Abstract
Intrascrotal lipoblastoma is a rare pediatric benign soft tissue neoplasm, and only 11 cases have been reported. The accurate preoperative diagnosis is difficult because of its rarelity and the similarity with the other soft tissue tumors. Among them, accurate preoperative diagnosis had been made in only one case. Thus, almost all of the cases had required inguinal mass excision (and orchidectomy in one case). In this paper, we discuss the accurate preoperative diagnosis of intrascrotal lipoblastoma and subsequent simple tumorectomy via minimal invasive scrotal skin incision, in 1-year-old boy. On physical examination, intrascrotal extra-testicular lobulated mass was palpated on the right scrotum. An ultrasonography revealed the well-circumscribed, iso-echoic, scant blood-flow, and lobulated tumors with each lobules of 1 to 4 cm in diameter, and the tumor located outside of the tunica vaginalis testis. The serum values of alpha-fetoprotein (AFP) and beta-human chorionic gonadotropin (b-hCG) were within normal limit. The preoperative diagnosis of intrascrotal lipoblastoma was made, and the mass was excised via minimal scrotal incision. The right testicle and epididymis were normal. The lesion consisted of the distinct two lobulated tumors, and microscopic examination confirmed the diagnosis of intrascrotal lipoblastoma. The postoperative course was uneventful without evidence of recurrence. A rare intrascrotal lipoblastoma is seldom made accurate preoperative diagnosis; however, the accurate preoperative suspicion of this tumor leads to the minimal invasive tumorectomy via scrotal skin incision and favorable postoperative recovery without recurrence.
Keywords: Intrascrotal lipoblastoma, Scrotal incision, Preoperative diagnosis
Background
In the first two decades of life, adipose tumors are relatively rare, comprising about 6 % of soft tissue neoplasms. About 60 % of these are simple lipomas or variants, and up to 30 % are lipoblastomas [1]. It is found most commonly in the trunk or upper and lower extremities as a painless nodule or mass [1]. Less common sites of involvement include the head and neck area [2], mediastinum [3], mesentery [4], omentum [5], retroperitoneum [6], and scrotum [7–16]. The accurate preoperative diagnosis is difficult because of its rarelity and the similarity with the other soft tissue tumors [17]. Previously, 11 cases of intrascrotal lipoblastoma have been reported [7–16]. Among them, accurate preoperative diagnosis had been made in only one case [14], and an another case had been underwent orchidectomy due to the preoperative suspicion of paratesticulsr rhabdomyosarcoma [13]. This report describes a case in which accurate preoperative diagnosis of this rare tumor z procedure (e.g., inguinal incision and orchidectomy) and to result in the favorable outcomes.
Case presentation
A 1-year and 7-month-old boy was taken to his pediatrician after his family members noticed a right swollen scrotum. An intrascrotal tumor was suspected, and he was referred to our pediatric surgery department. On physical examination, a 7-cm lobulated mass was palpated on the right scrotum, apart from the normal bilateral testes (Fig. 1). The rubbery-hard tumor had smooth surface and was mobile, suggesting benign pathology. An ultrasonography revealed the well-circumscribed, hyper-echoic, scant blood-flow, and lobulated tumors with each lobules of 1 to 4 cm in diameter, and the tumor is located outside of the tunica vaginalis testis. A contrast computed tomography (CT) scan showed the less enhancement of the tumors. All of the tumors revealed the high intensity on magnetic resonance imaging (MRI) T2-weighted image, but T1-weighted image showed the mosaic pattern (e.g., T1-low lesions and T1-high lesions were co-existed) (Fig. 2a, b). The serum values of alpha-fetoprotein (AFP) and beta-human chorionic gonadotropin (b-hcg) were within normal limit. We considered that the most likely preoperative diagnosis is the intrascrotal lipoblastoma, as the previously reported cases [8, 10, 11, 14, 15] had the quite similar features (e.g., a young child with well-circumscribed and lobulated intrascrotal lipoid mass apart from the testes or the epididymis) with our case. The other differential diagnoses were rhabdomyosarcoma, lipoma, and liposarcoma. The mass was excised by scrotal incision (Fig. 3b). The lesion developed out of the cord and was independent of the right testicle and of the processus vaginalis (Fig. 3a, b). The right testicle was normal (Fig. 3a). The lesion consisted of the distinct two lobulated and well-circumscribed tumors with diameters of 6 cm × 4 cm × 3 cm and 3.5 cm × 2 cm × 2 cm, respectively (Fig. 4).
Fig. 1.
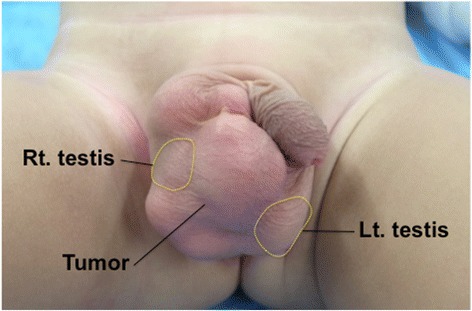
The preoperative finding of the scrotum. The tumors were apart from the bilateral testes
Fig. 2.
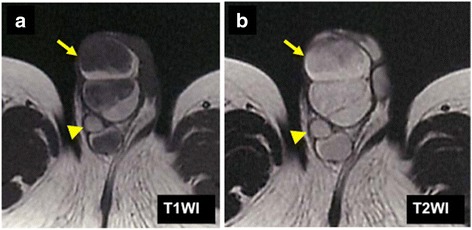
The MRI findings. a T1-weighted image showed the mosaic pattern (e.g., T1-low lesions and T1-high lesions were co-existed). b All of the tumor revealed the high intensity on T2-weighted image. (Arrow heads indicate right testis.)
Fig. 3.
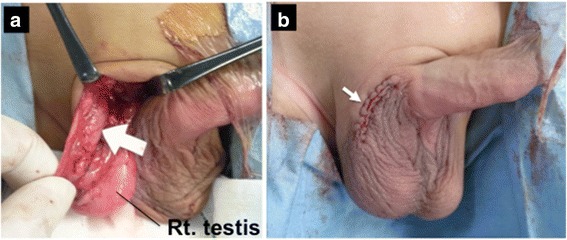
Operative findings of the scrotum. a The lesion located out of the cord and was independent of the normal right testicle and of the processus vaginalis. (White arrow indicates the tumor location.) b The mass was excised via the minimal scrotal incision
Fig. 4.
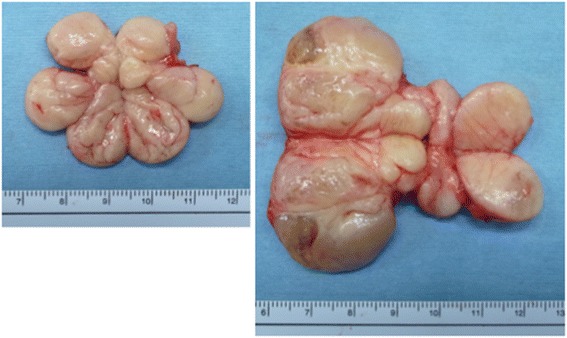
The cut surface of the specimens. The lesion consisted of the distinct two lobulated and well-circumscribed tumors with diameter of 6 cm × 4 cm × 3 cm and 3.5 cm × 2 cm × 2 cm, respectively
Microscopically, both tumors were multilobulated tumors of adipose tissue and were surrounded by the capsule composed of loose connective tissue. Lobules were separated by fibrous septa and were composed of mature adipocytes and vacuolated lipoblasts showing varying degrees of differentiation. Both tumors were diagnosed as lipoblastoma (Fig. 5).
Fig. 5.
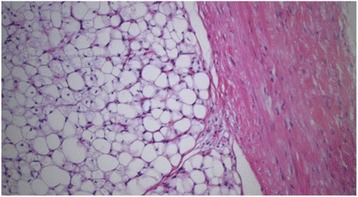
Pathological analysis. Microscopically, both tumors were multilobulated tumors of adipose tissue and were surrounded by the capsule composed of loose connective tissue. The both tumors were diagnosed as lipoblastoma (hematoxylin-eosin stain, ×100)
The postoperative course was uneventful, and the patient discharged home on postoperative day 1. The patient has been followed up for 8 months, without evidence of recurrence.
Discussion
Lipoblastoma, a relatively rare tumor of embryonal fat, is characterized by its benign nature, early presentation (90 % <3 years) [18], male predominance of 3:1 [19], and rapid growth. Although it is found most commonly in the trunk or upper and lower extremities [1], the involvement of the other lesion (e.g., head/neck [2], mediastinum [3], mesentery [4], omentum [5], retroperitoneum, and scrotum (Table 1) [7–16]) has been reported. The differential diagnoses of pediatric intrascrotal paratesticular tumor include benign tumors (e.g., lipoma, lipoblastoma, leimomyoma, and hemangioma) and malignant tumors (e.g., rhabdomyosarcoma, liposarcoma, and melanotic neuroectodermal tumor of infancy (MNTI)) [15, 20]. Of these, leiomyoma and MNTI generally originate from the epididymis, and hemangioma has the much vasculature. So at first, we could deny these three tumors. Rhabdomyosarcoma is the most common paratesticular malignancies in pediatric population [21], and it arises from the tunicae of the testis, epididymis, and spermatic cord. But, rhabdomyosarcoma commonly occurs in older children with median age of 7 years old [22] and reveals heterogeneous echogenicity and increased blood flow in ultrasonography (US) [23]. Liposarcoma lacks lobulated shape, and occurrence in pediatric population is extremely rare [20]. Also, lower intensity of T1-weighted MRI image has been noted with lipoblastoma compared with lipoma [24], likely because of increased cellularity. In our case, the intratumoral mosaic pattern (e.g., T1-low lesions and T1-high lesions were co-existed) on T1-weighted image suggested the lipoblastoma, rather than a lipoma. Furthermore, lipoblastoma has the following distinguishable characteristics: I: commonly involves in patients younger than 3 years old, predominantly in male by 3:1 and II: well-circumscribed, lobulated, hypovascular fatty tumor. Thus, we could make accurate preoperative diagnosis of lipoblastoma. Our case is the second case in which accurate preoperative diagnosis of lipoblastoma could be made (Table 1). However, the differential diagnosis of intrascrotal tumor in older patients might be more complicated, because the origin of the testicular or paratesticular might sometimes unclear. The testicular lesion includes teratoma, seminoma, or non-neoplastic lesion (e.g., hydrocele or inguinal hernia) [20].
Table 1.
Summary of cases of intrascrotal lipoblastoma in the literature
| Patient | Authors | Year | Age | Side | AFP (ng/ml) | β hCG (UI/L) | Preoperative image findings | Preoperative diagnosis | Approach | Treatment | Size of tumor (cm × cm × cm) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Arda et al. | 1993 | 15 months | Left | N.A | N.A | N.A | N.A | Inguinal | Mass excision | 6.5 × 4 × 3 |
| 2 | Turner et al. | 1998 | 9 months | Left | 11 | 1.8 | US: lobulated solid lesion with well-defined margin. | N.A | Inguinal | Mass excision | 5 × 2.5 × 1.5 |
| 3 | Chun | 2001 | 18 months | N.A | N.A | N.A | N.A | N.A | N.A | N.A | 2.3 × 2 × 1.3 |
| 4 | Somers et al. | 2004 | 7 months | Left | N.A | N.A | US: heterogeneous mass consisting of small cystic areas admixed with solid components. | N.A | Inguinal | Mass excision | 14 × 14 × 8a |
| 5 | Dy et al. | 2007 | 4 years | N.A. | N.A | N.A | N.A | N.A | Inguinal | Mass excision | 3.5 × 2 × 2 |
| 6 | Del Sordo et al. | 2007 | 4 years | Right | N.A | N.A | N.A | N.A | Inguinal | Mass excision | 2 × 1.2 × 0.8 |
| 7 | Robb et al. | 2010 | 10 months | Left | N | N | US: echogenic mass with good vascularity, separate to the testis. | RMS | Inguinal | Orchidectomy and Mass excision | 3 × 2.5 × 1.5 |
| 8 | Kamel et al. | 2011 | 4 months | Right | N.A | N.A | US and CT: large fatty tumor. | Lipoblastoma | Inguinal | Mass excision | 10 × 9 × 7 |
| 9 | Nakib et al. | 2013 | 10 years | Right | N | N | US: a hyper-echoic lesion above the upper pole of the testicle. | N.A | N.A | Mass excision | 5 × 5 × 1.5 |
| 10 | Eyssartier et al. | 2013 | 15 months | Left | 17 | 4 | US: echogenic solid lesion with well-defined margin. | N.A | Inguinal | Mass excision | 2 × 1.5 × 1 |
| 11 | Eyssartier et al. | 2013 | 16 months | Right | 7.8 | <1 | US: an echogenic mass. | N.A | Inguinal | Mass excision | 1.5 × 1.5 × 2 |
| 12 | Present case | 2015 | 19 months | Right | 6.0 | 225 | US: hyper-echoic lobulated mass with well-circumscribed margin. CT: less enhanced mass. MRI: TI high/low, T2 high. | Lipoblastoma | Scrotal | Mass excision | 6 × 4 × 3, 3.5 × 2 × 2 |
N.A not available; N normal; US ultrasonography; RMS rhabdomyosarcoma
aIn this case, the other two residual lesions were removed postoperatively
Regarding the surgical treatment, malignant lesions require the gold-standard surgical approach of radical inguinal orchidectomy [25]. On the other hand, standard treatment of the lipoblastoma is the complete resection of the tumor [17], to avoid recurrence. In fact, among the previously reported cases of intrascrotal lipoblastoma (Table 1), almost all of the cases had been performed inguinal mass excision (and orchidectomy in one case). Our case is the first case in which simple tumorectomy was performed via minimal scrotal skin incision. We consider that if the adequate preoperative suspicion of lipoblastoma could be made, we can avoid the invasive procedure (inguinal exploration or orchidectomy). In our case, accurate preoperative diagnosis of this rare tumor led to the simple tumor resection via minimal scrotal skin incision and favorable postoperative recovery without recurrence.
Conclusions
A rare intrascrotal lipoblastoma is seldom made accurate preoperative diagnosis; however, the accurate preoperative suspicion of this tumor leads to the minimal invasive tumorectomy via scrotal skin incision and favorable postoperative recovery without recurrence.
Consent
Written informed consent was obtained from the parents of the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Abbreviations
- AFP
alpha-fetoprotein
- b-hcg
beta-human chorionic gonadotropin
- CT
computed tomography
- MNTI
melanotic neuroectodermal tumor of infancy
- MRI
magnetic resonance imaging
- RMS
rhabdomyosarcoma
- US
ultrasonography
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
KY, HI, HM, and MS equally worked in the diagnosis and surgery. KY contributed to the data collection, perioperative care, and creating the manuscript. HI was the operating surgeon and contributed to the review of the manuscript. All authors read and approved the final manuscript.
Authors’ information
KY and HM are the assistant professors of surgery and worked as pediatric surgeons for more than 5 years. HI is the professor of pediatric surgery with experience of more than 20 years. MS is the chief professor of Gastointestinal/Pediatric Surgery.
References
- 1.Chung EB, Enzinger FM. Benign lipoblastomatosis. An analysis of 35 cases. Cancer. 1973;32:482–492. doi: 10.1002/1097-0142(197308)32:2<482::AID-CNCR2820320229>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 2.Pham NS, Poirier B, Fuller SC, Dublin AB, Tollefson TT. Pediatric lipoblastoma in the head and neck: a systematic review of 48 reported cases. Int J Pediatr Otorhinolaryngol. 2010;74:723–728. doi: 10.1016/j.ijporl.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 3.Salem R, Zohd M, Njim L, et al. Lipoblastoma: a rare lesion in the differential diagnosis of childhood mediastinal tumors. J Pediatr Surg. 2011;46:e21–23. doi: 10.1016/j.jpedsurg.2011.01.030. [DOI] [PubMed] [Google Scholar]
- 4.Yu DC, Javid PJ, Chikwava KR, et al. Mesenteric lipoblastoma presenting as a segmental volvulus. J Pediatr Surg. 2009;44:e25–28. doi: 10.1016/j.jpedsurg.2008.11.037. [DOI] [PubMed] [Google Scholar]
- 5.Koplin SA, Twohig MH, Lund DP, Hafez GR. Omental lipoblastoma. Pathol Res Pract. 2008;204:277–281. doi: 10.1016/j.prp.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 6.Api O, Akil A, Uzun MG, et al. Fetal retroperitoneal lipoblastoma: ultrasonographic appearance of a rare embryonal soft tissue tumor. J Matern Fetal Neonatal Med. 2010;23:1069–1071. doi: 10.3109/14767050903301025. [DOI] [PubMed] [Google Scholar]
- 7.Arda IS, Senocak ME, Gogus S, Buyukpamukcu N. A case of benign intrascrotal lipoblastoma clinically mimicking testicular torsion and review of the literature. J Pediatr Surg. 1993;28:259–261. doi: 10.1016/S0022-3468(05)80289-1. [DOI] [PubMed] [Google Scholar]
- 8.Turner DT, Shah SM, Jones R. Intrascrotal lipoblastoma. Br J Urol. 1998;81:166–167. doi: 10.1046/j.1464-410x.1998.00350.x. [DOI] [PubMed] [Google Scholar]
- 9.Chun YS, Kim WK, Park KW, Lee SC, Jung SE. Lipoblastoma. J Pediatr Surg. 2001;36:905–907. doi: 10.1053/jpsu.2001.23969. [DOI] [PubMed] [Google Scholar]
- 10.Somers GR, Teshima I, Nasr A, Cook A, Khoury AE, Taylor GP. Intrascrotal lipoblastoma with a complex karyotype: a case report and review of the literature. Arch Pathol Lab Med. 2004;128:797–800. doi: 10.5858/2004-128-797-ILWACK. [DOI] [PubMed] [Google Scholar]
- 11.Del Sordo R, Cavaliere A, Sidoni A, Colella R, Bellezza G. Intrascrotal lipoblastoma: a case report and review of the literature. J Pediatr Surg. 2007;42:E9–11. doi: 10.1016/j.jpedsurg.2006.12.022. [DOI] [PubMed] [Google Scholar]
- 12.Dy JS, Fuchs A, Palmer LS. Benign intrascrotal lipoblastoma in a child. Urology. 2007;70(372):e371–372. doi: 10.1016/j.urology.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 13.Robb A, Rogers T, Nicholls G. A tale of 3 testes? A rare presentation of lipoblastoma with a novel karyotype. J Pediatr Surg. 2010;45:E29–31. doi: 10.1016/j.jpedsurg.2009.10.093. [DOI] [PubMed] [Google Scholar]
- 14.Kamal NM, Jouini R, Yahya S, Haiba M. Benign intrascrotal lipoblastoma in a 4-month-old infant: a case report and review of literature. J Pediatr Surg. 2011;46:E9–12. doi: 10.1016/j.jpedsurg.2011.03.012. [DOI] [PubMed] [Google Scholar]
- 15.Eyssartier E, Villemagne T, Maurin L, Machet MC, Lardy H. Intrascrotal lipoblastoma: a report of two cases and a review of the literature. J Pediatr Urol. 2013;9:e151–154. doi: 10.1016/j.jpurol.2013.03.016. [DOI] [PubMed] [Google Scholar]
- 16.Nakib G, Calcaterra V, Avolio L, et al. Intrascrotal lipoblastoma in a ten year old: case report and review of literature. Rare Tumors. 2013;5:e11. doi: 10.4081/rt.2013.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kok KY, Telisinghe PU. Lipoblastoma: clinical features, treatment, and outcome. World J Surg. 2010;34:1517–1522. doi: 10.1007/s00268-010-0466-8. [DOI] [PubMed] [Google Scholar]
- 18.Coffin CM. Lipoblastoma: an embryonal tumor of soft tissue related to organogenesis. Semin Diagn Pathol. 1994;11:98–103. [PubMed] [Google Scholar]
- 19.Stringel G, Shandling B, Mancer K, Ein SH. Lipoblastoma in infants and children. J Pediatr Surg. 1982;17:277–280. doi: 10.1016/S0022-3468(82)80012-2. [DOI] [PubMed] [Google Scholar]
- 20.Ahmed HU, Arya M, Muneer A, Mushtaq I, Sebire NJ. Testicular and paratesticular tumours in the prepubertal population. Lancet Oncol. 2010;11:476–483. doi: 10.1016/S1470-2045(10)70012-7. [DOI] [PubMed] [Google Scholar]
- 21.Shapiro E, Strother D. Pediatric genitourinary rhabdomyosarcoma. J Urol. 1992;148:1761–1768. doi: 10.1016/s0022-5347(17)37023-4. [DOI] [PubMed] [Google Scholar]
- 22.Ferrari A, Bisogno G, Casanova M, et al. Paratesticular rhabdomyosarcoma: report from the Italian and German Cooperative Group. J Clin Oncol. 2002;20:449–455. doi: 10.1200/JCO.20.2.449. [DOI] [PubMed] [Google Scholar]
- 23.Akbar SA, Sayyed TA, Jafri SZ, Hasteh F, Neill JS. Multimodality imaging of paratesticular neoplasms and their rare mimics. Radiographics. 2003;23:1461–1476. doi: 10.1148/rg.236025174. [DOI] [PubMed] [Google Scholar]
- 24.Ha TV, Kleinman PK, Fraire A, et al. MR imaging of benign fatty tumors in children: report of four cases and review of the literature. Skelet Radiol. 1994;23:361–367. doi: 10.1007/BF02416994. [DOI] [PubMed] [Google Scholar]
- 25.Agarwal PK, Palmer JS. Testicular and paratesticular neoplasms in prepubertal males. J Urol. 2006;176:875–881. doi: 10.1016/j.juro.2006.04.021. [DOI] [PubMed] [Google Scholar]


