To the Editor
We report the 10-year survival rates in the first cohort of patients with AIDS who consecutively initiated antiretroviral therapy (ART) in Port-au-Prince, Haiti. A total of 910 patients 13 years of age or older who initiated ART from 2003 through 2004 were followed for 10 years; the initiation of ART and follow-up care were performed in accordance with World Health Organization (WHO) guidelines.1 Details regarding this cohort have been reported previously, and ethics approval for the retrospective study was received from the relevant institutional review boards.2,3 Death was ascertained from medical records. Data from patients who transferred to another clinic were censored at the time of the transfer. Loss to follow-up was defined as the absence of a clinic visit within 180 days before the 10-year follow-up date.
Three methods were used to assign survival status to patients who were lost to follow-up and to estimate the 10-year survival rate: Kaplan–Meier analysis censors patient data at the time of the loss to follow-up, inverse-probability weighting uses contact-tracing data, and multiple imputation estimates survival on the basis of baseline characteristics among those who are lost to follow-up. Cox modeling was used to identify the characteristics associated with 10-year survival (see the Supplementary Appendix, available with the full text of this letter at NEJM.org, for further details).
Among the 910 patients at baseline, 504 (55%) were female, the median age was 39 years, and the median CD4 count was 131 cells per cubic millimeter (interquartile range, 51 to 212). Approximately half the patients lived in extreme poverty, earning less than $1 (in U.S. dollars) per day.
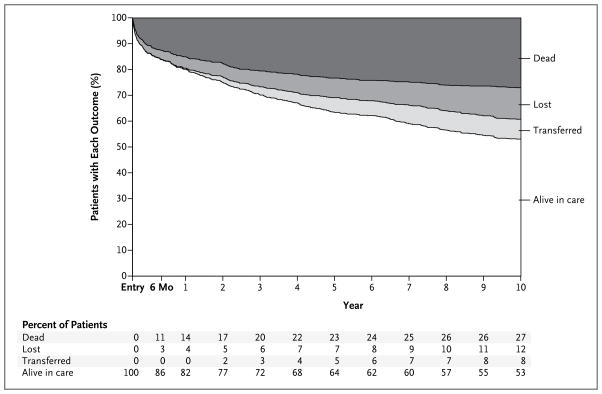
Ten years after ART initiation, 482 patients (53%) were alive in care, 246 (27%) were dead, 111 (12%) were lost to follow-up, and 71 (8%) had transferred to another clinic (Fig. 1). The estimates of the 10-year survival rate calculated by means of the three methods were similar: 71% (95% confidence interval [CI], 68 to 74) by the Kaplan–Meier method, 63% (95% CI, 59 to 67) by inverse-probability weighting, and 67% (95% CI, 64 to 71) by multiple imputation.
Figure 1.
Outcomes over 10 Years of Follow-up among 910 Patients Who Initiated Antiretroviral Therapy from 2003 through 2004 in Haiti.
Of the deaths that occurred, 42% were in the first 6 months; death within this period was associated with being male, being older than 50 years of age, being in the lowest weight quartile according to sex, having WHO stage III or IV disease, and having active tuberculosis (P<0.05 for all comparisons). The characteristics associated with death occurring after 6 months through 10 years were being older than 50 years of age, having an income of less than $1 per day, being in the lowest weight quartile, and being in the lowest quartile for adherence to therapy (see the Supplementary Appendix) (P<0.05 for all comparisons). The mortality rate in the year after the 2010 earthquake did not differ significantly from those in other years.
Among the 482 patients who were alive at 10 years, 351 (73%) continued to receive firstline therapy, and 178 (37%) had a noncommunicable disease (109 patients had cardiovascular disease, 67 had lung disease, and 2 had diabetes).
The 10-year survival rate estimate of 63 to 71% in one of the first large cohorts of patients receiving ART in the developing world — a large proportion of whom had advanced AIDS at the time of ART initiation — is similar to that among patients in the early era of ART in the United States.4 Our results indicate the long-term sustainability of international efforts to provide ART in resource-poor settings.
Supplementary Material
Acknowledgments
Supported by grants from the National Institutes of Health (AI098627, TW009337, and TW010062) and the President’s Emergency Plan for AIDS Relief, Centers for Disease Control and Prevention (GGH000545).
Footnotes
A complete list of authors is available with the full text of this letter at NEJM.org.
Disclosure forms provided by the authors are available with the full text of this letter at NEJM.org.
Contributor Information
Samuel Pierre, Groupe Haïtien d’Etude du Sarcome de Kaposi et des Infections Opportunistes (GHESKIO), Port-au-Prince, Haiti
Deanna Jannat-Khah, Weill Cornell Medical College, New York, NY
Daniel W Fitzgerald, Weill Cornell Medical College, New York, NY
Jean William Pape, GHESKIO, Port-au-Prince, Haiti
Margaret L McNairy, Email: mam9365@med.cornell.edu, Weill Cornell Medical College, New York, NY
References
- 1.Antiretroviral therapy for HIV infection in adults and adolescents: recommendations for a public health approach, 2006 revision. Geneva: World Health Organization; 2006. [PubMed] [Google Scholar]
- 2.Severe P, Leger P, Charles M, et al. Antiretroviral therapy in a thousand patients with AIDS in Haiti. N Engl J Med. 2005;353:2325–34. doi: 10.1056/NEJMoa051908. [DOI] [PubMed] [Google Scholar]
- 3.Leger P, Charles M, Severe P, Riviere C, Pape JW, Fitzgerald DW. 5-Year survival of patients with AIDS receiving antiretroviral therapy in Haiti. N Engl J Med. 2009;361:828–9. doi: 10.1056/NEJMc0809485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crum NF, Riffenburgh RH, Wegner S, et al. Comparisons of causes of death and mortality rates among HIV-infected persons: analysis of the pre-, early, and late HAART (highly active antiretroviral therapy) eras. J Acquir Immune Defic Syndr. 2006;41:194–200. doi: 10.1097/01.qai.0000179459.31562.16. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.