Abstract
To meet the mental health needs of infants from high-risk families, we examined the effect of a brief home-based adaptation of Parent-Child Interaction Therapy (PCIT) on improvements in infant and parent behaviors and reductions in parenting stress. Participants included 60 infants (55% male; average age of 13.5 ± 1.31 months) who were recruited at a large urban primary care clinic and were included if their scores exceeded the 75th percentile on a brief screener of early behavior problems. Most infants were from an ethnic or racial minority background (98%) and lived below the poverty line (60%). Families were randomly assigned to receive the home-based parenting intervention or standard pediatric primary care. Observational and parent-report measures of infant and parenting behaviors were examined at pre- and post-intervention and at 3- and 6-month follow-ups. Infants receiving the intervention were more compliant with maternal commands at the 6-month follow-up and displayed lower levels of externalizing and internalizing behavior problems across post and follow-up assessments compared to infants in standard care. Mothers receiving the intervention displayed a significantly higher proportion of positive and lower proportion of negative behaviors with their infant during play compared to mothers in the standard care group. There were no significant group differences for parenting stress. Results provide initial evidence for the efficacy of this brief and home-based adaptation of PCIT for infants. These findings highlight the benefit of identification and intervention as early as possible to promote mental health for infants from high-risk families.
Keywords: infancy, behavior problems, parent training, early intervention, risk
Early childhood behavior problems are the most common referral reason at mental health clinics serving young children (Keenan & Wakschlag, 2000; Thomas & Guskin, 2001) and occur in as many as 15% of young children (Carter, Briggs-Gowan, & Davis, 2004). Persistence of early externalizing behavior problems predicts a negative trajectory for more severe school-age conduct problems (Shaw, Gilliom, Ingoldsby, & Nagin, 2003), greater increases in concurrent and subsequent internalizing problems (Gilliom & Shaw, 2004), later difficulties in academic functioning and peer victimization (van Lier et al., 2012), and increased risk for more severe adult psychopathology (Moffitt, Caspi, Harrington, & Milne, 2002). In addition to the high prevalence and poor prognosis, the economic costs of health and educational services use and family burden (e.g., time spent on household tasks) were reportedly high for children with severe behavior problems and not different between younger compared to older children (Romeo, Knapp, & Scott, 2006), highlighting the significant public health need for effective treatment in early childhood.
Behavioral parent-training interventions, such as Parent-Child Interaction Therapy (PCIT; Zisser & Eyberg, 2010), Incredible Years (Webster-Stratton & Reid, 2010), Helping the Noncompliant Child (McMahon & Forehand, 2003), and Triple P (Sanders, Cann, & Markie-Dadds, 2003), represent a front-line approach for the treatment of early externalizing behavior problems given their documented efficacy based on studies conducted over the past 40 years (Eyberg, Nelson, & Boggs, 2008). However, families with the greatest need have been shown in these studies on parent-training interventions to benefit least (Lundahl, Risser, & Lovejoy, 2006; Reyno & McGrath, 2006; Webster-Stratton & Hammond, 1990). Specifically, rates of behavior problems are twice as high among young children from economically disadvantaged and underrepresented ethnic and racial minority families (Qi & Kaiser, 2003), but these families have disproportionately lower session attendance and higher dropout rates (Bagner & Graziano, 2013; Lavigne et al., 2010) and report several barriers to treatment participation, including required commitment to a high number of treatment sessions (Heinrichs, Bertram, Kuschel, & Hahlweg, 2005) and lack of transportation (Boggs et al., 2004). Therefore, in order to broaden the reach to high-risk families, it is essential to adapt behavioral parent-training interventions to be brief and more accessible (e.g., home-based).
Identifying behavior problems in infancy before they become more severe and entrenched would likely require less intensive and shorter interventions (Bakermans-Kranenburg, Van Ijzendoorn, & Juffer, 2003), thus decreasing burden for high-risk families. Patterson’s coercion model, a theoretical underpinning of behavioral parent training, suggests behavior problems are established and maintained in infancy by early parenting behavior (Patterson, 2002). Pathways leading to conduct problems begin in infancy and are associated with multiple psychosocial risk factors (Aguilar, Sroufe, Egeland, & Carlson, 2000; Shaw, Keenan, & Vondra, 1994; Shaw, Owens, Giovannelli, & Winslow, 2001), including poverty and negative parenting practices (Linver, Brooks-Gunn, & Kohen, 2002), highlighting the importance of intervening with infants from high-risk families.
By 12 months of age, behavior problems can be reliably assessed (Carter & Briggs-Gowan, 2006) and remain stable over the following year (Briggs-Gowan, Carter, Bosson-Heenan, Guyer, & Horwitz, 2006; van Zeijl, Mesman, Stolk et al., 2006). Therefore, the transition into the second year of life (i.e., 12 to 15 months) represents an ideal opportunity to intervene as parents begin to face challenges with their infant’s increased mobility and desire to exert independence but before problems become entrenched and develop into reliable diagnoses by 2 years (Egger & Angold, 2006) and into the preschool years (Keenan & Wakschlag, 2002). Promising work has been conducted with toddlers as young as 18 months (Bagner, Sheinkopf, Vohr, & Lester, 2010; Dombrowski, Timmer, Blacker, & Urquiza, 2005; Gross et al., 2003; Kohlhoff & Morgan, 2014), but parent-training interventions have not been examined in infancy during the transition into the second year of life.
A thorough review of infant programs yielded limited evidence for efficacy (Olds, Sadler, & Kitzman, 2007), with most interventions involving numerous sessions over the course of several years, including a broad focus, and leading to minimal behavioral improvements. The program with the most empirical support is the Nurse-Family Partnership, where nurses visit low-income mothers during pregnancy and the subsequent 2 years (Olds, 2002). However, its broad and long-term focus (32 to 33 visits) is expensive and time consuming, and effects on behavior problems were not significant (Olds et al., 2004). In contrast to comprehensive programs, the Family Check-Up is a brief intervention, which has led to significant decreases in toddler behavior problems and improvements in parenting (Shaw, Dishion, Supplee, Gardner, & Arnds, 2006). The Family Check-Up involves the use of motivational interviewing procedures (e.g., use of data collected during an assessment when providing feedback to parents) across three sessions to promote change in parenting practices and may include additional sessions based on the family’s needs (Dishion & Stormshak, 2007). However, the Family Check-Up does not include active coaching of parents interacting with their child, an approach that produced large effects on child behavior (Kaminski, Valle, Filene, & Boyle, 2008). Furthermore, active coaching provides an optimal fit for infants when behavior problems may not be obvious to parents, and therapists can help parents identify and respond appropriately to these behaviors.
The purpose of the current study was to evaluate an adaptation of PCIT, the Infant Behavior Program, which was designed for infants from low-income families by being brief and home-based. Similar to standard PCIT, the adaptation involves actively coaching parents to follow their infant’s lead in play in an effort to decrease disruptive (e.g., hitting) and increase prosocial (e.g., gentle touch) behaviors. An open trial provided promising findings on the feasibility and initial outcome of infant and parent behavior (Bagner, Rodríguez, Blake, & Rosa-Olivares, 2013). In the current randomized controlled trial, we hypothesized that relative to infants receiving standard pediatric primary care, infants receiving the home-based intervention would demonstrate higher levels of observed infant compliance to parental commands at a 6-month follow-up and decreases in infant behavior problems across an 8-month period (baseline, post-intervention, and 3- and 6-month follow-ups). Additionally, we expected that relative to parents in standard care, parents receiving the intervention would display increases in positive and decreases in negative observed behaviors during play with their infant, as well as decreases in parenting stress from baseline across the 8-month period.
Method
Participants
Participants were 60 mothers and their 12- to 15-month-old infant, who were recruited at a large hospital-based pediatric primary care clinic providing comprehensive, coordinated, and family-centered care to underserved families. Infants were 55% male, with an average age of 13.5 months old (SD = 1.31). On a demographic questionnaire, most mothers identified themselves (95%) and their infant (98%) as being from an ethnic or racial minority group. Specifically, 90% of mothers reported a Hispanic ethnicity and the following racial breakdown: 80% White, 10% Black, 2% Asian, 2% Bi-racial, and 6% other. For their infant, 93% of mothers reported a Hispanic ethnicity and the following racial breakdown: 80% White, 5% Black, 2% Asian, 2% Native American, 5% Bi-racial, and 6% other. A majority of families (60%) had incomes below the poverty line, and the median annual income for all families was $18,513.
For study inclusion, the primary caregiver, who was the mother in all cases, was required to rate their infant above the 75th percentile on the problem scale of the Brief Infant-Toddler Social and Emotional Assessment (Carter & Briggs-Gowan, 2006), a screener of infant behavior problems, and speak and understand either English or Spanish. Bilingual mothers were asked to choose their language preference based on their comfort level, and 57% of mothers chose to complete the screening and subsequent assessments in Spanish. To ensure ability to learn intervention skills, the mother was required to receive an estimated IQ score ≥ 70 on the two-subtest (vocabulary and matrix reasoning) version of the Wechsler Abbreviated Scale of Intelligence (Wechsler, 1999) for those speaking English or an average standard score ≥ 4 on the vocabulary and matrix reasoning subtests of the Escala de Inteligencia Wechsler Para Adultos – Third Edition (Pons, Flores-Pabón et al., 2008) for those choosing to complete the screening and assessment in Spanish. Major infant sensory impairments (e.g., deafness, blindness) or motor impairments that significantly impair mobility, as well as current child protection services involvement, were exclusion criteria, although no families were excluded based on these criteria.
Procedure
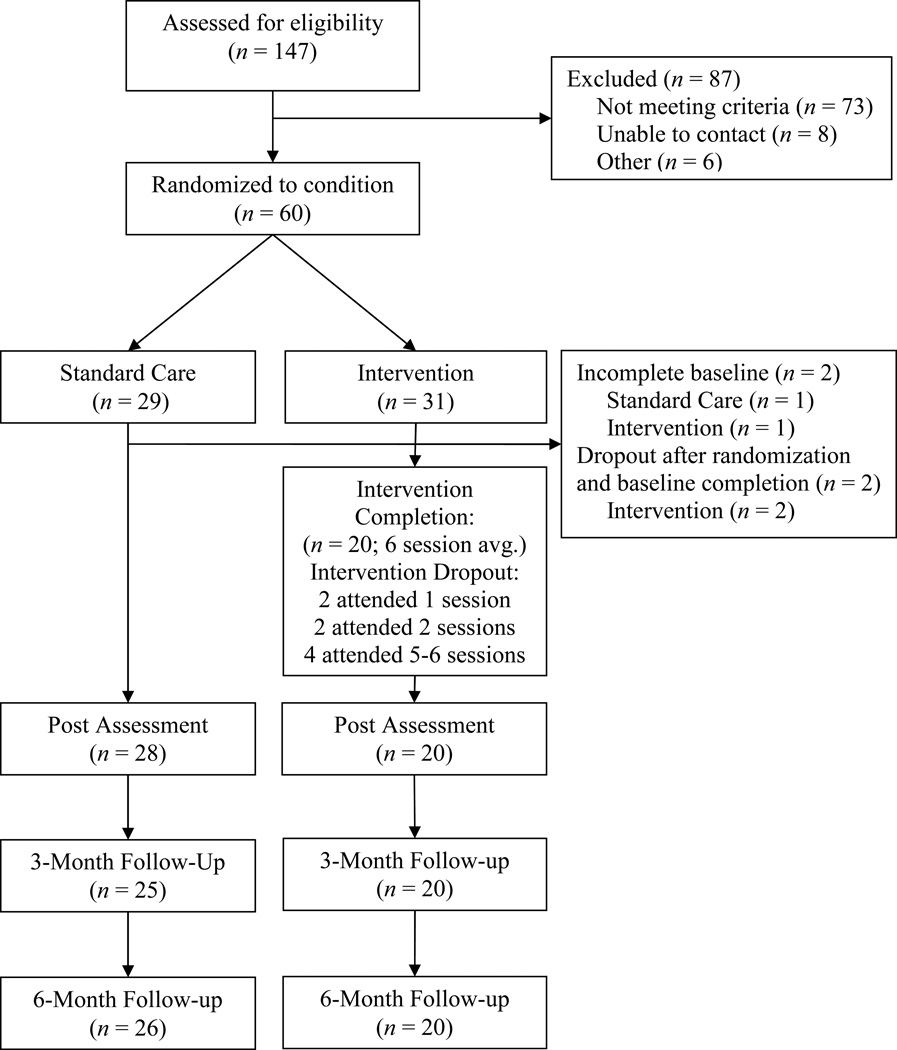
This study was a randomized controlled trial with repeated outcome measures at baseline and post and at 3- and 6-month follow-ups. Between 2011 and 2013, research staff approached families during well or sick visits for their infant between 12 and 15 months and obtained informed consent (approved by the University and Hospital Institutional Review Boards) before the screening. Of the 147 families participating in the screening, a total of 60 families (41%) met study criteria (see Figure 1) and were enrolled and randomized (using a computer-generated random numbers list) to the intervention (n = 31) or standard care (n = 29). The groups did not differ on any demographic characteristics (see Table 1). Data were collected from the primary caregiver, who was the biological mother in all cases, although other caregivers were encouraged to participate in the intervention (described in detail below). Families completed a baseline assessment in their home and were then informed of their group status at that time. Independent assessors masked to group status conducted a post (n = 48; 80% retention) assessment 2 months after the baseline and follow-up (n = 46; 77% retention) assessments 3 and 6 months after the post assessment. Families received $50 for participation in each assessment.
Figure 1. Participant flow through trial.
Table 1.
Participant Baseline Demographic Variables, by Initial Intervention Assignment
| Total Sample (n = 60) |
Intervention group (n = 31) |
Standard Care group (n = 29) |
|||||
|---|---|---|---|---|---|---|---|
| % | n | % | n | % | n | p value | |
| Child sex (male) | 55 | 33 | 58 | 18 | 52 | 15 | .622 |
| Child minority status | 98 | 59 | 97 | 30 | 100 | 29 | .697 |
| Mother minority status | 95 | 57 | 94 | 29 | 97 | 28 | .536 |
| Mother English speaking (vs. Spanish) | 43 | 26 | 55 | 17 | 31 | 9 | .074 |
| High school graduate or less | 70 | 42 | 65 | 20 | 76 | 22 | .338 |
| Below poverty line* | 60 | 35 | 58 | 18 | 63 | 17 | .704 |
| Mean | SD | Mean | SD | Mean | SD | p value | |
| Child age (months) | 13.47 | 1.31 | 13.71 | 1.40 | 13.21 | 1.18 | .138 |
| Mother age (years) | 29.57 | 5.49 | 30.03 | 5.50 | 29.07 | 5.54 | .502 |
| Mother IQ T-Score** | 46.35 | 12.55 | 47.21 | 12.17 | 45.43 | 13.09 | .588 |
| ASQ Communication | 35.85 | 17.24 | 34.50 | 17.24 | 34.35 | 17.74 | .493 |
| BITSEA Problem score | 20.15 | 8.10 | 22.02 | 9.22 | 18.35 | 6.55 | .076 |
Note: ASQ = Ages and Stages Questionnaire; BITSEA = Brief Infant-Toddler Social-Emotional Assessment.
Two mothers did not report income, and both were in the standard care group.
T-Scores are combined between the WASI and EIWA-III Vocabulary and Matrix Reasoning subtests;
Screening Measures
Brief Infant-Toddler Social and Emotional Assessment (BITSEA; Carter & Briggs-Gowan, 2006)
The BITSEA is a 42-item, nationally-standardized screener designed to assess behavioral problems and competencies in 12- to 36-month-olds. The 31-item problem scale has excellent test-retest reliability (r = .91 to .92) and very good inter-rater reliability (r = .70 to .78; Carter & Briggs-Gowan, 2006), as well as support for discriminative validity yielding excellent sensitivity and good specificity for those scoring above the clinical cutoff of the 75th percentile (Briggs-Gowan, Carter, Irwin, Wachtel, & Cicchetti, 2004). Examples of items on the problem scale include “restless and can’t sit still,” “is destructive,” and “hits, bites or kicks” and are rated on a scale of 0 (not true/rarely), 1 (somewhat true/sometimes), or 2 (very true/often). Cronbach’s alpha for the problem scale in the current sample was .77. The BITSEA was administered at the screening, and infants scoring above the 75th percentile on the BITSEA problem scale based on their age and sex were included in the study.
Wechsler Abbreviated Scale of Intelligence (WASI; Wechsler, 1999) and Escala de Inteligencia Wechsler Para Adultos – Third Edition (EIWA-III; Pons, Flores-Pabón et al., 2008)
The WASI is a brief measure of intelligence with high reliability and validity (Hays, Reas, & Shaw, 2002), and the EIWA-III is the Spanish version of the full Wechsler Scale of Intelligence (Wechsler, 1997) with demonstrated reliability (Pons, Flores-Pabón et al., 2008) and validity (Pons, Matías-Carrelo et al., 2008). The vocabulary and matrix reasoning subtests were administered, and mothers were required to receive an estimated IQ score ≥ 70 on the two-subtest version of the WASI or an average standard score ≥ 4 on the EIWA-III subtests, although no mothers were excluded based on this criterion.
Outcome Measures
Infant-Toddler Social and Emotional Assessment (ITSEA; Carter & Briggs-Gowan, 2006)
The ITSEA is a 166-item, nationally-standardized questionnaire designed to assess behavioral problems in 12- to 36-month-olds with excellent test-retest reliability (r = .85 to .91) and very good inter-rater reliability (r = .70 to .76; Carter & Briggs-Gowan, 2006), including support for high persistence of elevated behavior problems with the youngest age group of 12 to 23 months (Briggs-Gowan et al., 2006). We examined ITSEA scores on the externalizing and internalizing domains as outcome measures of infant behavior problems at all assessments. However, for approximately one-quarter of infants (22 to 29% at each assessment), the items on the peer aggression subscale were not applicable and thus not scored due to the infant’s limited contact with other children (aggression toward siblings is not included in this subscale). The peer aggression subscale is one of three subscales within the broader externalizing domain, so individual subscales were weighted differentially for the externalizing domain across infants with and without scores on the peer aggression subscale. Therefore, we reported scores on the other two subscales – activity/impulsivity (6 items, α = .22) and aggression/defiance (12 items, α = .77) – instead of the broader externalizing domain, as well as the 30-item internalizing scale (α = .69). Additionally, baseline scores on the compliance subscale (8 items, α = .59) were used as a covariate when examining group differences in observed infant compliance at the 6-month follow-up.
Dyadic Parent-Child Interaction Coding System-Third Edition (DPICS-III; Eyberg, Nelson, Duke, & Boggs, 2005)
The DPICS-III is a behavioral coding system with documented reliability and validity (Eyberg et al., 2005) that was used to assess observed parent and infant behaviors. Specifically, we coded mother do skills (i.e., praises, behavior descriptions, and reflections) and don’t skills (i.e., questions, commands, and negative talk) at all assessments to reflect positive and negative parent behaviors used during infant-led play. The proportion of each skill was calculated to account for total parent verbalizations (including neutral talk, which is not considered a do or a don’t skill). Specifically, the percent of do skills was equal to the number of do skills divided by the total number of parent verbalizations, and the percent of don’t skills was equal to the number of don’t skills divided by the total number of parent verbalizations. Infant compliance, defined as the number of times the infant complied to maternal commands divided by the total number of maternal commands (with an opportunity to comply), was coded during a clean-up situation at the 6-month follow-up assessment. Consistent with previous research (Shaw et al., 1994), the clean-up situation was only administered at the 6-month follow-up assessment when all infants were at least 18-months-old to ensure the task was developmentally appropriate. Coders masked to group status were trained to 80% agreement with a criterion tape and coded half the observations at baseline a second time for reliability, yielding an excellent overall kappa (.84) for all codes examined in the current study.
Parenting Stress Index, Fourth Edition, Short Form (PSI-SF; Abidin, 1995)
The PSI-SF is a 36-item self-report instrument for parents of children ages 1 month to 12 years containing three subscales (parent distress, parent-child dysfunctional interaction, difficult child) and a total scale with good reliability and validity (Abidin, 1995). Additionally, strong psychometric properties of the PSI-SF have been demonstrated among low-income parents of toddlers and preschoolers (Reitman, Currier, & Stickle, 2002; Whiteside-Mansell et al., 2007). We examined the PSI-SF total scale as an index of overall parenting stress, and Cronbach’s alpha for the total scale in the current sample was .89.
Intervention
The Infant Behavior Program is a home-based adaptation of the Child-Directed Interaction (CDI) phase of PCIT, an evidence-based intervention for preschool behavior problems (Nixon, Sweeney, Erickson, & Touyz, 2003; Schuhmann, Foote, Eyberg, Boggs, & Algina, 1998). Consistent with recommendations to adapt interventions for new populations (Eyberg, 2005), we maintained the core features of PCIT while addressing the unique developmental needs of infants. Similar to standard PCIT, in the first teach session, the therapist taught the parent(s) to follow their infant’s lead in play by decreasing don’t skills (i.e., commands, questions, and negative statements) and increasing do skills (i.e., PRIDE: Praising the infant, Reflecting the infant’s speech, Imitating the infant’s play, Describing the infant's behavior, and expressing Enjoyment in the play). Parents were taught to direct the PRIDE skills to their infant’s appropriate play and ignore disruptive behaviors (e.g., hitting, whining). Following the teach session, parent skills were assessed during a 5-minute observation at the start of each coach session, and data collected were used by the therapist to coach the parent(s) in their use of the skills. In addition to standard coaching practices, therapists incorporated strategies relevant for infants. For example, given lower receptive language abilities in infants, parents were encouraged to use non-verbal praise (e.g., clapping) along with verbal praise to enhance reinforcement for appropriate behaviors. Furthermore, consistent with research on PCIT for children with developmental delay (Bagner & Eyberg, 2007), parents were encouraged to repeat appropriate infant vocalizations.
Intervention Format
Sessions were conducted weekly with each family in their home and lasted approximately 1 to 1.5 hours. The therapists were all doctoral students in clinical psychology and trained by the first author, who is a PCIT Master Trainer. In each session, the therapist problem-solved with each family ways to optimize in-home coaching, such as choosing an appropriate location for the session and developing ways to minimize distractions (e.g., turning off the television). Parents were instructed to practice the skills described above for 5 minutes each day with their infant and were asked to complete weekly logs to document frequency of practice. Of the 28 families attending the first session, eight (29%) dropped out before completing the intervention, which is consistent with dropout rates in standard PCIT (e.g., 36%; Eyberg, Boggs, & Jaccard, 2014) and is relatively low given the high-risk nature of the current sample.
On average, families completed the intervention in 6.1 sessions (range from five to seven sessions), which included the initial teach session. Given findings that a time-limited, 14-session PCIT (which included an average of 6.5 CDI and 5.6 PDI sessions) fared as well as, and in some cases better than, variable PCIT wherein mastery criteria was required (Thomas & Zimmer-Gembeck, 2012), we capped the intervention at seven sessions (including the teach session) and did not require the primary caregiver to meet mastery criteria to complete the intervention. However, 45% of families completed the intervention in less than seven sessions (range of five to six sessions) because the primary caregiver met mastery criteria, which included the do skills (i.e., 10 labeled praises, 10 behavior descriptions, and 10 reflections or reflected 75% of the infant’s speech, consistent with previous work with children with developmental delay; Bagner & Eyberg, 2007) and the don’t skills (i.e., less than 3 questions, commands, and criticisms) during a 5-minute infant-led play. Of all the intervention completers, 65% of families met mastery criteria for both do and don’t skills at their final graduation session, and 90% of families met criteria for either do or don’t skills. Families not completing the intervention dropped out after completing an average of 3.1 sessions, and no dropout family met mastery criteria.
Intervention Fidelity
All sessions were videotaped, and 63% of sessions were randomly selected and coded. Average fidelity across sessions, defined as the percent with which the therapist adhered to key elements of each session detailed in the manual, was 97%. Of the coded tapes, 40% were randomly selected and coded a second time for reliability and yielded an interobserver reliability estimate of 95%.
Statistical Analysis
Mixed-effects regression models were used to analyze most longitudinal outcomes to examine individual change in an outcome as a function of continuous time, as well as examine group as a predictor of change (Hedeker & Gibbons, 2006). We considered time as a continuous predictor during this period of rapid developmental change. For continuous variables (ITSEA, PSI-SF), linear mixed models were used; for proportions (do and don’t skills), generalized linear (logistic) mixed models were used. For all models, the square root of months since baseline visit was used as the time predictor to linearize the relationship between time and outcomes (Cohen, Cohen, West, & Aiken, 2013). Each outcome variable was assessed using a separate mixedeffects model. For each model, the effects of time, intervention group, and the time by group interaction were included. For infant compliance, measured only at the 6-month follow-up, a logistic regression analysis of covariance (ANCOVA) model was used to examine infant compliance as an outcome variable. This model included a baseline outcome value for infant compliance (parent report on the ITSEA compliance subscale), intervention group, and the baseline by group interaction. All analyses were conducted in SPSS version 20.
Results
Missing values analysis
Fifty-eight families completed at least the baseline assessment and were included in the subsequent analyses (30 families in the intervention group and 28 families in standard care); the remaining two families completed only the screening and therefore had insufficient data (i.e., the BITSEA for the infant and the WASI for the mother), neither of which was included in subsequent analyses. There were no significant differences on any demographic or outcome measures between families completing all assessment waves and families not completing all assessment waves. Missing value analysis showed that missingness on outcome variables at later waves was related to intervention group membership and to values of previous waves of the same variable; both group membership and previous waves of the outcome variable were included in all models. This pattern of missingness is consistent with the missing at random (MAR; Rubin, 1976) definition and is common in longitudinal studies. The mixed-effects regression models used in the current study were estimated with maximum likelihood (ML) estimation; they create estimates using all available observations for each participant and provide unbiased parameter estimates when missing values are missing at random (Schafer & Graham, 2002).
Covariate selection
We evaluated all demographic variables shown in Table 1 as potential covariates. Any variable that significantly correlated with an outcome variable at baseline or 6-month follow-up was considered a covariate. As such, mother age, education, ethnicity, and language were included as covariates. Mother age and education were centered at their mean values, whereas mother language and ethnicity were binary and were not centered.
Infant and Parent Outcomes
Unadjusted means and associated group slopes and the group by time interaction for all infant and parent outcomes are displayed in Table 2. There were no baseline differences in any outcomes. Standardized mean difference effect sizes (i.e., Cohen’s ds) were calculated for significant interaction effects described in Feingold (2009) using the model-implied estimated means. In all cases, the effect size was calculated as the difference between the model-implied mean for the control group at the 6-month follow-up and the model-implied mean for the intervention group at the 6-month follow-up, divided by the baseline standard deviation of the measure. For observed compliance, infants in the intervention group were significantly more compliant to maternal commands compared to infants in the control group at the 6-month follow-up (d = .54); infants in the intervention group had a mean compliance rate slightly more than one-half of a standard deviation higher than that of the control group. Maternal report of aggression/defiance and internalizing problems on the ITSEA had significant group by time interaction terms (ds between groups at the 6-month follow-up were .51 and .74, respectively); infants in the intervention group had an aggression mean one-half of a standard deviation below that of the control group and an internalizing score three-quarters of a standard deviation below that of the control group. Specifically, maternal report of aggression/defiance significantly increased over time for the standard care group and did not change for the intervention group. Furthermore, maternal report of activity/impulsivity decreased over time for the intervention group and did not change for the standard care group, although the group by time interaction was not significant.
Table 2.
Unadjusted outcome means (SD) for intervention and standard care groups at each assessment and results of mixed models
| Baseline | Post | 3-month FU | 6-month FU | Slopes | Group by Time Interaction |
||
|---|---|---|---|---|---|---|---|
| Infant Outcomes | |||||||
| Observed Compliance a | Intervention | N/A | N/A | N/A | 0.51 (0.43) | 4.119 | −5.215* |
| Standard Care | N/A | N/A | N/A | 0.33 (0.24) | −1.096 | ||
| ITSEA Activity/Impulsivity | Intervention | 1.22 (0.32) | 1.03 (0.41) | 1.10 (0.51) | 1.05 (0.37) | −0.053* | 0.032 |
| Standard Care | 1.24 (0.32) | 1.19 (0.31) | 1.27 (0.32) | 1.15 (0.36) | −0.021 | ||
| ITSEA Aggression/Defiance | Intervention | 0.81 (0.35) | 0.77 (0.37) | 0.74 (0.30) | 0.84 (0.42) | −0.011 | 0.068* |
| Standard Care | 0.77 (0.45) | 0.88 (0.44) | 0.91 (0.48) | 0.88 (0.47) | 0.057** | ||
| ITSEA Internalizing | Intervention | 0.60 (0.25) | 0.60 (0.30) | 0.56 (0.28) | 0.57 (0.27) | −0.029 | 0.045* |
| Standard Care | 0.60 (0.23) | 0.67 (0.25) | 0.64 (0.29) | 0.64 (0.27) | 0.016 | ||
| Parent Outcomes | |||||||
| Observed Percent Do Skills b | Intervention | 0.15 (0.23) | 0.35 (0.20) | 0.27 (0.17) | 0.35 (0.23) | 0.451** | −0.403* |
| Standard Care | 0.09 (0.09) | 0.12 (0.11) | 0.10 (0.14) | 0.13 (0.14) | 0.047 | ||
| Observed Percent Don’t Skills b | Intervention | 0.53 (0.21) | 0.22 (0.23) | 0.18 (0.19) | 0.19 (0.18) | −0.869*** | 0.532* |
| Standard Care | 0.63 (0.20) | 0.52 (0.25) | 0.58 (0.26) | 0.48 (0.29) | −0.338* | ||
| PSI-SF Total | Intervention | 77.77 (18.13) | 80.60 (15.14) | 76.70 (16.30) | 80.00 (23.45) | −0.099 | −1.801 |
| Standard Care | 83.54 (16.71) | 79.89 (16.21) | 76.64 (14.81) | 78.88 (11.56) | −1.900 | ||
Note: FU = Follow-up; ITSEA = Infant-Toddler Social Emotional Assessment; PSI-SF = Parenting Stress Index – Short Form; all models include mother language, age, ethnicity and education as covariates; slopes reflect change in outcome per month.
p < .05;
p < .01;
p < .001
Logistic ANCOVA with baseline (ITSEA compliance), group, and baseline by group interaction; slopes reflect relationship between baseline measure and outcome.
Logistic mixed model; slopes reflect change in logit of outcome per month.
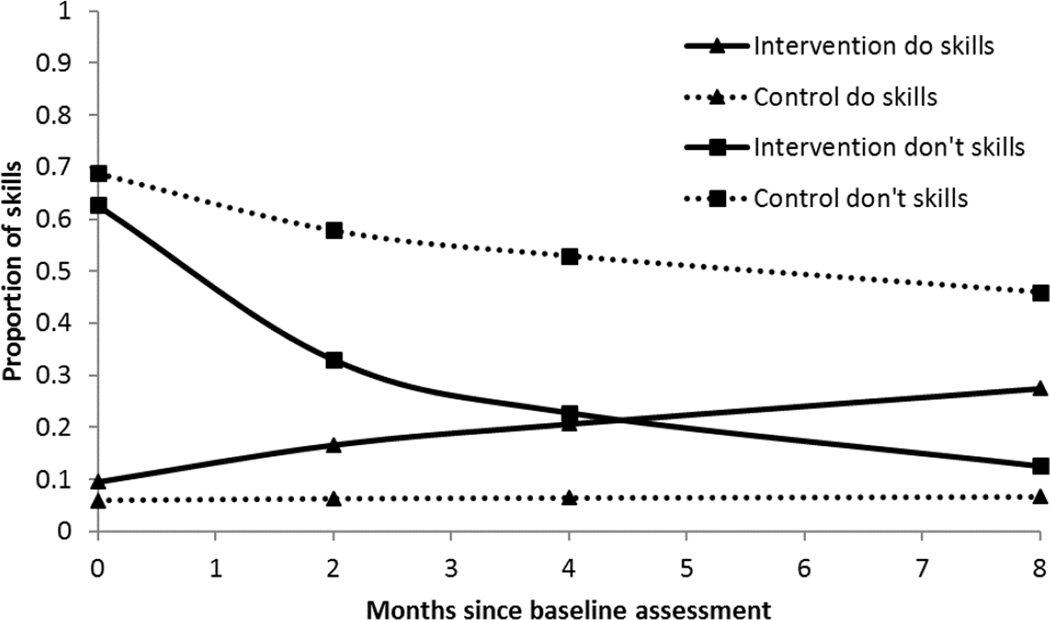
Observed maternal do and don’t skills had a significant group by time interaction term (odds ratio at the 6-month follow-up of 5.24 and 5.29, respectively, in the expected direction), suggesting change over time was significantly different for the intervention and standard care groups. As illustrated in Figure 2, maternal do skills significantly increased over time for the intervention group but did not significantly change over time for the standard care group, whereas maternal don’t skills significantly decreased for both groups with a steeper decrease for the intervention group. At the 6-month follow-up, mothers in the intervention group were 5 times more likely to display do skills and 5 times less likely to display don’t skills, compared to the control group. No significant group by time interaction or significant change within group was observed for parenting stress.
Figure 2. Predicted values for intervention and standard care groups for parenting skills.
The intervention group shows a significant increase in maternal do skills over time (b = 0.451, p < .01, whereas the control group shows a nonsignificant change in do skills over time (b = 0.047, NS). Significant interaction of group and time (b = −0.403, p < .05) indicates that the intervention group slope is significant different from the control group slope. Intervention and control groups both show significant decreases in maternal don’t skills over time (b = −0.869, p < .001; b = 0.338, p < .05); however the significant group by time interaction (b = 0.532, p < .05) suggests that the intervention group shows a steeper decrease in don’t skills than the control group. These are predicted values controlling for mother age, education, language, and ethnicity.
Discussion
Families of infants receiving a brief home-based parent-training intervention displayed significant improvements in infant behavior relative to families randomly assigned to receive standard pediatric primary care. Infants receiving the intervention were significantly more compliant to maternal commands during cleanup at the 6-month follow-up than infants in standard care. Although increased child compliance has been demonstrated in parent-training interventions for older children (Eyberg et al., 2008), it is remarkable we found a significant difference on infant compliance with a medium effect size when only targeting improvements in the parent-infant interaction and not teaching parents explicitly how to improve infant compliance (e.g., time out for noncompliance).
Similar to observed infant behavior, the intervention demonstrated a significant effect on parent-reported levels of infant aggression and defiance and overall internalizing problems, both of which yielded medium effect sizes. Given typical increases in aggression (Alink et al., 2006) and internalizing problems (Cote et al., 2009) in early childhood, the current findings suggest the intervention had a preventive effect on aggressive and internalizing behavior problems. With regard to clinical significance, more infants in the intervention group maintained scores below the clinical cutoff or decreased scores from above to below the clinical cutoff on the ITSEA aggression/defiance subscale (90%ile) and internalizing scale (T-score ≥ 63) at post (60% vs. 43% and 80% vs. 71%, respectively) and at the 3-month follow-up (70% vs. 48% and 85% vs. 80%, respectively). However, these clinically significant changes were not statistically significantly different between groups (using chi square analyses), and group differences were minimal at the 6-month follow-up. Taken together, these findings on parent-reported infant behavior suggest the intervention is promising but may have limited impact on clinical significance, particularly at later time points. However, clinical cutoff scores are known to represent an arbitrary metric and yield limited power in statistical analyses (Blanton & Jaccard, 2006). Therefore, future work should examine the clinical significance of this intervention with a larger sample and across a longer follow-up period.
Although infants in the intervention group displayed significant decreases in levels of activity and impulsivity over time, the change in the intervention group was not significantly different from the change in the standard care group. The lack of a statistically significant interaction on this subscale may be reflective of the low baseline internal consistency of the activity/impulsivity scale, although Cronbach’s alphas on the activity/impulsivity scale were higher at subsequent time points. Nevertheless, early aggression has been shown to have a stronger effect on later functioning (e.g., academic achievement) than do other externalizing dimensions, including activity and impulsivity (Brennan, Shaw, Dishion, & Wilson, 2012), and thus represents an important target for early intervention.
In addition to intervention effects on infant compliance and behavior problems, mothers receiving the intervention demonstrated significant increases in positive and decreases in negative observed behaviors during infant-led play. These parent behaviors were maintained, such that mothers receiving the intervention were five times more likely to use the do skills and avoid the don’t skills than were mothers in standard care at the 6-month follow-up. Despite the significant effect on parenting behaviors, however, the intervention did not have an effect on parenting stress. Although some studies with high-risk families suggest standard PCIT is associated with decreases in parenting stress (Bagner & Eyberg, 2007; Bagner et al., 2010), these effects have been limited to stress related to the child’s disruptive behavior. In the current sample, it is possible that the stress for the 40% of mothers reporting clinically elevated levels on the PSI-SF total scale was largely due to chronic stressors unrelated to the child and thus less responsive to change from a behavioral intervention targeting infant behavior, particularly among high-risk samples. For example, mothers in the current sample with higher percentile scores of parenting stress had significantly lower reported levels of education. However, the extent to which the lack of a statistically significant change on parenting stress was due to these other stressors should be investigated. Furthermore, the literature is conflicted as to whether or not parenting stress negatively impacts parenting intervention outcomes (Shelleby & Shaw, 2014), and future research should examine the moderating effect of parenting stress on outcomes of the current infant intervention to explore the need to intervene on parenting stress in addition to infant behavior.
The current study is the first to demonstrate promising findings for the initial efficacy of a behavioral parenting intervention for externalizing and internalizing problems in infants, as previous studies on behavioral parent training have included children ages 2 years and older (Eyberg et al., 2008). Previous work on the Family Check-Up, which targets parenting using motivational interviewing, has demonstrated findings on both early externalizing and internalizing problems with similarly high-risk families (Shaw, Connell, Dishion, Wilson, & Gardner, 2009; Shaw et al., 2006). However, studies on the Family Check-Up have primarily focused on 2-year-olds and have not examined the intervention with children younger than 17 months. There have also been promising effects for attachment-based interventions with infants (Bakermans-Kranenburg et al., 2003), but these studies typically do not target or examine intervention effects on infant behavior. An exception is a brief intervention called the Video-feedback Intervention to promote Positive Parenting and Sensitive Discipline for 1- to 3-year-olds, which revealed in a randomized controlled trial more positive parental discipline practices in the intervention group relative to a control group (Van Zeijl, Mesman, Van et al., 2006). However, there were no significant effects on child behavior at post-intervention, and no comparisons were conducted at follow-up. Thus, the current study adds to the current literature base by demonstrating promise of a brief behavioral parenting intervention on improving infant behavior during the important transition into the second year of life.
In interpreting the above findings, it is important to consider the limitations of the current study. First, the sample size was relatively small, which potentially resulted in reduced power to detect a significant intervention effect on some variables, such as parenting stress, and limited generalizability of the findings. Furthermore, an important next step is to examine potential moderators (e.g., maternal stress, depression) and mediators (e.g., parent behaviors) of the intervention, which would require a larger sample. Second, the control condition included standard pediatric primary care and not an active intervention comparison. Future research should compare outcomes and cost-effectiveness of this brief intervention with long and comprehensive parenting programs (e.g., Nurse Family Partnership) and may include economic analyses of previously conducted trials. Third, although other caregivers were encouraged to participate in the intervention, analyses were limited to mother-infant observations and maternal report. Given the importance of father involvement in parent training (Bagner, 2013; Bagner & Eyberg, 2003), research should examine the extent to which outcomes are consistent across caregivers. Finally, although we conducted follow-ups at 3 and 6 months, it will be important for future work to examine longer maintenance of the effects of this early behavioral intervention.
Despite these limitations, the current study demonstrates the initial efficacy of a brief home-based behavioral parent-training intervention for infants from high-risk families. The intervention targeted infants from primarily economically disadvantaged and ethnic minority families, for whom early behavior problems are widespread and resistant to treatment. Furthermore, the current intervention is brief and has high potential for dissemination among very young children, who rarely encounter the mental health system. For example, embedding this intervention within an existing system for high-risk families, such as the early intervention system (Kaiser, Cai, Hancock, & Foster, 2002), may prove beneficial in the promotion of infant mental health and should be examined in future mental health services research. Overall, the findings suggest promise intervening during the transition from infancy to toddlerhood – a window of opportunity to prevent behavior problems from becoming entrenched – and in the natural setting to help promote optimal behavioral functioning in infants from the most vulnerable families.
Acknowledgments
This work was supported by a career development award from the National Institute of Mental Health to the first author (K23MH085659). We thank Drs. Alice Carter, Paulo Graziano, and Jeremy Pettit for their consultation and feedback on this manuscript and all participating families for their commitment to our research program.
Footnotes
The authors report no conflicts of interest related to this work.
Contributor Information
Daniel M. Bagner, Florida International University
Stefany Coxe, Florida International University.
Gabriela M. Hungerford, Florida International University
Dainelys Garcia, Florida International University.
Nicole E. Barroso, Florida International University
Jennifer Hernandez, Florida International University.
Jose Rosa-Olivares, Nicklaus Children’s Hospital.
References
- Abidin RR. Parenting Stress Index Manual, Third Edition: Professional Manual. Odessa, FL: Psychological Assessment Resources, Inc; 1995. [Google Scholar]
- Aguilar B, Sroufe LA, Egeland B, Carlson E. Distinguishing the early-onset/persistent and adolescence-onset antisocial behavior types: From birth to 16 years. Development and Psychopathology. 2000;12:109–132. doi: 10.1017/s0954579400002017. Retrieved from http://journals.cambridge.org. [DOI] [PubMed] [Google Scholar]
- Alink LR, Mesman J, van Zeijl J, Stolk MN, Juffer F, Koot HM, van Ijzendoorn MH. The early childhood aggression curve: Development of physical aggression in 10- to 50-month-old children. Child Development. 2006;77:954–966. doi: 10.1111/j.1467-8624.2006.00912.x. [DOI] [PubMed] [Google Scholar]
- Bagner DM. Father’s role in parent training for children with developmental delay. Journal of Family Psychology. 2013;27:650–657. doi: 10.1037/a0033465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagner DM, Eyberg SM. Father involvement in parent training: When does it matter? Journal of Clinical Child and Adolescent Psychology. 2003;32:599–605. doi: 10.1207/S15374424JCCP3204_13. [DOI] [PubMed] [Google Scholar]
- Bagner DM, Eyberg SM. Parent-child interaction therapy for disruptive behavior in children with mental retardation: A randomized controlled trial. Journal of Clinical Child and Adolescent Psychology. 2007;36:418–429. doi: 10.1080/15374410701448448. [DOI] [PubMed] [Google Scholar]
- Bagner DM, Graziano PA. Barriers to success in parent training for young children with developmental delay: The role of cumulative risk. Behavior Modification. 2013;37:356–377. doi: 10.1177/0145445512465307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagner DM, Rodríguez GM, Blake CA, Rosa-Olivares J. Home-based preventive parenting intervention for at-risk infants and their families: An open trial. Cognitive and Behavioral Practice. 2013;20:334–348. doi: 10.1016/j.cbpra.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagner DM, Sheinkopf SJ, Vohr BR, Lester BM. Parenting intervention for externalizing behavior problems in children born premature: An initial examination. Journal of Developmental and Behavioral Pediatrics. 2010;31:209. doi: 10.1097/DBP.0b013e3181d5a294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakermans-Kranenburg MJ, Van Ijzendoorn MH, Juffer F. Less is more: Meta-analyses of sensitivity and attachment interventions in early childhood. Psychological Bulletin. 2003;129:195. doi: 10.1037/0033-2909.129.2.195. [DOI] [PubMed] [Google Scholar]
- Blanton H, Jaccard J. Arbitrary metrics in psychology. American Psychologist. 2006;61:27. doi: 10.1037/0003-066X.61.1.27. [DOI] [PubMed] [Google Scholar]
- Boggs SR, Eyberg SM, Edwards DL, Rayfield A, Jacobs J, Bagner D, Hood KK. Outcomes of parent-child interaction therapy: A comparison of treatment completers and study dropouts one to three years later. Child and Family Behavior Therapy. 2004;26:1–22. [Google Scholar]
- Brennan LM, Shaw DS, Dishion TJ, Wilson M. Longitudinal predictors of school-age academic achievement: Unique contributions of toddler-age aggression, oppositionality, inattention, and hyperactivity. Journal of Abnormal Child Psychology. 2012;40:1289–1300. doi: 10.1007/s10802-012-9639-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs-Gowan MJ, Carter AS, Bosson-Heenan J, Guyer AE, Horwitz SM. Are infant-toddler social-emotional and behavioral problems transient? Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:849–858. doi: 10.1097/01.chi.0000220849.48650.59. [DOI] [PubMed] [Google Scholar]
- Briggs-Gowan MJ, Carter AS, Irwin JR, Wachtel K, Cicchetti DV. The Brief Infant-Toddler Social and Emotional Assessment: Screening for Social-Emotional Problems and Delays in Competence. Journal of Pediatric Psychology. 2004;29:143–155. doi: 10.1093/jpepsy/jsh017. [DOI] [PubMed] [Google Scholar]
- Carter AS, Briggs-Gowan MJ. ITSEA/BITSEA: Infant Toddler and Brief Infant Toddler Social and Emotional Assessment Examiner's Manual. San Antonio, TX: Harcourt Assessment; 2006. [Google Scholar]
- Carter AS, Briggs-Gowan MJ, Davis NO. Assessment of young children's social-emotional development and psychopathology: Recent advances and recommendations for practice. Journal of Child Psychology and Psychiatry. 2004;45:109–134. doi: 10.1046/j.0021-9630.2003.00316.x. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. Mahwah, NJ: Routledge; 2013. [Google Scholar]
- Cote SM, Boivin M, Liu X, Nagin DS, Zoccolillo M, Tremblay RE. Depression and anxiety symptoms: Onset, developmental course and risk factors during early childhood. Journal of Child Psychology and Psychiatry. 2009;50:1201–1208. doi: 10.1111/j.1469-7610.2009.02099.x. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Stormshak EA. Intervening in children's lives: An ecological, family-centered approach to mental health care. American Psychological Association; 2007. [Google Scholar]
- Dombrowski SC, Timmer SG, Blacker DM, Urquiza AJ. A positive behavioural intervention for toddlers: Parent–child attunement therapy. Child Abuse Review. 2005;14:132–151. [Google Scholar]
- Egger HL, Angold A. Common emotional and behavioral disorders in preschool children: presentation, nosology, and epidemiology. Journal of Child Psychology and Psychiatry. 2006;47:313–337. doi: 10.1111/j.1469-7610.2006.01618.x. [DOI] [PubMed] [Google Scholar]
- Eyberg SM. Tailoring and adapting parent-child interaction therapy for new populations. Education and Treatment of Children. 2005;28:197–201. Retrieved from: www.jstor.org/stable/42899841. [Google Scholar]
- Eyberg SM, Boggs SR, Jaccard J. Does maintenance treatment matter? Journal of Abnormal Child Psychology. 2014;42:355–366. doi: 10.1007/s10802-013-9842-9. [DOI] [PubMed] [Google Scholar]
- Eyberg SM, Nelson MM, Boggs SR. Evidence-based psychosocial treatments for children and adolescents with disruptive behavior. Journal of Clinical Child and Adolescent Psychology. 2008;37:1–23. doi: 10.1080/15374410701820117. [DOI] [PubMed] [Google Scholar]
- Eyberg SM, Nelson MM, Duke M, Boggs SR. Manual for the dyadic parent-child interaction coding system. 3rd ed. Gainesville, FL: Department of Clinical and Health Psychology, University of Florida; 2005. Unpublished manuscript. [Google Scholar]
- Feingold A. Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychological Methods. 2009;14:43. doi: 10.1037/a0014699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilliom M, Shaw DS. Codevelopment of externalizing and internalizing problems in early childhood. Development and Psychopathology. 2004;16:313–334. doi: 10.1017/s0954579404044530. [DOI] [PubMed] [Google Scholar]
- Gross D, Fogg L, Webster-Stratton C, Garvey C, Julion W, Grady J. Parent training of toddlers in day care in low-income urban communities. Journal of Consulting and Clinical Psychology. 2003;71:261. doi: 10.1037/0022-006x.71.2.261. [DOI] [PubMed] [Google Scholar]
- Hays JR, Reas DL, Shaw JB. Concurrent validity of the Wechsler abbreviated scale of intelligence and the Kaufman brief intelligence test among psychiatric inpatients. Psychological Reports. 2002;90:355–359. doi: 10.2466/pr0.2002.90.2.355. [DOI] [PubMed] [Google Scholar]
- Hedeker D, Gibbons RD. Longitudinal data analysis. Vol. 451. Hoboken, NJ: John Wiley & Sons; 2006. [Google Scholar]
- Heinrichs N, Bertram H, Kuschel A, Hahlweg K. Parent recruitment and retention in a universal prevention program for child behavior and emotional problems: Barriers to research and program participation. Prevention Science. 2005;6:275–286. doi: 10.1007/s11121-005-0006-1. [DOI] [PubMed] [Google Scholar]
- Kaiser AP, Cai X, Hancock TB, Foster EM. Teacher-reported behavior problems and language delays in boys and girls enrolled in Head Start. Behavioral Disorders. 2002;28:23–39. Retrieved from: http://www.jstor.org/stable/23889147. [Google Scholar]
- Kaminski JW, Valle LA, Filene JH, Boyle CL. A meta-analytic review of components associated with parent training program effectiveness. Journal of Abnormal Child Psychology. 2008;36:567–589. doi: 10.1007/s10802-007-9201-9. [DOI] [PubMed] [Google Scholar]
- Keenan K, Wakschlag LS. More than the terrible twos: The nature and severity of behavior problems in clinic-referred preschool children. Journal of Abnormal Child Psychology. 2000;28:33–46. doi: 10.1023/a:1005118000977. [DOI] [PubMed] [Google Scholar]
- Keenan K, Wakschlag LS. Can a valid diagnosis of disruptive behavior disorder be made in preschool children? American Journal of Psychiatry. 2002;159:351–358. doi: 10.1176/appi.ajp.159.3.351. [DOI] [PubMed] [Google Scholar]
- Kohlhoff J, Morgan S. Parent-child interaction therapy for toddlers: A pilot study. Child and Family Behavior Therapy. 2014;36:121–139. [Google Scholar]
- Lavigne JV, LeBailly SA, Gouze KR, Binns HJ, Keller J, Pate L. Predictors and correlates of completing behavioral parent training for the treatment of oppositional defiant disorder in pediatric primary care. Behavior Therapy. 2010;41:198–211. doi: 10.1016/j.beth.2009.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linver MR, Brooks-Gunn J, Kohen DE. Family processes as pathways from income to young children's development. Developmental Psychology. 2002;38:719–734. [PubMed] [Google Scholar]
- Lundahl B, Risser HJ, Lovejoy MC. A meta-analysis of parent training: Moderators and follow-up effects. Clinical Psychology Review. 2006;26:86–104. doi: 10.1016/j.cpr.2005.07.004. [DOI] [PubMed] [Google Scholar]
- McMahon RJ, Forehand RL. Helping the Noncompliant Child: Family-based treatment for oppositional defiant disorder. New York, NY: Guilford Press; 2003. [Google Scholar]
- Moffitt TE, Caspi A, Harrington H, Milne BJ. Males on the life-course-persistent and adolescence-limited antisocial pathways: Follow-up at age 26 years. Development and Psychopathology. 2002;14:179–207. doi: 10.1017/s0954579402001104. Retrieved from http://journals.cambridge.org. [DOI] [PubMed] [Google Scholar]
- Nixon RDV, Sweeney L, Erickson DB, Touyz SW. Parent-child interaction therapy: A comparison of standard and abbreviated treatments for oppositional defiant preschoolers. Journal of Consulting and Clinical Psychology. 2003;71:251–260. doi: 10.1037/0022-006x.71.2.251. [DOI] [PubMed] [Google Scholar]
- Olds DL. Prenatal and infancy home visiting by nurses: From randomized trials to community replication. Prevention Science. 2002;3:153–172. doi: 10.1023/a:1019990432161. [DOI] [PubMed] [Google Scholar]
- Olds DL, Robinson J, Pettitt L, Luckey DW, Holmberg J, Ng RK, Henderson CR. Effects of home visits by paraprofessionals and by nurses: Age 4 follow-up results of a randomized trial. Pediatrics. 2004;114:1560–1568. doi: 10.1542/peds.2004-0961. [DOI] [PubMed] [Google Scholar]
- Olds DL, Sadler L, Kitzman H. Programs for parents of infants and toddlers: Recent evidence from randomized trials. Journal of Child Psychology and Psychiatry. 2007;48:355–391. doi: 10.1111/j.1469-7610.2006.01702.x. [DOI] [PubMed] [Google Scholar]
- Patterson GR. The early development of coercive family process. Washington, DC: American Psychological Association; 2002. [Google Scholar]
- Pons JI, Flores-Pabón L, Matías-Carrelo L, Rodríguez M, Rosario-Hernández E, Rodríguez JM, Yang J. Confiabilidad de la Escala de Inteligencia Wechsler para Adultos Versión III, Puerto Rico (EIWA-III) Revista Puertorriqueña de Psicología. 2008;19:112–132. Retrieved from: http://pepsic.bvsalud.org. [Google Scholar]
- Pons JI, Matías-Carrelo L, Rodríguez M, Rodríguez JM, Herrans LL, Jiménez ME, Yang J. Estudios de validez de la Escala de Inteligencia Wechsler para Adultos Versión III, Puerto Rico (EIWA-III) Revista Puertorriqueña de Psicología. 2008;19:75–111. Retrieved from: http://pepsic.bvsalud.org. [Google Scholar]
- Qi CH, Kaiser AP. Behavior problems of preschool children from low-income families review of the literature. Topics in Early Childhood Special Education. 2003;23:188–216. [Google Scholar]
- Reitman D, Currier RO, Stickle TR. A critical evaluation of the Parenting Stress Index-Short Form (PSI-SF) in a head start population. Journal of Clinical Child and Adolescent Psychology. 2002;31:384–392. doi: 10.1207/S15374424JCCP3103_10. [DOI] [PubMed] [Google Scholar]
- Reyno SM, McGrath PJ. Predictors of parent training efficacy for child externalizing behavior problems – a meta-analytic review. Journal of Child Psychology and Psychiatry. 2006;47:99–111. doi: 10.1111/j.1469-7610.2005.01544.x. [DOI] [PubMed] [Google Scholar]
- Romeo R, Knapp M, Scott S. Economic cost of severe antisocial behaviour in children–and who pays it. The British Journal of Psychiatry. 2006;188:547–553. doi: 10.1192/bjp.bp.104.007625. [DOI] [PubMed] [Google Scholar]
- Rubin DB. Inference and missing data. Biometrika. 1976;63:581–592. [Google Scholar]
- Sanders MR, Cann W, Markie-Dadds C. The Triple P-Positive Parenting Programme: A universal population-level approach to the prevention of child abuse. Child Abuse Review. 2003;12:155–171. [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147. [PubMed] [Google Scholar]
- Schuhmann EM, Foote RC, Eyberg SM, Boggs SR, Algina J. Efficacy of parent-child interaction therapy: Interim report of a randomized trial with short-term maintenance. Journal of Clinical Child Psychology. 1998;27:34–45. doi: 10.1207/s15374424jccp2701_4. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Connell A, Dishion TJ, Wilson MN, Gardner F. Improvements in maternal depression as a mediator of intervention effects on early childhood problem behavior. Development and Psychopathology. 2009;21:417–439. doi: 10.1017/S0954579409000236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw DS, Dishion TJ, Supplee L, Gardner F, Arnds K. Randomized trial of a family-centered approach to the prevention of early conduct problems: 2-year effects of the family check-up in early childhood. Journal of Consulting and Clinical Psychology. 2006;74:1–9. doi: 10.1037/0022-006X.74.1.1. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Gilliom M, Ingoldsby EM, Nagin DS. Trajectories leading to school-age conduct problems. Developmental Psychology. 2003;39:189–200. doi: 10.1037//0012-1649.39.2.189. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Keenan K, Vondra JI. Developmental precursors of externalizing behavior: Ages 1 to 3. Developmental Psychology. 1994;30:355–364. [Google Scholar]
- Shaw DS, Owens EB, Giovannelli J, Winslow EB. Infant and toddler pathways leading to early externalizing disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:36–43. doi: 10.1097/00004583-200101000-00014. [DOI] [PubMed] [Google Scholar]
- Shelleby EC, Shaw DS. Outcomes of parenting interventions for child conduct problems: A review of differential effectiveness. Child Psychiatry and Human Development. 2014;45:628–645. doi: 10.1007/s10578-013-0431-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas JM, Guskin KA. Disruptive behavior in young children: What does it mean? Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:44–51. doi: 10.1097/00004583-200101000-00015. [DOI] [PubMed] [Google Scholar]
- Thomas R, Zimmer-Gembeck MJ. Parent-child interaction therapy: An evidence-based treatment for child maltreatment. Child Maltreatment. 2012;17:253–266. doi: 10.1177/1077559512459555. doi: 1077559512459555. [DOI] [PubMed] [Google Scholar]
- van Lier PAC, Vitaro F, Barker ED, Brendgen M, Tremblay RE, Boivin M. Peer Victimization, Poor Academic Achievement, and the Link Between Childhood Externalizing and Internalizing Problems. Child Development. 2012;83:1775–1788. doi: 10.1111/j.1467-8624.2012.01802.x. [DOI] [PubMed] [Google Scholar]
- van Zeijl J, Mesman J, Stolk MN, Alink LR, van Ijzendoorn MH, Bakermans-Kranenburg MJ, Koot HM. Terrible ones? Assessment of externalizing behaviors in infancy with the Child Behavior Checklist. Journal of Child Psychology and Psychiatry. 2006;47:801–810. doi: 10.1111/j.1469-7610.2006.01616.x. [DOI] [PubMed] [Google Scholar]
- Van Zeijl J, Mesman J, Van IJzendoorn MH, Bakermans-Kranenburg MJ, Juffer F, Stolk MN, Alink LR. Attachment-based intervention for enhancing sensitive discipline in mothers of 1- to 3-year-old children at risk for externalizing behavior problems: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2006;74:994–1005. doi: 10.1037/0022-006X.74.6.994. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C, Hammond M. Predictors of treatment outcome in parent training for families with conduct problem children. Behavior Therapy. 1990;21:319–337. [Google Scholar]
- Webster-Stratton C, Reid MJ. In: The Incredible Years parents, teachers, and children’s training series: A multifaceted approach for young children with conduct disorder. Evidence-based psychotherapies for children and adolescents. Weisz JR, Kazdin AE, editors. New York, NY: Guilford Press; 2010. [Google Scholar]
- Wechsler D. Wechsler Adult Scale of Intelligence - Third Edition. San Antonio, TX: Pearson; 1997. [Google Scholar]
- Wechsler D. Wechsler Abbreviated Scale of Intelligence. San Antonio, TX: Pearson; 1999. [Google Scholar]
- Wechsler D. Ecala de Inteligencia Wechsler Para Adultos. San Antonio, TX: Pearson; 2008. [Google Scholar]
- Whiteside-Mansell L, Ayoub C, McKelvey L, Faldowski RA, Hart A, Shears J. Parenting stress of low-income parents of toddlers and preschoolers: Psychometric properties of a short form of the Parenting Stress Index. Parenting: Science and Practice. 2007;7:26–56. [Google Scholar]
- Zisser A, Eyberg SM. Treating oppositional behavior in children using Parent-Child Interaction Therapy. In: Kazdin AE, Weisz JR, editors. Evidence-based psychotherapies for children and adolescents. Vol. 2. New York, NY: Guilford Press; 2010. pp. 179–193. [Google Scholar]