Abstract
Rationale: Recent reports of progressive massive fibrosis and rapidly progressive pneumoconiosis in U.S. coal miners have raised concerns about excessive exposures to coal mine dust, despite reports of declining dust levels.
Objectives: To evaluate the histologic abnormalities and retained dust particles in available coal miner lung pathology specimens, and to compare these findings with those derived from corresponding chest radiographs.
Methods: Miners with severe disease and available lung tissue were identified through investigator outreach. Demographic as well as smoking and work history information was obtained. Chest radiographs were interpreted according to the International Labor Organization classification scheme to determine if criteria for rapidly progressive pneumoconiosis were confirmed. Pathology slides were scored by three expert pulmonary pathologists using a standardized nomenclature and scoring system.
Measurements and Main Results: Thirteen cases were reviewed, many of which had features of accelerated silicosis and mixed dust lesions. Twelve had progressive massive fibrosis, and 11 had silicosis. Only four had classic lesions of simple coal workers’ pneumoconiosis. Four had diffuse interstitial fibrosis with chronic inflammation, and two had focal alveolar proteinosis. Polarized light microscopy revealed large amounts of birefringent mineral dust particles consistent with silica and silicates; carbonaceous coal dust was less prominent. On the basis of chest imaging studies, specimens with features of silicosis were significantly associated (P = 0.047) with rounded (type p, q, or r) opacities, whereas grade 3 interstitial fibrosis was associated (P = 0.02) with the presence of irregular (type s, t, or u) opacities.
Conclusions: Our findings suggest that rapidly progressive pneumoconiosis in these miners was associated with exposure to coal mine dust containing high concentrations of respirable silica and silicates.
Keywords: anthracosis, coal mining, pneumoconiosis, pathology, silicosis
At a Glance Commentary
Scientific Knowledge on the Subject
There have been a number of reports of resurgent progressive massive fibrosis and rapidly progressive pneumoconiosis (RPP) in U.S. coal miners. The causes of this disease are not well understood. There have been no studies performed in which researchers evaluated the pathology underlying this severe and aggressive form of the disease; there are only reports of radiographic findings. Based on chest radiographs of miners from certain geographic regions with a high prevalence of RPP, these reports have shown a rising proportion of r-type pneumoconiotic opacities, suggesting increasing exposure to silica and silicates. However, this has not been confirmed pathologically.
What This Study Adds to the Field
To our knowledge, this study is the first in which lung pathology specimens were obtained from U.S. coal miners with RPP. Three expert occupational pulmonary pathologists systematically evaluated the lung pathology, patterns of inflammation, fibrosis, and retained mineral particles and compared findings with those from corresponding chest radiographs. We found that the lung pathology observed in these well-characterized cases of RPP in U.S. coal miners had features of accelerated silicosis, mixed dust pneumoconiosis, and progressive massive fibrosis. Our findings suggest that exposures to respirable silica and silicate minerals play an important role in the pathogenesis of RPP. This evidence is consistent with prior reports of radiologic patterns associated with heavy exposure to silica. Prevention of this disease likely requires more stringent efforts to monitor and control exposure to coal mine dust that may contain high quantities of respirable silica.
After passage of the Federal Coal Mine Health and Safety Act of 1969 (1), measures were adopted to limit exposure to respirable dust in U.S. coal mines, along with active surveillance of miners’ lung health based on work history, chest radiographs, and spirometry. These activities were temporally associated with a steady decline, from 1970 until about 2000, in the prevalence of coal workers’ pneumoconiosis (CWP) among participants in the Coal Workers Health Surveillance Program, which is administered by the National Institute for Occupational Safety and Health. Since that time, however, the proportion of miners with pneumoconiosis—defined as a chest radiograph showing International Labor Organization (ILO) (2) category 1/0 or greater profusion of small opacities—has increased significantly (3). Alarmingly, recent reports have described rapidly progressive, severe, and fatal forms of disease, including progressive massive fibrosis (PMF) (4–6) and rapidly progressive pneumoconiosis (RPP) (7). In some locations, the prevalence of PMF is now the same as that observed in 1970, just after ratification of the federal law (8). Severe disease is occurring in younger coal miners and in certain geographic regions that are so-called hot spots. Surveillance chest radiographs of miners in these regions show an increasing proportion of r-type pneumoconiotic opacities, suggesting greater exposure to silica and silicates (9). To our knowledge, the present study is the first to describe the lung pathology and patterns of inflammation, fibrosis, and retained mineral particles in biopsies of contemporary miners with severe pneumoconiosis.
An abstract describing this study was presented at the American Thoracic Society 2014 International Conference (10).
Methods
Study Population and Procedures
We identified miners who had both radiologic evidence of RPP and available lung tissue obtained by lung biopsy, lung resection, or autopsy. RPP was defined using a 12-point scale based on ILO profusion scores. With the use of this scale, the difference in the profusion score between the most recent radiograph and the prior radiograph is divided by one-fifth of the time difference in years between radiographs. This value must be greater than 1 (one ILO subcategory increase in profusion in less than 5 yr) to be rapidly progressive. If evidence of PMF has been documented (category A, B, or C) on any radiograph taken when the miner is younger than 70 years of age or has a coal-mining tenure shorter than 40 years, this is also presumed to represent RPP (7). We collected available specimens through outreach to the West Virginia Occupational Pneumoconiosis Board, the U.S. Health Resources and Services Administration Black Lung Clinics Program, and miners’ attorneys. The study protocol received institutional review board approval, and written informed consent was obtained in all cases. Miners (or the next of kin for miners who were deceased) completed a standardized questionnaire about demographic, smoking, and occupational histories. Chest radiographs were obtained and categorized by a senior investigator (E.L.P.) using the ILO classification scheme (2) to verify that the miner met the criteria for RPP. The B reader was blinded to the histologic findings derived from each miner’s lung sample. For one miner, only a portable chest radiograph was available. Slides of formalin-fixed, paraffin-embedded lung tissue sections were obtained, anonymized, and sent to three expert occupational pulmonary pathologists (A.C., J.L.A., and F.H.Y.G.), who were blinded to the case histories.
Histologic Definitions and Pathologic Scoring
Lung lesions were classified according to published standards (11). Macules were defined as a collection of dust-laden macrophages around a terminal bronchovascular bundle with mild reticulin fibrosis and small amounts of collagen. Macules were usually, but not always, surrounded by a halo of centriacinar (focal) emphysema. Coal dust macules were differentiated from mixed dust macules by a preponderance of dust particles consistent with coal.
Coal dust nodules were defined as lesions larger and more fibrotic than macules (usually >4 mm) containing coal mine dust. Collagen in these nodules had a haphazard arrangement of fibers (11). These nodules were not confined to the terminal bronchiolar region but were found throughout the parenchyma, including the interlobular septa, subpleural locations, and connective tissues of bronchovascular bundles (11).
Classic silicosis was characterized by the presence of lightly pigmented nodules with smooth borders and a central area of laminated, whorled collagen (fibrosis) (12). The silicotic lesions in these coal miners had a central core of whorled collagen along with a peripheral stellate component where there was greater deposition of coal and mineral dust particles.
Parenchymal mixed dust lesions contained more collagen and mineral dust, and less coal dust, than classic coal dust macules or nodules. The collagen did not show central whorling typical of silicotic nodules (13). Classic silicotic nodules were also present in most cases.
PMF was defined as a coal dust–pigmented fibrotic lesion with irregular or whorled deposition of collagen fibers, with or without areas of necrosis, measuring 1 cm or more in diameter. This size criterion was based on the definition in the Federal Coal Mine Health and Safety Act of 1969 (1).
Biopsies were graded using a previously published histopathologic scoring system for CWP (14) with slight modification. The grade was based on both the size and extent of the lesions on a scale of 0–3. Interstitial fibrosis, as described by McConnochie and colleagues (15), was also graded on a scale of 0–3, corresponding to absent, mild, moderate, or severe, respectively.
Dust present in the specimens was evaluated by incident and polarized light and the relative quantities of coal and mineral dust within the lungs, recorded on a scale of 1–3. Bituminous coal dust is golden brown, angular, translucent, and distinguishable from the opaque, rounded combustion products derived from sources such as cigarette smoke, burning of biomass, and diesel emissions. Bright, birefringent, and elongated or platy particles were classified as silicates; dull birefringent particles were classified as silica (16).
After independent review and grading, the three pathologists met in a consensus conference to resolve differences in pathologic classification. The predominant disease was determined on the basis of relative proportions of coal macules, coal nodules, silicotic nodules, mixed dust lesions, and interstitial fibrosis. We classified each miner’s lung tissue with a predominant disease type on the basis of the profusion scores for mixed dust, silicosis, CWP, and interstitial fibrosis. The pathology was classified as “mixed dust” when mixed dust lesions had a higher score than other lesions, as “silicosis” when silica nodules had a higher score than other lesions, and as “mixed dust/silicosis” when the scores were equal. Cases were classified as “nonspecific interstitial lung disease” when pulmonary fibrosis was the predominant lesion. PMF was characterized as either present or absent, without reference to radiographic findings.
Statistical Analysis
We used SAS software (version 9.4; SAS Institute, Cary, NC) for all statistical analyses. The pathologic classifications used in statistical analyses were based on consensus results. The significance of the association between radiographic opacity type and pathologic findings was examined using Fisher’s exact test. A P value less than 0.05 was considered significant.
Results
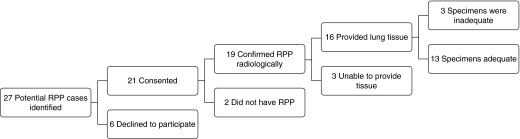
Twenty-seven miners with probable RPP and potentially available lung tissue were identified through investigator outreach (see Figure 1). Twenty-one of these miners or their family members provided informed consent. After expert review, 19 of the 21 miners’ radiographs met the criteria for RPP. Eighteen of these miners also met radiographic criteria for PMF, with at least one opacity greater than or equal to 1 cm in diameter (2). Figure 2 shows typical serial radiographs of one West Virginia miner for whom autopsy tissue was available. Of the 19 miners who met the criteria for RPP, 17 were from West Virginia, 1 was from Pennsylvania, and 1 was from Kentucky. The longest-held jobs were in underground coal mining for 17, including 12 who operated continuous mining machines and 5 who operated roof bolters. The remaining two were surface miners.
Figure 1.
Flow diagram of study participants. RPP = rapidly progressive pneumoconiosis.
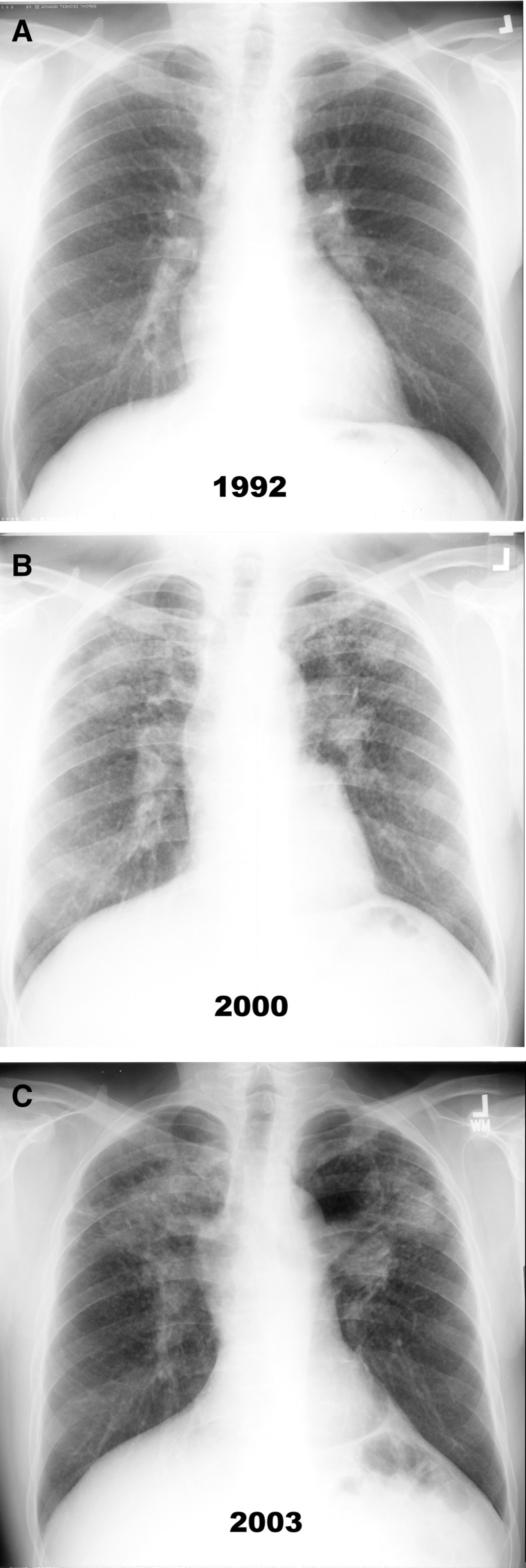
Figure 2.
Posteroanterior radiographs of a coal miner with rapidly progressive pneumoconiosis who underwent a bilateral lung transplant at age 60 years (see pathology in Figure 3). He had 35 years of coal-mining experience, of which 28 years were at the face of the mine, and no history of smoking. (A) Chest radiograph obtained after 24 years of coal mine employment showing category 3 simple pneumoconiosis with q- and r-type opacities. (B and C) Chest radiographs obtained after 32 and 35 years of coal-mining employment, respectively. Multiple, large, mass-like lesions and nodules in the bilateral upper lung fields, which coalesce further and enlarge as time progresses, are shown.
For the 19 miners with radiographic findings of RPP, we were able to obtain 16 lung tissue specimens for analysis. Six of these were surgical lung biopsies. The indications for surgical biopsy were given as “rule out malignancy” in five cases and “nodules with fever and weight loss” in the remaining case. Five specimens were lung explants following lung transplants, two were from autopsies, two were from needle core biopsies, and one was from a transbronchial biopsy. Three of the specimens were of poor quality or had insufficient tissue and were not suitable for classification, leaving 13 cases for complete pathologic evaluation. The demographics of these 13 miners are shown in Table 1.
Table 1.
Demographics of Miners with Evaluable Pathology Specimens
| Mean ± SD, n (%), or Median (IQR)* | Range | |
|---|---|---|
| Age at first exposure, yr | 21.3 ± 2.0 | 18–24 |
| Time between biopsy and CXR, yr | 2.7 ± 2.7 | 0.1–7.4 |
| Work history | ||
| Mining tenure, yr | 32 (26.5–35) | 10–39 |
| Mining face worker | 8 (62) | |
| Roof bolter at face | 4 (31) | |
| Surface worker | 1 (8) | |
| Smoking history | ||
| Ever smoker | 9 (69) | |
| Ever smoker, pack-years | 14.2 (1.4–22.5) | 0.6–50 |
Definition of abbreviations: CXR = chest radiograph; IQR = interquartile range.
Data are presented for a total of 13 miners with evaluable pathology specimens.
The radiographic findings based on these 13 cases are shown in Table 2. Chest imaging revealed that all but one miner had PMF, with large opacity sizes ranging from categories A through C. Category O indicates that no large opacities are visible; category A refers to opacities with long-axis diameters that are greater than 1 cm and less than or equal to 5 cm; category B indicates opacities greater than 5 cm up to the area of the right upper lung zone; and category C indicates opacities with an area greater than that of the right upper lung zone. Small opacities are recorded as ILO types p, q, r, s, t, and u. Small, rounded opacities (types p, q, and r) have diameters less than or equal to 1.5 mm, greater than 1.5 and less than or equal to 3 mm, and greater than 3 mm and less than or equal to 10 mm, respectively; irregular opacities (types s, t, and u) have short-axis diameters less than or equal to 1.5 mm, greater than 1.5 and less than or equal to 3 mm, and greater than 3 mm and less than or equal to 10 mm, respectively.
Table 2.
International Labor Organization Chest Radiography–based Classification of Most Recent Available Chest Radiographs among Miners with Rapidly Progressive Pneumoconiosis and Evaluable Lung Tissue
| Miner | Small-Opacity Profusion | Predominant Small-Opacity Shape/Size | Opacity Shape | Large-Opacity Category |
|---|---|---|---|---|
| 1 | N/A* | t/t | Irregular | C |
| 2 | 2/2 | r/r | Round | B |
| 3 | 1/0 | s/t | Irregular | C |
| 4 | 2/3 | q/q | Round | C |
| 5 | 1/2 | r/r | Round | B |
| 6 | 1/1 | s/t | Irregular | C |
| 7 | 2/2 | q/r | Round | C |
| 8 | 3/2 | q/r | Round | A |
| 9 | 1/1 | p/p | Round | C |
| 10 | 2/1 | q/q | Round | B |
| 11 | 2/2 | s/t | Irregular | C |
| 12 | 3/3 | s/t | Irregular | A |
| 13 | 2/3 | s/t | Irregular | O |
Definition of abbreviation: N/A = not applicable.
N = 13.
The only plain image available for this miner was a portable chest radiograph, making it impossible to evaluate profusion. The size and shape of opacities were determined on the basis of that image as well as a computed tomographic scan. The radiograph clearly demonstrated category C progressive massive fibrosis.
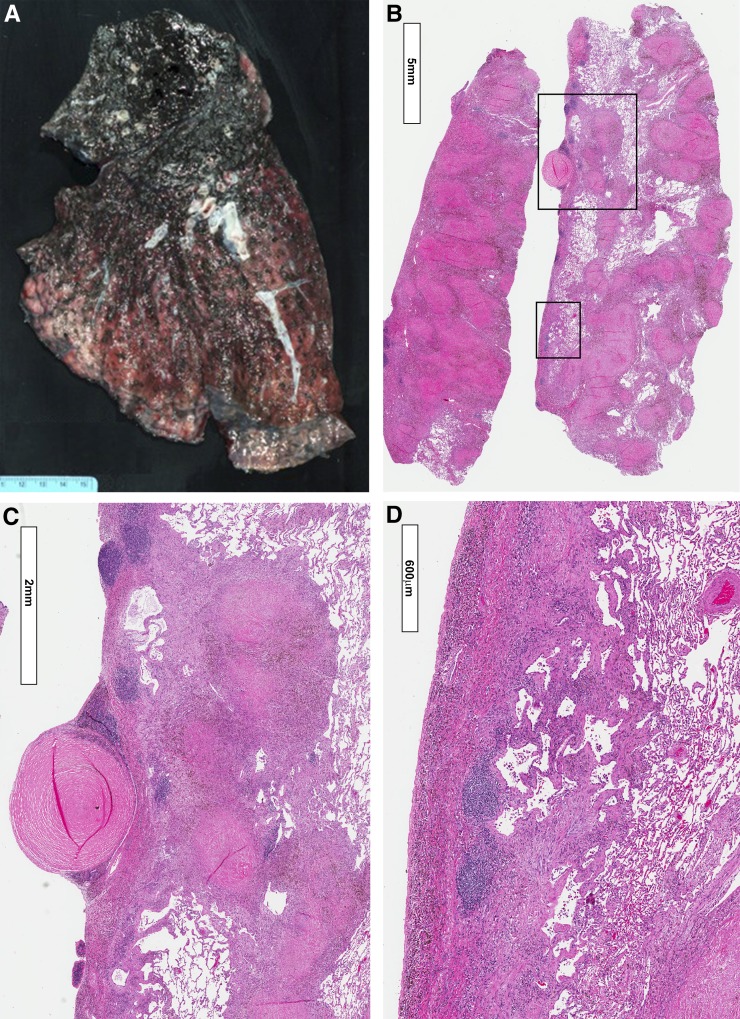
The expert pathology panel graded the profusion of coal dust macules and nodules, mixed dust lesions, and silicotic nodules present in each specimen (Table 3 and Figure 3; see also Figures E1 and E2 in the online supplement). Only 4 of 13 cases demonstrated classic lesions of CWP. Mixed dust pneumoconiosis was seen in 11 of the 13 cases (Figure E2). Silicotic lesions were also seen in 11 of 13 cases. Notably, two cases showed focal alveolar proteinosis (see Figure E1B), together with interstitial inflammation and silicotic nodules showing varying degrees of maturity, features consistent with accelerated silicosis (17). One of these miners had only 10 years of exposure as a surface worker, while the other had worked for 37 years as a roof bolter. Despite the variability in specimen size, PMF lesions were identified in 10 of the 13 specimens. Interstitial pulmonary fibrosis was noted in 11 cases, with moderate to severe disease (grades 2 and 3) found in four cases (Figures 3D, E3B, and E3C). Interstitial fibrosis was the predominant lesion in two miners (Figure E4). One was a roof bolter who had silica and silicates present at grade 1. The other was a face worker with coal, silica, and silicate particles. Silica and silicate particles in his specimens were found at grade 1. Patchy areas of emphysema were found in two miners, only one of whom was a smoker. Both miners had 35 years of coal mine dust exposure at the face. Emphysema was not a prominent histologic finding in the other cases.
Table 3.
Summary of Pathologic Classification of Miners with Rapidly Progressive Pneumoconiosis
| Miner | Source of Specimen | CWP* | Mixed Dust* | Silicosis† | PMF Present | Interstitial Fibrosis Grade | Predominant Disease Type |
|---|---|---|---|---|---|---|---|
| 1 | Explant | 0 | 3 | 2 | Yes | 2 | MD |
| 2 | Autopsy | 0 | 3 | 2 | Yes | 1 | MD |
| 3 | Autopsy | 0 | 3 | 2 | Yes | 3 | MD |
| 4* | Biopsy | 0 | 3 | 1 | No | 1 | MD |
| 5* | Biopsy | 0 | 3 | 3 | Yes | 1 | MD/silicosis‡ |
| 6 | Explant | 3 | 2 | 2 | Yes | 1 | MD/silicosis |
| 7* | Explant | 1 | 3 | 3 | Yes | 1 | MD/silicosis |
| 8* | Biopsy | 0 | 3 | 3 | Yes | 1 | MD/silicosis |
| 9 | Biopsy | 1 | 1 | 3 | Yes | 1 | Silicosis |
| 10* | Biopsy | 0 | 2 | 3 | Yes | 0 | Silicosis‡ |
| 11 | Biopsy | 3 | 1 | 1 | Yes | 0 | CWP |
| 12 | Explant | 0 | 0 | 0 | No | 3 | Nonspecific ILD |
| 13* | Explant | 0 | 0 | 0 | No | 3 | Nonspecific ILD |
| Total cases | 4 | 11 | 11 | 10 |
Definition of abbreviations: CWP = coal workers’ pneumoconiosis; ILD = interstitial lung disease; MD = mixed dust pneumoconiosis; PMF = progressive massive fibrosis.
Profusion category is given for each lesion type (range, 0–3). N = 13.
Sum of profusion scores for CWP and MD of macules and nodules. Maximum possible profusion score is 3.
Sum of profusion scores of silicotic nodules. Maximum possible profusion score is 3.
Features of alveolar proteinosis present.
Figure 3.
Explanted left lung from the miner whose radiographs are shown in Figure 2. (A) Photograph of the lung explant. The upper lobe is completely replaced by progressive massive fibrosis (PMF). Pale nodular areas can be seen within the PMF, indicative of silicosis. The apical segment of the lower lobe is also involved with PMF. Elsewhere the lung shows nodular lesions of pneumoconiosis. (B) Low-magnification view of section from area of PMF (left) and area involved with simple coal workers’ pneumoconiosis (right). Both areas show predominantly silicotic lesions. (C) Close-up of upper boxed area shown in B. A silicotic nodule can be seen on the pleural surface (pleural pearl), together with subpleural, semiconfluent, silicotic nodules. There is a marked lymphoid reaction in the pleura. (D) Close-up of lower boxed area in B showing pleural fibrosis with shallow underlying interstitial fibrosis as well as lymphoid aggregates.
We found that all four cases with the histologic finding of moderate to severe interstitial fibrosis of grade 2 or above had irregular opacities (ILO type s, t, or u opacities) classified independently on the basis of chest imaging, whereas only two other cases in the series had this finding (P = 0.02). In contrast, the six cases (cases 5 through 10) with predominant features of silicosis or mixed dust with silicosis were significantly associated (P = 0.047) with rounded opacities on chest imaging (p-, q-, or r-shaped opacities) compared with the three cases (cases 11–13) with CWP or predominant interstitial fibrosis. Cases with predominantly mixed dust lesions and few features of silicosis demonstrated both rounded and irregular radiographic opacities.
We found areas of usual interstitial pneumonia–like interstitial fibrosis in several specimens (Figure E3). A number of cases also showed prominent histiocytic and lymphocytic interstitial inflammatory responses (Figure E2). We found no evidence of neoplasia, granulomas, mycobacterial and/or fungal infection, or other specific lung diseases in any of the lung tissues reviewed.
A consensus score for the density of specific particles was provided for each lung tissue specimen. Coal particles were observed above background levels (grades 1–3) in 10 of 13 samples. Carbonaceous combustion particles were not observed above background in any specimen. In 11 of 13 cases, dull birefringent particles consistent with crystalline silica were observed above background. Bright birefringent particles consistent with silicates were observed above background levels in 10 of 13 cases (Figures E1E and E3F). Occasional ferruginous bodies were identified, but no asbestos bodies were seen. Among all 13 cases, there was no significant association by multinomial regression between the type and density of particles and the predominant pathologic lesion or the shape of opacities visualized by chest radiography in this small sample.
Discussion
Over the past two decades, public health professionals have been troubled by the emergence of a rapidly progressive form of pneumoconiosis observed in some U.S. coal miners, which is associated with significant respiratory compromise, premature death, and years of potential life lost (18, 19). This severe lung disease is distinguished by geographic clustering in central and eastern Kentucky, southwestern Virginia, and southern West Virginia and by its occurrence in younger miners (4, 6). Although most common in underground miners, PMF and rapidly progressive disease in surface coal miners have been described in several reports (20, 21). Moreover, an increase in the prevalence of ILO r-type chest radiographic opacities has been described in miners from these regions, implicating overexposure to respirable silica as a possible risk factor (9). Despite the importance of these findings and their implications for workplace exposure control, little information on the histology of RPP was previously available.
Our study shows an unusual spectrum of lung histologic findings in 13 coal miners with RPP meeting a stringent case definition based on serial chest imaging. The predominant pathologic findings were those of accelerated silicosis, mixed dust pneumoconiosis, and PMF. We use the term accelerated silicosis in cases where the pathology showed some features of acute silicosis, such as small foci of lipoproteinosis as well as immature silicotic nodules. The silicotic nodules of accelerated silicosis were usually smaller than the classic silicotic nodules seen in chronic silicosis and contained abundant histiocytes together with immature collagen (22). Accelerated and acute silicosis may overlap.
Classic lesions of simple CWP were present in some of the 13 cases, but they were not prominent. Four cases had interstitial fibrosis, including several with features resembling usual interstitial pneumonia, suggesting that the lung’s response to injury caused by inhaled coal mine dust may be quite variable. This pattern has been described previously in coal miners (15) and may be misclassified as idiopathic in circumstances where an inadequate occupational history has been obtained.
Findings of alveolar proteinosis, intense interstitial histiocytic and lymphocytic inflammation, and large amounts of weakly and strongly birefringent particles consistent with silicates and silica are histologic findings that support the link between RPP and exposure to high concentrations of mineral dust. By contrast, deposits of carbonaceous dust were less prominent than described in classic CWP (14).
Historically, both total cumulative dust exposure and silica fraction are critical factors contributing to the severity of CWP and the appearance of classic silicotic nodules. Autopsy studies have shown that the classic whorling of collagen in a silicotic nodule occurs when the proportion of silica (quartz) in the lung mineral dust is approximately 20% or greater (23). Overexposure to silica has been shown to be a significant risk factor for the rapid progression of radiographic disease (24), similar to that observed in the miners in our study.
We found a significant association between the predominant pathologic lesion of silicosis and round opacities on chest imaging. We found a similar link between interstitial fibrosis and radiographic irregular opacities. Previous studies have demonstrated correlations between radiologic and pathologic patterns in coal miners, including r-sized opacities associated with silicosis and irregular opacities (often more prominent in middle and lower lung zones) as under recognized manifestations of coal mine dust lung disease (25).
These findings suggest that exposures to respirable silica and silicate minerals play an important role in the pathogenesis of RPP. They also corroborate ecologic observations of lower average seam heights in RPP hot-spot regions (26). Mining of thin coal seams has been associated with greater silica exposure because more rock must be cut above and below the seam to deploy mining equipment (27). Improvements in processing techniques have made this type of mining more profitable because modern preparation plants can more easily separate coal from large amounts of waste rock than in the past (28). These technological changes, while increasing efficiency of mining operations, may be associated with a risk of a more virulent form of coal mine dust lung disease. The implication of silica and silicate minerals as culprits in this disease parallels the resurgence of silicosis globally (29) and in industries other than mining, including stone countertops (30) and sandblasting of textiles (31). Exposures in the rapidly expanding hydraulic fracturing industry may portend additional cases of this preventable disease (32).
Given the small sample size, it was not possible to fully model the relationship between job title and RPP; however, we did see an overrepresentation in our case series of those job categories considered to pose a high risk for exposure. Data from a representative national survey of coal mine employees (33) performed in 2008, the median year in which tissue was obtained from the miners in our study, gives some context. Overall, our sample had a higher proportion of face production workers. The principal job of 4 of the 13 (31%) study miners was operating an underground roof-bolting machine, more than double (14%) the proportion of roof bolters in the general population of U.S. coal production workers. Similarly, 8 (62%) of 13 miners in this study operated mining machines, while the national estimate was about 13%. One study miner (8%) worked in production at a surface coal mine; for this activity, the national estimate was 24%. The study miners had a median age of 56 years at the time of the biopsy or autopsy, which, as might be expected, was older than the average active coal mine worker, who is about 44 years old. On the basis of the consistent patterns of lung histologic abnormalities in even this small case series, we believe that our findings are likely representative of the larger population of affected miners. Future efforts to systematically collect lung tissue samples from all miners affected by RPP in studies designed to verify these observations will be important.
Our study has a number of limitations. We did not recruit from all states where cases of RPP have been reported, nor did we have access to complete occupational histories in the miners whose lung tissue was examined. There may be variability in lung mineral dust content based on geographical location of employment that is not reflected in our case series. Another limitation is the lack of access to chest high-resolution computed tomographic imaging for most of the miners whose lung tissue was examined. While serial chest radiographs allowed us to verify the presence of RPP, chest high-resolution computed tomography would have enabled a more comprehensive correlation between the pathologic findings we describe and relevant clinical imaging findings.
We found a large burden of mineral dust particles in the lung specimens of these miners, with morphologic qualities of birefringence and hue that are classic for silica and silicates; however, our study was limited by a lack of information linking these morphologic qualities with quantitative or qualitative elemental or mineralogic content. Future in-depth analysis of lung mineralogy would be of great interest, including bulk characterization for carbon, mineral, and metal content as well as in situ microanalysis, to determine the relationship between dust composition and specific pathologic features.
Conclusions
We found that the lung pathology observed in 13 well-characterized cases of RPP in U.S. coal miners had features of accelerated silicosis, mixed dust pneumoconiosis, and PMF. Prevention of this disease likely requires more stringent efforts to monitor and control exposure to coal mine dust that may contain high concentrations of respirable silica.
Acknowledgments
Acknowledgment
The authors thank Drs. Kirtee Raparia and Anjana Yeldandi of the Northwestern Memorial Hospital Department of Pathology for their assistance in organizing and participating in the consensus conference; Dr. Judith Graber for assistance in reviewing materials and gathering data; Dr. Leonard Go for his review of the manuscript; Andrea Chiu for assistance with the photomicrographs; and Sheon MacNeil, R.N., who provided indispensable administrative support for this work.
Footnotes
This study was supported by the National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention (contract 214-2011-M-40852). This work was also supported by the National Institute of General Medical Sciences of the National Institutes of Health under award U54GM104942 (M.R.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute for Occupational Safety and Health or the National Institutes of Health.
Author Contributions: R.A.C. had full access to all of the data in the study; takes responsibility for the integrity of the data and the accuracy of the data analysis as well as the content of the manuscript; and contributed to study design, data analysis, and manuscript preparation and revision. E.L.P. conceived the study and contributed to study design, data analysis, and manuscript preparation and revision. C.R., M.R., A.N., and B.Y. contributed to data analysis and manuscript preparation and revision. J.L.A., A.C., and F.H.Y.G. performed pathology review and contributed to study design, data analysis, and manuscript preparation and revision.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org
Originally Published in Press as DOI: 10.1164/rccm.201505-1014OC on October 29, 2015
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1. Federal Coal Mine Health and Safety Act of 1969, Public Law 91-173, 30 U.S.C. ch. 22, §§ 801 et seq.
- 2.International Labour Office. Geneva, Switzerland: International Labour Office; 2002. Guidelines for the use of the ILO international classification of radiographs of pneumoconioses. [Google Scholar]
- 3.National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention. Work-related lung disease (WoRLD) surveillance report [updated 2008 Jun 23; accessed 2015 Nov 11]. Available from: http://www2a.cdc.gov/drds/worldreportdata/tocArchive.asp.
- 4.Antao V, Petsonk EL, Attfield MD Centers for Disease Control and Prevention (CDC) Advanced cases of coal workers’ pneumoconiosis—two counties, Virginia, 2006. MMWR Morb Mortal Wkly Rep. 2006;55:909–913. [PubMed] [Google Scholar]
- 5.Wade WA, Petsonk EL, Young B, Mogri I. Severe occupational pneumoconiosis among West Virginian coal miners: one hundred thirty-eight cases of progressive massive fibrosis compensated between 2000 and 2009. Chest. 2011;139:1458–1462. doi: 10.1378/chest.10-1326. [DOI] [PubMed] [Google Scholar]
- 6.Attfield MD, Petsonk EL Centers for Disease Control and Prevention (CDC) Advanced pneumoconiosis among working underground coal miners—Eastern Kentucky and Southwestern Virginia, 2006. MMWR Morb Mortal Wkly Rep. 2007;56:652–655. [PubMed] [Google Scholar]
- 7.Antao VC, Petsonk EL, Sokolow LZ, Wolfe AL, Pinheiro GA, Hale JM, Attfield MD. Rapidly progressive coal workers’ pneumoconiosis in the United States: geographic clustering and other factors. Occup Environ Med. 2005;62:670–674. doi: 10.1136/oem.2004.019679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blackley DJ, Halldin CN, Laney AS. Resurgence of a debilitating and entirely preventable respiratory disease among working coal miners. Am J Respir Crit Care Med. 2014;190:708–709. doi: 10.1164/rccm.201407-1286LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laney AS, Petsonk EL, Attfield MD. Pneumoconiosis among underground bituminous coal miners in the United States: is silicosis becoming more frequent? Occup Environ Med. 2010;67:652–656. doi: 10.1136/oem.2009.047126. [DOI] [PubMed] [Google Scholar]
- 10.Najmuddin A, Cohen RA, Petsonk EL, Young B, MacNeill S, Tramma S, Regier M, Abraham JL, Churg A, Green F. Lung pathology in coal workers with rapidly progressive pneumoconiosis emphasizes importance of silica and silicates in addition to carbon [abstract] Am J Respir Crit Care Med. 2014;189:A5218. doi: 10.1164/rccm.201505-1014OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kleinerman J, Green FHY, Harley R, Lapp NL, Lacquer W, Naeye RL, Taylor G, Wiot J, Wyatt J. Pathology standards for coal workers’ pneumoconiosis: report of the Pneumoconiosis Committee of the College of American Pathologists to the National Institute for Occupational Safety and Health. Arch Pathol Lab Med. 1979;103:375–432. [PubMed] [Google Scholar]
- 12.Craighead J, Kleinerman J, Abraham JL, Gibbs AR, Green FHY, Harley RA, Ruettner JR, Vallyathan V, Juliano EB Silicosis and Silicate Disease Committee. Diseases associated with exposure to silica and nonfibrous silicate minerals. Arch Pathol Lab Med. 1988;112:673–720. [PubMed] [Google Scholar]
- 13.Honma K, Abraham JL, Chiyotani K, De Vuyst P, Dumortier P, Gibbs AR, Green FHY, Hosoda Y, Iwai K, Williams WJ, et al. Proposed criteria for mixed-dust pneumoconiosis: definition, descriptions, and guidelines for pathologic diagnosis and clinical correlation. Hum Pathol. 2004;35:1515–1523. doi: 10.1016/j.humpath.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 14.Vallyathan V, Landsittel DP, Petsonk EL, Kahn J, Parker JE, Osiowy KT, Green FHY. The influence of dust standards on the prevalence and severity of coal worker’s pneumoconiosis at autopsy in the United States of America. Arch Pathol Lab Med. 2011;135:1550–1556. doi: 10.5858/arpa.2010-0393-OA. [DOI] [PubMed] [Google Scholar]
- 15.McConnochie K, Green FHY, Vallyathan V, Wagner JC, Seal RME, Lyons JP. Interstitial fibrosis in coal workers—experience in Wales and West Virginia. Ann Occup Hyg. 1988;32(inhaled particles VI):553–560. [Google Scholar]
- 16.McDonald JW, Roggli VL. Detection of silica particles in lung tissue by polarizing light microscopy. Arch Pathol Lab Med. 1995;119:242–246. [PubMed] [Google Scholar]
- 17.Hutyrová B, Smolková P, Nakládalová M, Tichý T, Kolek V. Case of accelerated silicosis in a sandblaster. Ind Health. 2015;53:178–183. doi: 10.2486/indhealth.2013-0032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pon MRL, Roper RA, Petsonk EL, Wang ML, Castellan RM, Attfield MD, Wagner GR Centers for Disease Control and Prevention (CDC) Pneumoconiosis prevalence among working coal miners examined in federal chest radiograph surveillance programs—United States, 1996–2002. MMWR Morb Mortal Wkly Rep. 2003;52:336–340. [PubMed] [Google Scholar]
- 19.Petsonk EL, Rose C, Cohen R. Coal mine dust lung disease: new lessons from old exposure. Am J Respir Crit Care Med. 2013;187:1178–1185. doi: 10.1164/rccm.201301-0042CI. [DOI] [PubMed] [Google Scholar]
- 20.Halldin CN, Reed WR, Joy GJ, Colinet JF, Rider JP, Petsonk EL, Abraham JL, Wolfe AL, Storey E, Laney AS. Debilitating lung disease among surface coal miners with no underground mining tenure. J Occup Environ Med. 2015;57:62–67. doi: 10.1097/JOM.0000000000000302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Laney AS, Wolfe AL, Petsonk EL, Halldin CN Centers for Disease Control and Prevention (CDC) Pneumoconiosis and advanced occupational lung disease among surface coal miners—16 states, 2010–2011. MMWR Morb Mortal Wkly Rep. 2012;61:431–434. [PubMed] [Google Scholar]
- 22.Abraham JL, Wiesenfeld SL. Two cases of fatal PMF in an ongoing epidemic of accelerated silicosis in oilfield sandblasters: lung pathology and mineralogy. Ann Occup Hyg. 1997;41(Suppl 1):440–447. [Google Scholar]
- 23.Ruckley VA, Fernie JM, Chapman JS, Collings P, Davis JM, Douglas AN, Lamb D, Seaton A. Comparison of radiographic appearances with associated pathology and lung dust content in a group of coalworkers. Br J Ind Med. 1984;41:459–467. doi: 10.1136/oem.41.4.459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Buchanan D, Miller BG, Soutar CA. Quantitative relations between exposure to respirable quartz and risk of silicosis. Occup Environ Med. 2003;60:159–164. doi: 10.1136/oem.60.3.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vallyathan V, Brower PS, Green FH, Attfield MD. Radiographic and pathologic correlation of coal workers’ pneumoconiosis. Am J Respir Crit Care Med. 1996;154:741–748. doi: 10.1164/ajrccm.154.3.8810614. [DOI] [PubMed] [Google Scholar]
- 26.Suarthana E, Laney AS, Storey E, Hale JM, Attfield MD. Coal workers’ pneumoconiosis in the United States: regional differences 40 years after implementation of the 1969 Federal Coal Mine Health and Safety Act. Occup Environ Med. 2011;68:908–913. doi: 10.1136/oem.2010.063594. [DOI] [PubMed] [Google Scholar]
- 27.Pollock DE, Potts JD, Joy GJ. Investigation into dust exposures and mining practices in mines in the southern Appalachian region. Min Eng. 2010;62(2):44. [Google Scholar]
- 28.Bethell PJ. Coal preparation: current status and the way ahead. Presentation to the Report Committee of the National Commission on Energy Policy—Coal Study. September 2007, Denver, CO.
- 29.Ehrlich R. A century of miners’ compensation in South Africa. Am J Ind Med. 2012;55:560–569. doi: 10.1002/ajim.22030. [DOI] [PubMed] [Google Scholar]
- 30.Kramer MR, Blanc PD, Fireman E, Amital A, Guber A, Rhahman NA, Shitrit D. Artificial stone silicosis: disease resurgence among artificial stone workers. Chest. 2012;142:419–424. doi: 10.1378/chest.11-1321. [DOI] [PubMed] [Google Scholar]
- 31.Bakan ND, Özkan G, Çamsari G, Gür A, Bayram M, Açikmeşe B, Çetinkaya E. Silicosis in denim sandblasters. Chest. 2011;140:1300–1304. doi: 10.1378/chest.10-1856. [DOI] [PubMed] [Google Scholar]
- 32.Esswein EJ, Breitenstein M, Snawder J, Kiefer M, Sieber WK. Occupational exposures to respirable crystalline silica during hydraulic fracturing. J Occup Environ Hyg. 2013;10:347–356. doi: 10.1080/15459624.2013.788352. [DOI] [PubMed] [Google Scholar]
- 33.McWilliams LJ, Lenart PJ, Lancaster JL, Zeiner JR., Jr National survey of the mining population. Part 1: employees (Information Circular 9527/2012). DHHS (NIOSH) Publication 2012-152. Pittsburgh, PA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, Office of Mine Safety and Health Research; June 2012 [accessed 2015 Nov 11]. Available from: http://www.cdc.gov/niosh/mining/UserFiles/works/pdfs/2012-152.pdf.