Abstract
The Screening, Brief Intervention and Referral to Treatment (SBIRT) model is widely recommended as part of routine visits in pediatric primary care despite a dearth of evidence on its effectiveness, feasibility, and developmental appropriateness for adolescents in this setting. The purpose of this article is to explicate ways that SBIRT may be tailored to better serve adolescents in primary care under a set of recommended adaptations that we refer to collectively as SBIRT-A or Screening, Brief Intervention, and Referral to Treatment for Adolescents. Each component of the SBIRT-A framework incorporates recommendations to optimize developmental fit with adolescents based on extant empirical research, developmental theory, and well-documented barriers to service delivery in primary care. Commonalities across proposed adaptations include reliance upon proactive methods to identify and engage youth; innovation in service delivery aimed at improving the consistency and reach of interventions; and a family-focused approach to engagement, assessment, and intervention. Specific recommendations include taking advantage of every clinical encounter with the family to screen, involving caregivers in assessments and brief interventions, leveraging technology to administer brief interventions and booster sessions, and patient- and family-centered procedures for treatment referral and engagement. The adaptations proposed in this article have the potential to enhance the detection of adolescents with SU problems in primary care, the consistency of intervention provision, and engagement of this typically recalcitrant population into appropriate treatment.
Keywords: SBIRT, adolescent, substance use, primary care
1. Introduction
A perennial theme across research literatures pertaining to adolescent health is the magnitude of unmet need for treatment among adolescents with substance use disorders (SUDs) in the United States. Data from the 2013 National Survey on Drug Use and Health (Substance Abuse and Mental Health Services Administration [SAMHSA], 2014) indicates that among approximately 1.3 million adolescents who met diagnostic criteria for an SUD during the past year (5.2% of adolescents), only 9.1% received specialty SUD treatment. These service utilization figures have remained stubbornly persistent over the last decade and beyond and quantify the “treatment gap” for adolescent substance use (ASU; see Merikangas et al., 2011). The ASU treatment gap remains one of most serious public health issues in the U.S. given the propensity for untreated substance use (SU) problems during adolescence to persist into adulthood, thereby precipitating a cascade of health consequences and imparting enormous economic costs to society (CASA Columbia, 2011; National Drug Intelligence Center, 2011).
Perhaps the most widely endorsed and disseminated approach for addressing the ASU treatment gap is Screening, Brief Intervention, and Referral to Treatment (SBIRT; Babor et al., 2007; SAMHSA, 2013). SBIRT is both a public health model and a set of procedures for detecting individuals in the general population at risk of SUDs and administering appropriate prevention, early intervention, or treatment referral. The SBIRT model entails universal screening (S) of patients’ level of risk for SUD and formulaic guidelines for brief intervention (BI) and/or referral to treatment (RT). Services are targeted toward individuals who have initiated SU in order to provide opportunities for early intervention prior to the need for more extensive or specialized treatment (SAMHSA, 2013). Implementation of SBIRT has recently been bolstered by the enactment of the Affordable Care Act (ACA), which mandates that commercial insurance plans as well as Medicaid/Medicare fully cover the costs of SU screening and brief behavioral counseling during routine primary care (PC) visits, thereby paving the way for new reimbursement mechanisms to fund SBIRT in PC and other medical settings (see American Medical Association, 2015; Levy & Kokotailo, 2011).
To date, SBIRT has been implemented predominantly with adult patients in PC and emergency rooms (SAMHSA, 2013). Empirical evaluations of the effectiveness of SBIRT for this population have yielded promising though far from definitive results (Agerwala & McCance-Katz, 2012; Babor et al., 2007). The U.S Preventive Services Task Force (USPSTF) has deemed the evidence in support of SBIRT sufficient to recommend its routine use to identify risky alcohol consumption among adults in PC (Moyer, 2013). Data on the utility of SBIRT for addressing relatively severe alcohol use or illicit drug use among adults in PC are less compelling, however (Roy-Byrne et al., 2014; Saitz et al., 2014).
The evidence base in support of SBIRT for adolescents in PC and other settings is more equivocal than that pertaining to adults. A recent review of the empirical literature on SBIRT with adolescent populations by Mitchell and colleagues (2013) identified a total of seven randomized clinical trials (RCTs) conducted in emergency departments and seven conducted in schools settings, with the majority of studies in each setting finding little or inconclusive evidence of the benefits of SBIRT over control or comparison conditions (e.g., assessment only, brief informal advice, etc.; see also Patton et al., 2014).
At the current juncture, few randomized trials of SBIRT have been conducted with adolescents in PC. Existing evidence is inconclusive for gauging the model’s effectiveness in reducing SU and facilitating treatment entry among teens at moderate to high levels of risk for SUD (Mitchell, Gryczynski, O’Grady, & Schwartz, 2013; Patnode et al., 2014; Yuma-Guerrero et al., 2012). Accordingly, SBIRT is not currently endorsed by the USPSTF as an empirically supported approach for addressing ASU in pediatric PC settings (Moyer, 2013). Nonetheless, reviews of SBIRT acknowledge the model’s potential benefits for adolescents (see Mitchell et al., 2013), and it has been championed for use within this age group by virtually every major behavioral health organization including the American Academy of Pediatrics (AAP; Levy & Kokotailo, 2011), American Medical Association (AMA; 2015), National Institute on Alcohol Abuse and Alcoholism (NIAAA; 2011), National Institute on Drug Abuse (2014), and SAMHSA (2013). In addition, the Addiction Technology Transfer Center Network offers an array of online training materials for implementing SBIRT with adolescents (see http://attcnetwork.org/national-focus-areas/?rc=sbirt); both the AAP (Levy & Kokotailo, 2011) and NIAAA (2011) have provided written guidance on SBIRT for physicians; and medical residency programs have begun to provide formal training in implementing SBIRT with adolescents in PC (Schram et al., 2014; Whittle, Buckelew, Satterfield, Lum, & O’Sullivan, 2014).
1.2. Adapting SBIRT for Adolescents
Despite broad-based support for SBIRT in pediatric PC, questions persist regarding the model’s effectiveness, feasibility, and developmental appropriateness for adolescents (Clark & Moss, 2010). Moreover, the aforementioned resources for physicians tend to focus primarily on implementing SU screening procedures in a developmentally sensitive manner with relatively less attention to engaging, intervening with, and referring youth to treatment. In order to address such concerns and resource gaps, this article recommends a set of adaptations to the traditional SBIRT model to more effectively serve adolescent populations. We refer to these adaptations collectively as SBIRT-A. The recommendations in this article stem from the current evidence base regarding the efficacy of SBIRT for adolescents, guidelines for clinical intervention with adolescents based on developmental theory and research, and well-documented barriers to the delivery of substance use screening and intervention services in PC settings. Primary themes across adaptations include: reliance upon proactive (versus reactive) methods to identify and engage youth; innovation in service delivery aimed at improving the consistency and reach of interventions; and a family-focused approach to engagement, assessment, and intervention.
Although the SBIRT-A framework may be generalized for implementation in a variety of gateway service settings in which adolescents and their caregivers are encountered (e.g., PC, school, child welfare, and juvenile justice), this article focuses on implementing SBIRT-A in pediatric PC clinics. It is estimated that approximately one-third of adolescents encountered during PC visits exhibits moderate to high probability of recent SU (Bohnert et al., 2014). Given that the majority of teens in the U. S. visit PC clinics at least once per year (Nordin, Solberg, & Parker, 2010), PC clinics provide rich opportunities to detect and intervene with adolescents at risk for SUD. It is widely recognized, however, that due to both general and adolescent-specific barriers such opportunities go largely unrecognized in pediatric PC (Sterling, Weisner, Hinman, & Parthasarathy, 2010; Van Hook et al., 2007). In light of this reality, this article introduces the SBIRT-A framework by describing optimal screening, brief intervention, and treatment referral procedures for adolescents in pediatric PC settings. Specifically, it highlights concerns with the SBIRT status quo for adolescents and proposes developmentally informed adaptations that may bolster the model’s effectiveness in detecting adolescents at risk for SUD, administering appropriate BIs, and engaging this typically recalcitrant population into appropriate treatment.
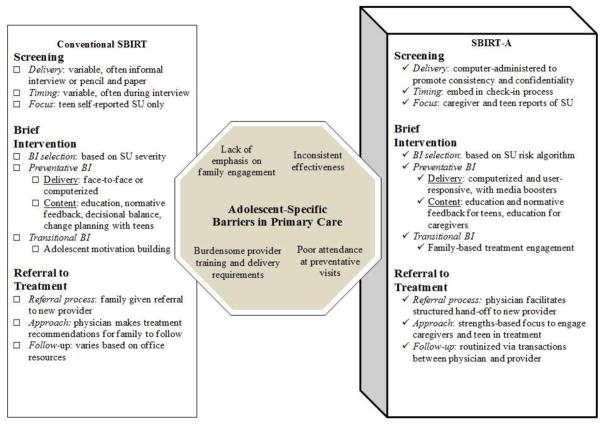
Figure 1 presents an overview of the recommended adaptations contained in the SBIRT-A framework. The recommendations are designed specifically for adolescents between ages 11 and 17 years for three reasons: (a) prevailing guidelines for PC physicians recommend universal SU screening for youth age 11 and older (AMA, 2015; Hagan, Shaw & Duncan, 2008); (b) USPSTF guidelines for adolescents apply to youth under the age of 18 (Moyer, 2014); and (c) age 18 is the point at which youth typically transition from pediatric to adult PC. In the following sections, we identify developmental concerns with each component of the traditional SBIRT model and discuss how the proposed adaptations within SBIRT-A address adolescent-specific barriers in PC.
Figure 1.
Adaptation of Conventional SBIRT components to SBIRT-A in order to Address Adolescent-Specific Barriers in Primary Care.
2. Screening
Screening is the first component of SBIRT-A and is the foundation upon which the other components depend. Historically, screening for ASU in PC has been recommended during annual preventive or well-child exams (see Elster, 1997). Such recommendations have been updated recently based on data indicating that adolescents are less likely to attend preventative visits than adults and younger children (Nordin et al., 2010; Rand et al., 2007), as well as data demonstrating that adolescents are more likely to screen positive for SU during acute care visits than well-child exams (Knight et al., 2007). As such, the most recent guidelines issued by the AAP prescribe universal SU screening for adolescents during both routine preventative appointments and non-preventative visits (Levy & Kokotailo, 2011).
Prevailing recommendations for universal SU screening include the use of time-efficient, developmentally appropriate, and well-validated screening tools that can be administered with minimal staff burden and that provide guidelines for steps to follow subsequent to screening (see Wissow et al., 2013). A number of screening tools for ASU exist, with briefer instruments generally being preferred due to the time constraints faced by PC practitioners and the desire to reserve more lengthy assessments for adolescents at elevated levels of risk (Levy & Koktailo, 2011). The 2011 AAP guidelines recommend the routine use of the 6-item CRAFFT screener (Knight, Sherritt, Harris, Gates, & Chang, 2002). A recent study by Levy and colleagues (2014), however, found that a single screening question (i.e., “How often have you used [specific drug] over the past year…”) is as effective as the full CRAFFT in triaging adolescents into four risk categories including: no risk (no history of use), mild risk (history of past year use), moderate risk (history of monthly use), and severe risk (history of weekly use). Such a brief screening strategy is consistent with the single-item screen promoted for adults (see Saitz et al., 2014) and with NIAAA’s (2011) youth alcohol screening guide which recommends that patient SU risk level be triaged based on frequency of past-year alcohol use.
Despite broad dissemination of these guidelines, screening for SU among adolescents in PC remains far from universal (see AAP, 1998; Sterling et al., 2010). Surveys of PC physicians suggest that less than half routinely screen adolescents for SU (Millstein & Marcell, 2003), with even lower rates in rural or impoverished regions (Gordon, Ettaro, Rodriguez, Mocik, & Clark, 2011). Among clinicians who regularly screen, over 50% report using “informal” screening methods rather than validated screening tools raising concerns about accurate detection (Harris et al., 2012a). One large study found that PC pediatricians conducting informal screening identified only 63% of adolescents with SU, with the lowest detection rates being observed for youth with the most serious SU problems (Wilson, Sherritt, Gates, & Knight, 2004). Such low rates of ASU detection (i.e., false negative rates) in PC underscore a myriad of barriers affecting physicians’ capacity to accurately and effectively conduct SU screening (with both adolescents and adults) including time constraints, logistical hurdles, discomfort with screening, low self-efficacy, and lack of motivation (see Sterling, Kline-Simon, Wibbelsman, Wong, & Weisner, 2012).
2.1 Adolescent-Specific Considerations for Screening
Among adolescents, several developmental factors pose formidable barriers to consistent and effective SU screening. First, adolescents in PC settings are likely to experience heightened concerns regarding the confidentiality of information revealed during SU screening and therefore may be prone to under-report or deny SU behavior (Ford, Millstein, Halpern-Felsher, & Irwin, 1997). Along these lines, studies have shown that the validity of adolescent self-report data is more sensitive to administration mode than adult data, with modes viewed as being less secure and confidential yielding less accurate results (see Brener, Billy, & Grady, 2003). An additional limiting factor to effective screening of adolescents in PC is that predominant SBIRT approaches do not incorporate caregivers in the S portion of the model, despite evidence indicating that utilizing multiple sources of information to detect SU among adolescents is more accurate than relying on any single source (Weissman et al., 1987; Winters, 1999).
The aforementioned issues suggest that the predominant approach of relying solely on adolescent self-report of SU behavior and involvement, often obtained via interviews or pencil-and-paper questionnaires, is likely to result in substantial missed opportunities to detect and intervene with youth in PC. Accordingly, the SBIRT-A framework espouses a no missed opportunities approach to SU screening (see Knight et al., 2007; Nordin et al., 2010) which incorporates caregivers in screening procedures and uses technology to embed screening instruments into the check-in process and to promote and assure confidentiality.
2.2. S Adaptation #1: Include Caregivers
The no missed opportunities paradigm recognizes caregivers as vital sources of information about adolescent SU risk. The SBIRT-A framework recommends that while adolescents complete brief empirically validated screens (either the CRAFFT or a single-item screen), caregivers also complete a brief screening instrument to provide a collateral report of adolescent SU over the past year. This conjoint approach to screening serves to increase the likelihood of case detection and to set the stage for caregiver involvement in subsequent components of the SBIRT-A model.
To optimize reach, the SBIRT-A framework prescribes that PC personnel administer screening tools to caregivers during every clinical encounter regardless of the target patient (caregiver, adolescent, sibling) or objective of the visit (preventative or non-preventative). For example, a mother of an adolescent could be administered a brief screening measure regarding ASU whenever she presented to the PC office regardless of whether the appointment is for herself or her teen. If the mother’s responses to the screener indicated moderate to severe risk of ASU, then the full SBIRT-A protocol could be implemented during the scheduled visit if the adolescent were present or during a follow-up visit if the adolescent were not present at the time of caregiver screening.
There has been limited research on the accuracy of caregiver reports of ASU, although evidence suggests that parental reports are fair-to-good proxy measures of ASU behavior (Ciesla, Spear, & Skala, 1999; McGillicuddy, Rychtarik, Morsheimer, & Burke-Storer 2012). As such, administering empirically validated SU screening tools to caregivers could help to more accurately triage adolescents into risk categories and increase early identification of adolescents who have initiated SU. Few well-validated caregiver measures of ASU currently exist, however, rendering caregiver screening a priority for future research on the SBIRT-A framework.
2.3. S Adaptation #2: Use Technology to Embed SBIRT-A into Check-In
Achieving the no-missed-opportunities threshold is likely to require that SU screening becomes a routine aspect of PC for adolescents. Therefore, the SBIRT-A approach encourages PC providers to embed screening into check-in procedures fronting every family visit using technology-based screening tools. Although paper-and-pencil measures are viable for this purpose, electronically administered screening via desktop or laptop computers, smart pads, or hand-held electronic devices may be superior for several reasons. Foremost, evidence suggests that adolescents perceive computer-administered SU screens to be more confidential than paper-and-pencil and/or interview screening formats, and therefore may provide more valid and accurate responses on technology-based screens (Pedersen, Grow, Duncan, Neighbors, & Larimer, 2012). Indeed, studies suggest that adolescents tend to report higher levels of SU frequency using computer-administered assessment tools compared to more traditional screening methods and modalities (e.g., Turner et al., 1998). Furthermore, adolescents are likely to prefer computer-administered screening over more traditional formats given the generally high levels of familiarity and aptitude with technology characterizing this age group (Madden, Lenhart, Duggan, Cortesi, & Gasser, 2013). Additionally, for PC staff the use of electronically administered screening may reduce administrative burden, decrease the likelihood of missed or inaccurate screens, facilitate incorporation of screening results into electronic medical records, and enable instantaneous scoring which can inform the BI and RT components of the framework (see Anand, Carroll, & Downs, 2012; Gadomski et al., 2015; Olson, Gaffney, Hedberg, & Gladstone, 2009).
Embedding screening into the check-in process rather than at other points during a PC visit may be advantageous by serving to routinize screening as part of usual intake procedures. Such an approach may reduce perceived stigma associated with SU screening by ensuring that adolescents don’t feel “singled out” as being under suspicion of SU (see Wissow et al., 2013). Administering screening measures during check-in is also consistent with standard practice in many PC offices, as well as recent empirical evaluations (Levy et al., 2014), thereby potentially enhancing feasibility and acceptability of SU screening among staff and patients alike.
3. Brief Intervention
Results of adolescent and caregiver screening procedures during the S phase inform the manner in which adolescents and caregivers progress to the BI component of SBIRT-A. Consistent with the AAP’s 2011 guidelines, the SBIRT-A framework recommends that adolescents reporting no history of SU (corroborated by caregiver report) receive positive feedback to reinforce continued abstinence whereas all other adolescents receive some form of BI. Although there is no widely accepted definition of what constitutes a BI across clinical service settings, such interventions are generally time-limited (ranging from one to five sessions of 5 to 60 minutes in duration), structured, and goal-directed (Winters, Leitten, Wagner, & O’Leary Tevyaw, 2007). Consistent with the traditional SBIRT model, SBIRT-A stipulates that adolescents at mild-to-moderate SUD risk (defined as substance use less than once per month over the past year) should receive a brief preventative BI to increase motivation to reduce or abstain from SU, whereas those at moderate-to-severe SUD risk (defined as substance use once or more per month over the past year) should receive a BI paired with RT.
A primary reason that the traditional SBIRT model gained traction so rapidly in the SU treatment field was the bold promise of the BI component for promoting substantive changes in treatment motivation and SU outcomes at modest clinical cost. However, as the evidence base has grown in size and rigor, enthusiasm for BI effectiveness has tempered proportionately. For adults in PC, studies early in the decade found that BIs reliably lowered alcohol consumption among men up to one-year follow-up (Kaner et al., 2007). But two recent large-scale trials reported that BI failed to outperform usual care for reducing either SU or use-related consequences among PC patients with severe SU (Roy-Byrne et al., 2014; Saitz et al., 2014). These results prompted a reluctant call “back to the drawing board” (Hingson & Compton, 2014) in order to (re)design BIs for PC that are both sustainable in standard practice and a demonstrable upgrade in effectiveness, especially for more severe SU problems.
3.1. Adolescent-Specific Considerations for Brief Intervention
For adolescents at risk for SUD, a central concern with implementing BIs in PC and elsewhere is inconsistent empirical support for their effectiveness. For example, one recent meta-analysis concluded that BIs led to significant if modest reductions in alcohol use and related problems up to one year post- treatment (Tanner-Smith & Lipsey, 2015). Yet a comprehensive review of randomized trials of motivational interviewing (MI), which is the clinical centerpiece of virtually every BI, labeled it probably efficacious for ASU with an equivalent number of successes and failures, leaving unclear whether stand-alone MI is routinely potent for effecting long-term reductions in alcohol or drug use (Hogue, Henderson, Ozechowski, & Robbins, 2014). In PC settings, BIs remain minimally tested as either a direct intervention for ASU or a motivational segue to treatment services; moreover, the few existing BI studies have varied widely in the length, number of sessions, and content of the intervention, with the majority focusing on alcohol use and not addressing illicit drug use (Mitchell et al., 2013; Tanner-Smith & Lispey, 2015). Given the recent disappointing results of BI among adults in PC and the ensuing call back to the drawing board, it is an ideal time to adapt BI to meet the unique developmental needs of adolescents. Accordingly this section offers a revised blueprint consisting of four transformations for incorporating BIs within the SBIRT-A framework to meet the SU intervention needs of adolescents and physicians.
3.2. BI Adaptation #1: Utilizing Risk Algorithms to Select BIs
As previously noted, BIs for adolescents comprise two distinct types serving overlapping functions: (1) preventative interventions to inhibit SU escalation and reduce SU consequences among those with mild-to-moderate SU; or (2) transitional interventions to link those with moderate-to-severe SU to more extensive treatment. SU risk profiling, used to determine which patients receive which type of BI (see Turner, Spithoff, & Kahan, 2014), is therefore a cornerstone feature of efficient SBIRT-A implementation. Once an adolescent screens positively for SUD risk, complementary data can be collected at the initiation of the BI phase to support SUD risk profiling, which we contend should include at least three dimensions (in addition to age). The first is SUD risk severity: a function of SU type, amount, and method of ingestion. Profiling SUD risk severity is supported by recent revisions to the Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 2013) that stipulate symptom thresholds for categorizing SUD diagnoses as mild, moderate, or severe. The second dimension is SUD protection, to be derived from brief assessment of an adolescent’s personal, family, and environmental strengths, including well-known caregiver protective factors such as monitoring, closeness to the child, and attitudes towards SU (see Oliver, Cress, Savolainen, & Epstein, 2014; Vakalahi, 2001; Wills & Yaeger, 2003). The third dimension is readiness to change SU behavior. Tools that assess readiness to change are invariably rooted in the stages of change framework (see Prochaska, DiClemente, & Norcross, 1992), which postulates a malleable sequence of SU behavior change: pre-contemplation, contemplation (recognizing SU problems), preparation (desiring help for SU problems), action (seeking and engaging in SU treatment), and maintenance.
The most promising option for assessing readiness to change in PC settings may be contemplation ladders that present single-choice, visual analogue scales depicting a ladder whose higher rungs represent greater levels of readiness (Biener & Abrams, 1991). Contemplation ladders provide a single continuous metric of motivation to change problematic behavior and have shown solid psychometric properties in smoking and SU populations (Hogue, Dauber, & Morgenstern, 2010). For adolescents, ladders have shown construct validity among smokers (Stephens, Celluci, & Gregory, 2004) and predictive validity for both treatment utilization and drug use consumption among marijuana users (King, Chung, & Maisto, 2009; Slavet et al., 2006). Thus they have great potential utility as robust and cost-efficient tools to support intervention tailoring for adolescents in various sectors of care.
Data from these three dimensions—SUD risk severity, protection, and change motivation—can be formulaically converted into “risk algorithms” that determine which BI models or components should be delivered to adolescents reporting which profiles of SU risk. The goal of producing multidimensional risk profiles is ambitious yet achievable if progress accelerates in (1) developing brief and valid tools for measuring SUD risk in pediatric settings and (2) articulating pediatric-specific risk algorithms that offer optimal reliability and utility in stratifying youth to receive preventative versus transitional BIs, as well as monitoring their risk status and re-stratifying as needed over the course of continuous PC visits. Of course the feasibility of assessing risk in busy outpatient settings and calculating age-appropriate algorithms is a central concern. Although risk algorithms generated from brief screening tools can be readily depicted in printed reference tables, we recommend that pediatric offices employ widely available computer-based assessment software (see section below) to streamline the assessment and calculation process. Once established, risk algorithms can provide a data-based complement to clinical judgment, or perhaps drive BI decision-making altogether.
3.3. BI Adaptation #2: Delivering Computer-Based Interventions
To accommodate the multifaceted BI sequence of processing risk algorithms, assigning patients to best-fit BIs, monitoring risk profiles longitudinally, and implementing BIs with fidelity (which can be particularly challenging for PC providers; Dunn et al., 2015), PC practices are advised to adopt computer-based intervention platforms. Face-to-face BI sessions grounded in MI techniques require about 30–45 minutes (Clark & Moss, 2010)—although brief advice sessions can be completed in 5–20 minutes (e.g., D’Onofrio et al., 2008) —on top of time needed to review the risk profile of each patient. Computer-delivered BIs are designed to reduce practitioner burden, minimize provider differences in implementation fidelity, maximize information processing efficiency, and allow self-guided and response-sensitive intervention delivery (Carey, Scott-Sheldon, Elliot, Garey, & Carey, 2012). The initial wave of effectiveness studies on computer-based SBIRT for adolescents indicates that computerized BIs perform comparably to face-to-face versions, producing beneficial effects on SU in some but not all studies (Harris et al., 2012b; Tanner-Smith & Lipsey, 2015; Walton et al. 2013).
In addition to reduced physician burden, the largest potential benefit of computerized BI is the capacity to tailor the selection and duration of BI components based on real-time adolescent response to ongoing intervention. Although the added value of tailored versus non-tailored BI has not been rigorously tested in any age group, the possibilities are highly appealing. For example, animated SU psychoeducation programs can selectively deliver variations in advice-giving options or role-play scenarios depending on successive respondent choices (e.g., Curtis et al., 2014; Levy & Kokalito, 2011; Walton et al., 2013), so that each adolescent experiences a personalized and dynamic curriculum. The next section describes BI content and procedures that appear especially promising for adolescents in PC.
3.4. BI Adaptation #3: Emphasizing Psychoeducation
Cumulative wisdom from BI studies in adolescents, in line with those targeting adults, recommends that certain BI elements be emphasized in locations other than SU specialty treatment. A mainstay, cost-effective feature of youth behavioral health interventions of all kinds is psychoeducation (PE) about the nature of the disorder, individual and family factors that impact the disorder, and clarification about service needs and options (Hoagwood, 2010). PC clinics are ideal settings for PE on ASU such as normative feedback (comparing a given patient’s consumption to national norms in similarly aged peers) and didactics on neurobiological effects and developmental risks (Turner et al., 2014). ASU education and personalized feedback are pillars of one-session BIs that have shown effects for deterring SU in multiple contexts, including schools (Carney, Myers, Louw, & Okwundu, 2014) and pediatric care (Harris et al., 2012b). Another BI staple, decisional balance, has mixed support. Decisional balance interventions prompt patients to carefully consider the positive and negative personal impacts of SU and specify the cost/benefit ratio that leads to consumption (Mitchell et al., 2013). Such interventions are intended to encourage ambivalence about SU as a prelude to therapeutic negotiation culminating in change commitment. One recent meta-analysis of interventions for college drinking (Carey et al., 2012) found that decisional balance was one of few MI components associated with poor outcomes whereas a second (Tanner-Smith & Lipsey, 2015) determined that decisional balance and goal-setting for high-school age drinking were as potent as norm-referencing and personalized feedback. At this juncture it seems prudent to omit decisional balance interventions from time-limited BI sessions (i.e., fewer than 15 allotted minutes) in PC clinics (Walton et al., 2013).
3.5. BI Transformation #4: Involving Caregivers
As discussed previously, the family confers important risk and protective factors for adolescent SUD. A handful of studies on family-focused BIs in high school settings (e.g., Winters, et al., 2007, 2012) and pediatric settings (Gayes & Steele, 2014) demonstrate that BIs incorporating caregivers have added value over adolescent-only BIs. To balance the value of family involvement with the need for adolescent confidentiality, we recommend expanding BIs to caregivers by providing them with basic PE on ASU (though not feedback about their adolescent’s SUD risk). A computerized caregiver PE module would present minimal burden to PC staff as well as set the stage for family involvement in transitional BIs for adolescents whose high-risk status warrants treatment referral (described in next section). As with adolescents, the content could be made personal and dynamic based on caregiver data from the S phase and their interaction with the PE. To our knowledge, no computerized programs are currently available that cover all of the recommended screening and BI content described here, suggesting that development of such a program is a priority for future tests of the SBIRT-A framework.
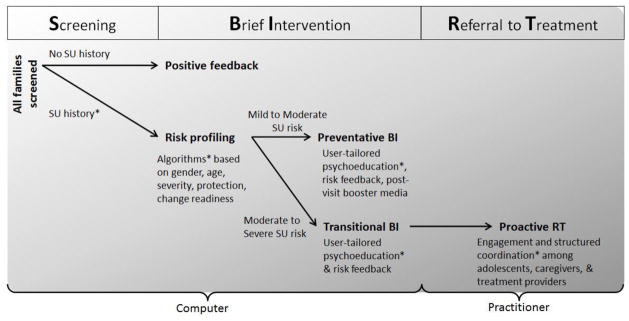
When the BI transformations recommended for BI in pediatric care are assembled into a whole, the following sequence materializes: multidimensional SUD risk algorithms dictate whether families track into (a) computer-based preventative BI modules for low/moderate-risk adolescents, featuring user-responsive PE for adolescents and caregivers; or (b) transitional BIs folded into RT procedures for moderate/severe-risk adolescents. Figure 2 illustrates how adolescents and parents progress through this sequence.
Figure 2.
SBIRT-A Continuum of Care: Case Flow across Phases. Components of the model that involve caregivers are denoted by asterisk.
One additional transformation might offer great added value within a comprehensive SBIRT-A framework: Providers can leverage fast-moving advances in communication media to offer between-visit booster interventions that reinforce the effects of preventative BIs. Booster content can be delivered in a multitude of formats, ranging from brief text messages in a preset series to interactive video messaging (Jones, 2014). Booster contacts can also incorporate assessment functions to monitor changes in SUD risk status (Kumar et al., 2013) and even alert providers to consider immediate patient outreach. A host of technical, validity, and confidentiality issues must be resolved before media options can be fully exploited for behavioral health disorders (Jones, 2014); moreover, media boosters have not yet proven superior to standard patient tracking and follow-up procedures in routine PC. Still, the potential value of BI media enhancements is enormous, and PC offices are well-positioned to take advantage of emerging capabilities in this area.
4. Referral to Treatment
For adolescents at moderate to severe SUD risk, receipt of a transitional BI is followed by progression to the RT component of SBIRT-A. Generally speaking, RT is deemed successfully completed when a high-risk individual is not only referred to treatment but actually enrolls in and receives treatment (SAMHSA, 2013). Relative to the S and BI components, protocols for executing RT for adolescents are largely uncodified and untested (Mitchell et al., 2013). A general directive for implementing RT with high-risk populations is for gateway service providers to establish relationships and referral procedures with treatment programs in the local community (SAMHSA, 2013). Beyond such global prescriptions, however, few guidelines are in place to inform the typically complex process of channeling high-risk individuals into treatment, especially adolescents with severe SUD risk profiles (see Cucciare, Coleman, & Timko, 2014).
4.1. Adolescent-Specific Considerations for Referral to Treatment
It is well known that ASU are unlikely to receive treatment unless coerced by an external agency such as the school or juvenile justice system, especially in absence of a comorbid disorder or precipitating crisis event that could signal the presence of a SU problem (Ozechowski & Waldron, 2010). Accordingly, it is reasonable to suspect that rates of clinical service access and utilization may be quite low among adolescents screened as high-risk for SUD and referred to treatment by PC physicians. Although virtually no empirical data exist on RT’s effectiveness with adolescents, findings by Hacker and colleagues (2014) indicated that fewer than one-fifth of adolescents referred by PC physicians for mental health problems detected during wellness visits received any face-to-face services despite ample availability of in-network treatment providers. Service utilization results such as these underscore the challenges of linking high-risk youth screened in PC settings to necessary clinical services even when communication channels between physicians and treatment providers are in place and referral procedures are well established.
In contrast to the S and BI components of SBIRT-A, which optimally are administered using electronic formats, the RT component of SBIRT-A relies on direct provider involvement. Although general prescriptions for implementing SBIRT call for active gateway service provider involvement in the referral process, the SBIRT-A framework entails more intense and proactive interactions involving PC providers, adolescents, caregivers, and SU treatment providers in order to close gaps in the referral process. The following sections present an overview of the core objectives associated with the RT component of SBIRT-A in routine pediatric care.
4.2. RT Adaptation #1: Enhancing the Physician-Adolescent Process
Adolescents tracked into the RT phase should be engaged by physicians in ways that lay essential groundwork for enrollment in SU treatment. In particular, adolescents at high risk for SUD should be helped to recognize (a) the risks and detriments to health and well-being associated with SU, (b) the benefits of abstaining from (or at least substantially curtailing) further SU, and (c) the potential value of seeking treatment for overcoming SU problems. Second, adolescents should be supportively encouraged to talk directly with caregivers regarding the nature of their SU involvement as a first step toward help-seeking and behavior change (Ford, English, & Sigman, 2004). Adolescents are most likely to disclose SU behavior with PC physicians whom they perceive to be credible sources of health information and genuinely concerned for patients’ personal well-being (Kadivar et al., 2014), and when confidentiality is assured (Ford et al., 1997). Physicians are best positioned to convey these messages by interacting with adolescents in one-on-one sessions from a youth-centered, strength-based perspective (Sanders & Munford, 2014) during which they convey interest in adolescents’ personal qualities, aptitudes, resiliencies, and potential for success. Moreover, physicians should express confidence in adolescents’ capacity to manage their lives productively, including making adaptive decisions regarding SU involvement and participation in SU treatment. Physicians may also wish to remind adolescents of state and federal regulations that protect their confidentiality (see Ford, et al., 2004; Weddle & Kokotailo, 2002), while leveraging strength-based alliances to encourage adolescent assent to disclose SU problems to those caregivers who can provide assistance, guidance, and support with such issues.
4.3. RT Adaptation #2: Enhancing the Physician-Caregiver Process
It is widely recognized that persuading or directing ASU to enroll in treatment typically requires substantial family influence and involvement (Logan & King, 2001). Unfortunately, there is often an array of challenges to engaging family caregivers in this process, many of which are rooted in caregiver attitudes that impede momentum toward treatment enrollment (Ozechowski & Waldron, 2010). Such obstacles include caregiver unawareness or minimization of adolescent SU severity, skepticism about the value of treatment, fear of being judged for adolescent SU problems, and hopelessness about the possibility of change. The RT component of SBIRT-A calls for PC physicians to engage caregivers in ways that address these challenges and mobilize caregiver influence to enroll high-risk adolescents into treatment.
PC physicians are ideally positioned to shape caregiver attitudes about SU health risks and treatment options given their recognized medical expertise and authority on health care issues. During the RT phase, physicians should facilitate caregiver awareness and understanding of ASU problems by sharing the SUD risk data collected during the S and BI phases (with adolescent assent, as described above) and explaining the corresponding risks and ramifications. Physicians should also attempt to join with caregivers in talking directly with adolescents about SU involvement (instead of confronting adolescents about their caregivers’ concerns), while being sensitive to those caregivers who opt not to participate in such discussions or have the concerns they disclosed in confidence shared with their adolescent children.
Paralleling interactions with adolescents, physicians can spur momentum toward treatment enrollment by adopting an empathic and strength-based demeanor with caregivers (see Kemp, Marcenko, Lyons, & Kruzich, 2014). Such a stance may entail acknowledging caregivers’ past efforts to cope with ASU and associated behavior; validating caregivers’ desire to safeguard their children from harm; reinforcing the vital importance of caregiver involvement and influence on adolescent well-being; and reassuring that change is possible (though not guaranteed) with strong caregiver participation in efforts to deter and protect adolescents from engaging in substance use. In addition, physicians can enlist active caregiver collaboration in supporting treatment enrollment, offering not only to provide a program referral but also to facilitate the initial contact between the family and SU treatment providers. Strength-based strategies such as these are consistent with established family-based treatment engagement procedures for ASU and associated problems (e.g., Alexander, Waldron, Robbins, & Neeb, 2013; Liddle, 2002; Szapocznik, Zarate, Duff, & Muir, 2013). Likewise, these physician-caregiver adaptations to RT are consistent with empirically validated family-based clinical procedures that mobilize caregiver support to influence highly resistant adolescents to enroll in SU treatment (Kirby et al., 2015; Waldron, Kern-Jones, Turner, Petersen, & Ozechowski, 2007).
4.4. RT Adaptation #3: Enhancing the Physician-Treatment Provider Process
Within the SBIRT-A framework, the RT component constitutes a coordinated patient handoff or transfer of responsibility for patient care from one provider to another in a manner upholding patient safety and continuity of care (Deutsch, Black, Moore, & Karsh, 2008). Unlike patient handoff in the conventional sense, referred adolescents and caregivers should be instrumentally involved in the RT process so that sufficient levels of patient “buy-in” may be cultivated (see Yatchmenoff, 2005). Thus, effective RT hinges on adolescent and caregiver engagement in the referral process. Ideally, PC providers should initiate the RT process by contacting SU treatment providers in the presence of adolescents and caregivers, thereby enabling physicians to make personal introductions and to elicit adolescent and caregiver questions, concerns, and input regarding SU issues, treatment goals, and processes. If PC and SU treatment services are co-located, these conversations can occur face-to-face. Otherwise, conference phone calls or videoconferences (e.g., Skype) can be used. The end goal of family involvement in RT discussions is to ensure successful patient handoff and procure treatment engagement. Enlisting patients as active partners in health care discussions is a hallmark of patient-centered approaches to health care delivery (Bechtel & Ness, 2010; Coulter, 2011), which are themselves associated with better health outcomes, lower rates of subsequent and more intensive service utilization, and reduced costs (Hibbard & Greene, 2013; Hibbard, Greene, & Overton, 2013).
One caveat regarding the RT adaptions discussed above is that caregiver presence during PC visits is assumed. However, older adolescents frequently attend PC visits alone. Although the S and BI components of SBIRT-A may be implemented without caregiver presence, the recommended adaptations to RT hinge on direct caregiver involvement. If caregivers are absent for the RT phase, PC personnel should attempt to contact caregivers by phone (with adolescent assent) to relay concerns regarding ASU and engage them directly in the RT process during a follow-up in-person visit or via telehealth methods (Kriechman & Bonham, 2013).
5. Discussion
This article describes SBIRT-A, which is a framework comprising a set of developmentally informed adaptations to the SBIRT model to enhance its effectiveness in detecting elevated levels of risk for SUD and facilitating indicated intervention services among adolescents in PC clinics. Relative to conventional SBIRT, the SBIRT-A framework incorporates more proactive, assertive, and family-focused strategies for addressing the clinical needs of adolescents with SU problems that are otherwise likely to go unnoticed during routine PC encounters. Comprehensive, developmentally informed identification and intervention engagement strategies for adolescents at high risk for SUD appear essential for meaningfully reducing the ASU treatment gap (Ozechowski & Waldron, 2010).
The proposed developmental adaptations encompassed within SBIRT-A are aligned with broad-based shifts in pediatric healthcare policy and practice emphasizing integration of behavioral health care and PC services (Stancin & Perrin, 2014). Generally speaking, the prevailing paradigm for integrating behavioral health and PC is the coordinated care model (CCM) under which providers in separate health care settings establish formal linkages to facilitate patient referrals; exchange patient diagnostic, assessment, and health status information; schedule patient appointments; and track patient follow-through, treatment progress, and needs for additional services (Heath, Wise-Romero, & Reynolds, 2013). Historically, managing the process of treatment linkage and coordination across provider organizations in accordance with the CCM has proven fraught with complexity (see Institute of Medicine, 2006). With regard to conventional SBIRT for adolescents, such complexities have hampered the formulation of systematic guidelines and procedures for collaboration between PC and SU treatment providers (see Mitchell et al., 2013). Contemporary innovations and advances in models of healthcare delivery emphasizing integrated and co-located PC and behavioral health services may streamline the RT process, ultimately enhancing rates of SU treatment utilization among high-risk ASU referred by PC physicians using the SBIRT-A framework (see Heath et al., 2013; Stancin & Perrin, 2014). Furthermore, evolving electronic health information exchange networks incorporating both PC and behavioral health care providers hold great promise for facilitating interagency referrals and coordination of care in keeping with the SBIRT-A framework (Office of the National Coordinator for Health Information Technology, 2014).
As is the case regarding traditional SBIRT, physician time restrictions may pose a barrier to implementing the SBIRT-A framework in PC clinics (Van Hook et al., 2007). As noted previously, however, the S and BI components of the framework rely largely upon electronic delivery formats requiring little or no physician involvement. Furthermore, most or all of the proposed adaptations within the RT component may be implemented by properly trained ancillary healthcare personnel (e.g., nurse practitioners, physician assistants, behavioral health counselors) rather than by physicians. In fact, Stoner and colleagues (2014) showed that physicians, nurse practitioners, and physician assistants can be trained to implement SBIRT with equivalent levels of proficiency using self-administered online tutorials and instructional materials. The notion of utilizing non-physicians to implement the RT process is consistent with the emerging public health service policy and practice known as “task shifting” by which ancillary workers are trained to provide basic healthcare services in the face of provider shortages and other constraints on service availability and accessibility (Kazdin & Rabbitt, 2013). Task-shifting with regard to SBIRT-A is likely to be a viable and practical service delivery option that merits further investigation.
A key question to be addressed is the degree to which the additional clinical components and procedures encompassed within SBIRT-A render the model more costly than traditional SBIRT in PC clinics. To date, the costs of implementing SBIRT with adolescents in PC have not been evaluated. For adults in outpatient medical settings, Zarkin, Bray, Hinde, and Saitz (2015, p. 226) estimated the total cost per patient of substance use screening to be $15.61; of a 15-minute preventative BI to be $38.94; and of a complete transitional BI session (perhaps followed by RT) to be $252.26 (in 2001 dollars, with all components implemented by non-physician behavioral health clinicians). The costs of the corresponding S and BI components of SBIRT-A are likely to be comparable to those for adults, although RT is bound to be more costly given the level of time and effort entailed in orchestrating coordinated interactions among adolescents, caregivers, and SU treatment providers. These implementation costs could be recovered numerous times over, however, if SBIRT-A were proven to prevent a substantial proportion of at-risk youth from progressing toward SUD in young adulthood and beyond (see Cohen & Picquaro, 2009; Griffin, Ramchand, Edelen, McCaffery, & Morral, 2011). Among adult SBIRT recipients in medical settings, cost-benefits have been documented in the form of reduced health care service utilization and other costs to society (Barbosa, Cowell, Bray, & Aldridge, 2015; Estee et al., 2010). In recognition of these types of public health benefits, financial coverage for SBIRT is a priority under the ACA (Ghitza & Tai, 2014; Tai & Volkow, 2013) and as well as within the managed care industry (Rahm et al., 2013). In like manner, reimbursement for SBIRT-A services in PC clinics would likely be a prudent public health investment for policy makers as well as health insurance companies and managed care organizations (see CASA, 2011; Lee et al., 2012). Fortunately, an array of AMA-approved billing codes are in place to provide reimbursement for activities encompassed within the S and preventative BI components of SBIRT-A, as well as more extended counseling activities entailed within transitional BI and RT (see SAMHSA, 2015). A manual detailing these codes for pediatricians is provided by the AAP (2015). Levy and Kokotailo (2011) also provide a helpful overview of billing issues for pediatricians providing SBIRT services to adolescents in PC.
This article provides a fairly broad overview of the SBIRT-A framework. Moving forward, the proposed SBIRT-A adaptations will require more detailed specification, manualization, and training materials to facilitate systematic application across PC clinics (e.g., DiClemente, Crouch, Norwood, Delahanty, & Welsh, 2015). In particular, the validation of caregiver screening measures and the development of software programs for implementing the S and preventive BI components, including algorithms for determining the appropriate BI based on a given profile of adolescent- and caregiver-reported risk factors, are critical next-steps for the dissemination and implementation of SBIRT-A. Also, experimental studies are needed to evaluate the effectiveness of SBIRT-A relative to conventional SBIRT for detecting adolescents at risk for SUD, promoting intervention access and utilization, preventing the onset of SUD among adolescents at low-to-moderate risk, and producing long-term reductions in substance use behavior and associated consequences among high-risk adolescents. In addition, empirical evaluations focused on identifying the essential framework components, optimal implementation strategies, and the cost-effectiveness for SBIRT-A are needed to its support widespread dissemination and adoption. For the time being, we hope this article stimulates further thinking regarding novel and clinically resourceful ways to identify and intervene with adolescents at risk for SUD in PC and other gateway service arenas.
Manuscript Highlights.
SBIRT (Screening, Brief Intervention and Referral to Treatment) is widely recommended for adolescents in primary care and other settings.
SBIRT lacks substantial evidence of effectiveness, feasibility, and developmental appropriateness for adolescents.
SBIRT-A is a set of recommended adaptations to the SBIRT model to better serve the developmental needs of adolescents.
Key adaptations in SBIRT-A include reliance upon proactive (versus reactive) methods to identify and engage youth; innovation in service delivery aimed at improving the consistency and reach of interventions; and a family-focused approach to engagement, assessment, and intervention.
Acknowledgments
Funding for the second author’s contribution to this manuscript came from the National Institute on Drug Abuse grant K23DA031743. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse. We gratefully acknowledge the contribution of the journal editor and reviewers, whose comments significantly improved this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Timothy J. Ozechowski, Oregon Research Institute
Sara J. Becker, Center for Alcohol and Addictions Studies at Brown University School of Public Health
Aaron Hogue, National Center on Addiction and Substance Abuse at Columbia University
References
- Agerwala SM, McCance-Katz EF. Integrating screening, brief intervention, and referral to treatment (SBIRT) into clinical practice settings: A brief review. Journal of Psychoactive Drugs. 2012;44:307–317. doi: 10.1080/02791072.2012.720169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander JF, Waldron HB, Robbins MS, Neeb AA. Functional family therapy for adolescent behavior problems. Washington, D.C: American Psychological Association; 2013. [Google Scholar]
- American Academy of Pediatrics. Coding for Pediatrics 2015: A manual for pediatric documentation and payment. Elk Grove Village, IL: American Academy of Pediatrics; 2015. [Google Scholar]
- American Academy of Pediatrics, Division of Child Health Research. Research update: 45% of fellows routinely screen for alcohol use. AAP News. 1998;14:1–12. [Google Scholar]
- American Medical Association. Guidelines for Adolescent Preventative Services. 2015 Retrieved on March 1, 2015 from http://www.uptodate.com/contents/guidelines-for-adolescent-preventive-services.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Anand V, Carroll AE, Downs SM. Automated primary care screening in pediatric waiting rooms. Pediatrics. 2012;129:e1275–e1281. doi: 10.1542/peds.2011-2875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J. Screening, Brief Intervention, and Referral to Treatment (SBIRT): Toward a public health approach to the management of substance abuse. Substance Abuse. 2007;28:7–30. doi: 10.1300/J465v28n03_03. [DOI] [PubMed] [Google Scholar]
- Barbosa C, Cowell A, Bray J, Aldridge A. The cost-effectiveness of alcohol screening, breif intervention, and referral to treatment (SBIRT) in emergency and outpatient medical settings. Journal of Substance Abuse Treatment. 2015;53:1–8. doi: 10.1016/j.jsat.2015.01.003. [DOI] [PubMed] [Google Scholar]
- Bechtel C, Ness DL. If you build it, will they come? Designing truly patient-centered health care. Health Affairs. 2010;29:914–920. doi: 10.1377/hlthaff.2010.0305. [DOI] [PubMed] [Google Scholar]
- Biener L, Abrams DB. The Contemplation Ladder: Validation of a measure of readiness to consider smoking cessation. Health Psychology. 1991;10:360–365. doi: 10.1037//0278-6133.10.5.360. [DOI] [PubMed] [Google Scholar]
- Bohnert KM, Walton MA, Resko S, Barry KT, Chermack ST, Zucker RA, Blow FC. Latent class analysis of substance use among adolescents presenting to urban primary care clinics. American Journal of Drug and Alcohol Abuse. 2014;40:44–50. doi: 10.3109/00952990.2013.844821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brener ND, Billy JOG, Grady WR. Assessment of factors affecting the validity of self-reported health-risk behavior among adolescents: Evidence from the scientific literature. Journal of Adolescent Health. 2003;33:436–457. doi: 10.1016/s1054-139x(03)00052-1. [DOI] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LA, Elliott JC, Garey L, Carey MP. Face-to-face versus computer-delivered alcohol interventions for college drinkers: a meta-analytic review, 1998 to 2010. Clinical Psychology Review. 2012;32:690–703. doi: 10.1016/j.cpr.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carney T, Myers BJ, Louw J, Okwundu CI. Brief school-based interventions and behavioural outcomes for substance-using adolescents. Cochrane Database of Systematic Reviews. 2014 doi: 10.1002/14651858.CD008969.pub2. [DOI] [PubMed] [Google Scholar]
- CASA Columbia. Adolescent substance abuse: America’s #1 public health problem. New York: National Center on Addictions and Substance Abuse at Columbia University; 2011. [Google Scholar]
- Ciesla JR, Spear SF, Skala SY. Reliability over time of self-reports given by adolescents and their parents in substance abuse outcome research. Journal of Child and Adolescent Substance Abuse. 1999;9:57–73. [Google Scholar]
- Clark DB, Moss HB. Providing alcohol-related screening and brief interventions to adolescents through health care systems: Obstacles and solutions. PLoS medicine. 2010;7(3):e1000214. doi: 10.1371/journal.pmed.1000214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen MA, Piquero AR. New evidence on the monetary value of saving a high risk youth. Journal of Quantitative Criminology. 2009;25:25–49. [Google Scholar]
- Coulter A. Engaging patients in health care. New York: McGraw-Hill Open University Press; 2011. [Google Scholar]
- Cucciare MA, Coleman EA, Timko C. A conceptual model to facilitate transitions from primary care to specialty substance use disorder care: A review of the literature. Primary Health Care Research and Development. 2014;12:1–14. doi: 10.1017/S1463423614000164. [DOI] [PubMed] [Google Scholar]
- Curtis BL, McLellan AT, Gabellini BN. Translating SBIRT to public school settings: An initial test of feasibility. Journal of Substance Abuse Treatment. 2014;46(1):15–21. doi: 10.1016/j.jsat.2013.08.001. [DOI] [PubMed] [Google Scholar]
- D’Onofrio G, Pantalon MV, Degutis LC, Fiellin DA, Busch SH, Chawarski MC, O’Connor PG. Brief intervention for hazardous and harmful drinkers in the emergency department. Annals of Family Medicine. 2008;51:742–750. doi: 10.1016/j.annemergmed.2007.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deutsch ES, Black B, Moore G, Karsh B. S*T*A*R*T: A great handoff – An approach to effective medical communication in a high-risk environment. In: Savage GT, Ford EW, editors. Patient safety and health care management. Bingley, UK: JAI Press; 2008. pp. 241–258. [Google Scholar]
- DiClemente CC, Crouch TB, Norwood AEQ, Delahanty J, Welsh C. Evaluating training of Screening, Brief Intervention, and Referral to Treatment (SBIRT) for substance use: Reliability of the MD3 SBIRT coding scale. Psychology of Addictive Behaviors. 2015;29:218–224. doi: 10.1037/adb0000022. [DOI] [PubMed] [Google Scholar]
- Dunn C, Darnell D, Carmel A, Atkins DC, Bumgardner K, Roy-Byrne P. Comparing the motivational interviewing integrity in two prevalent models of brief intervention service delivery for primary care settings. Journal of Substance Abuse Treatment. 2015;51:47–52. doi: 10.1016/j.jsat.2014.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elster A. The American Medical Association guidelines for adolescent preventive services. Archives of Pediatrics & Adolescent Medicine. 1997;151:958–959. doi: 10.1001/archpedi.1997.02170460096021. [DOI] [PubMed] [Google Scholar]
- Estee S, Wickizer T, He L, Shah MF, Mancuso D. Evaluation of the Washington State Screening, Brief Intervention, and Referral to Treatment Project: Cost outcomes for Medicaid patients screened in hospital emergency departments. Medical Care. 2010;48:18–24. doi: 10.1097/MLR.0b013e3181bd498f. [DOI] [PubMed] [Google Scholar]
- Ford C, English A, Sigman G. Confidential health care for adolescents: A position paper of the Society for Adolescent Medicine. Journal of Adolescent Health. 2004;35:1–8. [PubMed] [Google Scholar]
- Ford CA, Millstein SG, Halpern-Felsher BL, Irwin CE., Jr Influence of physician confidentiality assurances on adolescents’ willingness to disclose information and seek future health care: A randomized controlled trial. JAMA. 1997;278:1029–1034. [PubMed] [Google Scholar]
- Gadomski AM, Fothergill KE, Larson S, Wissow LS, Winegrad H, Nagykaldi ZJ, Olson AL, Roter DL. Integrating mental health into adolescent annual visits: Impact of previsit comprehensive screening on within-visit processes. Journal of Adolescent Health. 2015;56:267–273. doi: 10.1016/j.jadohealth.2014.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gayes LA, Steele RG. A meta-analysis of motivational interviewing interventions for pediatric health behavior change. Journal of Consulting and Clinical Psychology. 2014;82:521–535. doi: 10.1037/a0035917. [DOI] [PubMed] [Google Scholar]
- Ghitza UE, Tai B. Challenges and opportunities for integrating preventive substance-use-care services in primary care through the Affordable Care Act. Journal of Health Care for the Poor and Underserved. 2014;25:36–45. doi: 10.1353/hpu.2014.0067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon AJ, Ettaro L, Rodriguez KL, Mocik J, Clark DB. Provider, patient, and family perspectives of adolescent alcohol use and treatment in rural settings. The Journal of Rural Health. 2011;27:81–90. doi: 10.1111/j.1748-0361.2010.00321.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin BA, Ramchand R, Edelen MO, McCaffery DF, Morral AR. Associations between abstinence in adolescence and economic and educational outcomes seven years later among high-risk youth. Drug and Alcohol Dependence. 2011;113:118–124. doi: 10.1016/j.drugalcdep.2010.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hacker K, Arsenault L, Franco I, Shaligram D, Sidor M, Olfson M, Goldstein J. Referral and follow-up after mental health screening in commercially insured adolescents. Journal of Adolescent Health. 2014;55:17–23. doi: 10.1016/j.jadohealth.2013.12.012. [DOI] [PubMed] [Google Scholar]
- Harris SK, Herr-Zaya K, Weinstein Z, Whelton K, Perfas F, Jr, Castro-Donlan C, Levy S. Results of a statewide survey of adolescent substance use screening rates and practices in primary care. Substance Abuse. 2012a;33:321–326. doi: 10.1080/08897077.2011.645950. [DOI] [PubMed] [Google Scholar]
- Harris SK, Csémy L, Sherritt L, Starostova O, Van Hook S, Johnson J, Knight JR. Computer-facilitated substance use screening and brief advice for teens in primary care: An international trial. Pediatrics. 2012b;129:1072–1082. doi: 10.1542/peds.2011-1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heath B, Wise-Romero P, Reynolds KA. A standard framework for levels of integrated healthcare. Washington D.C: SAMHSA-HRSA Center for Integrated Health Solutions; 2013. [Google Scholar]
- Hibbard JH, Greene J. What the evidence shows about patient activations: Better health outcomes and care experiences: Fewer data on costs. Health Affairs. 2013;32:207–214. doi: 10.1377/hlthaff.2012.1061. [DOI] [PubMed] [Google Scholar]
- Hibbard JH, Greene J, Overton V. Patients with lower activation associated with higher costs: Delivery systems should know their patients’ scores’. Health Affairs. 2013;32:216–222. doi: 10.1377/hlthaff.2012.1064. [DOI] [PubMed] [Google Scholar]
- Hingson R, Compton WM. Screening and brief intervention and referral to treatment for drug use in primary care: Back to the drawing board. JAMA. 2014;312:488–489. doi: 10.1001/jama.2014.7863. [DOI] [PubMed] [Google Scholar]
- Hoagwood KE. Family support in children’s mental health: A review and synthesis. Clinical Child & Family Psychology Review. 2010;13:1–45. doi: 10.1007/s10567-009-0060-5. [DOI] [PubMed] [Google Scholar]
- Hogue A, Dauber S, Morgenstern J. Validation of a contemplation ladder in an adult substance use disorder sample. Psychology of Addictive Behaviors. 2010;24:137–144. doi: 10.1037/a0017895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, Henderson CE, Ozechowski TJ, Robbins MS. Evidence base on outpatient behavioral treatments for adolescent substance use: Updates and recommendations 2007–2013. Journal of Clinical Child and Adolescent Psychology. 2014;43:697–720. doi: 10.1080/15374416.2014.915550. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Improving the Quality of Health Care for Mental and Substance-Use Conditions. Washington, DC: National Academy Press; 2006. [Google Scholar]
- Jones DJ. Future directions in the design, development, and investigation of technology as a service delivery vehicle. Journal of Clinical Child & Adolescent Psychology. 2014;43:128–142. doi: 10.1080/15374416.2013.859082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadivar H, Thompson L, Wegman M, Chisholm T, Khan M, Eddleton K, Shenkman E. Adolescent views on comprehensive health risk assessment and counseling: Assessing gender differences. Journal of Adolescent Health. 2014;55:24–32. doi: 10.1016/j.jadohealth.2013.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaner EF, Dickinson HO, Beyer F, Pienaar E, Campbell F, Schlesinger C, Heather N, Saunders J, Burnand B. Effectiveness of brief alcohol interventions in primary care populations (Review) Cochrane Database of Systematic Reviews. 2007 doi: 10.1002/14651858.CD004148.pub3. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Rabbitt SM. Novel models for delivering mental health services and reducing the burdens of mental illness. Clinical Psychological Science. 2013;1:170–191. [Google Scholar]
- Kemp SP, Marcenko MO, Lyons SJ, Kruzich JM. Strength-based practice and parental engagement in child welfare services: An empirical examination. Children and Youth Services Review. 2014;47:27–35. [Google Scholar]
- King KM, Chung T, Maisto SA. Adolescents’ thoughts about abstinence curb the return of marijuana use during and after treatment. Journal of Consulting and Clinical Psychology. 2009;77:554–565. doi: 10.1037/a0015391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby KC, Versek B, Kerwin ME, Meyers K, Benishek LA, Bresani E, Washio Y, Arria A, Meyers RJ. Developing Community Reinforcement and Family Training (CRAFT) for parents of treatment-resistant adolescents. Journal of Child and Adolescent Substance Abuse. 2015;24:155–165. doi: 10.1080/1067828X.2013.777379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight JR, Harris SK, Sherritt L, Van Hook S, Lawrence N, Brooks T, Kulig J. Prevalence of positive substance abuse screen results among adolescent primary care patients. Archives of Pediatrics & Adolescent Medicine. 2007;161:1035–1041. doi: 10.1001/archpedi.161.11.1035. [DOI] [PubMed] [Google Scholar]
- Knight JR, Sherritt L, Harris SK, Gates EC, Chang G. Validity of brief alcohol screening tests among adolescents: a comparison of the AUDIT, POSIT, CAGE and CRAFFT. Alcoholism: Clinical and Experimental Research. 2002;27:67–73. doi: 10.1097/01.ALC.0000046598.59317.3A. [DOI] [PubMed] [Google Scholar]
- Kumar S, Nilsen WJ, Abernethy A, Atienza A, Patrick K, Pavel M, Swendeman D. Mobile health technology evaluation: the mHealth evidence workshop. American Journal of Preventive Medicine. 2013;45:228–236. doi: 10.1016/j.amepre.2013.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy SJ, Kokotailo PK. Substance use screening, brief intervention, and referral to treatment for pediatricians. Pediatrics. 2011;128:e1330–e1340. doi: 10.1542/peds.2011-1754. [DOI] [PubMed] [Google Scholar]
- Levy S, Weiss R, Sherritt L, Ziemnik R, Spalding A, Van Hook S, Shrier LA. An electronic screen for triaging adolescent substance use by risk levels. JAMA Pediatrics. 2014;168:822–828. doi: 10.1001/jamapediatrics.2014.774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liddle HA. Multidimensional Family Therapy for adolescent cannabis users: Cannabis youth treatment series, Volume 5. Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental Health; 2002. DHHS Pub. No. 02–3660. [Google Scholar]
- Logan DE, King CA. Parental facilitation of adolescent mental health services utilization: A conceptual and empirical review. Clinical Psychology: Science and Practice. 2001;8:319–333. [Google Scholar]
- Madden M, Lenhart A, Duggan M, Cortesi S, Gasser U. Teens and technology 2013. Pew Research Center; 2013. [Accessed on 7/20/2015]. from: http://www.pewinternet.org/2013/03/13/teens-and-technology-2013/ [Google Scholar]
- McGillicuddy NB, Rychtarik RG, Morsheimer ET, Bruke-Storer MR. Agreement between parent and adolescent reports of adolescent substance use. Journal of Child and Adolescent Substance Abuse. 2012;16:59–78. doi: 10.1300/J029v16n04_04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, He J, Burstein M, Swendsen J, Avenevoli S, Case B, Olfson M. Service utilization for lifetime mental disorders in U.S. adolescents: Results of the National Comorbidity Survey – Adolescent Supplement (NCS-A) Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50:32–45. doi: 10.1016/j.jaac.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millstein SG, Marcell AV. Screening and counseling for adolescent alcohol use among primary care physicians in the United States. Pediatrics. 2003;111:114–122. doi: 10.1542/peds.111.1.114. [DOI] [PubMed] [Google Scholar]
- Mitchell SG, Gryczynski J, O’Grady KE, Schwartz RP. SBIRT for adolescent drug and alcohol use: Current status and future directions. Journal of Substance Abuse Treatment. 2013;44:463–472. doi: 10.1016/j.jsat.2012.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyer VA. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: U.S. Preventive Services Task Force recommendation statement. Annals of Internal Medicine. 2013;159:210–218. doi: 10.7326/0003-4819-159-3-201308060-00652. [DOI] [PubMed] [Google Scholar]
- National Drug Intelligence Center. The economic impact of illicit drug use on American society. Washington, DC: United States Department of Justice; 2011. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Alcohol Screening and Brief Intervention for Youth: A Practitioner’s Guide. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2011. NIH Publication 11-7805. [Google Scholar]
- National Institute on Drug Abuse. Principles of Adolescent Substance Use Disorder Treatment: A Research-Based Guide. Bethesda, MD: National Institute on Drug Abuse; 2014. [Google Scholar]
- Nordin JD, Solberg LI, Parker ED. Adolescent primary care visit patterns. Annals of Family Medicine. 2010;8:511–516. doi: 10.1370/afm.1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of the National Coordinator for Health Information Technology. Behavioral health data exchange consortium. ONC State Health Policy Consortium Project: Final Report. Research Triangle Park, NC: RTI International; 2014. [Google Scholar]
- Oliver RM, Cress CJ, Savolainen H, Epstein MH. Strength-based assessment issues, tools, and practices in school-related contexts and schools in the United States and Finland. In: Walker HMG, FM, editors. Handbook of evidence-based practices for emotional and behavioral disorders: Applications in schools. New York: The Guilford Press; 2014. [Google Scholar]
- Ozechowski TJ, Waldron HB. Assertive outreach strategies for narrowing the adolescent substance abuse treatment gap: Implications for research, practice, and policy. Journal of Behavioral Health Services and Research. 2010;37:40–63. doi: 10.1007/s11414-008-9136-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patnode CD, O’Connor E, Rowland M, Burda BU, Perdue LA, Whitlock EP. Primary care behavioral interventions to prevent or reduce illicit drug use and nonmedical pharmaceutical use in children and adolescents: A systematic evidence review for the U.S. Preventive Services Task Force. Annals Internal Medicine. 2014;160:612–620. doi: 10.7326/M13-2064. [DOI] [PubMed] [Google Scholar]
- Patton R, Deluca P, Kaner E, Newbury-Birch D, Phillips T, Drummond C. Alcohol screening and brief intervention for adolescents: The how, what and where of reducing alcohol consumption and related harm among young people. Alcohol and Alcoholism. 2014;49:207–212. doi: 10.1093/alcalc/agt165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen ER, Grow J, Duncan S, Neighbors C, Larimer ME. Concurrent validity of an online version of the Timeline Followback assessment. Psychology of Addictive Behaviors. 2012;26:672. doi: 10.1037/a0027945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC, Norcross JC. In search of how people change: Applications to addictive behaviors. American Psychologist. 1992;47:1102–1114. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- Rahm AK, Martin C, Boggs J, Price D, Beck A, Dearing J, Backer T. Implementation of a Screening Brief Intervention and Referral to Treatment (SBIRT) protocol in primary care. Clinical Medicine & Research. 2013;11:165. [Google Scholar]
- Rand CM, Shone LP, Albertin C, Auinger P, Klein JD, Szilagyi PG. National health care visit patterns of adolescents: implications for delivery of new adolescent vaccines. Archives of Pediatric Adolescent Medicine. 2007;161:252–259. doi: 10.1001/archpedi.161.3.252. [DOI] [PubMed] [Google Scholar]
- Roy-Byrne P, Bumgardner K, Krupski A, Dunn C, Ries R, Donovan D, Zarkin G. Brief intervention for problem drug use in safety-net primary care settings: A randomized clinical trial. JAMA. 2014;312:492–501. doi: 10.1001/jama.2014.7860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saitz R, Palfai TP, Cheng DM, Alford DP, Bernstein JA, Lloyd-Travaglini CA, Samet JH. Screening and brief intervention for drug use in primary care: the ASPIRE randomized clinical trial. JAMA. 2014;312:502–513. doi: 10.1001/jama.2014.7862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanders J, Munford R. Youth-centered practice: Positive youth development practices and pathways to better outcomes for vulnerable youth. Children and Youth Services Review. 2014;46:160–167. [Google Scholar]
- Schram P, Harris SK, Van Hook S, Forman S, Mezzacappa E, Pavlyuk R, Levy S. Implementing adolescent Screening, Brief Intervention, and Referral to Treatment (SBIRT) in a pediatric residency curriculum. Substance Abuse. 2014;18:1–7. doi: 10.1080/08897077.2014.936576. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Slavet JD, Stein LA, Colby SM, Barnett NP, Monti PM, Golembeske C, Labeau-Craven R. The Marijuana Ladder: Measuring motivation to change marijuana use in incarcerated adolescents. Drug and Alcohol Dependence. 2006;83:42–48. doi: 10.1016/j.drugalcdep.2005.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stancin T, Perrin EC. Psychologists and pediatricians: Opportunities for collaboration in primary care. American Psychologist. 2014;69:332–343. doi: 10.1037/a0036046. [DOI] [PubMed] [Google Scholar]
- Stephens S, Celluci T, Gregory J. Comparing stages of change measures in adolescent smokers. Addictive Behaviors. 2004;29:759–764. doi: 10.1016/j.addbeh.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Sterling S, Kline-Simon AH, Wibbelsman C, Wong A, Weisner C. Screening for adolescent alcohol and drug use in pediatric health-care settings: Predictors and implications for practice and policy. Addiction Science and Clinical Practice. 2012;7:13. doi: 10.1186/1940-0640-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterling S, Weisner C, Hinman A, Parthasarathy S. Access to treatment for adolescents with substance use and co-occurring disorders: Challenges and opportunities. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:637–646. doi: 10.1016/j.jaac.2010.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoner SA, Mikko AT, Carpenter KM. Web-based training for primary care providers on screening, brief intervention, and referral to treatment (SBIRT) for alcohol, tobacco, and other drugs. Journal of Substance Abuse Treatment. 2014;47:362–370. doi: 10.1016/j.jsat.2014.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Systems-Level Implementation of Screening, Brief Intervention, and Referral to Treatment. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. Technical Assistance Publication (TAP) Series 33. HHS Publication No. (SMA) 13–4741. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. NSDUH Series H-48, HHS Publication No. (SMA) 14–4863. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Reimbursement for SBIRT. n.d Retrieved from http://www.integration.samhsa.gov/sbirt/reimbursement_for_sbirt.pdf.
- Szapocznik J, Zarate M, Duff J, Muir J. Brief Strategic Family Therapy: Engaging drug using/problem behavior adolescents and their families in treatment. Social Work in Public Health. 2013;28:206–223. doi: 10.1080/19371918.2013.774666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tai B, Volkow ND. Treatment for substance use disorder: Opportunities and challenges under the Affordable Care Act. Social Work in Public Health. 2013;28:165–174. doi: 10.1080/19371918.2013.758975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner-Smith EE, Lipsey MW. Brief alcohol interventions for adolescents and young adults: a systematic review and meta-analysis. Journal Substance Abuse Treatment. 2015;51:1–18. doi: 10.1016/j.jsat.2014.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner SD, Spithoff S, Kahan M. Approach to cannabis use disorder in primary care: Focus on youth and other high-risk users. Canadian Family Physician. 2014;60:801–808. [PMC free article] [PubMed] [Google Scholar]
- Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behavior, drug use, and violence: increased reporting with computer survey technology. Science. 1998;280:867–873. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]
- Vakalahi HF. Adolescent substance use and family-based risk and protective factors: A literature review. Journal of Drug Education. 2001;31:29–46. doi: 10.2190/QP75-P9AR-NUVJ-FJCB. [DOI] [PubMed] [Google Scholar]
- Van Hook S, Harris SK, Brooks T, Carey P, Kossack R, Kulig J, Knight JR the New England Partnership for Substance Abuse Research. The “six T’s” : Barriers to screening teens for substance abuse in primary care. Journal of Adolescent Health. 2007;40:456–461. doi: 10.1016/j.jadohealth.2006.12.007. [DOI] [PubMed] [Google Scholar]
- Waldron HB, Kern-Jones S, Turner CW, Peterson TR, Ozechowski TJ. Engaging resistant adolescents in drug abuse treatment. Journal of Substance Abuse Treatment. 2007;32:133–142. doi: 10.1016/j.jsat.2006.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton MA, Bohnert K, Resko S, Barry KL, Chermack ST, Zucker RA, Blow FC. Computer and therapist based brief interventions among cannabis-using adolescents presenting to primary care: one year outcomes. Drug and Alcohol Dependence. 2013;132:646–653. doi: 10.1016/j.drugalcdep.2013.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Warner V, John K, Prusoff B, Merikangas K, Gammon D. Assessing psychiatric disorders in children: Discrepancies between mothers’ and children’s reports. Archives of General Psychiatry. 1987;44:747–753. doi: 10.1001/archpsyc.1987.01800200075011. [DOI] [PubMed] [Google Scholar]
- Whittle AE, Buckelew SM, Satterfield JM, Lum PJ, O’Sullivan P. Addressing adolescent substance use: Teaching SBIRT and MI to residents. Substance Abuse. 2014;26 doi: 10.1080/08897077.2014.965292. epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Wills TA, Yaeger AM. Family factors and adolescent substance use models and mechanisms. Current Directions in Psychological Science. 2003;12:222–226. [Google Scholar]
- Wilson CR, Sherritt L, Gates E, Knight JR. Are clinical impressions of adolescent substance use accurate? Pediatrics. 2004;114:e536–540. doi: 10.1542/peds.2004-0098. [DOI] [PubMed] [Google Scholar]
- Winters KC. Screening and assessing adolescents for substance use disorders (Treatment Improvement Protocol (TIP) Series 31. Rockville, MD: Center for Substance Abuse Treatment; 1999. [Google Scholar]
- Winters KC, Fahnhorst T, Botzet A, Lee S, Lalone B. Brief intervention for drug-abusing adolescents in a school setting: Outcomes and mediating factors. Journal of Substance Abuse Treatment. 2012;42:279–288. doi: 10.1016/j.jsat.2011.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winters KC, Leitten W, Wagner E, O’Leary Tevyaw T. Use of brief interventions within a middle and high school setting. Journal of School Health. 2007;77:196–206. doi: 10.1111/j.1746-1561.2007.00191.x. [DOI] [PubMed] [Google Scholar]
- Wissow LS, Brown J, Fothergill KE, Gadomski A, Hacker K, Salmon P, Zelkowitz R. Universal mental health screening in pediatric primary care: A systematic review. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52:1134–1147. doi: 10.1016/j.jaac.2013.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yatchmenoff DK. Measuring client engagement from the client’s perspective in nonvoluntary child protective services. Research on Social Work Practice. 2005;15:84–96. [Google Scholar]
- Yuma-Guerrero PJ, Lawson KA, Velasquez MM, von Sternberg K, Maxson T, Garcia N. Screening, brief intervention, and referral for alcohol use in adolescents: a systematic review. Pediatrics. 2012;130:115–122. doi: 10.1542/peds.2011-1589. [DOI] [PubMed] [Google Scholar]
- Zarkin G, Bray J, Hinde J, Saitz R. Costs of screening and brief intervention for illicit drug use in primary care settings. Journal of Studies on Alcohol and Drugs. 2015;76:222–228. doi: 10.15288/jsad.2015.76.222. [DOI] [PMC free article] [PubMed] [Google Scholar]