---|---|---|---|---|---|---|
| Wang et al., 2014 | China | Community-based | 2530 | 31.0 | Cross-sectional | No | Yes | Yes | MMT-only & combination of MMT and VCT associated with needle sharing and unprotected sexual behaviors |
| Wang et al., 2014 | China | Clinics, Hospitals | 2662 | 36.9 | Randomized Controlled Trial | Yes | No | Yes | MMT supplemented with CP or CM reduce heroin use and related risk behaviors |
| Chen et al., 2013 | China | Clinic-based | 5305 | 38.7 | Longitudinal | No | Yes | Yes | Positive effects of MMT on HIV prevention |
| Alavian et al., 2013 | Iran | Clinic-based | 259 | 33.0 | Longitudinal | No | Yes | Yes | MMT shown to prevent transmission of STDs |
| Pettes et al., 2010 | Canada | NR | 353 | NR | Longitudinal | No | No | Yes | MMT use associated with a reduced likelihood of drug use related risk behavior |
| Corsi et al., 2009 | USA | Community-based | 160 | 39.0 | Cross-sectional | No | Yes | Yes | Retaining IDUs in MMT is needed in order to maximize the successful treatment |
| Qian et al., 2007 | China | Clinics | 557 | NR | Cross-sectional | Yes | Yes | Yes | MMT participants less likely to use or inject drugs & share needles & less likely to have multiple sexual partners or have unprotected sex |
| Willner-Reid et al., 2008 | USA | Clinic-based | 659 | 38.0 | Longitudinal | Yes | Yes | Yes | both drug- and sex-related risk behaviors decrease during MMT |
| Pang et al., 2007 | China | Clinic-based | 1662 | 32.9 | Cross-sectional | No | Yes | Yes | MMT contributed to a reduction in drug use, drug injecting behaviors |
| Millson et al., 2007 | Canada | NR | 183 | NR | Longitudinal | Yes | No | Yes | Low-threshold MMT programs can reduce the risk of HIV |
| Palepu et al., 2006 | Canada | NR | 278 | NR | Longitudinal | Yes | No | Yes | Among HIV/HCV co-infected IDUs on HAART, enrollment in MMT associated with reduced heroin use |
| Kerr et al., 2005 | Canada | NR | 1587 | 33.4 | Longitudinal | Yes | Yes | No | MMT associated with reductions in heroin use and HIV risk behavior |
Note: NR: Not reported | CP: Counseling psychology | CM: Contingency Management
Overall, 16,195 IDUs were enrolled across the study. Study sample sizes ranged from 160 to 5305, with the average number of 1,350 per study. The average age across samples was 35.4 years (range = 31.0 – 39.2; k = 8). Study participants were predominantly recruited from venues that served active drug users, including substance abuse treatment clinics, service organizations, or defined communities. Half (k = 6) of the studies paid incentives to individuals for participation in the study. A complete summary of the outcome measures generated from each citation appears in Table 1.
MMT and HIV risk behaviors
All studies reviewed in the present study found a significant association between MMT and reduction of sex- and drug-related HIV risk behaviors among IDUs. For example, a recent study by Wang et al. (2014) on long-term effects of MMT among 2662 patients in China found that the use of illicit drug and related risk behavior among the participants with MMT was significantly lower.[19] Similarly, Chen, Xia, Hong, Hall and Ling (2013) showed that the HIV-risk behaviors among drugs users decreased over the course of MMT, especially in the first 6 months, indicating positive effects of MMT on HIV prevention.[20] Likewise, Wang et al. (2014) examined the associations of MMT and voluntary counselling and testing (VCT) with HIV risk behaviors among 2530 IDUs in China. The findings showed that the prevalence of unprotected sex and drug use risk behavior was significantly more common among those receiving VCT-only than those receiving both MMT and VCT.[21]
In a prospective study that sought to longitudinally investigate MMT use among HIV positive IDUs in Canada, Pettes, Wood, Guillemi, Mmath, Montaner and Kerr (2010) showed that MMT use was associated with a reduced likelihood of frequent heroin injection, syringe borrowing, non-fatal overdose, and public injection.[22] Likewise, Corsi, Lehman and Booth (2009) found that spending more time in MMT was a significant predictor of positive outcomes on drug use and HIV risk behaviors.[23] The results underscore the importance of retaining IDUs in MMT in order to maximize their treatment success.
In addition, Willner-Reid, Belendiuk, Epstein, Schmittner and Preston (2008) examined the impact of MMT on risk behaviors for transmission of blood-borne disease in poly drug users. The study found that HCV-positive participants were engaged in more HIV risk behaviors than HCV-negative participants. Interestingly, this difference was specific to injection-related behaviors and decreased significantly within the first few weeks of MMT.[24] In a cohort study of HIV/HCV co-infected IDUs in Canada, Palepu et al (2006) found that enrollment in MMT was associated with reduced heroin use, and improved adherence, HIV-1 RNA suppression and CD4 cell count response.[25] These findings demonstrate that both drug- and sex-related risk behaviors decrease during MMT, and emphasize the benefits of MMT for public health and HIV/HCV prevention.
A cross-sectional study conducted by Qian et al. (2008) revealed that opioid addicted individuals in MMT were less likely to use or inject drugs, share needles, have multiple sexual partners or have unprotected sex as compared to their counterparts.[26] Similarly, Pang eta al. (2007) demonstrated that the MMT contributed to a reduction in drug use, drug injecting behaviors, drug-related criminal behaviors, and HIV infections.[27] Furthermore, Millson et al. (2007) assessed injection–related HIV risk behavioral changes among opioid users 6 months after enrollment in low-threshold MMT programs in Canada. Results found that the proportion of participants injecting drugs, sharing needles, sharing drug equipment, indirectly sharing and using shooting galleries declined with follow–up for the whole cohort.[18] These findings suggest that low-threshold MMT programs can reduce the risk of HIV risk behaviors.
Moreover, Kerr, marsh, Li, Montaner and Wood (2005) evaluated the correlates of MMT use within a prospectively followed cohort of 1587 IDUs in Vancouver, Canada. The study demonstrated that the use of MMT was associated with reductions in heroin use and HIV risk behavior.[28]
Discussion
We reviewed studies that included data on the influence of MMT on HIV risk behaviors among high-risk injection drug users. Consistent with our hypotheses, we found both direct and indirect associations between use of MMT and risk behaviors. The studies identified in this review, whether controlled trials or other types of study, provide evidence that MMT in IDU is associated with significant reductions in HIV risk behaviors. The studies consistently revealed a decrease in the proportion of participants reporting injecting use, the frequency of injection, the sharing of injecting equipment, and drug-related HIV risk scores. The data from the studies included in this review suggests that substantial reductions in injecting drug use occur in the first six months. Similarly, data also suggest that MMT is associated with a lower likelihood of multiple sex partners or unprotected sex.
Our results support the notion that the use of MMT may influence the degree to which IDUs engage in risky behaviors. Importantly, some studies showed that reduction in drug-related risk behaviors were observed after participating in the MMT, so that the changes in behavior were less likely to be caused by factors other than the MMT.[19–22] Also, one study found the cumulative effect of VCT and MMT on reducing the HIV-related risk behaviors among people who inject drugs.[21] It could be that the psychological counseling, health education, group activities, social support and skills training that were provided along with MMT had some impact for better outcome. Thus, the finding from this review highlights that more attention needs to be given for measures to promote adherence among MMT clients.
Some of the limitations of this systematic review should be acknowledged. First, the review was restricted to peer-reviewed journal articles published in English, which likely biased our collection toward primarily English-speaking countries. The search itself was restricted to one database, although this is unlikely to have been a major limitation as PubMed Central (PMC) is the largest repository research article in the world. In addition, only abstracts were screened for this review to determine whether the study investigated the impact of MMT on HIV risk behavior. Thus, any secondary findings and analyses relevant to our topics of interest not mentioned within the abstracts may have been excluded from this review. Many behaviors were self-reported, thus, recall or social desirability biases might be present. In some studies participants were not randomly allocated to each of the treatment groups as a result of conditional limitations of the participating clinics and related ethical issues.
Although randomized allocation was not carried out, comparisons of drug use and demographic characteristics, such as age, and gender, were found to be not significantly different among groups. In addition, there were significant differences in methadone dosages in the different treatment groups. Some studies reported monthly urine tests instead of weekly tests, which could potentially lower the rate of positive urine tests obtained. Similarly, we included only a limited number of outcome and independent variables in the survey; other important psychosocial measures, such as mental health status as well as structural factors such as social support and social networks were not included. These variables might explain more about the relationship between continued HIV-risk behaviors and MMT characteristics.
Conclusions
The findings of this study indicate that the majority of the available research has shown a close and direct association between the uses of MMT and reduced HIV risk behaviors. There is evidence that MMT is associated with a significant decrease in injecting drug use, sharing of injecting equipment. Evidence on sex-related risk behavior is limited, but suggest that MMT is associated with a lower incidence of multiple sex partners and unprotected sex.[21, 26] The literature also suggests that the most significant factor in reducing HIV risks was treatment adherence. As such, more attention needs to be given in future studies to ensure the higher rates of access to MMT as well as to improve the adherence to MMT.
Acknowledgments
Funding
Funding to support the preparation of the article was provided by a National Institute of Health (NIH) Grant (K02DA033139) to Michael M. Copenhaver.
List of abbreviations
- MMT
methadone maintenance treatment
- IDU
injecting drug user
Footnotes
Conflicting interest
The authors have declared that no competing interests exist.
Author Contributions
Conceived and designed the study: PK, THM, and MC. Analyzed the data: RK, RS, THM, and MC. Wrote the paper: RK, RS, THM, and MC. Proof read the paper: RK, RS, THM, and MC. Final approval: RK, RS, THM, and MC.
References
- 1.UNAIDS. How AIDS changed everything? Geneva, Switzerland: 2015. [Google Scholar]
- 2.Centers for Disease Control and Prevention. HIV Surveillance Report, 2014. Vol. 26. Atlanta, GA: Centers for Disease Control and Prevention; 2014. [Google Scholar]
- 3.Volkow ND. Drug Abuse and HIV. Washington, DC: National Institute of Drug Abuse; 2012. [Google Scholar]
- 4.Cepeda JA, Niccolai LM, Lyubimova A, Kershaw T, Levina O, Heimer R. High-risk behaviors after release from incarceration among people who inject drugs in St. Petersburg, Russia Drug and alcohol dependence. 2015;147:196–202. doi: 10.1016/j.drugalcdep.2014.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mateu-Gelabert P, Guarino H, Jessell L, Teper A. Injection and sexual HIV/HCV risk behaviors associated with nonmedical use of prescription opioids among young adults in New York City. Journal of substance abuse treatment. 2015;48:13–20. doi: 10.1016/j.jsat.2014.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Broz D, Wejnert C, Pham HT, DiNenno E, Heffelfinger JD, Cribbin M, et al. HIV infection and risk, prevention, and testing behaviors among injecting drug users—National HIV Behavioral Surveillance System, 20 US Cities, 2009. MMWR Surveill Summ. 2014;63:1–51. [PubMed] [Google Scholar]
- 7.El-Bassel N, Shaw SA, Dasgupta A, Strathdee SA. Drug use as a driver of HIV risks: re-emerging and emerging issues. Current Opinion in HIV and AIDS. 2014;9:150–155. doi: 10.1097/COH.0000000000000035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Decker MR, Wirtz AL, Baral SD, Peryshkina A, Mogilnyi V, Weber RA, et al. Injection drug use, sexual risk, violence and STI/HIV among Moscow female sex workers. Sexually transmitted infections. 2012;88:278–283. doi: 10.1136/sextrans-2011-050171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aspinall EJ, Nambiar D, Goldberg DJ, Hickman M, Weir A, Van Velzen E, et al. Are needle and syringe programmes associated with a reduction in HIV transmission among people who inject drugs: a systematic review and meta-analysis. International journal of epidemiology. 2014;43:235–248. doi: 10.1093/ije/dyt243. [DOI] [PubMed] [Google Scholar]
- 10.Bärnighausen T, Salomon JA, Sangrujee N. HIV treatment as prevention: issues in economic evaluation. PLoS medicine. 2012;9:891. doi: 10.1371/journal.pmed.1001263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nachega JB, Mugavero MJ, Zeier M, Vitória M, Gallant JE. Treatment simplification in HIV-infected adults as a strategy to prevent toxicity, improve adherence, quality of life and decrease healthcare costs. Patient preference and adherence. 2011;5:357. doi: 10.2147/PPA.S22771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization. Global update on HIV treatment 2013: results, impact and opportunities. 2013. [Google Scholar]
- 13.Booth RE, Campbell BK, Mikulich-Gilbertson SK, Tillotson CJ, Choi D, Robinson J, et al. Reducing HIV-Related Risk Behaviors Among Injection Drug Users in Residential Detoxification. AIDS and behavior. 2011;15:30–44. doi: 10.1007/s10461-010-9751-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.MacArthur GJ, Minozzi S, Martin N, Vickerman P, Deren S, Bruneau J, et al. Opiate substitution treatment and HIV transmission in people who inject drugs: systematic review and meta-analysis. Bmj. 2012:345. doi: 10.1136/bmj.e5945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hedrich D, Alves P, Farrell M, Stöver H, Møller L, Mayet S. The effectiveness of opioid maintenance treatment in prison settings: a systematic review. Addiction. 2012;107:501–517. doi: 10.1111/j.1360-0443.2011.03676.x. [DOI] [PubMed] [Google Scholar]
- 16.Otiashvili D, Piralishvili G, Sikharulidze Z, Kamkamidze G, Poole S, Woody GE. Methadone and buprenorphine-naloxone are effective in reducing illicit buprenorphine and other opioid use, and reducing HIV risk behavior—outcomes of a randomized trial. Drug and alcohol dependence. 2013;133:376–382. doi: 10.1016/j.drugalcdep.2013.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lambdin BH, Masao F, Chang O, Kaduri P, Mbwambo J, Magimba A, et al. Methadone Treatment for HIV Prevention-Feasibility, Retention and Predictors of Attrition in Dar es Salaam, Tanzania: A Retrospective Cohort Study. Clinical Infectious Diseases. 2014:ciu382. doi: 10.1093/cid/ciu382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Millson P, Challacombe L, Villeneuve PJ, Strike CJ, Fischer B, Myers T, et al. Reduction in injection-related HIV risk after 6 months in a low-threshold methadone treatment program. AIDS Educ Prev. 2007;19:124–136. doi: 10.1521/aeap.2007.19.2.124. [DOI] [PubMed] [Google Scholar]
- 19.Wang L, Wei X, Wang X, Li J, Li H, Jia W. Long-term effects of methadone maintenance treatment with different psychosocial intervention models. PLoS One. 2014;9:e87931. doi: 10.1371/journal.pone.0087931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen W, Xia Y, Hong Y, Hall BJ, Ling L. Predictors of continued HIV-risk behaviors among drug users in methadone maintenance therapy program in China--a prospective study. Harm Reduct J. 2013;10:23. doi: 10.1186/1477-7517-10-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang M, Mao W, Zhang L, Jiang B, Xiao Y, Jia Y, et al. Methadone maintenance therapy and HIV counseling and testing are associated with lower frequency of risky behaviors among injection drug users in China. Subst Use Misuse. 2015;50:15–23. doi: 10.3109/10826084.2014.957768. [DOI] [PubMed] [Google Scholar]
- 22.Pettes T, Wood E, Guillemi S, Lai C, Montaner J, Kerr T. Methadone use among HIV-positive injection drug users in a Canadian setting. J Subst Abuse Treat. 2010;39:174–179. doi: 10.1016/j.jsat.2010.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Corsi KF, Lehman WK, Booth RE. The effect of methadone maintenance on positive outcomes for opiate injection drug users. J Subst Abuse Treat. 2009;37:120–126. doi: 10.1016/j.jsat.2008.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Willner-Reid J, Belendiuk KA, Epstein DH, Schmittner J, Preston KL. Hepatitis C and human immunodeficiency virus risk behaviors in polydrug users on methadone maintenance. J Subst Abuse Treat. 2008;35:78–86. doi: 10.1016/j.jsat.2007.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Palepu A, Tyndall MW, Joy R, Kerr T, Wood E, Press N, et al. Antiretroviral adherence and HIV treatment outcomes among HIV/HCV co-infected injection drug users: the role of methadone maintenance therapy. Drug Alcohol Depend. 2006;84:188–194. doi: 10.1016/j.drugalcdep.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 26.Qian HZ, Hao C, Ruan Y, Cassell HM, Chen K, Qin G, et al. Impact of methadone on drug use and risky sex in China. J Subst Abuse Treat. 2008;34:391–397. doi: 10.1016/j.jsat.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 27.Pang L, Hao Y, Mi G, Wang C, Luo W, Rou K, et al. Effectiveness of first eight methadone maintenance treatment clinics in China. Aids. 2007;21(Suppl 8):S103–107. doi: 10.1097/01.aids.0000304704.71917.64. [DOI] [PubMed] [Google Scholar]
- 28.Kerr T, Marsh D, Li K, Montaner J, Wood E. Factors associated with methadone maintenance therapy use among a cohort of polysubstance using injection drug users in Vancouver. Drug Alcohol Depend. 2005;80:329–335. doi: 10.1016/j.drugalcdep.2005.05.002. [DOI] [PubMed] [Google Scholar]