Abstract
Objectives
An increased inter-arm blood pressure difference is an easily determined physical finding, may use as an indicator of cardio vascular event and other sever diseases. Authors evaluated 477 patients to determine the prevalence and significance of inter-arm blood pressure difference.
Methodology
477 routine outdoor patients selected to observe the inter-arm blood pressure difference. Age, height, weight, body mass index, history of disease and blood pressure recorded.
Results
The prevalence of ≥10 mmHg systolic inter-arm blood pressure difference was 5.0% was more as compared to 3.8% had diastolic inter-arm blood pressure difference. The prevalence of systolic and diastolic inter-arm difference between 6 to 10 mmHg was 31.4% and 27.9% respectively. Mean systolic inter-arm blood pressure difference was significantly higher among those patients had a multisystem disorder (10.57±0.98 mmHg) and followed by patients with cardiovascular disease (10.22±0.67 mmHg) as compared to healthy patients (2.71±0.96 mmHg). Various diseases highly influenced the increase in blood pressure irrespective of systolic or diastolic was confirmed strongly significant (p<0.001) at different inter arm blood pressure difference levels.
Conclusion
This study supports the view of inter-arm blood pressure difference as an alarming stage of increased disease risk that incorporated to investigate potential problems at an early diagnostic stage. A significant mean difference between left and right arm blood pressure recorded for many diseases.
Keywords: Inter-arm Difference, Blood Pressure, Systolic Blood Pressure, Diastolic Blood Pressure, Cardio Vascular Disease
Introduction
The inter-arm difference (IAD) in blood pressure (BP) has received attention globally was discovered by Osler in 1915 who noted first. (1) The blood pressure should be measured in both the arms at the first visit because differences exist and measurement in only one arm may lead to under diagnosis of hypertension. (2–3) Hypertension guidelines recommend that blood pressure should be assessed in both arms at the initial visit. (4) The IAD in BP has received increasing attention in recent years because it has found to be associated with peripheral vascular disease (5) but the justification has been poor and adoption in primary care practice negligible to date. (6) The importance of measuring blood pressure in both arms is initially to prevent the misdiagnosis of hypertension due to normal differences in blood pressure between the arms. (7)
Right and left arm differences of a few mm of Hg are quite normal, but more than 10 mm of Hg could significantly increase the risk for cardiovascular outcomes, including increased cardiovascular mortality and all-cause mortality (8–11) and IAD is associated with increased cardiovascular morbidity. (12–14) The arm with the higher values should be used for subsequent measurements was suggested by current guidelines for the management of hypertension. (15) The blood pressure differences between arms are reproducible therefore the BP arm should be pre-specified. IAD is observed with a significant increase in blood pressure whether it is systolic or diastolic, was measured strongly significant (16) and is greater in hypertensive subjects and in patients with peripheral arterial disease. (17)
When both arms are measured, it has been suggested that simultaneous measurement of both arms seems preferable since sequential measurement of BP overestimates the prevalence of systolic IAD. (18) The differences have prognostic importance and the extent to which these differences are reproducible is unknown. Differences between arms are reproducible, but often have variations, therefore; the BP arm should be pre-specified. An average of at least three observations of blood pressure should be used to identify the inter arm blood pressure difference in the left and right arm of patients diagnosed with severe diseases. The arms should not be used interchangeably to obtain BP recordings at repeated visits.
Some studies have shown that IAD in BP even found among youth. IAD in BP is common in young healthy patients, is not dependent on which arm measured first, and unrelated to age, body mass index, and heart rate. The clinical significance of IAD in BP in young, healthy individuals requires long-term follow-up. (19)
The authors hypothesized that IAD in BP may be associated with many diseases and thus the significance of blood pressure differences between arms were identified to examine the relationship between IAD in BP and the increased risk of various diseases, were the goal of research. Henceforth, the authors aimed to determine the prevalence and significance of inter-arm blood pressure difference.
Purpose
This study aimed to identify the prevalence of IAD in BP and its relationship to many diseases. The inter-arm blood pressure difference of a patient is easily recordable and therefore may use as an indicator of diseases such as multisystem disorders, hypertension, cardio vascular in the absence of more costly diagnostic tools.
Materials and Methods
Background and Study Design
A crosssectional study designed and carried out at Sri Aurobindo Medical College and P. G. Institute, Indore (M. P.), India among routine OPD patients.
Participants
Participants were 477 outdoor patients randomly selected for the study during October 2012 to March 2013. Ethical approval obtained from the institution and prior informed consent from the patients obtained for the publication of the clinical details. The inclusion criteria were between the ages of 18 and 81 years and not critically ill were those patients who had at high risk for actual or potential life-threatening health problems and unable to walk. Patients previously diagnosed with various diseases had excluded and those who were not currently taking medicines included.
Blood Pressure Measurements
All patients attended a pre-clinic appointment as part of routine clinical care and assessed by one trained doctor experienced in collecting clinical data. Following five minutes of rest in a supine position, both palpatory and auscultatory methods used to record the blood pressure using two validated standard sphygmomanometers with appropriately sized cuffs simultaneously in both the arms (left and right). Three consecutive systolic and diastolic blood pressures measurements obtained for both the arms. Average of the three measurements for systolic and diastolic blood pressure utilized for further statistical analysis.
Absolute Inter-arm difference
The difference in blood pressure between the left and right arm noted as the presence of inter-arm difference (IAD) in BP. In the present study, the absolute value (││) of the difference in BP noted between arms treated as absolute IAD. For example, the IAD between the left and right arms in SBP for a patient calculated as 123 mmHg − 131 mmHg= −8 mmHg. The absolute value of numeric character −8 is +8 (│−8│=8), therefore the absolute IAD in BP would be read as 8mmHg.
Other Variables
The age recorded according to information provided by patient. The height and weight noted on height measuring scale with weighing machine and history of disease obtained after confirmation from reports. Overall, the information collected by patient charts and by asking the patients.
Statistical analysis
The data analyzed by using SPSS which version 11.0. The descriptive statistics and the prevalence of inter arm blood pressure difference along with 95% confidence interval was calculated. Data expressed as percentages of individuals with systolic IAD and diastolic IAD, and mean ± standard deviation for inter-arm difference in systolic blood pressure and diastolic blood pressure (DBP). The Z-test used to identify the statistical significance of mean differences of systolic and diastolic blood pressure between left and right arm while one-way analysis of variance (ANOVA) used to identify the significance of mean systolic and diastolic blood pressure differences in left arm and right arm at different inter-arm blood pressure difference levels. The probability value p<0.05 was considered as significant while the probability value p<0.001 was considered as highly/strongly significant.
Results
Of the 477 patients in the study, 359 (75.3%) belonged to urban areas. The majority of patients (215, 45.1%) were identified in the age group of 19–39 years, followed by 184 (38.6%) of patients who belonged to age group of 39–59 years. The older age group of 59–79 years consisted of 71 (14.9%) patients. Few (7, 1.5%) patients were 79–81 years old.
Blood pressure-related characteristics of the selected patients have shown in Table 1. The average age of all patients was 41.40±14.99 years while average body mass index was 24.43±3.45 kg/m2. The mean age (51.58±11.05 years) and body mass index (27.00±3.61 kg/m2) was noted raised in those who had IAD for SBP≥10 mmHg. There were 276 (57.9%) female patients and 201 (42.1%) male patients. 16 female found with IAD for SBP≥10 mmHg while 14 found with IAD for DBP≥10 mmHg. IAD for SBP≥10 mmHg reported in 9 (37.5%) patients out of total (76, 15.9%) who had cardiovascular disorders, in 7 (29.2%) out of 67 (14.0%) patients presented with multi-system disorders and in 4 (16.7%) who had endocrine/metabolic disorders. IAD for DBP≥10 mmHg noted in 6 (33.3%) patient had multi-system disorder and followed by 4 (22.2) patients had cardiovascular disorders (Table 1).
Table 1.
Anthropometric and Clinical Findings of Patients
| Characteristics | All patients (n = 477) | IAD for SBP ≥10 mmHg (n=24) | IAD for DBP ≥10 mmHg (n=18) | |
|---|---|---|---|---|
|
| ||||
| Mean ± SD or frequency (%) | Mean ± SD or frequency (%) | Mean ± SD or frequency (%) | ||
| Age (years) | 41.40±14.99 | 51.58±11.05 | 45.22±9.69 | |
| Sex | Male | 201 (42.1) | 8 (33.3) | 4 (22.2) |
| Female | 276 (57.9) | 16 (66.7) | 14 (77.8) | |
| Body Mass Index (kg/m2) | 24.43±3.45 | 27.00±3.61 | 25.81±4.08 | |
| Type of disease | Cardiovascular | 76 (15.9) | 9 (37.5) | 4 (22.2) |
| Gastro-Intestinal & Hemoglobin | 64 (13.4) | - | 2 (11.1) | |
| Endocrine/Metabolic | 67 (14.0) | 4 (16.7) | 2 (11.1) | |
| Infection | 42 (8.8) | 2 (8.3) | 1 (5.6) | |
| Psycho Somatic | 34 (7.1) | 1 (4.2) | 2 (11.1) | |
| Diabetes Mellitus and Hypertension | 15 (3.1) | 1 (4.2) | 1 (5.6) | |
| Multi-System Disorders | 57 (11.9) | 7 (29.2) | 6 (33.3) | |
Comparison between left and right arm showed that the mean absolute IAD for SBP was 3.88 ± 3.04 mmHg while it was 3.47 ± 3.13 mmHg for DBP. IAD was statistically significant (p<0.05) between left and right arm. See Table 2. The absolute IAD of SBP and DBP were independent and significantly different (p<0.05) but the authors believe that the study lacks long-term follow-up and thus unable to reach conclusions regarding the long-term implications of the findings.
Table 2.
Comparison of Absolute Inter-Arm Difference between Left and Right Arm
| Parameters | Blood Pressure | Mean Difference | Standard Error of Difference | Z-value |
|---|---|---|---|---|
| Absolute Inter Arm Difference (mm of Hg) | SBP | 3.88 ± 3.04 | 0.20 | 2.06* |
| DBP | 3.47 ± 3.13 |
p<0.05
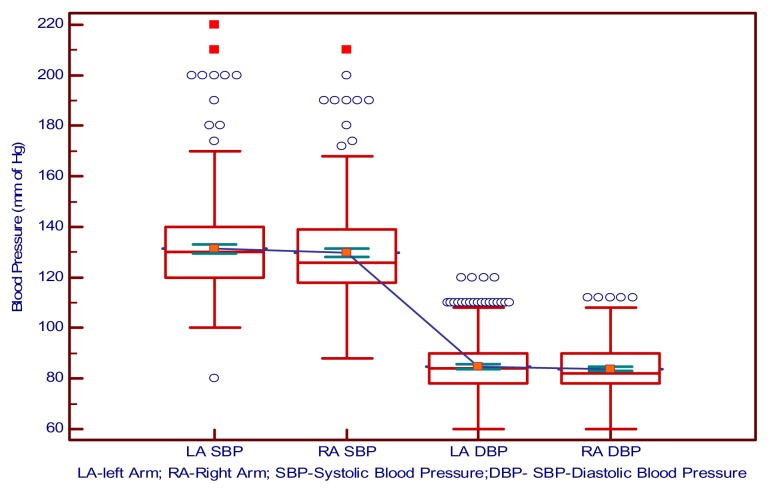
Figure 1 depicts the mean blood pressure with first, second and third quartiles of blood pressure in left and right arm of patients.
Figure 1.
Blood pressure in left and right arm of patients
Box-and-Whisker diagram showing the systolic and diastolic blood pressure in left and right arms of all patients.
Table three shows that the mean of absolute IAD in SBP of patients was the highest amongst those that had diseases of multisystem disorders, (10.57±0.98 mmHg) followed by patients with cardiovascular disorders (10.22±0.67mmHg) while the third maximum was 10.0±0.0 mmHg found among patients with infection, psychosomatic, endocrine/metabolic and diabetes with hypertension. The mean of absolute IAD in DBP was more as compared to SBP and it was maximum for those patients who had multisystem disorders (13.00±7.35 mmHg) followed by patients with endocrine/metabolic (11.00±1.41 mmHg) while the third maximum was 10.50±1.00 mmHg found among patients with cardiovascular disorder. Subjects with renal diseases did not find with absolute IAD > 6 (Table 3).
Table 3.
Mean Absolute Inter-Arm Difference of Disease Conditions
| Type of Disease | IAD Ranges (mm of Hg) | IAD SBP (Mean±SD) | IAD DBP (Mean±SD) |
|---|---|---|---|
| Multisystem Disorders | 6–10 | 6.91±1.02 | 6.93±1.03 |
| >10 | 10.57±0.98 | 13.00±7.35 | |
| Cardiovascular | 6–10 | 6.92±1.01 | 6.78±0.99 |
| >10 | 10.22±0.67 | 10.50±1.00 | |
| Psycho Somatic | 6–10 | 7.18±1.01 | 6.53±0.92 |
| >10 | 10.0±0.0 | 10.0±0.0 | |
| Endocrine/Metabolic | 6–10 | 6.85±1.00 | 6.76±0.98 |
| >10 | 10.00±0.0 | 11.00±1.41 | |
| Diabetes Mellitus & Hypertension | 6–10 | 6.83±1.03 | 6.25±0.71 |
| >10 | 10.0±0.0 | 10.0±0.0 | |
| Infection | 6–10 | 6.50±1.00 | 6.00±0.0 |
| >10 | 10.0±0.0 | 10.0±0.0 | |
| Muscoskeletol | 6–10 | 7.33±1.16 | 7.00±1.16 |
| Nervous System | 6–10 | 7.00±1.41 | 6.00±0.0 |
| Gastro-Intestinal & Hemoglobin | 6–10 | 7.00±1.10 | 8.00±0.0 |
| Respiratory | 6–10 | 6.40±0.89 | 6.00±0.0 |
| Hematology | 6–10 | 6.00±0.0 | 6.67±1.12 |
|
| |||
| Type of diseases with ⇔ | Left arm | F=28.53*** | F=22.88*** |
| Right arm | F=27.68*** | F=18.63*** | |
p<0.001
A very strong mean difference between left and right arm blood pressure identified for different type of disease accompanied with a significant increase in blood pressure. Comparison showed that various IAD level in BP influenced the increase in both systolic as well as in diastolic blood pressure which was confirmed strongly significant for left (p<0.001) and right arm (p<0.001) SBP, and left (p<0.001) and right arm (p<0.001) DBP (Table 3).
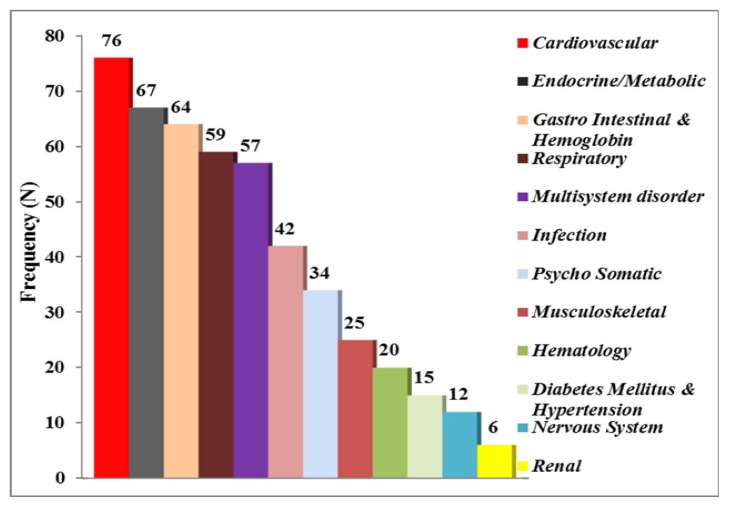
Figure 2 presents disease prevalence among participants. A substantial number of patients (76, 15.9%) presented with cardiovascular disorders followed by 67 (14.0%) with endocrine/metabolic disorders while 64 (13.4%) had gastro-intestinal disorders. Fifty-nine (12.4%) patients were suffering from respiratory ailments and Fifty-seven (11.9%) patients had multisystem disorders, were group of significant disorders that have varied manifestations and can affect so many organs that it is not possible to tie them to a single predominant organ system. Few (42, 8.8%) had infectious disorders whereas 34 (7.1%) suffered from psychosomatic disorders. Musculoskeletal, hematologic, neurologic, renal disorders accounted for the remainder of the patients.
Figure 2.
Type of diseases among patients
Bar diagram showing the distribution of type of diseases among all patients.
Discussion
The present study offers an understanding of the presence and significance of IAD in BP. The term IAD was secondly recognized more than 95 years ago and employed in the year 1920 by Cyriax.(20) An increase in blood pressure difference between left and right arm of a patient in a clinical condition may be considered as an alarming condition for many diseases. Study suggested that 80.5% had absolute IAD of 3.88 ± 3.04 mm of Hg in SBP while 74.8% had absolute IAD of 3.47 ± 3.13 mm of Hg in DBP, confirmed significant on statistical ground which is in agreement with Su et al. (11)
Most of the (15.9%) patients evidenced with cardiovascular disorders followed by 14.0% had endocrine/metabolic disorders. The mean SBP and DBP either in left or in right arm measured different confirmed strongly significant at different IAD levels. The results reported by Clark et al. found to be connected with the findings of the study that an inter-arm difference of 10 mmHg or more in SBP was strongly associated with increased cardiovascular mortality and all-cause mortality. (5, 12, 14)
IAD levels in patients suffering from various diseases highly influenced the increase in BP irrespective of SBP or DBP that is collaborated with the findings of Sharma and Inamdar. (16) Selection of measurement of BP in arm either first in left or right or vice-versa couldn’t make a change in IAD. This was supported by Grossman et al. (19) showed that no difference in BP levels and in IAD between those who measure BP first in the right and those who measure first in the left arm, suggesting that the alert reaction is not an important contributor for IAD.
A study reported the presence of a systematic but clinically insignificant difference in SBP between arms. (17) Marginable mean difference in BP was identified with different type of disease which is in agreement with Su et al. (11) observed that other factors, hypertension and obesity were also associated with an inter-arm difference in SBP of 10 mmHg or more.
The mean of IAD in DBP was more as compared to SBP. Study methods have contributed to the large IAD in blood pressure and even four-limb. BP measurement has become feasible with current technology and might be useful in cardiovascular prevention (21) evidenced in the recent study conducted by Sheng et al. (22)
Comparison between left and right arm BP showed that various diseases highly influenced the increase in both systolic as well as in diastolic blood pressure was confirmed strongly significant, which reflected in the findings of the study conducted by Canepa et al. (23) who reported that an IAD in SBP ≥10 mmHg could potentially be considered as a marker of increased arterial stiffness and support the opportunity to assign individuals with a significant IAD in SBP to further cardiovascular assessment whereas Lane et al. (3) stated that the variation in mean interarm blood pressure was unrelated to age, sex, ethnicity, arm circumference, handedness, being hypertensive, diabetic, or previous history of cardiovascular disease.
The important findings of the study that various diseases significantly influenced the increase in BP correlated with the recent findings of Weinberg et al. (24) showed that an inter-arm SBP difference is common and associated with a significant increased risk for future cardiovascular events, even when the absolute difference in arm in SBP is modest. The present finding may be justified with the findings of the investigators Igarashi et al. who reported that IAD in blood pressure might regard as a simple marker for coronary and peripheral artery diseases. (10) The mean blood pressure difference for left-arm and right-arm was higher in some cases but found statistically insignificant. The similar opinion reflected in the reporting of Pesola et al. (25)
Kim et al. (26) showed that the presence of IAD ≥10 mmHg is a strong independent prognostic marker in acute ischemic stroke whereas if a large IAD of 25.1 mmHg using the arm with the highest reading detected with sequential measurement, healthcare professionals should re-measure the BP in the original arm. (27) Recently, Durrand had confirmed that large IADs are common in vascular surgical patients, with a high potential for monitoring error. (28)
The present study highlights the limitations of single clinic readings, which are not accurate. It suggested the recent recommendations that BP should be measuring in both arms. Bursztyn reported that an instrument designed for simultaneous measurements should be superior. (29) Overall, findings of the study reported that IAD in BP might be relate to many diseases and therefore incorporated to investigate potential problems at an early diagnostic stage.
Limitations of the study
Authors acknowledge that this is a study with sample of only routine patients selected from one medical college and did not conducted any diagnostic tests to rule out any unilateral disease that can have effect on blood pressure values. The study lacks long-term follow-up, therefore unable to reach conclusions regarding the long-term implications of the findings. These could consider as the limitations of this study. A prospective long-term follow-up study could carry out with a cohort of all type of patients across the country to look at the clinical significance of inter-arm blood pressure difference so that preventive measures can take into account.
Implications
This study highlights the limitations of single clinic readings, which may overlook significant health risks. If an inter-arm difference of ≥10 mmHg is present, then the readings should take on the arm with the higher readings. Interarm blood pressure difference may test as a simple marker for chronic diseases. The study evaluated the presence of an inter-arm difference and the risk of many diseases and therefore awareness among medical professional regarding the blood pressure difference in left and right arm may create.
Conclusion
Various types of diseases accompanied with a significant increase in blood pressure. Thus, inter-arm blood pressure difference may nest as a simple marker for diseases. A significant difference in IAD between left and right arm considered as a sign of some type of underlying pathology supported to investigate potential problems at an earlier diagnostic stage. In conclusion, this study explored the prevalence of inter-arm difference in blood pressure measurements among outpatients. The authors suggest that assessment of blood pressure in both arms should become a “core component” when treating patients with high blood pressure or any fatal disease in primary care.
Acknowledgements
Authors are grateful to Dr. Sameer Inamdar (General Medicine Department) who helped in assessing the various parameters and provided valuable suggestions during research.
Footnotes
Conflict of interests: There is no conflict of interests regarding the publication of this paper.
Funding details: None
References
- 1.Osler W. Modern Medicine. Vol. 4. Philadelphia: Lea & Febiger; 1915. [Google Scholar]
- 2.Clark CE, Campbell JL, Evans PH, Millward A. Prevalence and clinical implications of the inter-arm blood pressure difference: a systematic review. J Hum Hypertens. 2006;20:923–31. doi: 10.1038/sj.jhh.1002093. [DOI] [PubMed] [Google Scholar]
- 3.Lane D, Beevers M, Barnes N, Bourne J, John A, Malins S, et al. Inter-arm differences in blood pressure: when are they clinically significant? J Hypertens. 2002;20(6):1089–95. doi: 10.1097/00004872-200206000-00019. [DOI] [PubMed] [Google Scholar]
- 4.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertens. 2003;42(6):1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 5.Clark CE, Campbell JL, Powell RJ. The interarm blood pressure difference as predictor of cardiovascular events in patients with hypertension in primary care: Cohort study. J Hum Hypertens. 2007;2:633–8. doi: 10.1038/sj.jhh.1002209. [DOI] [PubMed] [Google Scholar]
- 6.McManus RJ, Mantm J. Do differences in blood pressure between arms matter? Lancet. 2012;379(9819):872–873. doi: 10.1016/S0140-6736(11)61926-0. [DOI] [PubMed] [Google Scholar]
- 7.Cassidy P, Jones K. A study of inter-arm blood pressure differences in primary care. J Hum Hypertens. 2001;15:519–22. doi: 10.1038/sj.jhh.1001224. [DOI] [PubMed] [Google Scholar]
- 8.Clark CE, Powell RJ. The differential blood pressure sign in general practice: Prevalence and prognostic value. Fam Pract. 2002;19:439–41. doi: 10.1093/fampra/19.5.439. [DOI] [PubMed] [Google Scholar]
- 9.Clark CE, Taylor RS, Shore AC, Campbell JL. The difference in blood pressure readings between arms and survival: Primary care cohort study. BMJ. 2012;344:e1327. doi: 10.1136/bmj.e1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Igarashi Y, Chikamori T, Tomiyama H, Usui Y, Hida S, Tanaka H, et al. A clinical significance of inter-arm pressure difference and ankle-brachial pressure index in patients with suspected coronary artery disease. J Cardi. 2007;50(5):281–89. [PubMed] [Google Scholar]
- 11.Su HM, Lin TH, Hsu PC, Chu CY, Lee WH, Chen SC, et al. Association of inter arm systolic blood pressure difference with atherosclerosis and left ventricular hypertrophy. PLoS ONE. 2012;7(8):e41173. doi: 10.1371/journal.pone.0041173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clark CE, Taylor RS, Shore AC, Ukoumunne OC, Campbell JL. Association of a difference in systolic blood pressure between arms with vascular disease and mortality: a systematic review and meta-analysis. Lancet. 2012;379(9819):905–14. doi: 10.1016/S0140-6736(11)61710-8. [DOI] [PubMed] [Google Scholar]
- 13.Agarwal R, Bunaye Z, Bekele DM. Prognostic significance of between-arm blood pressure differences. Hypertens. 2008;51(3):657–662. doi: 10.1161/HYPERTENSIONAHA.107.104943. [DOI] [PubMed] [Google Scholar]
- 14.Clark CE, Taylor RS, Shore AC, Campbell JL. The difference in blood pressure readings between arms and survival: primary care cohort study. BMJ. 2012;344:e2714. doi: 10.1136/bmj.e1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Williams B, Poulter NR, Brown MJ, Davis M, McInnes GT, Potter JF, et al. Guidelines for management of hypertension: report of the fourth working party of the British Hypertension Society. J Hum Hypertens. 2004;18:139–185. doi: 10.1038/sj.jhh.1001683. [DOI] [PubMed] [Google Scholar]
- 16.Sharma BK, Inamdar S. The assessment of the clinical significance of inter-arm blood pressure difference and depression in general practice: A health initiative cross sectional study. J Health Sci. 2013;3(4):303–318. [Google Scholar]
- 17.Mehlsen J, Wiinberg N. Inter arm difference in blood pressure: reproducibility and association with peripheral vascular disease. Int J Vasc Med. doi: 10.1155/2014/841542. Article2014; ID 841542:4 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Verberk WJ, Kessels AG, Thien T. Blood pressure measurement method and interarm differences: a meta-analysis. Am J Hypertens. 2011;24:1201–8. doi: 10.1038/ajh.2011.125. [DOI] [PubMed] [Google Scholar]
- 19.Grossman A, Prokupetz A, Gordon B, Morag-Koren N, Grossman E. Inter-arm blood pressure differences in young, healthy patients. J Clin Hypertens (Greenwich) 2014;15(8):575–8. doi: 10.1111/jch.12125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cyriax EF. Unilateral alterations in blood-pressure caused by unilateral pathological conditions: the differential blood pressure sign. Q J Med. 1920;13(50):148–164. [Google Scholar]
- 21.Goldhil DR. Bilateral simultaneous indirect systolic blood pressure. Cardiovasc Res. 1986;20(10):774–777. doi: 10.1093/cvr/20.10.774. [DOI] [PubMed] [Google Scholar]
- 22.Sheng CS, Liu M, Zeng WF, Huang QF, Li Y, Wang JG. Four-limb blood pressure as predictors of mortality in elderly Chinese. Hypertens. 2013;61(6):1155–60. doi: 10.1161/HYPERTENSIONAHA.111.00969. [DOI] [PubMed] [Google Scholar]
- 23.Canepa M, Milanesch Y, Ameri P, AlGhatrif M, Leoncini G, Spallarossa P, et al. Relationship between inter-arm difference in systolic blood pressure and arterial stiffness in community-dwelling older adults. J Clin Hypertens (Greenwich) 2013;15(12):880–87. doi: 10.1111/jch.12178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weinberg I, Gona P, O’Donnell CJ, Jaff MR, Murabito JM. The systolic blood pressure difference between arms and cardiovascular disease in the Framingham Heart Study. American Journal of Medicine. 2014;127(3):209–215. doi: 10.1016/j.amjmed.2013.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pesola GR, Pesola HR, Nelson MJ, Westfal RE. The normal difference in bilateral indirect blood pressure recordings in normotensive individuals. Am J Emerg Med. 2001;19(1):43–5. doi: 10.1053/ajem.2001.20021. [DOI] [PubMed] [Google Scholar]
- 26.Kim J, Song TJ, Song D, Lee HS, Nam CM, Nam HS, et al. Interarm blood pressure difference and mortality in patients with acute ischemic stroke. Am Acad Neurol. 2013;80(16):1457–64. doi: 10.1212/WNL.0b013e31828cf87c. [DOI] [PubMed] [Google Scholar]
- 27.Martin U, Holder R, Hodgkinson J, McManus R. Inter-arm blood pressure differences compared with ambulatory monitoring. Br J Gen Pract. 2013;63(610):240. doi: 10.3399/bjgp13X663055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Durrand JW, Batterham AM, O’Neill BR, Danjoux GR. Prevalence and implications of a difference in systolic blood pressure between one arm and the other in vascular surgical patients. Anaesthesia. 2013;68(12):1247–52. doi: 10.1111/anae.12452. [DOI] [PubMed] [Google Scholar]
- 29.Bursztyn M. Inter-arm blood pressure difference. J Clin Hypertens (Greenwich) 2013;15(11):774–775. doi: 10.1111/jch.12216. [DOI] [PMC free article] [PubMed] [Google Scholar]