Abstract
Visceral leishmaniasis is a life-threatening disease of great public health relevance in Brazil. The municipality of Petrolina is an endemic area in the State of Pernambuco, Brazil. This study was designed to assess the recent expansion of VL in the municipality of Petrolina, Pernambuco. Patients data were obtained from the Brazilian National Information System for Notifiable Diseases (SINAN). A total of 111 records from 2007 to 2013 were investigated, of which 69 were residents in Petrolina. The disease has predominantly affected 1-4 year old children (34.8%). Most of the patients were males (59.4%). Co-infection with human immunodeficiency virus occurred in 14.5% of the cases. The criterion most frequently used was the clinical and epidemiological confirmation (59.4%), with clinical cure in 78.3% of cases and one fatal outcome. Visceral leishmaniasis is endemic in Petrolina with transmission levels varying from moderate to high. The present study has shown the precariousness of the use of diagnostic tests in primary healthcare units, and this misuse has interfered with the diagnosis and treatment of cases.
Keywords: Visceral leishmaniasis, Epidemiology, Endemic diseases
INTRODUCTION
Visceral leishmaniasis (VL) is a major public health problem in many parts of the world and is endemic in 77 countries, mainly in the tropical and subtropical regions of Asia, the Middle East, Africa, Central America, and South America. Approximately 0.2-0.4 million VL cases occur every year in 11 countries in the Americas and in 66 countries in Europe, Asia and Africa, according to recent estimates1 , 2.
In Brazil, VL is a zoonotic vector-borne disease widely distributed with a mean annual incidence rate of two cases per 100,000 inhabitants3. VL constitutes an important public health issue due to the increasing number of new cases diagnosed and the continuous expansion of the disease in State capitals and adjacent metropolitan regions4 - 7. Once considered a rural disease, VL has undergone an urbanization process associated with changes in the behavior of the phlebotomine vector, environmental degradation, and the migration of human and canine populations to larger urban centers7.
As in other States in northeastern Brazil, VL is historically endemic inPernambuco State. The disease is widely distributed in the entire State, with records of cases in all geographic regions (i.e., metropolitan region of Recife, Atlantic Forest region, Agreste(Scrub) zone and semiarid region). During the 1990s, there was a great expansion in the geographic distribution of the disease in Pernambuco 8.
The municipality of Petrolina is located in the semiarid region ofPernambuco, where VL is historically endemic. The municipality is experiencing a rapid population increase due to migration waves that result from the process of industrialization and expansion of agriculture. In this context, Cesse et al.9 reported that in the 1990s there was an increase in the number of VL cases and an expansion in the spatial distribution of the disease in Petrolina, with an epidemic peak in 1995. Since then, VL has continuously spread to urbanized areas, in spite of the efforts to control the disease. Therefore, the aim of the present study was to access the current epidemiological situation of VL in Petrolina,from 2007 to 2013, ultimately to identify possible changes in the epidemiological profile of VL patients in this municipality.
MATERIAL AND METHODS
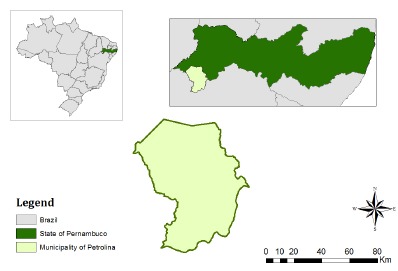
Study area: The municipality of Petrolina (S 9°23'55", W 40°30'03") is located in the semiarid region ofPernambuco, and occupies an area of 4,561.872 km2(Fig. 1). According to the Brazilian Institute of Geography and Statistics (IBGE)10, the municipality has a population of 326,017 inhabitants, most of them living in the urban area of the municipality.
Fig. 1. - Location of the municipality of Petrolina,Pernambuco State, Brazil.
Agriculture is the main economic activity of Petrolina, mostly based on the production of irrigated fruits, especially grapes, mango, banana and guava. The climate is tropical semi-arid, with an average altitude of 376 m. The average annual rainfall is 431.8 mm; the vegetation is composed mainly of a savanna with deciduous forest hyper xerophilic stretches10.
Data source: Retrospective data of human VL confirmed cases recorded in Petrolina from January 2007 to December 2013 were obtained from the Brazilian National Information System for Notifiable Diseases (Sistema de Informação de Agravos de Notificação - SINAN)11, managed by the epidemiological vigilance service of the Municipal Health Department (Secretaria Municipal de Saúde) of Petrolina. The population estimates for each year were provided by the Brazilian Institute of Geography and Statistics (Instituto Brasileiro de Geografia e Estatística - IBGE)10.
Data analysis: Data were obtained from leishmaniasis case report forms and the following variables analyzed were: age, gender, education level, diagnostic methods, co-infection with human immunodeficiency virus (HIV), and case outcome (cure or death). Data were tabulated and analyzed using descriptive statistics. The incidence and lethality rates per 100,000 inhabitants were estimated based on the records of confirmed disease cases and deaths. Incidence rates per 100,000 inhabitants were calculated by year of case report, age group and gender.
Ethical considerations: The study was approved by the Ethics in Human and Animal Studies Committee at the Federal University of the Valley of São Francisco under the protocol number 0002/190213.
RESULTS
From January 2007 to December 2013, a total of 111 cases of VL diagnosed inPetrolina were reported to SINAN, of which 69 were patients residing in this municipality. The remaining cases were patients from surrounding areas and therefore they were excluded from this study. The average number of cases per year in the studied period was 9.9, with the highest annual number of cases (n = 15) being recorded in 2012. The distribution of cases according to the year of reporting is presented in Table 1.
Table 1. Number of cases and coefficient of incidence of human visceral leishmaniasis in Petrolina,Pernambuco, Brazil, between 2007 and 2013.
| Year | Estimated human population | Visceral leishmaniasis cases (n) | Coefficient of incidence (per 100,000 inhabitants) |
|---|---|---|---|
| 2007 | - | 11 | - |
| 2008 | 276,174 | 9 | 3.2 |
| 2009 | 281,851 | 4 | 1.4 |
| 2010 | 293,962 | 11 | 3.7 |
| 2011 | 299,752 | 8 | 2.7 |
| 2012 | 305,352 | 15 | 4.9 |
| 2013 | 319,893 | 11 | 3.4 |
| Total | - | 69 | - |
Most of the 69 patients were males (59.4%) and children under the age of nine (63.8%) (Table 2).
Table 2. Number of cases of visceral leishmaniasis and attributable deaths, according to age and gender in Petrolina,Pernambuco, Brazil, between 2007 and 2013.
| Age groups (years) | Males | Females | Total | Deaths | |||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||||
| <1 | 2 | 4.9 | 2 | 7.1 | 4 | 5.8 | 0 | ||
| 1-4 | 14 | 34.1 | 10 | 35.7 | 24 | 34.8 | 0 | ||
| 5-9 | 8 | 19.5 | 8 | 28.6 | 16 | 23.2 | 0 | ||
| 10-19 | 0 | - | 5 | 17.9 | 5 | 7.2 | 0 | ||
| 20-39 | 10 | 24.4 | 2 | 7.1 | 12 | 17.4 | 1 | ||
| 40-59 | 7 | 17.1 | 1 | 3.6 | 8 | 11.6 | 0 | ||
| > 60 | 0 | - | 0 | - | 0 | - | 0 | ||
| Total | 41 | 59.4 | 28 | 40.6 | 69 | 100 | 1 | ||
Regarding the evolution of the cases, 54 (78.3%) patients progressed to clinical cure and one (1.5%) died; for the remaining patients (n = 14) this information was missing. Cases were confirmed mainly through clinical-epidemiological data (41/69 - 59.4%). Laboratory testing was performed in 28 cases (40.6%). Serological tests were performed in 13 out 69 patients, with six positive results, whereas parasitological examinations were performed in 14, with 12 positive results. In cases that were not subjected to laboratory testing, diagnosis was confirmed based on the therapeutic response (diagnosis ex juvantibus).
Co-infection of Leishmania and the human immunodeficiency virus (HIV) occurred in 14.5% (10/69) of the cases. There was no information regarding co-infection in 43.5% of the analyzed case report forms.
DISCUSSION
This study was based on retrospective data obtained from VL case report forms that are often incomplete, which may impair a deeper analysis of the disease epidemiology in Petrolina. Nonetheless, considering the limited clinical data available in the patient's case report forms and the evident fragilities in terms of laboratory diagnosis confirmation in the primary healthcare units, it may be suggested that VL is an underreported disease in Petrolina, as it is observed in many other endemic areas. Interestingly, an apparent absence of a cyclical pattern of transmission was observed in Petrolina during the study period, when a peak in the number of cases was recorded in 2012. This is in contrast with the pattern observed in Pernambuco State during the same period, in which VL cases peaked in 2008 and 201111.
The human VL case series reported here demonstrates that the disease epidemiology is similar to that observed in other localities in Brazil, affecting mainly children and young males. Indeed, most of the cases were found in children under the age of nine, which is in accordance to data described by Brazuna et al.12, Botelho & Natal13 and Prado et al. 14. This may be related to long-term immunity that was not yet fully developed or to an increased exposure to phlebotomine sand flies. In fact, these data are consistent with previous studies that had pointed to a high incidence of infection, with peri-domestic or even indoor transmission. Indeed, it is recognized that Lutzomyia longipalpis is highly adapted to peri-domestic environments (e.g., chicken coops)15, eventually invading the houses where it may feed on humans and domestic animals such as dogs.
Indeed, the percentages of males and females among patients under the age of 9 were similar (58.5% versus 71.4%), whereas among patients aged 20 to 59 years, the percentage of males (41.5%) was clearly higher (almost 4-fold) than that of females (10.7%). These data suggest that males and females may be similarly exposed to the risk of infection at younger ages, when the transmission may take place inside the houses, whereas adult males may be at a higher risk in comparison with adult females. The higher frequency of VL in males is in accordance with other studies12 , 13 , 14 , 16. This is probably because males are more involved in nighttime outdoor activities (including outdoor resting/sleeping) and therefore they are more exposed to phlebotomine sand fly bites.
Most of the cases reported herein were diagnosed based on clinical-epidemiological data (59.4%). Alvarenga et al.16 reported that laboratory confirmation was possible in 89.5% of the 76 VL patients referred to the Infectology Clinic of the Campo GrandeUniversity Hospital Center, Mato Grosso do Sul, from 2000 to 2005. Direct examination looking for parasites was also the most frequently used method to confirm the diagnosis in the study of Brazuna et al.12 and Botelho & Natal13 with 76.8% and 80%, respectively. Laboratory testing was available only for the minority of the cases analyzed herein, which is an issue that should be prioritized by local public health authorities.
The presence of co-infection with HIV was observed in 14.5% of the patients, a higher percentage than that found by Botelho & Natal13 and Brazuna et al.12, who reported 5% and 7.1%, respectively. It is noteworthy that 43.5% of the case report forms had no information regarding HIV infection. Therefore, this is a variable that may be underestimated by the incomplete anamnesis during the clinical examination of patients. Certainly, this information is of paramount importance since co-infection with HIV may influence the outcome of cases.
In conclusion, even considering the inherent limitations of using secondary data, the results of this study have clearly demonstrated that VL transmission still occurs in Petrolina at moderate to high levels, affecting mainly young children. This indicates that control measures in Petrolina are not effectively reducing the incidence of human cases, as well as it may reflect a limited access of patients to primary healthcare units (e.g., diagnostic tests), impairing early diagnosis and treatment. Therefore, local public health authorities should improve the access to in-clinic diagnostic tests and emphasize the importance of early diagnosis and treatment of human patients.
REFERENCES
- 1.Alvar J, Vélez ID, Bern C, Herrero M, Desjeux P, Cano J. Leishmaniasis worldwide and global estimates of its incidence. PLoS ONE. 2012;7:e35671. doi: 10.1371/journal.pone.0035671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . Programme for the surveillance and control of leishmaniasis. 2004. [2014 Nov 17]. http://www.who.int/emc/diseases/leish/index.html [Google Scholar]
- 3.Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Departamento de Vigilância Epidemiológica. Manual de vigilância e controle da leishmaniose visceral. Brasília: Ed. Ministério da Saúde; 2006. [Google Scholar]
- 4.Barreto ML, Teixeira MG, Bastos FI, Ximenes RAA, Barata RB, Rodrigues LC. Sucessos e fracassos no controle de doenças infecciosas no Brasil: o contexto social e ambiental, políticas, intervenções e necessidades de pesquisa. Lancet. 2011;(Série:Saúde no Brasil 3):47–Saúde no Brasil 3):60. [Google Scholar]
- 5.Costa CHN. Characterization and speculations on the urbanization of visceral leishmaniasis in Brazil. Cad Saúde Publica. 2008;24:2959–2963. doi: 10.1590/s0102-311x2008001200027. [DOI] [PubMed] [Google Scholar]
- 6.Oliveira CDL, Morais MHF, Machado-Coelho GLL. Visceral leishmaniasis in large Brazilian cities: challenges for control. Cad. 2008;24:2953–2958. doi: 10.1590/s0102-311x2008001200026. [DOI] [PubMed] [Google Scholar]
- 7.Werneck GL. Forum: geographic spread and urbanization of visceral leishmaniasis in Brazil. Introduction. 2008;24:2937–2940. doi: 10.1590/s0102-311x2008001200023. [DOI] [PubMed] [Google Scholar]
- 8.Dantas-Torres F. Situação atual da epidemiologia da leishmaniose visceral em Pernambuco. Rev Saúde Pública. 2006;40:537–541. doi: 10.1590/s0034-89102006000300024. [DOI] [PubMed] [Google Scholar]
- 9.Cesse EAP, Carvalho EF, Andrade PP, Ramalho WM, Luna L. Organização do espaço urbano e expansão do calazar. Rev Bras Saúde Matern Infant. 2001;1:167–176. [Google Scholar]
- 10.Instituto Brasileiro de Geografia e Estatística [2015 July 17];Estimativas da população residente com data de referência 1 de julho de 2014 publicada no Diário Oficial da União em 28/08/2014. 2014 http://www.cidades.ibge.gov.br/xtras/perfil.php?lang=&codmun=2611101 Internet.
- 11.Sistema de Informação de Agravos de Notificação . SINAN. 2015. http://dtr2004.saude.gov.br/sinanweb/ [Google Scholar]
- 12.Brazuna JCM, Silva EA, Brazuna JM, Domingos IH, Chaves N, Honer MR. Profile and geographic distribution of reported cases of visceral leishmaniasis in Campo Grande, State of Mato Grosso do Sul, Brazil, from 2002 to 2009. Rev Soc Bras Med Trop. 2012;45:601–606. doi: 10.1590/s0037-86822012000500012. [DOI] [PubMed] [Google Scholar]
- 13.Botelho ACA, Natal D. Primeira descrição epidemiológica da leishmaniose visceral em Campo Grande, Estado de Mato Grosso do Sul. Rev Soc Bras Med Trop. 2009;42:503–508. doi: 10.1590/s0037-86822009000500006. [DOI] [PubMed] [Google Scholar]
- 14.Prado PF, Rocha MF, Sousa JF, Caldeira DI, Paz GF, Dias ES. Epidemiological aspects of human and canine visceral leishmaniasis in Montes Claros, State of Minas Gerais, Brazil, between 2007 and 2009. Rev Soc Bras Med Trop. 2011;44:561–566. doi: 10.1590/s0037-86822011000500006. [DOI] [PubMed] [Google Scholar]
- 15.Costa PL, Dantas-Torres F, Silva FJ, Guimarães VCFV, Gaudêncio K, Brandão-Filho SP. Ecology of Lutzomyia longipalpis in an area of visceral leishmaniasis transmission in north-eastern Brazil. Acta Trop. 2013;126:99–102. doi: 10.1016/j.actatropica.2013.01.011. [DOI] [PubMed] [Google Scholar]
- 16.Alvarenga DG, Escalda PMF, Costa ASV, Monreal MTF. Leishmaniose visceral: estudo retrospectivo de fatores associados à letalidade. Rev Soc Bras Med Trop. 2010;43:194–197. doi: 10.1590/s0037-86822010000200017. [DOI] [PubMed] [Google Scholar]


