Abstract
Background: Childhood maltreatment (CM) can increase the risk of psychosocial risk factors in adulthood (e. g. intimate partner violence, financial problems, substance abuse or medical problems). The transition to parenthood presents those affected by CM with particular challenges, in addition to usual birth-related stressors. Methods: In this cross-sectional study a total of 240 women were interviewed in the puerperium with respect to CM experiences, using the German version of the Childhood Trauma Questionnaire (CTQ). Current psychosocial risk factors (e. g. financial concerns, maternal mental illness, single parent) were assessed using the Constance Index (KINDEX) for early childhood risk factors. Associations between CM experience and psychosocial risk factors were calculated using simple correlation. Results: The average age of participants was 33 years. On the CTQ 13.8 % of participants reported emotional abuse, 6.7 % physical abuse and 12.5 % sexual abuse, while 32.1 % reported emotional neglect and 7.5 % physical neglect during childhood. With rising severity of CM, more psychosocial risk factors (KINDEX) were present. Conclusions: This study shows a clear association between experiences of maltreatment during childhood and the presence of psychosocial stressors among women in the puerperium. Regular screening for a history of CM and parental psychosocial stressors should be conducted early, i.e. during pregnancy, to avoid negative consequences for the child.
Key words: psychosocial risk factors, childhood maltreatment, prevalence, prenatal screening, KINDEX
Abstract
Zusammenfassung
Hintergrund: Missbrauch, Misshandlung und Vernachlässigung (MMV) in der Kindheit können das Risiko für psychosoziale Belastungen im Erwachsenenalter (bspw. partnerschaftliche Gewalt, finanzielle Schwierigkeiten, Substanzkonsum oder medizinische Probleme) erhöhen. Im Übergang von der Schwangerschaft zur Elternschaft sind Betroffene, zusätzlich zu alltäglichen Stressoren rund um die Geburt, vor besondere Herausforderungen gestellt. Methode: Insgesamt 240 Frauen im Wochenbett wurden bez. MMV-Erfahrungen in der Kindheit mit der deutschen Version des Childhood Trauma Questionnaire (CTQ) und psychosozialer Risiken (bspw. finanzielle Sorgen, psychische Erkrankung der Mutter, alleinerziehend) mit dem Konstanzer Index (KINDEX) für frühkindliche Risiken in einer Querschnittsstudie befragt. Zusammenhänge zwischen MMV-Erfahrungen und psychosozialen Risiken wurden mittels Korrelationen berechnet. Ergebnisse: Von den durchschnittlich 33 Jahre alten Frauen berichteten 13,8 % emotionale und 6,7 % körperliche Misshandlung, 12,5 % sexuellen Missbrauch sowie 32,1 % emotionale und 7,5 % körperliche Vernachlässigung anhand des CTQs in der Kindheit. Je mehr MMV erlebt worden war, desto mehr psychosoziale Risikofaktoren (KINDEX) lagen vor. Schlussfolgerungen: Die Studienergebnisse zeigen einen deutlichen Zusammenhang zwischen MMV-Erfahrungen in der eigenen Kindheit und dem Auftreten psychosozialer Belastungen bei Frauen im Wochenbett. Um negative Auswirkungen dieses Zusammenhangs auf die Kinder zu vermeiden, sollten frühzeitige und regelmäßige Screening-Verfahren nach MMV-Erfahrungen und elterlichen psychosozialen Belastungen bereits während der Schwangerschaft eingesetzt werden.
Schlüsselwörter: psychosoziale Risikofaktoren, Missbrauchs- und Vernachlässigungserfahrungen, Prävalenz, pränatales Screening, KINDEX
Introduction
Critical life events such as the transition to parenthood present new challenges to expectant parents 1. Aside from the happiness about the childʼs birth, this period is sometimes characterised by worries about the future as a family. Parents often reflect on their own childhood – both positive and negative experiences. Childhood traumata such as childhood maltreatment (CM) can be particularly burdensome for those affected, with long-term consequences well into adulthood 2. Mothers with a history of childhood maltreatment are more vulnerable to stress 3, suffer postnatal depression more often 4, and in many cases lack adequate role models of sensitive parenting in their own childhood 5. The birth of a child and the associated workload, as well as adjustment to the parenting role represent particular challenges for these mothers.
According to the World Health Organization CM is a global problem 6 with far reaching (including financial) consequences for society 7. CM is defined as acts of commission (physical, emotional and sexual abuse) or acts of omission (emotional and physical neglect) by parents/care givers that harm or threaten of harm children or their well-being 8. As the number of CM experiences increases, so the risk of secondary psychological and physical disorders seems to rise 9.
In comparison to other countries only few studies of CM prevalence have been carried out in the German-speaking region 10. The following prevalence rates for at least mild CM experiences were obtained using the Childhood Trauma Questionnaire (CTQ; 11) on a representative German population sample: emotional neglect 49.5 %, physical neglect 48.4 %, physical abuse 12 %, emotional abuse 15 % and sexual abuse 12.6 % 12.
Childhood maltreatment influences not only mental health in childhood and adolescence, but also the risk of psychosocial problems throughout life (for a review see 2 or 13; for women specifically: 14). Those affected have more health problems 13, 15, increased risk of psychopathology (e.g. depression, post-traumatic stress disorder, personality disorders 16, 17, 18) and tend to be less stress resistant 3 in adulthood.
The children of parents with CM have an increased risk of being neglected and/or abused in turn 19, 20, 21. However a transmission rate of 6.7 % 22 indicates that the majority of parents with CM experience manage to break this so-called “cycle of maltreatment”, and that the presence of further risk factors is essential: “parenthood under the age of 21 years”, “a history of mental illness” and “intimate partner violence” are responsible for 53 % of intergenerational transmission 19. Safe and stable relationships are protective 23. In addition to increased risk via direct transmission of CM, indirect mechanisms can also contribute to unfavourable outcomes for these children. The increased likelihood of maternal mental illness and unsecure, disorganised mother-child attachment can have negative effects on maternal parenting style and the relationship to her child 2, 24.
In the transition from pregnancy to parenthood, childhood maltreatment and its consequences are risk factors that impact on both maternal health and child welfare. In Germany, partly as a consequence of various tragic child protection cases, the availability of preventive support for young families has increased as part of so-called “Frühe Hilfen” (early support – a governmental initiative for coordinated support systems for parents and children during pregnancy and early childhood).
The aim of this study was to establish the prevalence of childhood maltreatment in early postpartum mothers retrospectively, and to gather information on further psychosocial risk factors using the Constance INDEX (KINDEX; 25, 26, 27) – a screening tool for use around the time of birth that assesses the following risk factors: (previous) maternal mental illness, complicated prenatal attachment, current stress, socioeconomic problems, young mother, migration, single parent, intimate partner violence, medical problems and substance abuse. We aimed to explore to what extent CM experiences correlate positively with the occurrence of psychosocial risk factors in these postpartum mothers.
Materials and Methods
Study design and sample
Of the 2884 women who gave birth in the obstetric department of the University Hospital Ulm between 03/2012 and 05/2013, 240 gave written informed consent to participation in the study. Exclusion criteria were age under 18 years, insufficient knowledge of the German language and maternal psychotic disorder or drug abuse. In addition, for ethical reasons no women whose newborns were admitted to the neonatal intensive care unit were approached, since they were regarded as being under additional stress. For similar reasons no women were included whose own health problems were regarded by medical staff as too severe to allow interviewing. See Fig. 1 for a summary of the recruitment process, withdrawal rates and reasons for exclusion. Participants were interviewed on the postnatal ward by trained interviewers within six days after parturition. In addition to sociodemographics, data were collected on psychosocial risk factors, using the KINDEX, and CM experiences using the Childhood Trauma Questionnaire 11. Acknowledging the special emotional condition of women in the immediate postpartum period, all data were collected in a single interview by trained study personnel, ensuring that possible emotional reactions to questions pertaining to CM experiences be picked up and managed if necessary. The Ulm Universityʼs ethics commission approved the study.
Fig. 1.
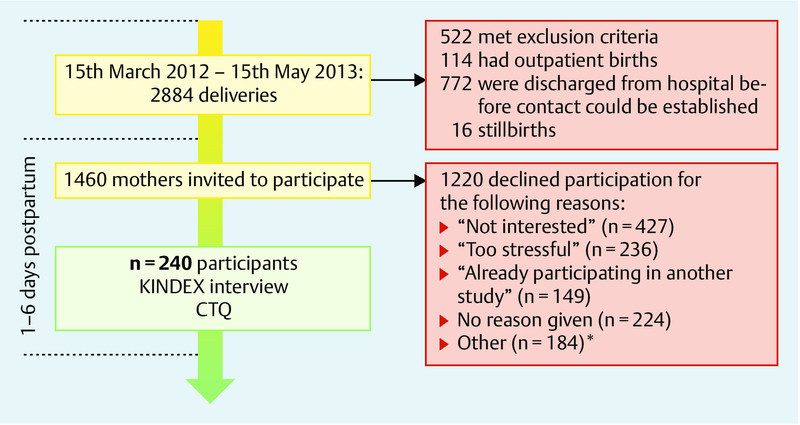
Study recruitment and withdrawal rates. * Other reasons given for participation refusal include husbands not agreeing to the participation of their wives, that questions were too private, or that women did not want to talk about their childhood.
Instruments
Maternal experiences of CM were assessed using the German version of the Childhood Trauma Questionnaire (CTQ; 11). Experiences of emotional abuse (e.g. “people in my family said hurtful or insulting things to me”), physical abuse (e.g. “people in my family hit me so hard that it left me with bruises or marks”), emotional neglect (items with inverted formulation e.g. “I felt loved”), physical neglect (e.g. “I had to wear dirty clothes”) and sexual abuse (e.g. “someone tried to make me do sexual things or watch sexual things”) are assessed on a 5-point Likert scale with five items per scale. Study workers read the questions to participants in a standardised way, and the women answered according to the CTQ Likert scale, which they were given in paper form. Clinical cut-offs allow subclassification on each subscale into “none/mild”, “mild/moderate”, “moderate/severe” and “severe/extreme” experiences 11. The total score from the entire scale gives a value between 25 and 125 that is a measure of cumulative CM experience.
Psychosocial risk factors for healthy child development were assessed using the KINDEX 25. This instrument was developed for use by medical personnel without special psychotherapeutic training, such as midwives and gynaecologists, to facilitate the referral of high-risk women for appropriate support. We modified the KINDEX for retrospective acquisition of psychosocial data in the postnatal period. In its paper version the KINDEX interview takes 20 to 40 minutes to complete. It covers 11 risk areas that can negatively influence healthy child development, with 31 items from which a cumulative score is arrived at (Table 1, cf. 26, 27, 28; Cronbachʼs alpha: 0.62). This multidimensional instrument has no built-in thresholds. To avoid repetition of questions, the subscales “physical abuse” and “sexual abuse” from the CTQ replaced the two similar titled items from the KINDEX for the risk area “traumatic experiences during childhood”. The risk area was regarded as fulfilled if at least mild/moderate experiences of physical abuse or sexual abuse were reported on the CTQ.
Table 1 Psychosocial risk factors (KINDEX) in the 240 participating mothers.
| n | % | |
|---|---|---|
| 1 Housing index (rooms/no. of people) ≤ 0.5 2 E. g. birth-related symptoms (e.g. afterpains, lower abdominal/pelvic pain etc.). 3 E. g. breech presentation, pregnancy-related diabetes, antepartum haemorrhage. 4 E. g. advanced maternal age, hypertension and obesity. 5 Low = 0 to 3 on a scale of 0 to 10. 6 n = 238 7 High = 7 to 10 on a scale of 0 to 10. 8 n = 239 9 Assessed using the Perceived Stress Scale 4 (PSS-4); PSS-4 sum score ≥ 12. 10 38 women reported depression (70.4 %), 13 (24.1 %) an anxiety disorder, 7 (13 %) an eating disorder, 4 (7.4 %) borderline personality disorder and ADHD symptoms, posttraumatic stress disorder, somatisation disorder, addiction were each reported by 1 woman (each 1.9 %). | ||
| 1) Young age | ||
|
0 | 0 |
| 2) Migration | ||
|
38 | 15.8 |
|
50 | 20.8 |
| 3) Single parent/parents living apart | ||
|
14 | 5.8 |
| 4) Financial problems | ||
|
15 | 6.3 |
|
7 | 2.9 |
| 5) Medical problems | ||
|
142 | 59.2 |
|
96 | 40 |
|
90 | 37.5 |
| 6) Complicated prenatal attachment | ||
|
45 | 18.8 |
|
0 | 0 |
|
2 | 0.8 |
|
39 | 16.3 |
|
42 | 17.6 |
| 7) Perceived stress levels in previous 4 weeks very high9 | 5 | 2.1 |
| 8) Intimate partner violence | ||
|
38 | 15.9 |
|
44 | 18.4 |
|
1 | 0.4 |
|
31 | 13.0 |
| 9) Substance abuse | ||
|
16 | 6.7 |
|
9 | 3.8 |
|
0 | 0 |
|
62 | 25.9 |
|
147 | 61.5 |
|
4 | 1.7 |
| 10) Mental illness (current or previous) in mother | ||
|
54 | 22.5 |
|
39 | 16.3 |
|
89 | 37.1 |
|
18 | 7.5 |
Statistics
The statistics program SPSS version 21 29 was used for all analyses. Descriptive data were described as mean values (M) and standard deviations (SD) or absolute (n) and relative incidence (in %). Because of the ordinal scale level of the KINDEX, comparison of groups was performed using the Mann-Whitney U test, and relationships between variables was analysed using Pearson correlation for continuous data and Spearman correlation for ordinally scaled data. P-value correction by the Holm method 30 was performed for multiple comparisons. Because of the theoretical overlap between the KINDEX and the CTQ, the KINDEX risk area “traumatic experiences during childhood” was removed from the analysis of the association between CM (CTQ sum score) and psychosocial risk factors (KINDEX sum score) in order to avoid multicollinearity.
Results
Sample description
The average age of the 240 participants at the time of parturition was 33 years (range = 21–46), the average number of children (including the newborn) was 1.78 (range = 1–6) and the current pregnancy was planned in 81.3 % (n = 195). 77.5 % (n = 186) was married and 95 % (n = 228) cohabited with their partner/spouse. The majority were of German origin (84.2 %; n = 202) and 57.1 % (n = 137) had achieved a general higher education exemption.
99.17 % of women stated their biological mother had been their main female parental figure in the period from birth to 17 years of age; the biological father was the main male parental figure for this time period for 96.25 % of women. All women gave female parental figures while three (1.25 %) could not name a male parental figure. Six women (2.5 %) spent time in foster homes or similar institutions (from 1 week to 18 years; M = 3.45 years, SD = 7.14 years). Two of these women reported at least moderate CM experiences in at least one type of CM on the CTQ. 45 womenʼs parents separated during their childhood or youth (data missing for 35 women) and 28.9 % (n = 13) of these women reported at least moderate CM experiences compared to 12.5 % (n = 20) of women whose parents remained together (n = 160). With a mean value of 5.7 (SD = 3.7), women whose parents had separated showed higher levels of psychosocial stress on the KINDEX than those whose parents had not separated (M = 4.4, SD = 2.4), however the difference missed statistical significance (Mann-Whitney U = 2911, p = 0.09).
Prevalence of childhood maltreatment
Overall 97 women (40.4 %) reported at least mild to severe CM experiences in at least one type of CM. 37 women (15.4 %) had at least moderate to severe CM experiences in childhood. The women reported:
emotional abuse: at least mild: 33 women (13.8 %), at least moderate: 13 women (5.4 %)
physical abuse: at least mild: 16 women (6.7 %), at least moderate: 10 women (4.2 %)
sexual abuse: at least mild: 30 women (12.5 %), at least moderate: 17 women (7.1 %)
emotional neglect: at least mild: 77 women (32.1 %), at least moderate: 23 women (9.6 %)
physical neglect: at least mild: 18 women (7.5 %), at least moderate: 8 women (3.3 %)
There was highly significant correlation between all forms of abuse and neglect (all r = 0.24 to 0.70, all p < 0.001). In addition 42 women (17.5 %) reported at least mild, and 18 women (7.5 %) at least moderate CM experiences in more than two subscales. Values for CTQ sum score, as a measure of cumulative CM experience, lay between 25 and 107 (M = 32.53, SD = 11.21).
CM and psychosocial risk factors
The frequencies of psychosocial risk factors reported on the KINDEX are shown in Table 1. The average sum score of all participants was 4.68 (SD = 2.71, range = [0;15]). The CTQ sum score correlated significantly with psychosocial risk factors on the KINDEX at the end of pregnancy (r = 0.32, p < 0.001; Fig. 2). The associations with individual KINDEX risk areas are shown in Table 2. CM correlated most strongly with self-reported mental health problems (r = 0.36, p < 0.001) and intimate partner violence (r = 0.33, p < 0.001).
Fig. 2.
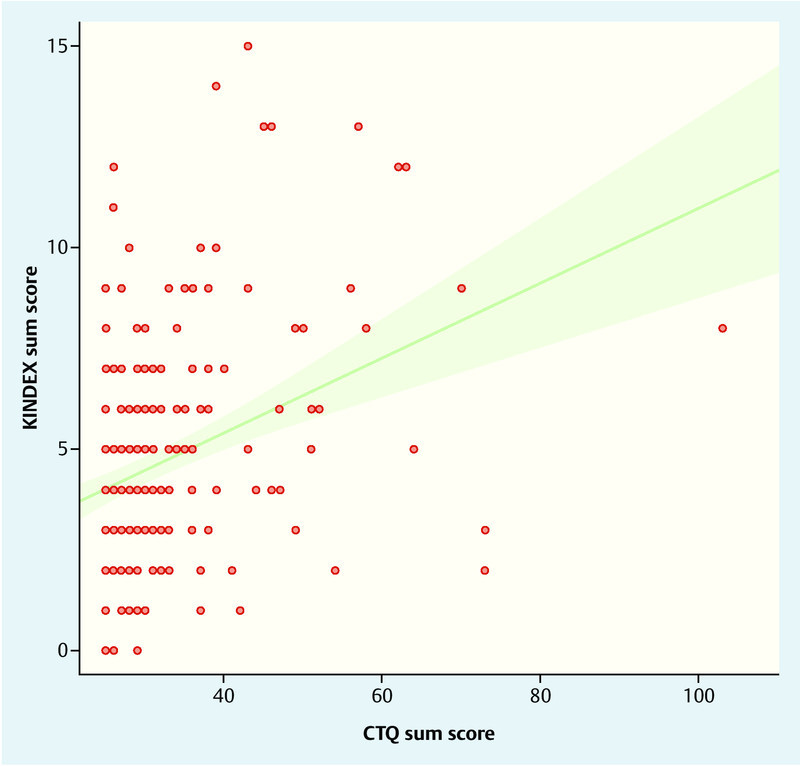
Estimated linear association between CTQ and KINDEX sum scores. The green area represents the 95 % confidence interval. Possible range of CTQ sum score: [25;125]. Possible range of KINDEX sum score: [0;29].
Table 2 Spearman Rho correlations of KINDEX risk areas with CM experiences (represented by the CTQ sum score).
| Correlations with CTQ sum score | ||||
|---|---|---|---|---|
| n | r | p | padj 2 | |
| * p < 0.05, ** p < 0.01, *** p < 0.001 1 assessed using the Perceived Stress Scale 4 (PSS-4) sum score. 2 p-values after Holm correction for multiple comparisons 30. | ||||
| Migration | 240 | 0.04 | 0.51 | 1 |
| Single parent | 240 | 0.19 | 0.004** | 0.024* |
| Financial problems | 240 | 0.23 | < 0.001*** | 0.002** |
| Medical problems | 240 | 0.10 | 0.14 | 0.56 |
| Complicated prenatal attachment | 238 | 0.04 | 0.50 | 1 |
| Very high perceived stress level1 | 240 | 0.12 | 0.07 | 0.35 |
| Intimate partner violence | 239 | 0.33 | < 0.001*** | < 0.001*** |
| Substance abuse | 239 | 0.04 | 0.53 | 1 |
| (Previous) mental illness | 240 | 0.36 | < 0.001*** | < 0.001*** |
Discussion
The prevalence rates for CM found in this sample of women in the puerperium are consistent with previously described prevalences of Germany (Table 3) with the exception of physical abuse (6.7 vs. 22.9 % in Europe as a whole; 31) and physical neglect (7.5 vs. 48.4 % in a German population sample; 12). These discrepancies may partially be due to the relatively younger average age of women in the current study (Table 3): Häuser et al. 12 describe an association between more advanced age and more reported physical neglect. In addition, the catchment area of the obstetric department of the University Hospital Ulm is characterised by very good socioeconomic status (e.g. low unemployment rate). Other contributing factors may include study method, sample characteristics and differing definitions of CM.
Table 3 CM prevalence rates of current study compared to Häuser et al. 12 and Stoltenborgh et al. 31.
| n | Age range in years | Emotional abuse | Physical abuse | Sexual abuse | Emotional neglect | Physical neglect | |
|---|---|---|---|---|---|---|---|
| 1 Review of four metaanalyses; the reported frequencies are taken from the summary of prevalence rates of 90 European studies; no total sample size or average proband age is stated for the European studies. 2 Only women surveyed. 3 Insufficient European studies, therefore worldwide prevalence stated. | |||||||
| Koenig et al. | 240 | 21–46(M = 33.1, SD = 5.2) | 13.8 %2 | 6.7 %2 | 12.5 %2 | 32.1 %2 | 7.5 %2 |
| Häuser et al. | 2 504 | 14–90(M = 50.6, SD = 18.6) | 15 % | 12 % | 12.6 % | 49.5 % | 48.4 % |
| Stoltenborgh et al.1 | – | – | 29.2 % | 22.9 % | 13.5 %2 | 18.4 %3 | 6.5 % |
A national strategy to record CM prevalence rates would constitute an important step towards sustained improvement of child protection in Germany 32. The 2013 change to the coding ordinance, which up until then has forbidden the use of ICD-10 codes (ICD-10 GM) for CM in German hospitals (T.74x; covers among others the diagnoses “neglect or abandonment”, “physical abuse”, “sexual abuse”, “psychological abuse”), could constitute an empiric basis for recording exact prevalence rates if used more systematically in clinical practice. Such data have proven to be reliable and resilient in other cultural contexts 33. A more detailed classification of traumatising (relationship) experiences, currently made difficult by unclear criteria, is being discussed for the ICD-11 to facilitate easier identification of CM during health examinations (for a review see 34).
The number of risk factors also had an effect on healthy or negative child development. The more CM had been experienced, the more psychosocial risk factors were present at transition to parenthood. Especially strong positive correlations were shown between CM and the KINDEX risk factors “(previous) mental illness” and “intimate partner violence” – a combination that can lead to negative parenting behaviour 4 and less appropriate, sensitive maternal reactions towards her child 35. In general, literature indicates an elevated risk for CM of children whose parents exihibit increased psychosocial risk factors 23, 36 – a cycle of maltreatment. Preventive programs can help to break this cycle of maltreatment such as linking up with community midwives, parental counselling by so-called “Babylotsen” (baby guards) while still on the postnatal ward as in the Berlin project “Babylotse plus Charité”, promotion of early parent-child attachment through e. g. developmental psychological advice 37 and others. In the context of the so-called “Frühe Hilfen” (early support) numerous political and communal initiatives as well as project models have been promoted, both regionally and nationally in Germany, and a national centre for early support (“Nationales Zentrum für Frühe Hilfen”) has been established. A preliminary endpoint was achieved with the passing of the Child Protection Act (01. 01. 2012) and the incorporated national early support initiative (financial support for community midwives, network structures). In addition to the creation and development of a broad, locally available, interdisciplinary pallet of offers for parents, a central aim of the Act is to establish and strengthen local networks, particularly between the health system and Child and Youth Welfare. Reliable, evaluated risk screening tools designed for use around the time of childbirth are an empiric requirement for the development of a “common language” between systems. Some examples of the few tools available in German-speaking countries include the “Anhaltsbogen für ein vertiefendes Gespräch” or the “LuPE-Bogen” 38, 39, the “Pädiatrischer Anhaltsbogen zur Einschätzung von psychosozialem Unterstützungsbedarf (U3–U6)” 40 and the KINDEX 25, 26, 27. These screening methods can help to systematically identify potential risks to child development, thus allowing referral of parents for specific, appropriate support.
A limitation of the study is that only 16.4 % of women approached in the obstetric department agreed to participate. For data protection reasons the extent to which non-participants differed from participants with regards to sociodemographics and medical factors is not determinable. Refusal to participate may have been due to the difficult/awkward nature of the study subject matter, CM in particular, although patients did not specifically state this as a reason. Systematic screening incorporated into medical examinations – where possible during pregnancy – is therefore a desirable aim. In addition we cannot be sure that the reporting of CM experiences was not influenced by the fact that the CTQ was administered as an interview. The study sample comprised adult women over the age of 21 years, meaning the KINDEX risk area “young age” cannot be interpreted. Associations between CM and psychosocial risk factors were demonstrated even in the group of women with relatively mild psychosocial stress, above average education and CM prevalence slightly lower than that of the general population, which again underlines the need for preventive screening – even for mild CM experiences.
Conclusion
Experiencing maltreatment and neglect in oneʼs own childhood is associated with psychosocial risk factors later in life at the transition to parenthood. The more childhood maltreatment experiences occur, the higher the risk of mental illness and the more likely those affected will be single parents, have financial problems or experience intimate partner violence. Early and systematic screening for potential psychosocial risk factors in parents using an appropriate tool such as the KINDEX (downloadable as an interview and mobile app at http://www.mykind.info; 41) is indispensible in preventing the negative consequences of a “cycle of maltreatment”. Screening can markedly improve early, individually tailored, interdisciplinary support provided by diverse social systems. Practical experience to date (e.g. the national project model “Guter Start ins Kinderleben” in Ludwigshafen 39, 42, the practice and research project “Babylotse plus Charité” in Berlin, “Babyforum” in the Constance/Ortenaukreis and others) has shown that systematic screening as part of clinical routine in obstetric departments works – provided the local protocols and referral pathways to early support services are well established.
Acknowledgements
Alexandra Koenig received a scholarship from the Konrad Adenauer Foundation. Katharina Schury was supported by a scholarship from the German National Academic Foundation.
Footnotes
Conflict of Interest Iris-Tatjana Kolassa gave a talk in a symposium sponsored by Souvenaid. All other authors declare no conflict of interest.
Supporting Information
References
- 1.Deave T, Johnson D, Ingram J. Transition to parenthood: the needs of parents in pregnancy and early parenthood. BMC Pregnancy Childbirth. 2008;8:30. doi: 10.1186/1471-2393-8-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gilbert R, Widom C S, Browne K. et al. Burden and consequences of child maltreatment in high-income countries. Lancet. 2009;373:68–81. doi: 10.1016/S0140-6736(08)61706-7. [DOI] [PubMed] [Google Scholar]
- 3.Vranceanu A M, Hobfoll S E, Johnson R J. Child multi-type maltreatment and associated depression and PTSD symptoms: the role of social support and stress. Child Abuse Negl. 2007;31:71–84. doi: 10.1016/j.chiabu.2006.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Malta L A, McDonald S W, Hegadoren K M. et al. Influence of interpersonal violence on maternal anxiety, depression, stress and parenting morale in the early postpartum: a community based pregnancy cohort study. BMC Pregnancy Childbirth. 2012;12:153. doi: 10.1186/1471-2393-12-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Godbout N, Briere J, Sabourin S. et al. Child sexual abuse and subsequent relational and personal functioning: the role of parental support. Child Abuse Negl. 2014;38:317–325. doi: 10.1016/j.chiabu.2013.10.001. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization Hrsg.Global Status Report on Violence Prevention 2014 Genf: World Health Organization; 20141–18. [Google Scholar]
- 7.Fang X, Brown D S, Florence C S. et al. The economic burden of child maltreatment in the United States and implications for prevention. Child Abuse Negl. 2012;36:156–165. doi: 10.1016/j.chiabu.2011.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Leeb R T Paulozzi L J Melanson C et al. Hrsg.Child Maltreatment Surveillance: uniform Definitions for public Health and recommended Data Elements, Version 1.0 Atlanta, GA: Centers of Disease Control and Prevention, National Center for Injury Prevention and Control; 200811–19. [Google Scholar]
- 9.Schury K, Kolassa I T. Biological memory of childhood maltreatment – current knowledge and recommendations for future research. Ann N Y Acad Sci. 2012;1262:93–100. doi: 10.1111/j.1749-6632.2012.06617.x. [DOI] [PubMed] [Google Scholar]
- 10.Pillhofer M, Ziegenhain U, Nandi C. et al. Prävalenz von Kindesmisshandlung und -vernachlässigung in Deutschland – Annäherung an ein Dunkelfeld. Kindh Entwickl. 2011;20:64–71. [Google Scholar]
- 11.Bader K, Haenny C, Schaefer V. et al. Childhood Trauma Questionnaire – Psychometrische Eigenschaften einer deutschsprachigen Version. Z Klin Psychol Psychother. 2009;38:223–230. [Google Scholar]
- 12.Häuser W, Schmutzer G, Brähler E. et al. Maltreatment in childhood and adolescence – results from a survey of a representative sample of the general German population. Dtsch Arztebl Int. 2011;108:287–294. doi: 10.3238/arztebl.2011.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leeb R T, Lewis T, Zolotor A. A review of physical and mental health consequences of child abuse and neglect and implications for practice. Am J Lifestyle Med. 2011;5:454–468. [Google Scholar]
- 14.Briere J, Jordan C. Childhood maltreatment, intervening variables, and adult psychological difficulties in women: an overview. Trauma Violence Abuse. 2009;10:375–388. doi: 10.1177/1524838009339757. [DOI] [PubMed] [Google Scholar]
- 15.Krug E G Dahlberg L L Mercy J A et al. Hrsg.World Report on Violence and Health Genf: World Health Organization; 200259–86. [Google Scholar]
- 16.Hovens J G, Giltay E J, Spinhoven P. et al. Impact of childhood life events and childhood trauma on the onset and recurrence of depressive and anxiety disorders. J Clin Psychiatry. 2015;76:931–938. doi: 10.4088/JCP.14m09135. [DOI] [PubMed] [Google Scholar]
- 17.Wosu A C, Gelaye B, Williams M A. Childhood sexual abuse and posttraumatic stress disorder among pregnant and postpartum women: review of the literature. Arch Womens Ment Health. 2015;18:61–72. doi: 10.1007/s00737-014-0482-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Samuels J. Personality disorders: epidemiology and public health issues. Int Rev Psychiatry. 2011;23:223–233. doi: 10.3109/09540261.2011.588200. [DOI] [PubMed] [Google Scholar]
- 19.Dixon L, Browne K, Hamilton-Giachritsis C. Risk factors of parents abused as children: a mediational analysis of the intergenerational continuity of child maltreatment (part I) J Child Psychol Psychiatry. 2005;46:47–57. doi: 10.1111/j.1469-7610.2004.00339.x. [DOI] [PubMed] [Google Scholar]
- 20.Berlin L, Appleyard K, Dodge K. Intergenerational continuity in child maltreatment: mediating mechanisms and implications for prevention. Child Dev. 2011;82:162–176. doi: 10.1111/j.1467-8624.2010.01547.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Widom C S, Czaja S J, DuMont K A. Intergenerational transmission of child abuse and neglect: real or detection bias? Science. 2015;347:1480–1485. doi: 10.1126/science.1259917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dixon L, Browne K, Hamilton-Giachritsis C. Patterns of risk and protective factors in the intergenerational cycle of maltreatment. J Fam Viol. 2009;24:111–122. [Google Scholar]
- 23.Thornberry T P, Henry K L, Smith C A. et al. Breaking the cycle of maltreatment: the role of safe, stable, and nurturing relationships. J Adolesc Health. 2013;53:S25. doi: 10.1016/j.jadohealth.2013.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cicchetti D, Toth S L. Child maltreatment. Annu Rev Clin Psychol. 2005;1:409–438. doi: 10.1146/annurev.clinpsy.1.102803.144029. [DOI] [PubMed] [Google Scholar]
- 25.Schauer M Ruf-Leuschner M KINDEX: Pränatale Erfassung psychosozialer Risiken für die Entwicklung über die Lebensspanne – Der Konstanzer INDEXSubmitted
- 26.Spyridou A, Schauer M, Ruf-Leuschner M. Obstetric care providers assessing psychosocial risk factors during pregnancy: validation of a short screening tool – the KINDEX Spanish version. Child Adoles Psychiatry Ment Health. 2014;8:30. doi: 10.1186/s13034-014-0030-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Spyridou A, Schauer M, Ruf-Leuschner M. Obstetric care providers are able to assess psychosocial risks, identify and refer high-risk pregnant women: validation of a short assessment tool – the KINDEX Greek version. BMC Pregnancy Childbirth. 2015;15:41. doi: 10.1186/s12884-015-0462-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ruf-Leuschner M Schauer M Externale und prospektive Validität des KINDEX – ein Instrument zur pränatalen Erfassung von psychosozialen Risikofaktoren bei SchwangerenIn preparation
- 29.IBM Corp . Armonk, NY: IBM Corp; 2012. IBM SPSS Statistics for Windows, Version 21.0. [Google Scholar]
- 30.Holm S. A simple sequentially rejective multiple test procedure. Scand Stat Theory Appl. 1979;6:65–70. [Google Scholar]
- 31.Stoltenborgh M, Bakermans-Kranenburg M J, Alink L R. et al. The prevalence of child maltreatment across the globe: review of a series of meta-analyses. Child Abuse Rev. 2015;24:37–50. [Google Scholar]
- 32.Pillhofer M. Erlangen-Nürnberg: Friedrich-Alexander-Universität Erlangen-Nürnberg; 2015. Prävalenz, Diagnostik und Prävention von Kindeswohlgefährdung. [Dissertation]
- 33.McKenzie K, Scott D A, Waller G S. et al. Reliability of routinely collected hospital data for child maltreatment surveillance. BMC Public Health. 2011;11:8. doi: 10.1186/1471-2458-11-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Slep A M, Heyman R E, Foran H M. Child maltreatment in DSM-5 and ICD-11. Fam Proc. 2015;54:17–32. doi: 10.1111/famp.12131. [DOI] [PubMed] [Google Scholar]
- 35.Malone J C, Levendosky A A, Dayton C J. et al. Understanding the “ghosts in the nursery” of pregnant women experiencing domestic violence: prenatal maternal representations and histories of childhood maltreatment. Infant Ment Health J. 2010;31:432–454. doi: 10.1002/imhj.20264. [DOI] [PubMed] [Google Scholar]
- 36.Stith S M, Liu T, Davies L C. et al. Risk factors in child maltreatment: a meta-analytic review of the literature. Aggress Violent Behav. 2009;14:13–29. [Google Scholar]
- 37.Ziegenhain U Derksen B Fegert J M Entwicklungspsychologische Beratung für junge Eltern Weinheim: Beltz Juventa; in press [Google Scholar]
- 38.Kindler H. Weinheim, München: Juventa; 2009. Wie könnte ein Risikoinventar für frühe Hilfen aussehen? pp. 170–261. [Google Scholar]
- 39.Filsinger B, Bechtold I, Gehrmann J. Die geburtshilfliche Anamnese als Schlüssel für frühe individuelle Hilfen nach der Geburt: das Präventionsprojekt am Ludwigshafener St. Marienkrankenhaus. Frauenarzt. 2008;49:528–530. [Google Scholar]
- 40.Barth M, Mall V. Köln: Nationales Zentrum Frühe Hilfen; 2015. Pädiatrischer Anhaltsbogen zur Einschätzung von psychosozialem Unterstützungsbedarf (U3 – U6) [Google Scholar]
- 41.Ruf-Leuschner M Brunnemann N Schauer M et al. Die KINDEX-App – ein Instrument zur Erfassung und unmittelbaren Auswertung von psychosozialen Belastungen bei Schwangeren in der täglichen Praxis bei Gynäkologinnen, Hebammen und in Frauenkliniken Verhaltenstherapie 2016. in press [Google Scholar]
- 42.Ziegenhain U, Schöllhorn A, Künster A K, Köln: Nationales Zentrum Frühe Hilfen; 2010. Modellprojekt Guter Start ins Kinderleben. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


