Letter to the Editor
Myeloid/lymphoid neoplasms associated with eosinophilia (MLN-eos) and rearrangement of PDGFRA, PDGFRB or FGFR1 are established types of hematologic neoplasms according to the most recent World Health Organization (WHO) classification. Such classification has therapeutic implications because these MLN-eos are driven by chimeric oncoproteins, including targetable receptor or non-receptor tyrosine kinases (TKs).(1)
ETS variant gene 6 (ETV6) maps to chromosome 12p13 and encodes a nuclear protein crucial for hematopoietic regulation. ETV6 is frequently rearranged in hematologic malignancies and can participate in fusion with genes coding for TKs, often resulting in the constitutive activation of the latter.(2) In particular, ETV6 has been found fused to the Fms-like tyrosine kinase 3 (FLT3) gene in several cases of MLN-eos as a result of the t(12;13)(p13;q12) translocation.(3-5) We report a case of indolent ETV6-FLT3-positive MLN-eos successfully treated with the FLT3 inhibitor sorafenib followed by allogeneic stem cell transplantation (SCT).
A 40-year-old woman was admitted to the hospital due to acute viral gastroenteritis. A complete blood count (CBC) performed at that time showed leukocytosis and thrombocytopenia. A second CBC performed after resolution of symptoms showed a white blood cell count (WBC) of 19.7×109/l (neutrophils 58%, lymphocytes 7%, monocytes 16%, eosinophils 12%), hemoglobin 10.7 g/dl, and platelets 112×109/l. A bone marrow (BM) biopsy showed hypercellularity (85%), with no increase in CD34+ blasts and moderate reticulin fibrosis. Conventional cytogenetics showed 46,XX,t(12;13)(p13;q12) in all metaphases. The patient was provisionally assigned a diagnosis of myelofibrosis and referred to our institution for a second opinion.
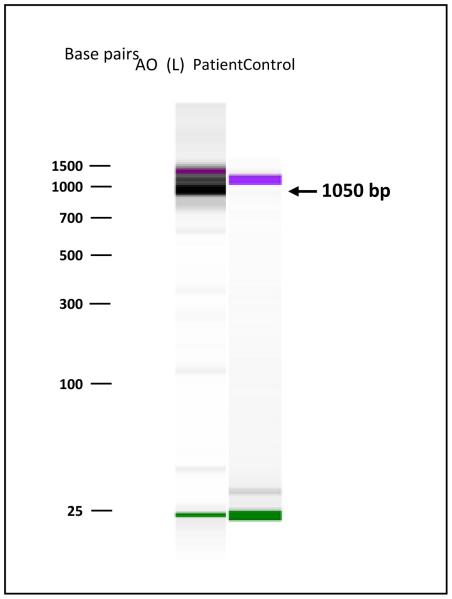
At the time of referral, the patient’s only complaint was mild fatigue. A physical exam was unremarkable and her spleen measured 11.5×6.3×10.0 cm(3) by ultrasound. The CBC abnormalities were confirmed (WBC 20×109/l, hemoglobin 10.3 g/dl, platelets 90×109/l). A repeat BM biopsy revealed a cellularity of nearly 100%, significantly decreased megakaryocytes and erythroid precursors, without dysplastic features. Mast cells were absent. There was diffuse increase in thick reticulin with extensive intersections and focal coarse collagen bundles. Overall, the picture was consistent with a diagnosis of eosinophilia-associated myeloproliferative neoplasm with myelofibrosis MF-2, unclassified. Conventional cytogenetic analysis, performed according to the protocols used in our clinical cytogenetics laboratory as previously described,(6) confirmed the abnormal karyotype in 20/20 metaphases (Supplementary Figure 1A). Fluorescence in-situ hybridization (FISH) analyses for BCR-ABL or rearrangements of PDGFRA or PDGFRB were negative. Real-time PCR failed to detect the JAK2V617F or MPLW515K gene mutations. A next generation sequencing-based analysis for the detection of cancer-associated mutations in 53 genes was negative (Supplementary Table 1). BM cells tested by flow cytometry using an extensive T-cell panel did not show aberrant T-cell clones. Given the patient’s cytogenetic abnormality, we performed a dual-color break-apart FISH test for ETV6 rearrangements. FISH was performed using an LSI ETV6 probe (Abbott Molecular, Inc., Des Plaines, IL, USA), which hybridizes to band 12p13 of chromosome 12. A total of 200 interphases were analyzed according to the protocols used in our clinical cytogenetics laboratory, using a cutoff of 3.2% for the FISH probe. A split signal was observed in 82% of the 200 interphases analyzed (Supplementary Figure 1B). To identify the fusion partner of ETV6 we performed a first round of 3’-Rapid Amplification of cDNA Ends (RACE)-PCR using the first-strand cDNA as a template, primers located at ETV6 exons 4 and 5 and a universal adapter (5’-AGCAGAGTGACG-3’, homologous to the adapter sequence used to prime the first-strand cDNA synthesis). The diluted product of the first RT-PCR was submitted to nested PCR with ETV6 exon-5 primer and a universal adapter reverse primer (Supplementary Figures 2A and B). The PCR products were separated by electrophoresis on a 1.5% agarose gel and purified (sequences of all PCR primers used are listed in Supplementary Table 2). Since the 3’-RACE-PCR technology can give rise to artefacts, we performed RT-PCR using specific ETV6 forward and FLT3 reverse primers on the purified products of nested PCR. This resulted in an amplicon of 1050 base pairs, confirming that the two genes were indeed fusion partners. RT-PCR performed on a sample from a control patient negative for ETV6-FLT3 fusion failed to show a fusion product confirming the specificity of the above RT-PCR primers for the ETV6-FLT3 fusion gene (Figure 1). These results indicated that the fusion occurred downstream of ETV6 exon-5 and upstream of FLT3 exon-15. Sequencing of the fusion product was not possible due to limited availability of the patient sample.
Figure 1.
Identification of the ETV6-FLT3 fusion gene. RT-PCR using ETV6 exon-5 forward primer and FLT3 exon-15 reverse primer results in an amplicon of 1050 base pairs, confirming the identity of the two fusion partners (center lane). RT-PCR conducted on an ETV6-FLT3-negative control patient sample using forward ETV6 exon-5 primer and reverse FLT3 exon-15 primer, fails to generate an amplicon (right lane).
The patient was treated with the FLT3 inhibitor sorafenib at a dose of 400 mg twice daily. Owning to severe fatigue, the dose was reduced to 200 mg twice daily after 2 weeks. After 1.5 months of therapy, the patient’s CBC showed a WBC of 3.8×109/l (normal differential), hemoglobin 9.8 g/dl, and platelets 137×109/l. BM biopsy revealed marked hypocellularity, mild dysmyelopoiesis, and mild dyserythropoiesis. Karyotype showed the t(12;13)(p13;q12) translocation in 2/15 metaphases. Collectively, these data indicated a complete hematological and very good partial cytogenetic response. Because of the patient’s young age and availability of a fully matched sibling donor, she underwent consolidation with SCT. Conditioning consisted of fludarabine, busulfan and anti-thymocyte globulin. Only transient mild cutaneous and gastrointestinal graft-versus-host disease (GVHD) was observed post SCT. BM biopsies at 3 and 6 months post SCT showed complete morphological and cytogenetic remission. Eleven months after the diagnosis and 249 days post SCT, the patient is alive in clinical, marrow and cytogenetic complete remission, with no evidence of GVHD.
ETV6-FLT3-positive MLN-eos is an extremely rare condition, with only 4 cases reported to date.(3-5) Only two of the four patients received a FLT3 inhibitor (sunitinib and/or sorafenib), and the disease was rapidly fatal in 3 cases. The patient described by Vu et al.(3) presented with leukocytosis and eosinophilia, which progressed while on hydroxyurea and, subsequently, imatinib. It is unclear whether the progression occurred in the form of acute leukemia. The patient died despite the initiation of high-dose chemotherapy. The second patient reported(5) presented with T-cell lymphoblastic lymphoma (T-LBL) and concomitant myeloid neoplasm with eosinophilia, both of which were ETV6-FLT3-positive. The patient received intensive chemotherapy followed by SCT, and achieved a complete cytogenetic remission. A cytogenetic relapse post SCT responded to a tacrolimus taper, suggesting the existence of a graft-versus-leukemia effect. Walz et al.(4) reported two cases of ETV6-FLT3-positive MLN-eos. The first patient presented with increased BM myeloid blasts and nodal T-LBL, which initially responded to sunitinib but rapidly relapsed with increased BM blasts and complex karyotype. The patient was rechallenged with sorafenib but developed a resistant FLT3 mutation and died despite receiving high-dose chemotherapy. The second patient was diagnosed with MLN-eos after being treated for peripheral T-cell lymphoma, which subsequently relapsed as T-LBL with increased eosinophilia. His disease initially responded to sunitinib but rapidly progressed in the BM, with complex karyotype, and the patient died shortly afterwards.
Here, we report the first patient with chronic-phase ETV6-FLT3-positive MLN-eos to be treated upfront with sorafenib. The patient obtained a very good partial cytogenetic response after only 1.5 months of therapy. Given the aggressive clinical course described in the other published cases, the patient decided to proceed to SCT as soon as a response was documented.
FLT3 is the single most commonly mutated gene in hematologic malignancies,(7-9) but it is rarely a partner in fusion genes. ETV6-FLT3 has been associated with the development of MLN-eos.(3-5) In vitro studies have shown that the ETV6-FLT3 oncoprotein induced interleukin-3-independent growth of murine hematopoietic Ba/F3 cells.(3) The juxtamembrane domain of FLT3 appears critical for proliferation.(10) In addition, growth factor receptor-binding protein 2, an adaptor protein that mediates survival signaling in ligand-activated wild-type FLT3, may play a role in ETV6-FLT3 leukemogenesis.(11) Breakpoints involved in the formation of ETV6-FLT3 have been reported at exons 4 or 5 of ETV6 and exon 14 of FLT3. Whether the peculiar breakpoints found in our case (ETV6 exon 5-FLT3 exon 15) determined the more indolent behavior of the MLN-eos remains to be ascertained, but clearly the ETV6-FLT3 fusion represented a “driving lesion” in our patient. It is unknown whether long-term remissions are achievable after obtaining a cytogenetic response with FLT3 inhibitors and whether SCT is mandatory in patients with MLN-eos and ETV6-FLT3 as the sole abnormality.
In conclusion, ETV6-FLT3-positive MLN-eos appears to be a consistent clinical entity that could eventually fall under the WHO-defined category of MLN-eos. Given its extreme rarity, but important therapeutic implications due to the availability of FLT3 inhibitors, similar cases need to be reported to allow better understanding of their biology, natural history and treatment outcomes.
Supplementary Material
Footnotes
Conflict of interest statement: The authors have no competing financial interests to disclose.
Supplementary information accompanies this paper on the Leukemia website (http://www.nature.com/leu)
Author contributions
LF conceived and designed the work that led to the submission, acquired and interpreted the data, and drafted and approved the final manuscript; MM GL, KPP, RL, UP and LML acquired data and revised and approved the final manuscript; treated the patient and revised and approved the final manuscript; SV conceived and designed the work that led to the submission, interpreted the data, revised and approved the final manuscript.
References
- 1.Bain B, Gilliland D, Horny H-P, Vardiman J. Myeloid and Lymphoid Neoplasms with Eosinophilia and Abnormalities of PDGFRA, PDGFRB, or FGFR1. World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of Haematopoietic and Lymphoid Tissues. IARC Press; Lyon, France: 2008. pp. 68–73. [Google Scholar]
- 2.De Braekeleer E, Douet-Guilbert N, Morel F, Le Bris MJ, Basinko A, De Braekeleer M. ETV6 fusion genes in hematological malignancies: a review. Leuk Res. 2012;36:945–961. doi: 10.1016/j.leukres.2012.04.010. [DOI] [PubMed] [Google Scholar]
- 3.Vu HA, Xinh PT, Masuda M, Motoji T, Toyoda A, Sakaki Y, et al. FLT3 is fused to ETV6 in a myeloproliferative disorder with hypereosinophilia and a t(12;13)(p13;q12) translocation. Leukemia. 2006;20:1414–1421. doi: 10.1038/sj.leu.2404266. [DOI] [PubMed] [Google Scholar]
- 4.Walz C, Erben P, Ritter M, Bloor A, Metzgeroth G, Telford N, et al. Response of ETV6-FLT3-positive myeloid/lymphoid neoplasm with eosinophilia to inhibitors of FMS-like tyrosine kinase 3. Blood. 2011;118:2239–2242. doi: 10.1182/blood-2011-03-343426. [DOI] [PubMed] [Google Scholar]
- 5.Chonabayashi K, Hishizawa M, Matsui M, Kondo T, Ohno T, Ishikawa T, et al. Successful allogeneic stem cell transplantation with long-term remission of ETV6/FLT3-positive myeloid/lymphoid neoplasm with eosinophilia. Ann Hematol. 2013;93:535–537. doi: 10.1007/s00277-013-1843-9. [DOI] [PubMed] [Google Scholar]
- 6.Jaso JM, Yin CC, Lu VW, Zhao M, Abruzzo LV, You MJ, et al. B acute lymphoblastic leukemia with t(14;19)(q32;p13.1) involving IGH/EPOR: a clinically aggressive subset of disease. Mod Pathol. 2013 doi: 10.1038/modpathol.2013.149. [DOI] [PubMed] [Google Scholar]
- 7.Matthews W, Jordan CT, Wiegand GW, Pardoll D, Lemischka lR. A receptor tyrosine kinase specific to hematopoietic stem and progenitor cell-enriched populations. Cell. 1991;65:1143–1152. doi: 10.1016/0092-8674(91)90010-v. [DOI] [PubMed] [Google Scholar]
- 8.Rosnet O, Mattei M-G, Marchetto S, Birnbaum D. Isolation and chromosomal localization of a novel FMS-like tyrosine kinase gene. Genomics. 1991;9:380–385. doi: 10.1016/0888-7543(91)90270-o. [DOI] [PubMed] [Google Scholar]
- 9.Stirewalt DL, Radich JP. The role of FLT3 in haematopoietic malignancies. Nat Rev Cancer. 2003;3:650–665. doi: 10.1038/nrc1169. [DOI] [PubMed] [Google Scholar]
- 10.Vu HA, Xinh PT, Kano Y, Tokunaga K, Sato Y. The juxtamembrane domain in ETV6/FLT3 is critical for PIM-1 up-regulation and cell proliferation. Biochem Biophys Res Commun. 2009;383:308–313. doi: 10.1016/j.bbrc.2009.03.157. [DOI] [PubMed] [Google Scholar]
- 11.Chonabayashi K, Hishizawa M, Kawamata S, Nagai Y, Ohno T, Ishikawa T, et al. Direct binding of Grb2 has an important role in the development of myeloproliferative disease induced by ETV6/FLT3. Leukemia. 2013;27:1433–1436. doi: 10.1038/leu.2012.333. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.