Abstract
The role of ownership in the provision of nursing home care has long been a challenging issue for policymakers and researchers. Although much of the focus historically has been on differences between for-profit and not-for-profit facilities, this simple distinction has become less useful in recent years as companies have employed more complicated ownership and management structures. Using detailed ownership data from the State of Texas, we describe the evolution of nursing home corporate structures from 2000–2007, analyze the effect of these structures on quality of care and staffing in nursing homes, and discuss the policy implications of these changes.
INTRODUCTION
The role of ownership in the provision of nursing home care has long been a challenging issue for policymakers and researchers. Historically, much of the focus in this area has been on for-profit providers, which have played a prominent role in the nursing home sector for decades. Nearly two-thirds of facilities in the United States currently operate on a proprietary basis, and many of these facilities operate as part of multi-facility chains. In the context of recurring quality of care problems, the role of for-profit companies often has been investigated as a possible contributing factor, and a large body of research has compared care delivered by for-profit and not-for-profit facilities.(Hillmer, Wodchis, Gill, Anderson, & Rochon, 2005)
In recent years, the simple description of “for-profit” or “not-for-profit” has become less useful in describing nursing home ownership. For instance, as detailed in a 2007 account in the New York Times, nursing homes can use complex management structures that might obscure the entities responsible for delivering care and hamper the ability of residents and families to seek recourse through litigation.(Duhigg, 2007) Although the findings of the Times were presented in the context of exploring private equity investment in nursing homes, the ability to structure ownership in ways that separate real estate from operations and that decentralize ownership across distinct sub-companies has relevance for the nursing home industry as a whole. In other words, knowing the proprietary status of a nursing home provider is insufficient to discern how organizational assets are structured and the operational approach of the company managing the delivery of nursing home services.
In the wake of the New York Times article, the immediate attention of Congressional policymakers and other stakeholders centered on private equity investment in the nursing home sector, specifically focusing on its impact on the quality of resident care. At the same time, policy attention to the issue played out in multiple state legislatures, as advocates and labor organizations raised concerns about the purchase of the nation’s largest nursing home chain, HCR Manor Care, by the private equity firm the Carlyle Group.(Heath, 2007) Importantly, the empirical evidence of the quality impact of private equity investment in the nursing home industry has been mixed to date. Research by consumer advocates and labor union representatives found that staffing and quality decreased after private equity firms purchased nursing homes from national chains.(Testimony before the US House Committee on Ways and Means by Charlene Harrington and Arvid Mueller (November 15 2007)) In contrast, the Florida Agency for Health Care Administration reviewed the impact of similar transactions in the state of Florida and did not find a drop in quality following facilities’ purchase.(Florida Agency for Health Care Administration, 2007) Similarly, a review of these transactions nationally did not find a negative impact of private equity purchase on nursing home quality of care.(D. G. Stevenson & Grabowski, 2008) The same study emphasized that its findings presented an early snapshot only and that the long-term impact of these types of transactions could vary substantially depending on the organizational structures and capitalization of the resulting companies, the length of time the assets were held, and the exit strategies that were ultimately employed.
Perhaps reflecting the reality that for-profit investment, both privately and publicly held, will likely play a continued role in the nursing home sector, policymakers have focused increasingly on broader issues of ownership transparency and accountability. A key example of this attention is inclusion of provisions from the Nursing Home Transparency and Improvement Act in the broader health reform legislation that was passed in 2010. The provisions seek to increase transparency of and accountability for nursing home care and include ownership-focused components such as requiring the Department of Health and Human Services (DHHS) to identify entities that have either a significant ownership interest (greater than 5 percent) in a nursing home or play an important role in its management, financing, or operations. In addition, provisions require the DHHS Secretary to conduct a two-year demonstration project to develop, test, and implement an independent monitoring program to oversee interstate and large intrastate nursing home chains.
A key lynchpin in researching and enforcing policy directives around nursing home ownership is having timely, detailed data about ownership structures and management arrangements. Importantly, Federal datasets are not yet able to facilitate these tasks adequately. On-Line Survey Certification and Reporting (OSCAR) data offer only cursory information about ownership, including for-profit and chain status and, where relevant, the name and organizational type of the parent company. Even the straightforward task of identifying facilities with the same chain owner can be difficult with OSCAR data, as this field in the database is an open-ended text field subject to slight variations and errors in data entry. In addition, the Provider Enrollment, Chain, and Ownership System (PECOS) data have faced multiple implementation challenges to date and have not yet fulfilled their purpose to provide detailed information on ownership structures and changes over time.(U.S. Government Accountability Office, 2010)
At this time, the most viable option to pursue these types of questions is to obtain ownership data from state licensure agencies, which play an important regulatory role in nursing home oversight. To this end, we obtained detailed nursing home ownership data from the State of Texas in the context of a project funded by the Office of the Assistant Secretary for Planning and Evaluation (ASPE) within DHHS. In the following paper, we first describe the evolution of nursing home ownership structures over time, including the use of limited liability structures, the role of management companies, and the overall complexity of corporate structures. Second, we seek to understand the relationship between corporate structure and a range of facility characteristics, including quality of care and staffing.
DATA AND METHODS
The core analyses in this project were conducted based on a comprehensive dataset compiled from the Texas Ownership Management and Tracking (OMT) dataset and merged with data from the Online Survey, Certification and Reporting system (OSCAR). The former is managed by the Texas Department of Health, while the latter falls under federal jurisdiction in the Centers for Medicare and Medicaid Services (CMS). The design and roles of these data sources are discussed below.
Texas OMT Data
Maintained by the Texas Department of Health, the OMT system is a large database summarizing ownership and management details of nursing homes and other health facilities in Texas, beginning roughly in 2000. OMT data, available back in time, are collected when nursing home entities apply for licensure (at inception and every two years subsequently) and when ownership structures change. The data include information on nursing home ownership multiple layers deep to the level of the individual person, information about management companies used by operators (e.g., for staffing or payroll), and limited, cross-sectional information about property ownership.
Analyses of the OMT dataset focused on two types of entries: facilities, which refer to the brick-and-mortar buildings in which nursing home services are provided, and entities, which are the businesses and people with controlling stakes in either the ownership of the facility’s license or in the management of these facilities. The OMT data were obtained through a Data Use Agreement with the State of Texas and were accessible in Microsoft Access as a series of tables that are linked together through various facility and entity identifiers. Our analyses used seven of the available tables, including information about facility demographics, facility ownership management, and corporate structures for both ownership and management entities. More details about these data can be found here: http://aspe.hhs.gov/daltcp/reports/2009/TXNHown.htm.
OSCAR Data
For several of our analyses, we merged OMT data for facilities with widely-used data from the On-line Survey, Certification, and Reporting (OSCAR) system. OSCAR contains survey and certification data for all Medicaid- and Medicare-certified facilities in the United States. Collected and maintained by CMS, the OSCAR data include information about whether homes are in compliance with federal regulatory requirements. Nursing homes submit facility, resident, and staffing information. Deficiencies are entered into OSCAR by survey agencies when facilities are found to be out of compliance with federal regulatory standards (regular inspections occur every 9–15 months; complaint investigations can occur at any time). Each deficiency is categorized into one of 17 areas and rated by scope and severity (on an ascending scale ranging from “A” to “L” in order of increasing severity). OSCAR data have important limitations that should be noted, including a lack explicit auditing procedures of facility-reported information, potential variation in the survey process across states, and possible under-reporting of serious quality problems.(Institute of Medicine (U.S.). Committee on Improving Quality in Long-Term Care, Wunderlich, & Kohler, 2001; US Government Accountability Office, 2008)
Analyses
The final database was designed primarily around OSCAR observations, layering information about ownership type, the use of management companies, and the complexity of ownership structures onto these data. The final dataset captured information about all entities with at least a 5% ownership stake in either the ownership or management of a nursing home (or both), including the percentage stake that each entity controlled and the number of levels deep that such control existed.
Using the merged dataset, we first analyzed nursing home ownership type over time. “Ownership type” generally referred to for-profit corporations, non-profit corporations, limited liability corporations (LLC), general, limited, and limited liability partnerships (GP, LP, and LLP, respectively), and other ownership types including sole proprietorship. Detailing the features of these different ownership types is beyond the scope of this paper; however, it is important to note that we were particularly interested in the use of structuring options that limited the degree of liability for investors and other, commonly-owned facilities, a point to which we return below.1 Of note, we aggregate the three partnership types into a single “partnership” category; the vast majority of these in the Texas data are limited partnerships.
Second, we analyzed the use of management companies by nursing homes and their relationship to facility ownership over time. The relationships between the ownership and managing entities were classified as follows: Self-Managed, meaning that no managing company was hired to run the facility; Separate Owner, implying the ownership and management entities were separate; or Same Owner, meaning the owner and manager could reasonably be thought of as the same or connected parties (if at least one entity had a 10% or greater stake in both aspects of the nursing home).
Third, we examine, at a simplified level, the changing complexity of ownership structures for Texas nursing homes over time. We measure complexity as the number of levels deep at which the final entities maintain ownership stakes in nursing homes. In the OMT data, complexity ranged from 1 (when the top-level owner was the final owner) to 7 (when the final owners were 6 layers deeper than the top-level (i.e., separated by multiple sub-entities)). If a facility had multiple final owners at different levels, the deepest level at which ownership was held was recorded as the home’s complexity.
Fourth, we analyzed descriptive traits of nursing homes across three ownership types of interest: limited liability corporations, partnership structures, and other company structures. Traits of interest included characteristics from the OSCAR data (e.g., structural traits, staffing and payer mix) and the OMT data (e.g., ownership complexity and use of a management company).
Finally, we examined the relationship of ownership and corporate structure and six nursing home traits of interest: total deficiencies; G-level deficiencies (Y/N); percent Medicare; percent Medicaid; registered nurse (RN) staffing; and certified nurse aide (CNA) staffing. We used linear regressions except in the case of G-level deficiencies, where we used logistic regression and reported odds ratios. We used facility-level fixed effects for each regression and included a range of control variables, including year dummies. Thus, given the inclusion of facility and year dummies, these models are identified via within-facility changes in ownership structure over the study period. The regressions included all management/ownership types in the same model, thus identifying the marginal effects of these features in the context of the others.
For each of the dependent variables, the main models structured the explanatory variables of interest as follows: i) a dummy variable grouping facilities where any limited liability structure is implemented (LLC, LP, GP); ii) a dummy variable grouping facilities that used any management company (including cases where the facility and management company are owned by the same entity) to compare against facilities not using any management company. As both for-profit and non-profit companies may use these structures, we included an interaction term with for-profit status interacted with this variable. As a sensitivity check, we also ran models i) with separate dummy variables for each of the structure types of interest (for-profit, LLC, LP; using non-profit as the comparison group) and no additional interaction terms; and ii) with a dummy variable grouping facilities that used an external management company where the facility and management company are owned by different entities. These results are not reported below but were consistent across specifications.
RESULTS
Corporate Structure and Ownership Type
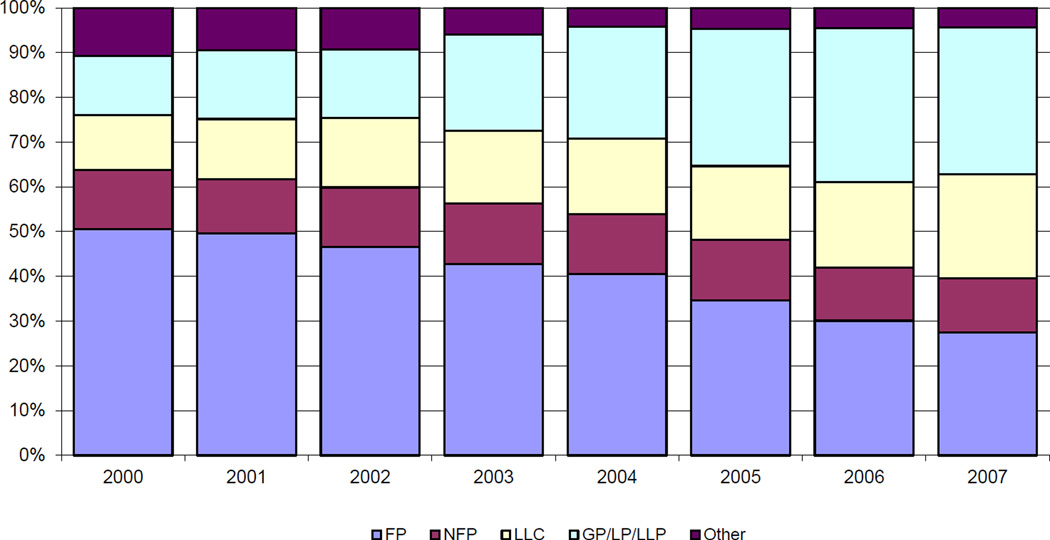
Figure 1 uses an ownership type field available in the OMT data to indicate whether facilities are owned by a for-profit corporation (FP), not-for-profit corporation (NFP), limited liability company (LLC), general partnership (GP), limited partnership (LP), limited liability partnership (LLP), or other (e.g., government owned) structure. As can be seen in the figure, the percent of facilities that use the for-profit corporate structure decreased over the study period (from 51% in 2000 to 28% in 2007), while the percent owned by a limited liability company and a partnership of some kind (the vast majority use the limited partnership structure in particular) increased substantially—from 12% in 2000 to 23% in 2007 for LLCs, and from 13% to 33% for partnerships. The prevalence of facilities using the not-for-profit corporate structure, meanwhile, was relatively stable over the observation period. Both for-profit and non-profit facilities in Texas used structures such as LLCs and LPs, but for-profit facilities tend to employ these structures to a much greater extent – 65% of for-profit facilities used either a LLC or LP structure in 2007, compared to 21% of non-profit facilities (not shown). Similarly, although chain and non-chain facilities used these alternate structures, chain facilities use them to a greater extent (66% of chain facilities used either a LLC or LP structure in 2007, compared to 48% of non-chain facilities)
Figure 1. Nursing Home Ownership Types in Texas Nursing Homes, 2000–2007.
Source: Texas Ownership Management and Tracking (OMT) data. FP=for-profit; NFP=not-for-profit; LLC=limited liability corporation; GP=general partnership; LP=limited partnership; LLP=limited liability partnership. Other includes government owned facilities, facilities owned by trusts.
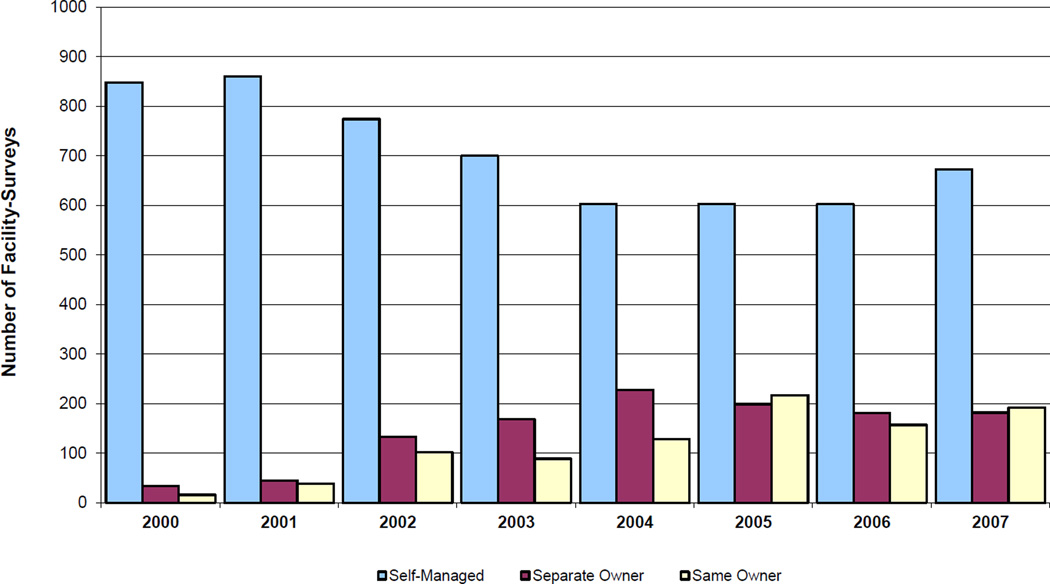
Use of Management Companies
OMT data convey the degree that nursing homes engage management companies, according to the management-ownership relationship variable described earlier. Figure 2 shows a trend toward the use of other companies in the management of facility operations. Since 2000 the number of facilities that were self-managed steadily decreased. Management companies are either “Separate Owner” entities or “Same Owner” entities, based on whether there is commonality in the core owners. As shown, the use of a management company is indicative of “outsourcing” only about half of the time. In 2007, for instance, around 50% of management companies were owned by the same entities that owned the facility.
Figure 2. Management/Ownership Relationships in Texas Nursing Homes, 2000–2007.
Source: Texas Ownership Management and Tracking (OMT) data. The relationships between the ownership and managing entities were classified as follows: Self-Managed, meaning that no managing company was hired to run the facility; Separate Owner, implying the ownership and management entities were separate; or Same Owner, meaning the owner and manager could reasonably be thought of as the same or connected parties (if at least one entity had a 10% or greater stake in both aspects of the nursing home).
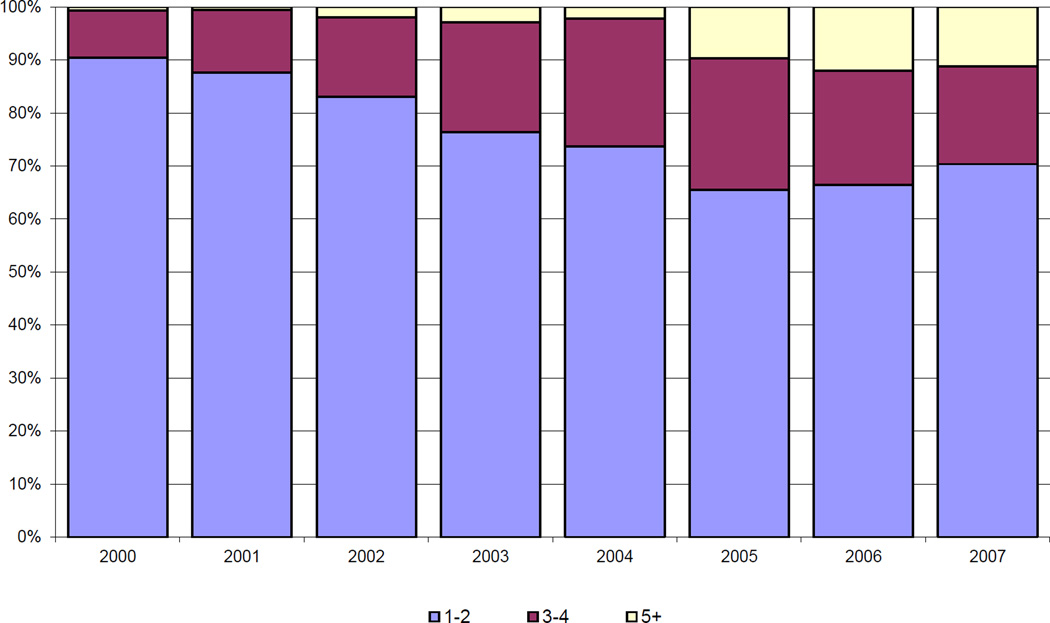
Increase in Ownership Complexity
The rate of Texas nursing home ownership changes, especially toward partnerships and LLCs, gives some sense of the changing corporate structures. However, these changes alone do not tell the whole story. Not only have there been major changes in ownership structure and management, the degree of complexity has greatly increased We measured complexity as the number of levels deep at which the final entities maintain ownership stakes in nursing homes. As discussed earlier, this number ranged from 1, if the top-level owner was the final owner, to 7, if the final owners were 6 layers deeper than the top-level. As shown in Figure 3, ownership complexity has been increasing over time. For example, the percent of Texas nursing homes with ownership structures at least 5 levels deep increased from 0.6% in 2000 to 11% in 2007. Meanwhile, the percent of facilities with ownership structures of 1–2 levels deep decreased from 90% in 2000 to 70% in 2007. Although the most common configuration in any given year was two levels deep, final ownership at three levels deep is now almost as frequent as one level (whereas in 2000 there was a 7%–29% split); the more complex levels have grown from almost zero to being a small minority of facilities. Put differently, the overall level of complexity has increased from final ownership being almost 2 levels deep to final ownership being 3 levels deep, on average.
Figure 3. Ownership Complexity in Texas Nursing Homes, 2000–2007.
Source: Texas Ownership Management and Tracking (OMT) data. Complexity is defined as the number of levels deep at which the final entities maintain ownership stakes in nursing homes. In the OMT data, complexity ranged from 1 (when the top-level owner was the final owner) to 7 (when the final owners were 6 layers deeper than the top-level. If a facility had multiple final owners at different levels, the deepest level at which ownership was held was recorded as the home’s complexity.
Descriptive Traits, by Ownership Structure
Using OMT data merged with information in the OSCAR dataset, we display descriptive trends for various nursing home traits by ownership structure, from 2000 to 2006 in Table 1. We compare facilities in Texas that employ a partnership structure, those that employ a limited liability company (LLC) structure, and those that have all other types of structures, such as not-for-profits, publicly-traded companies and government-run facilities.
Table 1.
Ownership Structure and Nursing Home Traits in Texas NHs, 2000–2006
| Partnership Structure | LLC Structure | Other Structure | ||||
|---|---|---|---|---|---|---|
| 2000 | 2006 | 2000 | 2006 | 2000 | 2006 | |
| Chain Status | 74.6%* | 72.2%* | 92.6%* | 74.1%* | 71.1% | 50.0% |
| Profit Status | 99.2%* | 99.7%* | 96.7%* | 83.8%* | 74.9% | 65.3% |
| ADL Score | 3.7 | 3.7 | 3.6 | 3.7 | 3.6 | 3.7 |
| Acuity Index | 10.6 | 10.2 | 10.2 | 10.4 | 10.3 | 10.3 |
| Payer Status | ||||||
| % Medicare | 18.9%* | 18.0%* | 8.0%* | 13.0%* | 16.4% | 17.3% |
| % Medicaid | 62.4%* | 65.0%* | 74.8%* | 68.9%* | 66.0% | 61.9% |
| % Other | 18.8% | 17.1%* | 17.2%* | 18.2%* | 17.7% | 20.8% |
| Total Beds | 118.6 | 117.7 | 101.6 | 108.0 | 102.5 | 103.5 |
| Occupancy Rate | 69.3%* | 73.6%* | 63.4%* | 71.1%* | 69.2% | 71.6% |
| Total Deficiencies | 6.6 | 6.8 | 7.3* | 7.4 | 6.3 | 6.3 |
| Any G-Level+ Deficiency | 23.8%* | 15.2%* | 30.6% | 16.2%* | 29.2% | 10.3% |
| Staffing Per Resident | ||||||
| Registered Nurses (RNs) | 0.07 | 0.04* | 0.04* | 0.02* | 0.11 | 0.06 |
| Nurses' Aides (CNAs) | 0.51* | 0.34* | 0.35* | 0.34* | 0.53 | 0.50 |
| OMT Ownership Complexity | 2.35* | 3.80* | 2.12* | 2.75* | 1.74 | 2.07 |
| Outsourced Management Company | 3.1%* | 9.6%* | 9.9%* | 37.1%* | 2.3% | 11.8% |
| Number of Observations | 130 | 356 | 121 | 197 | 733 | 262 |
Source: Texas Ownership Management and Tracking System (OMT) data and Online Survey Certification and Reporting (OSCAR) data. LLC=limited liability corporation.
Significantly different from Other Structure (p<0.05).
Several trends are worth noting. First, the number of facilities using a partnership structure has almost tripled from 2000 to 2006, while the number of LLCs increased substantially as well. Both of these structures have been available to providers throughout the time period, but have become increasingly used over time. Given that the total number of Texas facilities has been fairly stable, the number of other types of facilities has decreased over the study period. Both partnership and LLC structures tend to be used by for-profit, chain facilities, relative to other facilities in Texas. In particular, nearly all partnerships (99.5% in 2007) are for-profit owned. Still, an increasing number of non-chain and non-profit facilities have used these structures. For example, non-profit facilities grew from only 3.3% of all facilities using a LLC structure in 2000 to 16.2% in 2006.
Resident acuity and ADL scores, payer mix and survey deficiencies are fairly comparable across the three categories, indicating that there may be little relationship between corporate structuring and resident characteristics. Nurse and aide staffing, however, tends to be higher in not-for-profit and other facilities than in LLC and partnership facilities throughout the study period. In 2006, partnerships and LLCs have only 0.04 and 0.02 RN FTEs per resident, respectively, compared to 0.06 in not-for-profit and other facilities, and a similar skew is observed in CNA staffing.
Ownership complexity was significantly greater in partnerships (3.80 levels in 2007) and LLCs (2.75 levels) compared to not-for-profit corporations and others (2.12 levels). Use of a separately-owned management company was highest among LLC facilities, growing substantially from 9.9% in 2000 to 37.1% in 2006. Partnerships and not-for-profit/other facilities also used management companies increasingly, but not to the same extent; their 2006 levels were roughly comparable, at 9.6% for partnerships and 11.8% for not-for-profit/other.
Another way of looking at the relationship of ownership and corporate structure with nursing home traits is with regression models. Table 2 shows the regression of various nursing home traits on several ownership (structure, management outsourcing) and facility-level controls (ownership complexity, facility size, acuity, profit status, chain status, etc.). The table examines six dependent variables: RN staffing; CNA staffing; total deficiencies; G-level deficiencies (Y/N); percent Medicare; and percent Medicaid. As described above, all are linear regressions except for those looking at G-level deficiencies, which uses logistic regression and reports odds ratios. Across the regressions, we found few statistically significant relationships between the ownership variables of interest and the quality-related traits of interest. Moreover, the few statistically significant results paint no consistent picture, and we can discern relatively little from these regression results. The bottom line is that these structural changes alone do not result in shifts in staffing, payer mix, or survey deficiencies.
Table 2.
Relationship between Nursing Home and Ownership Traits of Interest in Texas NHs, 2000–2007
|
Use of a Liability Limiting Structure (0/1) |
Liability × Profit Interaction | Use of a Mgmt Company | |
|---|---|---|---|
| Registered Nurse Staffing Per Resident | −0.012 | 0.021 | −0.011 |
| (0.013) | (0.017) | (0.006) | |
| Aide Staffing Per Resident | −0.147 | 0.186* | −0.005 |
| (0.087) | (0.091) | (0.018) | |
| Total Deficiencies | 0.117 | −1.496 | −0.172 |
| (0.934) | (1.003) | (0.245) | |
| G-Level (or higher) Deficiency (OR) | 0.776 | 0.969 | 1.031 |
| (0.352) | (0.449) | (0.121) | |
| Percent Medicare Payment | −0.449 | 0.681 | −0.798* |
| (2.346) | (2.384) | (0.396) | |
| Percent Medicaid Payment | −4.753* | 4.507* | 1.048* |
| (1.965) | (2.103) | (0.450) |
Source: Texas Ownership Management and Tracking System (OMT) data and Online Survey Certification and Reporting (OSCAR) data Use of a liability limiting structure groups facilities that employed a limited liability corporation (LLC) or limited partnership (LP) ownership structure.
Each deficiency is rated by its scope and severity on a scale of A to L in order of increasing severity. G-level deficiencies or higher are violations including actual harm or immediate jeopardy to residents’ health or safety.
Estimates generated from linear regressions except in case of G-level deficiencies, where we use logistic regression and report odds ratios. Models used facility-level fixed effects for each regression and included a range of control variables, including year dummies. Thus, given the inclusion of facility and year dummies, these models are identified via within-facility changes in ownership structure over the study period. The regressions included all management/ownership types in the same model, thus identifying the marginal effects of these features in the context of the others.
Reference ownership type is not-for-profit.
Significance at p<0.05.
DISCUSSION
Based on detailed ownership data from the State of Texas, nursing home ownership and corporate structures changed substantially in the state during the 2000–2007 time period. Similar to what has occurred in other states, nursing home ownership by large national chains has declined and been replaced by smaller, more regionally-focused private investment-owned facilities.(D.G. Stevenson, Grabowski, & Coots, 2006 (Available at: http://aspe.hhs.gov/daltcp/reports/2006/NHdivest.htm)) Along with these changes, Texas nursing homes increasingly used limited liability company structures and partnership structures (primarily general partnerships and limited partnerships), replacing their previous reliance on basic for-profit and not-for-profit structures. From 2000–2007 the percent of Texas facilities using either a LLC or partnership structure increased from around one-quarter of all facilities to almost two-thirds of all facilities.
Nursing homes in Texas also have increasingly used management companies to deliver care. In part, this shift reflects broader structural changes rather than facilities outsourcing resident care. Of the 35% of Texas facilities that used a management company in 2007, a little more than half of these facilities used a management company that had common ownership to the facility itself. Finally, the combination of these changes gave rise to nursing home corporate structures that were relatively more complex in 2007 compared to previous years. For instance, many of the larger owners in the state now use facility-level limited liability structures that are separated from final level ownership (i.e., the investors) by additional layers of limited liability company structures.
The structural changes used by facility ownership, in particular limited liability company and limited partnership structures, appear to be used disproportionately by for-profit, chain providers. This association is consistent with the rationale for restructuring in the context of the litigation and private investment trends during the study period. Not surprisingly, the facilities that used these limited liability structures have significantly more complex ownership structures overall.
Although facilities using the LLC or LP structure generally exhibited greater numbers of survey deficiencies and lower staffing per resident on average compared to facilities that do not use these structures, the structural changes themselves do not appear to have driven broader changes in the way care is delivered by individual facilities, including their quality of care. In particular, across our regression models, the structural changes we identified did not result in significant shifts in facility staffing, payer mix, or survey deficiencies in the facilities that used these limited liability structures compared to those that did not. In other words, the main story of these changes seems to be the altered corporate structures themselves and not the relationship between these structural shifts and corresponding changes in care. From a quality of care perspective in particular, these results imply that care does not seem to improve or decline overall in the wake of structural or management changes. In other words, the facilities that had higher deficiencies and lower staffing before restructuring tend to look relatively similar after these types changes.
Limitations
Importantly, our study data are based on one state and may not be generalizable to other locales. Although the trends identified in our data appear to be occurring in other states,(Duhigg, 2007) the Texas nursing home market is distinct in important ways. According to recent OSCAR data, for instance, Texas has a larger share of for-profit (83.7% vs. 66.9%) and chain nursing homes (64.5% vs. 53.6%) relative to the national average. In addition, Texas has the ninth lowest occupancy rate in the country (73.2% relative to the national average of 84.3%) and one of the lowest Medicaid payment rates in the country.
Another distinctive feature of the Texas nursing home market that has likely played a central role in spurring changes in nursing home ownership in recent years is the rise of nursing home litigation in the state. Along with Florida, Texas nursing homes were hit especially hard by the rise in malpractice litigation that occurred in the late 1990s and early 2000s, (D. G. Stevenson & Studdert, 2003) possibly leading to increased use of corporate restructuring to help shield parent companies from potentially costly lawsuits. Restructuring can help protect owners from a range of other liabilities as well, including sanctions related to oversight of the Medicare and Medicaid programs and liability under the False Claims Act.(Casson & McMillen, 2003) More specifically, restructuring can limit the reach of sanctions to individual facilities as opposed to entire chains. At the same time, driven in part by liability trends, some larger for-profit nursing home chains exited the Texas market, selling their facilities to private investment companies and others. Similar to broader trends nationally, private investors purchased nursing homes and, in the process of financing these deals, often created companies with re-organized asset and management structures.(D. G. Stevenson & Grabowski, 2008) For instance, investment companies that previously focused on properties such as hotels and shopping malls saw opportunities in the nursing home sector that were shaped by real estate values, inexpensive access to capital, and reliable cash flow for operators.
Policy Implications
Of course, nursing homes are different from other commercial properties, not least because of their mission to care for a frail resident population. Towards this end, Section 6101 of the Patient Protection and Affordable Care Act (PPACA) now requires Medicaid/Medicare certified nursing homes to have available for inspection required ownership and other disclosable party information.2 By March 2012, DHHS will issue final regulations that create a standardized format for reporting the ownership and other disclosable party information specified in PPACA, and by July 2012, facilities will report this information to DHHS via this standardized format. By March 2013, DHHS will make the ownership information submitted via the standardized form available to the public. In this context, it is important to assess the relevance of data on corporate structure and how it might be used by stakeholders. We will focus below on the potential use of detailed ownership data in regulatory oversight activities.
Federal and state quality assurance efforts generally focus at the level of the individual nursing facility.(Testimony before the US Senate Special Committee on Aging by Kerry Weems (November 15 2007)) In the context of chain ownership, this approach implies that state and federal regulators typically do not investigate or sanction corporate culpability beyond the level of the facility. If quality of care is heavily influenced by practices, policies, and systems inherent to ownership, regulators’ facility-specific approach might be ineffective and fail to identify root causes. Switching to a broader regulatory approach may not be feasible for the survey and certification system but could be a central feature for quality improvement organizations (QIOs) identifying areas for improvement. More important, a reformed approach could extend responsibility for resident care beyond where the line has been drawn previously at the individual nursing facility. An important example of this approach is the Corporate Integrity Agreement model used by the HHS Office of the Inspector General over the past several years with 15 corporate nursing home providers.(U.S. Office of the Inspector General, 2009)
To raise a more specific question relevant in the context of the detailed Texas ownership data, what should be done to ensure accountability in the context of complex ownership structures, especially where it can be unclear which entities have responsibility for resident care? Should responsibility extend beyond entities that sign provider agreements with Medicare/Medicaid to other parties that are ostensibly not involved in caring for residents? The answer seems to depend on the extent to which these other entities directly or indirectly influence resident care processes, something that remains unclear.
In the context of this uncertainty, a possible use of detailed ownership data in facility oversight is to monitor involvement of investors (whether of property, management, or operating companies) in the nursing home business and to use this information at the point of licensure application. Indeed, this is one of the primary functions of the OMT data in Texas. If an entity involved in a nursing home sale or new application for licensure has a previous history of being associated with substandard care, detailed ownership data can help flag these instances. Armed with these data, licensure agencies could identify bad actors and introduce potential safeguards to lessen the potential for future problems. In addition, having detailed ownership data could be a useful point of leverage if facilities in operation are unable to meet their regulatory obligations (e.g., hiring a temporary management company or paying financial sanctions). More broadly, detailed ownership data could be useful in determining the factors that influence the provision of excellent and poor quality nursing home care and help delineate the role of ownership in its provision. Greater investigation into these topics by researchers could help advance these objectives.
One outstanding question in the collection and maintenance of nursing home ownership data is whether it has relevance for consumer decision making. As noted above, PPACA mandates that—by March 2013—the DHHS make standardized ownership data available to the public. This reporting will complement ongoing efforts that have developed over the last decade to collect, maintain, and report a wide range of nursing home data via the Nursing Home Compare website and assorted state reporting sites.(Castle & Lowe, 2005; D. G. Stevenson, 2006) As a result of these collective efforts, information about nursing home characteristics, staffing, and the care that is delivered is much more widely available than it was in the past. To some, offering consumers further information on nursing home ownership and corporate structuring could offer another piece of valuable data for consumers to consider in choosing the right nursing homes. Yet, given the complexity of these data and the difficulty consumers may have in navigating the information available on Nursing Home Compare,(Shugarman & Brown, 2006) the use of such data in regulatory oversight seems to be a higher priority. In fact, given the questionable usefulness of these data to consumer decision making (e.g., in discerning a reliable signal related to quality of care), policymakers should be cautious in adding complex ownership data to the wide range of inputs already available to consumers about nursing home care.
As the DHHS develops a standardized format for reporting detailed ownership data, several considerations should guide this process.(Weil, Fung, Graham, & Fagotto, 2006) The ownership data that are collected should have relevance to their intended use, they should be comprehensible to the parties that will use them, and they should streamline the cost of data collection to the extent possible. If detailed ownership data will be used to monitor the involvement of potentially bad actors in the nursing home sector, for instance, the data should be flexible enough to execute queries of particular entities based on parameters of interest. In the context of the Texas OMT data, the complex structures that are used and the multiple layers of ownership possible for operations, management, and property investment imply that a simplistic, flat-file approach would likely not prove dynamic enough to meet the demands of the data. Indeed, a hierarchical, relational database – which Texas uses – seems necessary to capture this information sufficiently.
Conclusion
As the current push toward transparency of nursing home ownership continues, progress to use these data productively will depend on multiple factors. Most obviously, detailed ownership data are not yet available nationally. In addition to the data collected under PPACA, CMS-maintained PECOS data could also serve this role in the future; however, the PECOS data have not yet proven comprehensive or reliable enough for use.(U.S. Government Accountability Office, 2010) Once these core data are in place, important analytic questions remain, namely whether and how nursing home ownership, including corporate structure, matters to the provision of nursing home care. We currently have inadequate understanding of central topics around ownership and nursing home care, including the impact of common ownership across facilities (e.g., does one chain provide consistently better or worse quality of care than another?) and the potential influence of entities beyond the operator/facility itself (e.g., the real property owner) on care delivery. To understand the dynamic effect of ownership in the nursing home sector, a first step is to move beyond the simple distinctions of for-profit/not-for-profit and chain/non-chain to gain a better understanding of how nursing home care and the companies that provide it are evolving. Beyond that, however, it will be important to disentangle which features of nursing home ownership and corporate structuring are most relevant to resident care and to develop an evidence-based and streamlined approach for how this information should be used to ensure high quality of care for residents.
Acknowledgments
The authors are grateful to Assistant Secretary for Planning and Evaluation in the U.S. Department of Health and Human Services for funding the work on which this paper is based (contract #HHSP23320084300EC) and to Susan Polniaszek for overall project guidance. The authors also thank the J.W. Kieckhefer Foundation for providing further support of this work. The opinions and views expressed in this paper are those of the authors and do not necessarily reflect the views of the Department of Health and Human Services or Harvard Medical School.
Footnotes
Sole proprietorship has the greatest liability for the owner, as this business arrangement is characterized by the owner and business being recognized as the same entity (i.e., profits and losses are classified as personal taxes, not corporate taxes, and the normal rules about corporate liability not extending to individual owners do not apply). In contrast, for-profit and not-for-profit corporations are distinct legal entities from their shareholders. For-profit and not-for-profit corporations refer to the corporate structures and not solely to the proprietary status. For instance, a for-profit nursing home may use a for-profit corporate structure, a LLC structure, a LP structure, etc. At the same time, however, under a for-profit corporate structure, liabilities from part of the corporation (e.g., a nursing home) extend to the corporation as a whole. General partnerships – a group of 2+ general partners who all share the risks, liabilities, debts and profits of a company – share some of the same features of sole proprietorship. However, in the Texas data, this corporate structure is used almost exclusively in combination with the limited partnership model. The LP model limits the liability of investors up to their level of investment, and they receive a dividend-like payment instead of a percentage of the profits. The limited liability partnership model is used rarely in the Texas data. Unlike a limited partnership where there are some GPs and some LPs, the LLP structure limits the liabilities of all partners. Each investor takes an active role in management, but they are each insulated from any liability due to misconduct by another member. Finally, the limited liability company is an entity with features of both a corporation and a partnership (especially a LLP). Like a corporation, LLC owners have limited personal liability for the debts and actions of the LLC. Like a partnership, the LLC provides management flexibility and the benefits of pass-through taxation.
Under the legislation, nursing homes are required to have available for inspection the name, title, and period of service for each member of the governing body of the facility, and any person or entity who is an officer, director, member, partner, trustee, managing partner or additional disclosable party of the facility. An “additional disclosable party” includes anyone who exercises operational, financial or managerial control over the facility or any part of the facility; anyone who provides financial or cash management services to the facility; anyone who leases or subleases real property to the facility, or owns a whole or part interest equal to 5 percent of the total value of such real property; and anyone who provides management or administrative services, management or clinical consulting services, or accounting or financial services to the facility. Finally, the facility must disclose the organizational structure of each additional disclosable party to the facility and to one another.
References
- Casson J, McMillen J. Protecting nursing home companies: limiting liability through corporate restructuring. Journal of Health Law. 2003;36(4):577–613. [PubMed] [Google Scholar]
- Castle NG, Lowe TJ. Report Cards and Nursing Homes. Gerontologist. 2005;45(1):48–67. doi: 10.1093/geront/45.1.48. [DOI] [PubMed] [Google Scholar]
- Duhigg C. At Many Homes, More Profit and Less Nursing. New York Times. 2007 Sep 23;:A1. [Google Scholar]
- Florida Agency for Health Care Administration. Long Term Care Review: Florida Nursing Homes Regulation, Quality, Ownership, and Reimbursement. Tallahassee: FL: AHCA; 2007. [Google Scholar]
- Heath T. Under Pressure, Carlyle Issues Patient Promise: Buyout of Nursing-Home Chain Sparks Worries on Staffing Levels. Washington Post. 2007 Oct 22; [Google Scholar]
- Hillmer MP, Wodchis WP, Gill SS, Anderson GM, Rochon PA. Nursing home profit status and quality of care: is there any evidence of an association? Med Care Res Rev. 2005;62(2):139–166. doi: 10.1177/1077558704273769. [DOI] [PubMed] [Google Scholar]
- Wunderlich GS, Kohler PO. Institute of Medicine (U.S.). Committee on Improving Quality in Long-Term Care. Improving the quality of long-term care. Washington, D.C.: National Academy Press; 2001. [PubMed] [Google Scholar]
- Shugarman LR, Brown JA. Nursing Home Selection: How Do Consumers Choose? Washington, DC: Assistant Secretary for Planning and Evaluation; 2006. [Google Scholar]
- Stevenson DG. Is a public reporting approach appropriate for nursing home care? J Health Polit Policy Law. 2006;31(4):773–810. doi: 10.1215/03616878-2006-003. [DOI] [PubMed] [Google Scholar]
- Stevenson DG, Grabowski DC. Private equity investment and nursing home care: is it a big deal? Health Aff (Millwood) 2008;27(5):1399–1408. doi: 10.1377/hlthaff.27.5.1399. [DOI] [PubMed] [Google Scholar]
- Stevenson DG, Grabowski DC, Coots LA. Nursing Home Divestiture and Corporate Restructuring: Final Report. Washington, D.C.: Assistant Secretary for Planning and Evaluation, US Department of Health and Human Services; 2006. (Available at: http://aspe.hhs.gov/daltcp/reports/2006/NHdivest.htm)) [Google Scholar]
- Stevenson DG, Studdert DM. The Rise of Nursing Home Litigation: Findings from a National Survey of Attorneys. Health Aff (Millwood) 2003;22(2):219–229. doi: 10.1377/hlthaff.22.2.219. [DOI] [PubMed] [Google Scholar]
- Testimony before the US House Committee on Ways and Means by Charlene Harrington and Arvid Mueller. 2007 Nov 15; [Google Scholar]
- Testimony before the US Senate Special Committee on Aging by Kerry Weems. 2007 Nov 15; [Google Scholar]
- U.S. Government Accountability Office. Nursing Homes: Complexity of Private Investment Purchases Demonstrates Need for CMS to Improve the Usability and Completeness of Ownership Data. Washington, D.C.: U.S. GAO; 2010. (No. GAO-10-710) [Google Scholar]
- U.S. Office of the Inspector General. Nursing Home Corporations under Quality of Care Corporate Integrity Agreements. Washington, D.C.: OIG; 2009. [Google Scholar]
- US Government Accountability Office. Federal Monitoring Surveys Demonstrate Continued Understatement of Serious Care Problems and CMS Oversight Weaknesses (US GAO-08-517) Washington, DC: 2008. [Google Scholar]
- Weil D, Fung A, Graham M, Fagotto E. The Effectiveness of Regulatory Disclosure Policies. Journal of Policy Analysis and Management. 2006;25(1):155–181. [Google Scholar]