Abstract
Genotoxic chemotherapeutics particularly cisplatin remain effective for clinical management of various malignancies including lung cancer. However, the development of chemoresistance leads to treatment failure. The mechanisms by which tumor cells acquire resistance to chemotherapy are multifaceted in nature and some remain to be fully elucidated. Recently, a potential role of RNA-binding protein hnRNPA0 in chemoresistance of p53-defective lung cancer cells was reported. Genotoxic (DNA damaging) chemotherapy was reported to activate hnRNPA0 which in turn post-transcriptionally regulated p27Kip1 and Gadd45-alpha by stabilizing their mRNAs. Regulation of p27Kip1 and Gadd45-alpha led to enforcement of G1/S and G2/M checkpoints thereby providing time for DNA repair and thus, resistance to chemotherapy. The identification of a signaling network involving the kinase MK2, hnRNPA0, p27Kip1 and Gadd45-alpha that may predict response to chemotherapy is an interesting finding. Further studies are now needed to gain additional insights as to whether this network is restricted only to a subset of tumors or more broadly relevant across multiple tumor types.
Keywords: hnRNPA0; Gadd45-alpha; p27Kip1, p53; Lung cancer
Cellular responses to genotoxic stress induced by DNA damaging agents still remain complex (1, 2 and refs. therein) although substantial progress has been made in this area of investigation in recent years. The complexity stems from a variety of reasons including the facts that DNA damage (genotoxic stress) causes cancer and that treatment of cancer also involves DNA damaging anticancer drugs. As well, many cytotoxic effects of several of the clinically relevant anticancer drugs occur due to DNA damage. Nonetheless, in the era of molecular targeted therapy, when approaches to develop targeted therapeutics have started to take center stage, the use of conventional genotoxic chemotherapeutics still remains the mainstay in the clinic for various malignancies including lung cancer.
Lung cancer is one of the major malignancies for both males and females. The American Cancer Society estimates that for the year 2015, there will be 221,200 new cases of cancers of the lung and bronchus, and 158,040 deaths will occur due to these malignancies (3). Lung cancer is divided into two major histologic groups including small cell lung carcinoma (SCLC) and non-small cell lung carcinoma (NSCLC) (reviewed in 4). NSCLC is more common than SCLC and is further subdivided into adenocarcinoma, squamous cell carcinoma and large cell carcinoma (reviewed in 4). Cigarette smoking is associated with lung cancer as all histologic varieties can be detected in smokers and also those who have quit smoking (reviewed in 5). Squamous cell carcinoma and SCLC-types are almost always associated with smoking; in general however, the adenocarcinoma-type is more common among non-smokers (reviewed in 5).
Early detection remains to be a challenge for diagnosing lung cancer and thus, the majority of patients at the time of diagnosis have a metastatic disease (reviewed in 4). Depending on the tumor type and stage, the management of lung cancer involves surgery, radiation therapy and/or chemotherapy. For SCLC, surgery is generally not possible. However, in some cases of early stage SCLC, surgery may be an option that is coupled with chemotherapy or chemoradiation (6). In limited and extensive stage SCLC patients, surgery is not an option and thus, chemotherapeutic approach of two-drug combination of cisplatin and etoposide is used coupled also with radiation (6, reviewed in 5). Management of stage I, II and IIIA NSCLC involves surgery coupled with neoadjuvant or adjuvant therapy (4, 6). For more advanced disease, however, chemotherapy involving two-drug combination is the mainstay. In the US, for stage III (for example, stage IIIB and inoperable stage IIIA) NSCLC there are two commonly used regimens including concurrent carboplatin, paclitaxel and radiation therapy on a weekly basis and then carboplatin and paclitaxel for consolidation or concurrent cisplatin, etoposide and radiation therapy (reviewed in 5). In the case of stage IV NSCLC, cisplatin-based regimens involving gemcitabine or pemetrexed are used (reviewed in 5).
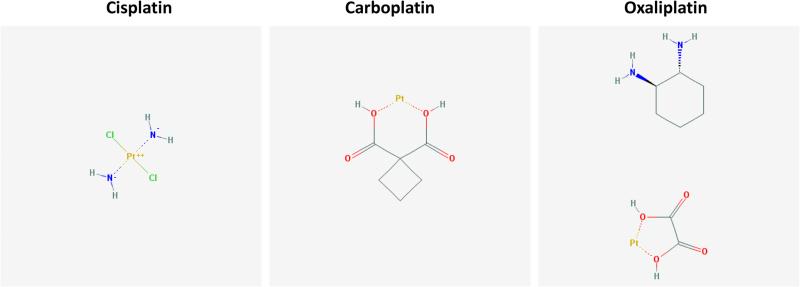
Clearly, genotoxic chemotherapeutics particularly cisplatin remain the effectively used agents for clinical management of lung cancer. However, one of the major causes of treatment failure is the development of chemoresistance. The mechanisms by which tumor cells acquire resistance to chemotherapy are multifaceted in nature (reviewed in 7). Cisplatin is one of the platinum-based antineoplastic agents (Figure 1). It is used for the treatment of various solid malignancies and thus, one of the essential medicines listed by the World Health Organization (WHO). Its mode of action involves interaction with DNA, particularly purines, resulting in the formation of intrastrand adducts as lesions (reviewed in 8, 9). These lesions are believed to cause DNA damage and in the absence of effective DNA repair, cell death ensues (reviewed in 8, 9). Some of the mechanisms that account for cisplatin resistance are alterations in (i) drug uptake and efflux, (ii) biotransformation and detoxification, (iii) DNA repair mechanisms and (iv) events regulating cell death (reviewed in 8, 9, 7). Because cisplatin induces DNA damage that leads also to activation and/or inhibition of various molecules and pathways, alterations in regulation of these events could also conceivably lead to drug resistance. More work is certainly needed to delineate the full circuitry of these molecules and pathways to solve the jigsaw puzzle of chemoresistance.
Figure 1.
Chemical structures of platinum-based antineoplastic agents. Source: PubChem.
Recently, Cannell et al (10) have reported a potential role of RNA-binding protein hnRNPA0 in chemoresistance of p53-defective lung cancer cells. To date, multiple RNA-binding proteins have been identified in eukaryotic cells. These proteins bind to heterogeneous nuclear ribonucleic acids (hnRNAs) and the hnRNAs bound by various proteins exist in larger complexes known as heterogeneous nuclear ribonucleoprotein (hnRNP) particles (11, reviewed in 12). The hnRNP proteins, some of which shuttle between nucleus and cytoplasm, play a variety of roles including pre-mRNA processing, mRNA export, stability and translation (reviewed in 12). hnRNPA0 was originally cloned as a 32 kDa protein that associated with hnRNP complex from the nuclear extracts of HeLa cells (11). hnRNPA0 has also been reported to belong to a minor group of proteins and is reported to play a role in splicing (reviewed in 12). In recent years, hnRNPA0 has been implicated in post-transcriptional regulation of Gadd45-alpha mRNA stability (reviewed in 13). Gadd45-alpha, a growth arrest and DNA damage-regulated protein, it is regulated by p53 and has been implicated in various cellular processes including DNA damage-induced G2/M checkpoint (14, 15). It has been reported that the checkpoint kinase MK2 is an upstream regulator of hnRNPA0 as it phosphorylates hnRNPA0 at serine 84 and thereby activates hnRNPA0 (10, reviewed in 13). Phosphorylated hnRNPA0 is reported to stabilize Gadd45 alpha mRNA (10, reviewed in 13).
In the recent study by Cannell et al (10), it was reported that in response to genotoxic (DNA damaging) chemotherapy in p53-defective cells, the activated-hnRNPA0 post-transcriptionally regulated p27Kip1 and Gadd45-alpha by stabilizing mRNAs of each of these two proteins. In addition to in vitro studies, the authors also performed in vivo studies that involved the used the syngeneic system including hnRRNPA0-knocked down KP7B cells and immune-competent mice. The results of in vivo studies indicated that the growth of hnRNPA0-deficient tumors was considerably suppressed in response to cisplatin treatment including survival benefit to animals harboring hnRNPA0-deficient tumors. Thus, the authors concluded that hnRNPA0 serves to promote cisplatin resistance in lung tumors. They also performed additional studies using H1299 human lung cancer cells null for p53 and noted increased sensitization to cisplatin following hnRNPA0 knockdown. Interestingly, knockdown of either p27Kip1 or Gadd45alph alone did not alter cellular sensitivity to cisplatin but combined knockdown of both gave results similar to those obtained for hnRNPA0. Based on these results and those form other series of experiments, the authors reported that hnRNPA0-mediated increased p27Kip1 led to activation of the G1/S checkpoint whereas increased Gadd45-alpha activated the G2/M checkpoint. They concluded that in p53-Defective cells, the DNA damaging chemotherapeutics such as cisplatin can activate hnRNPA0-dependent p27Kip1 and Gadd45-alpha to induce G1/S and G2/M checkpoints and thereby limit the effectiveness of the anticancer drugs. The authors performed additional studies to explore the clinical relevance of their findings and to that end, utilized data from a clinical trial that had NSCLC stage IB or II patients managed with surgery plus cisplatin/vinorelbine in adjuvant setting or no adjuvant chemotherapy. They specifically focused on stage II patients and found that tumors from patients expressing higher levels of p27Kip1 and Gadd45-alpha did not benefit from adjuvant chemotherapy while those with tumors expressing low levels of these markers did. Furthermore, the authors also stratified patients in relation to p53 status and that was done using the p53 immunohistochemical staining because they assumed that immunohistochemistry-based p53 positivity would indicate p53 mutant status while the absent staining would suggest wild type p53. The authors noted that patients with tumors having low levels of p27Kip1 and Gadd45-alpha as well as possible p53 mutations (based on immunohistochemistry) benefited from cisplatin-based chemotherapy.
It is clear, Cannell et al (10), have provided interesting new insights into the potential mechanisms by which NSCLC cells may exhibit sensitivity/resistance to genotoxic chemotherapy. The reported hnRNPA0-mediated post-transcriptional regulation of p27Kip1 and Gadd45-alpha are interesting findings. Another interesting finding is the implication of p27Kip1 in DNA damage-induced G1/S checkpoint control as p27Kip1 was generally not thought of a major player in this context. Because Gadd45-alpha is transcriptionally regulated by p53 in response to DNA damage, the notion that a switch from transcriptional control to post-transcriptional control can occur in terms of Gadd45-alpha regulation is also an interesting concept. The outcome of the clinically-relevant studies also supports their in vitro and in vivo studies and highlights the potential of hnRNPA0, p27Kip1 and Gadd45-alpha as markers of response to therapy in NSCLC. Clearly however, there are also limitations of their findings. For example, the patient pool is small. Furthermore, p53 analyses were performed by immunohistochemistry that is not an optimal approach to determine the wild type or mutant status of p53. Because it is generally thought that mutant-p53 is more stable and consequently amenable to detection by immunohistochemistry, immunohistochemical approach is often used to determine the p53 wild type or mutant status. However, there are reports of false-positive and false-negative results associated with this approach to detect p53 status (reviewed in 16). Furthermore, not all mutations disrupt the wild type function of p53 thus, identification of the nature of p53 mutation is also important (17). In addition, function of wild type p53 could still be compromised through various other means including p53 mislocalization, presence of p53 interacting viral proteins, status of MDM2 and other ligases, just to name a few. It is of note that in the clinic, the contribution of the wild type or mutant p53 in predicting response to anti-cancer therapies remains debatable (17 and refs. therein). Clearly then, the extent to which the p53 status would play a role in modulating genotoxic regulation of its downstream effectors such as Gadd45-alpha and hnRNPA0 would require more in-depth studies.
Gadd45-alph is a downstream target of p53 and is transcriptionally upregulated by p53 in response to genotoxic agents. Cannell et al (10), conclude that in p53-null cells because genotoxic regulation of Gadd45-alpha occurs via the MK2/hnRNPA0-dependent post-transcriptional stability of its mRNA therefore, the Gadd45-alpha-dependent G2/M checkpoint control remains intact. In this context, it is of note that in earlier studies, Gadd45-alpha-mediated checkpoint has been reported to require wild type p53 function (15, 18). It has also been reported that Gadd45-alpha appeared to be required for G2/M checkpoint induced by genotoxic agents such as UV and MMS but not for that induced by ionizing radiation (15). Clearly, more in-depth studies are needed in lung cancer and other malignancies to ascertain the extent of the contribution of Gadd45-alpha in mounting G2/M checkpoint particularly in relation to hnRNPA0, p53 status and the type of genotoxic chemotherapy.
The genomic landscape of tumors originating from different organs remains variable and that is in addition to the heterogeneity that exists among tumors of the same organ type. Cannell et al (10) have identified a signaling network involving MK2/hnRNPA0, p27Kip1 and Gadd45-alpha that may predict response to chemotherapy. The question now is, whether this network is restricted only to a subset of tumors or more broadly relevant across multiple tumor types. Further studies are certainly needed to gain additional insights.
Acknowledgement
The work in author's laboratory was supported in part by the NIH grant CA157168.
Footnotes
Conflicts of Interest
No conflicts of interest to declare.
References
- 1.Sheikh MS, Carrier F, Papathanasiou MA, et al. Identification of several human homologs of hamster DNA damage-inducible transcripts. Cloning and characterization of a novel UV-inducible cDNA that codes for a putative RNA-binding protein. J Biol Chem. 1997;272:26720–6. doi: 10.1074/jbc.272.42.26720. [DOI] [PubMed] [Google Scholar]
- 2.Corcoran CA, Luo X, He Q, Jiang C, Huang Y, Sheikh MS. Genotoxic and endoplasmic reticulum stresses differentially regulate TRB3 expression. Cancer Biol Ther. 2005;4:1063–7. doi: 10.4161/cbt.4.10.2205. [DOI] [PubMed] [Google Scholar]
- 3.American Cancer Society . Cancer facts & figures. American Cancer Society; Atlanta: 2015. 2015. [Google Scholar]
- 4.Esposito L, Conti D, Ailavajhala R, Khalil N, Giordano A. Lung cancer: are we up to the challenge? Curr Genomics. 2010;11:513–18. doi: 10.2174/138920210793175903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johnson DH, Schiller JH, Bunn PA., Jr Recent clinical advances in lung cancer management. J Clin Oncol. 2014;32:973–82. doi: 10.1200/JCO.2013.53.1228. [DOI] [PubMed] [Google Scholar]
- 6.American Cancer Society [Dec 28, 2015];Lung Cancer. http://www.cancer.org/cancer/lungcancer/
- 7.Chang A. Chemotherapy, chemoresistance and the changing treatment landscape for NSCLC. Lung Cancer. 2011;71:3–10. doi: 10.1016/j.lungcan.2010.08.022. [DOI] [PubMed] [Google Scholar]
- 8.Siddik ZH. Cisplatin: mode of cytotoxic action and molecular basis of resistance. Oncogene. 2003;22:7265–79. doi: 10.1038/sj.onc.1206933. [DOI] [PubMed] [Google Scholar]
- 9.Dasari S, Tchounwou PB. Cisplatin in cancer therapy: molecular mechanisms of action. Eur J Pharmacol. 2014;740:364–78. doi: 10.1016/j.ejphar.2014.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cannell IG, Merrick KA, Morandell S, et al. A leiotropic RNA-binding protein controls distinct cell cycle checkpoints to drive resistance of p53-Defective tumors to chemotherapy. Cancer Cell. 2015;28:623–37. doi: 10.1016/j.ccell.2015.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Myer VE, Steitz JA. Isolation and characterization of a novel, low abundance hnRNP protein: A0. RNA. 1995;1:171–82. [PMC free article] [PubMed] [Google Scholar]
- 12.Chaudhury A, Chander P, Howe PH. Heterogeneous nuclear ribonucleoproteins (hnRNPs) in cellular processes: Focus on hnRNP E1's multifunctional regulatory roles. RNA. 2010;16:1449–62. doi: 10.1261/rna.2254110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reinhardt HC, Cannell IG, Morandell S, Yaffe MB. Is post-transcriptional stabilization, splicing and translation of selective mRNAs a key to the DNA damage response? Cell Cycle. 2011;10:23–7. doi: 10.4161/cc.10.1.14351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hollander MC, Sheikh MS, Bulavin DV, et al. Genomic instability in Gadd45a-deficient mice. Nat Genet. 1999;23:176–84. doi: 10.1038/13802. [DOI] [PubMed] [Google Scholar]
- 15.Wang XW, Zhan Q, Coursen JD, et al. GADD45 induction of a G2/M cell cycle checkpoint. Proc Natl Acad Sci USA. 1999;96:3706–11. doi: 10.1073/pnas.96.7.3706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Olivier M, Hollstein M, Hainaut P. TP53 mutations in human cancers: origins, consequences, and clinical use. Cold Spring Harb Perspect Biol. 2010;2:a001008. doi: 10.1101/cshperspect.a001008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Netter J, Lehmann-Che J, Lambert J, Tallet A, et al. Functional TP53 mutations have no impact on response to cytotoxic agents in metastatic colon cancer. Bull Cancer. 2015;102:117–25. doi: 10.1016/j.bulcan.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 18.Jin S, Tong T, Fan W, et al. GADD45-induced cell cycle G2-M arrest associates with altered subcellular distribution of cyclin B1 and is independent of p38 kinase activity. Oncogene. 2002;21:8696–704. doi: 10.1038/sj.onc.1206034. [DOI] [PubMed] [Google Scholar]