Abstract
Background
Physical activity is important for maintaining healthy weight. The time of day when exercise is performed—a highly discretionary aspect of behavior— may impact weight control, but evidence is limited. Thus, we examined the association between the timing of physical activity and obesity risk in women.
Methods
A cross-sectional analysis was conducted among 7157 Women’s Health Study participants who participated in an ancillary study begun in 2011 that is measuring physical activity using accelerometers. The exposure was percentage of total accelerometer counts accumulated before 12:00 noon and the outcome was obesity.
Results
Mean (±SD) BMI among participants was 26.1 (±4.9) kg/m2 and 1322 women were obese. The mean activity counts per day was 203,870 (±95,811) of which a mean 47.1% (±11.5%) were recorded in the morning. In multivariable-adjusted models, women who recorded <39% (lowest quartile) of accelerometer counts before 12:00 noon had a 26% higher odds of being obese, compared to those recording ≥54% (highest quartile) of counts before noon (Ptrend = 0.02).
Conclusions
These study findings—that women who are less active during morning hours may be at higher risk of obesity—if confirmed can provide a novel strategy to help combat the important health problem of obesity.
Keywords: exercise, accelerometry, overweight, epidemiology
INTRODUCTION
Engaging in regular physical activity on most days of the week is important for maintaining healthy weight.1 Although prior evidence supports 150 – 250 minutes of moderate-intensity physical activity per week to manage weight, the pattern through which physical activity is accumulated—duration, intensity, frequency, time of day—may also impact weight control.1-3 Of these, time of day may be easily changed, but there is little evidence available to determine if timing of exercise during the day has an effect on managing weight. A small intervention study found post-menopausal women who walked in the evening had greater reductions in fat mass than morning walkers.4 However, another small study showed that exercising in a fasted state (typically morning) is preferable for weight maintenance.5 Therefore, the purpose of this study was to examine the association between the time of day when physical activity occurred and prevalence of obesity in a large sample of older women.
METHODS
The Women’s Health Study is a completed randomized trial (1992-2004) testing aspirin and vitamin E for preventing cardiovascular disease and cancer among 39 876 initially healthy, U.S. female health professionals.6 Women provided written consent to participate and the study was approved by the institutional review board of Brigham and Women’s Hospital (Boston, Massachusetts). Following trial completion, participants were followed in an observational study. Women reported on medical history and lifestyle characteristics at baseline and annually during follow-up. An observational ancillary study begun in 2011 is assessing physical activity using accelerometers. This cross-sectional analysis includes women who returned their accelerometer by March 2013.
The accelerometer (Actigraph GT3X+, ActiGraph Corp.), detailed instructions for use, and wear time diary were mailed to participants. Subjects were instructed to wear the monitor for seven days during waking hours and record the days the monitor was worn.
Accelerometer data were screened for wear time using standard methods.7, 8 Briefly, non-wear time was defined as 90 consecutive minutes of zero counts, with an allowance of up to 2 minutes of nonzero counts, if there were 30-minute consecutive zero counts upstream and downstream. Wear days were identified using a diary (to avoid counting spurious physical activity while monitors were moving in mail transit). Participants with at least 4 days with ≥ 10 hours of wear per day were included in the analysis.9
Statistical Analysis
Participants were divided into quartiles based on percentage of total accelerometer counts accumulated before 12:00 noon. Total accelerometer counts per day was chosen as the exposure for this analysis as it represents total volume of physical activity performed.10 Body mass index (BMI, kg/m2) was calculated from self-reported height and weight and participants were classified as obese (BMI ≥ 30 kg/m2) or not obese. Logistic regression models were used and adjusted for wear time, age, smoking, caloric intake, fruit and vegetable intake, and total accelerometer counts to examine the association between morning exercise and odds of obesity. All analyses were performed using SAS statistical software, version 9.3 (SAS Institute Inc, Cary, North Carolina, United States).
RESULTS
Of 8373 women who returned the accelerometer by March 2013, we excluded 723 without a wear-time diary, 406 without at least 4 days of at least 10 hours of wear per day, and 87 missing BMI, resulting in 7157 women with mean (SD) age 71.4 (5.8) years. Women wore the accelerometer for a mean (SD) of 14.8 (1.2) hours per day over a mean (SD) of 6.8 (0.57) days. Mean (SD) BMI was 26.1 (4.9) kg/m2 and 1322 women were obese.
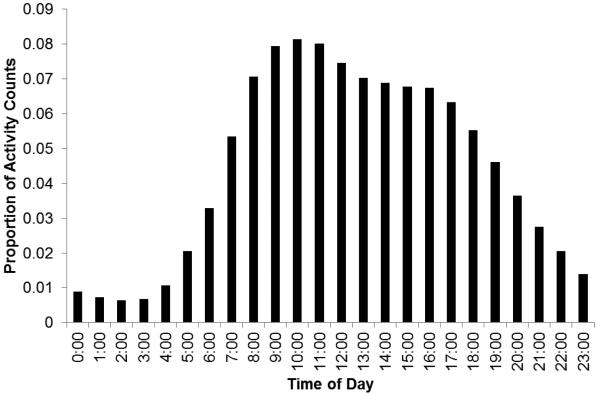
The mean (SD) total activity counts per day was 203,870 (95,811) of which a mean (SD) 47.1% (11.5%) were recorded in the morning. The distribution of counts per hour is shown in the Figure.
Figure.
Mean proportion of total accelerometer counts recorded during each hour of the day.
There was a significant trend (P = 0.02) for higher odds of obesity with lower percentages of accelerometer counts recorded in the morning (Table). In multivariable-adjusted models including total physical activity, women who recorded < 39% of their daily accelerometer counts before 12:00 noon had a 26% higher odds of being obese, compared to those recording ≥ 54% of counts before noon.
Table.
Odds ratios (95% CI) of obesity according to percentage of total accelerometer counts recorded before 12:00 noon.
| Percentage of daily accelerometer counts recorded before 12:00 noon | |||||
|---|---|---|---|---|---|
| ≥ 54% | 46 – 53.9% | 39 – 45.9% | < 39% | P for linear trend | |
| N | 1833 | 1893 | 1696 | 1735 | |
| Cases | 260 | 346 | 319 | 397 | |
| Crude | 1.00 | 1.35 (1.14, 1.61) | 1.40 (1.17, 1.68) | 1.80 (1.51, 2.13) | <.001 |
| Age-adjusted | 1.00 | 1.35 (1.13, 1.61) | 1.38 (1.16, 1.66) | 1.75 (1.47, 2.08) | <.001 |
| Age and wear-time adjusted |
1.00 | 1.34 (1.12, 1.59) | 1.35 (1.13, 1.62) | 1.62 (1.36, 1.93) | <.001 |
| Multivariable-adjusteda | 1.00 | 1.34 (1.12, 1.60) | 1.35 (1.13, 1.62) | 1.62 (1.36, 1.93) | <.001 |
| Multivariablea + total counts per day |
1.00 | 1.11 (0.92, 1.33) | 1.05 (0.87, 1.27) | 1.26 (1.05, 1.51) | 0.02 |
Adjusted for age, wear time, smoking, total calories, and fruit and vegetable intake.
DISCUSSION
To our knowledge, this is the first epidemiological study of the association between time of day of exercise and body weight. In this large study of older women, we found that time of day of objectively-measured physical activity was associated with obesity. Women who performed less of their total physical activity during the morning had higher odds of obesity compared to those who performed more. If these findings are confirmed, timing of physical activity can be a novel strategy for helping to control the health problem of obesity.
The present results are congruent with findings from a small study that showed early morning exercise in the fasted state improved insulin sensitivity and weight maintenance5. In that study, all healthy participants received a hyper-caloric, fat-rich diet and were assigned to either endurance training in the fasted state (no breakfast), endurance training with a carbohydrate-rich breakfast before training and carbohydrate ingestion during training sessions, and not training (control). Body weight increased in the control and carbohydrate before/during training group, but not in the fasted training group. Although we unfortunately do not have information on timing of breakfast consumption relative to physical activity in the current study, it is plausible that individuals who do more physical activity in the morning may perform some of that activity while in the fasted state.
Another plausible explanation for these findings is that engaging in morning activity is indicative of being awake during more of the morning hours and, thus, attaining more biologically appropriate light exposure, which influences sleep and circadian rhythms, both of which affect body weight.11,12 One recent study reported that having a majority of average daily light exposure of moderate intensity or greater earlier in the day was associated with lower BMI.11 Similarly, another study found a significant positive association between exposure to light at night and odds of obesity.12 An additional explanation, given the cross-sectional study design, is that being obese results in a reduction in morning physical activity, potentially through changes in sleep patterns or energy levels due to poor sleep quality.13
Strengths of present study include the large number of women and the objective measurement of physical activity using an accelerometer. Additionally, the results were adjusted for many variables that could potentially confound the association between timing of physical activity and obesity, including total amount of physical activity performed. In a sensitivity analysis, hours of sleep per night was also included in the model, since this may influence body weight, and the results were unchanged.
Limitations of this study include its cross-sectional design as physical activity and weight were measured during the same time period. Weight was self-reported, but this has been found to be highly correlated (r = 0.97) with directly measured weight in health professionals.14 The study population, consisting of predominantly white women of higher socioeconomic status, is not representative of the general population. Finally, although we had information on hours of sleep per night, we did not assess sleep quality, which may influence this association.
This intriguing finding that being active earlier in the day may lower the odds of being obese merits further research, since timing of activity could be a fairly simple behavior to change (as opposed to asking people to do more activity than they would typically carry out). Nonetheless, it should be emphasized that these results are hypothesis-generating only as they were based on cross-sectional analyses; thus additional prospective studies employing longitudinal designs are needed to confirm these findings. In the meantime, given the innumerable health benefits of exercise1, it is important to be active, regardless of time of day.
ACKNOWLEDGEMENTS
We are grateful to the staff of the Women’s Health Study (Brigham and Women’s Hospital), particularly Ara Sarkissian, MM, Bonnie Church, BA, Colby Smith, BS, and Jane Jones, MEd as well as Dr. Patty Freedson, PhD.
This research was supported by research grants CA154647, CA047988, HL043851, HL080467, and HL099355 from the National Institutes of Health.
REFERENCES
- 1.Physical Activity Guidelines Advisory Committee . Physical Activity Guidelines Committee Report, 2008. U.S. Department of Health and Human Services; Washington, D.C.: 2008. p. 683. [Google Scholar]
- 2.Donnelly JE, Blair SN, Jakicic JM, et al. American College of Sports Medicine. American College of Sports Medicine Position Stand Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009;41(2):459–71. doi: 10.1249/MSS.0b013e3181949333. doi: 10.1249/MSS.0b013e3181949333. [DOI] [PubMed] [Google Scholar]
- 3.Li J, O’Connor LE, Zhou J, Campbell WW. Exercise patterns, ingestive behaviors, and energy balance. Physiol Behav. 2014;134:70–5. doi: 10.1016/j.physbeh.2014.04.023. doi: 10.1016/j.physbeh.2014.04.023. [DOI] [PubMed] [Google Scholar]
- 4.Di Blasio A, Di Donato F, Mastrodicasa M, et al. Effects of the time of day of walking on dietary behaviour, body composition and aerobic fitness in post-menopausal women. J Sports Med Phys Fitness. 2010;50(2):196–201. [PubMed] [Google Scholar]
- 5.Van Proeyen K, Szlufcik K, Nielens H, et al. Training in the fasted state improves glucose tolerance during fat-rich diet. J Physiol. 2010;588:4289–302. doi: 10.1113/jphysiol.2010.196493. Pt 21. doi: 10.1113/jphysiol.2010.196493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ridker PM, Cook NR, Lee IM, et al. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med. 2005;352(13):1293–304. doi: 10.1056/NEJMoa050613. [DOI] [PubMed] [Google Scholar]
- 7.Choi L, Liu Z, Matthews CE, Buchowski MS. Validation of accelerometer wear and nonwear time classification algorithm. Med Sci Sports Exerc. 2011;43(2):357–64. doi: 10.1249/MSS.0b013e3181ed61a3. doi: 10.1249/MSS.0b013e3181ed61a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shiroma EJ, Freedson PS, Trost SG, Lee IM. Patterns of accelerometer-assessed sedentary behavior in older women. JAMA. 2013;310(23):2562–3. doi: 10.1001/jama.2013.278896. doi: 10.1001/jama.2013.278896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tudor-Locke C, Camhi SM, Troiano RP. A catalog of rules, variables, and definitions applied to accelerometer data in the National Health and Nutrition Examination Survey, 2003 – 2006. Prev. Chronic Dis. 2012;9:E113. doi: 10.5888/pcd9.110332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bassett DR, Troiano RP, McClain JJ, Wolff DL. Accelerometer-based physical activity: total volume per day and standardized measures. Med Sci Sports Exerc. 2015;47(4):833–8. doi: 10.1249/MSS.0000000000000468. doi: 10.1249/MSS.0000000000000468. [DOI] [PubMed] [Google Scholar]
- 11.Reid KJ, Santostasi G, Baron KG, et al. Timing and intensity of light correlate with body weight in adults. PloS One. 2014;9(4):e92251. doi: 10.1371/journal.pone.0092251. doi: 10.1371/journal.pone.0092251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McFadden E, Jones ME, Schoemaker MJ, Ashworth A, Swerdlow AJ. The relationship between obesity and exposure to light at night: cross-sectional analyses of over 100,000 women in the breakthrough generations study. Am J Epidemiol. 2014;180(3):245–50. doi: 10.1093/aje/kwu117. doi: 10.1093/aje/kwu117. [DOI] [PubMed] [Google Scholar]
- 13.Panossian LA, Veasey SC. Daytime sleepiness in obesity: mechanisms beyond obesity: mechanisms beyond sleep apnea—a review. Sleep. 2012;35(5):605–15. doi: 10.5665/sleep.1812. doi: 10.5665/sleep.1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rimm EB, Stampfer MJ, Colditz GA, et al. Validity of self-reported waist and hip circumferences in men and women. Epidemiology. 1990;1(6):466–73. doi: 10.1097/00001648-199011000-00009. [DOI] [PubMed] [Google Scholar]