Abstract
Introduction:
Smokers receiving support in specialist centers tend to have a higher short-term quit rate, compared with those receiving support in other settings from professionals for whom smoking cessation is only a part of their work. We investigated the difference in longer-term abstinence after short-term smoking cessation treatment from specialist and nonspecialist smoking cessation services.
Methods:
We conducted a secondary analysis of data from a randomized controlled trial of self-help booklets for the prevention of smoking relapse. The trial included 1088 short-term quitters from specialist stop smoking clinics and 316 from nonspecialist cessation services (such as general practice, pharmacies, and health trainer services). The difference in prolonged smoking abstinence from months 4 to 12 between specialist and nonspecialist services was compared. Multivariable logistic regression analyses were conducted to investigate the association between continuous smoking abstinence and the type of smoking cessation services, adjusted for possible confounding factors (including demographic, socioeconomic, and smoking history variables).
Results:
The proportion of continuous abstinence from 4 to 12 months was higher in short-term quitters from specialist services compared with those from nonspecialist services (39% vs. 32%; P = .023). After adjusting for a range of participant characteristics and smoking variables, the specialist service was significantly associated with a higher rate of longer-term smoking abstinence (odds ratio: 1.48, 95% CI = 1.09% to 2.00%; P = .011).
Conclusions:
People who receive support to stop smoking from a specialist appear to be at lower risk of relapse than those receiving support from a nonspecialist advisor.
Introduction
Behavioral and pharmacological interventions are effective for smoking cessation in smokers who are motivated to quit. 1 Since 2001, a national network of NHS stop smoking services has been established in England to provide behavioral support and pharmacotherapy to smokers who would like to quit. 2 In 2012/2013, the English stop smoking services provided support to 724 247 quit attempts, and generated 265 140 biochemically validated quitters (37% of quit attempts) at 4 weeks after the quit date. 3
In the English stop smoking services, smokers motivated to quit may receive support in specialist clinics, primary care, pharmacy, or other settings. 3 Previous studies reported that smokers receiving support in specialist centers tended to have a higher quit rate at 4 weeks after quit dates, compared to those receiving support in other settings from professionals for whom smoking cessation was only a part of their work. 4,5 However, a recent study using routine monitoring data found little difference in quit rates between different types of smoking cessation advisors, except that smoking cessation support by nurses tended to be less effective than by specialist advisors. 6 Previous studies have only compared short-term smoking outcomes. For longer-term smoking outcomes, it has been assumed that the rate of smoking relapse would be similar among short-term quitters, irrespective of the type of smoking cessation support provided. 4,5,7 There is a lack of evidence to compare the longer-term smoking outcomes between different types of smoking cessation advisors.
In a randomized controlled trial of self-help materials for smoking relapse prevention (ISRCTN: 36980856), 8 we recruited 1407 short-term quitters and conducted follow-up interviews at 3 and 12 months after quit dates. Participants in the treatment group received a set of eight self-help booklets for relapse prevention, and those in the control group were sent a single leaflet that is currently used in practice. It was found that there was no difference between the intervention groups in prolonged smoking abstinence from month 4 to 12 (37% vs. 39%, P = .51), and main findings of the trial will be published elsewhere. 9 In the trial, we also collected data on the type of stop smoking services (specialist services, or from general practice nurses, pharmacists, or community health trainers). In a secondary analysis, we examined whether there was a difference in longer-term smoking abstinence at 12 months between quitters who received smoking cessation treatment in different settings.
Methods
Study Participants
Study participants were those included in a randomized controlled trial of self-help material for smoking relapse prevention. 9 The target population for this trial was people who had stopped smoking, as verified by carbon monoxide (CO) reading, at 4 weeks after the quit date, following the provision of cessation support from NHS stop smoking services. The biochemically verified 4-week quitter is defined as a treated smoker who reports abstinence from at least day 14 after the quit date to the 4-week follow-up point and who blows an exhaled CO reading of less than 10 ppm. 10 Quitters who were pregnant, unable to read booklets in English, from families at the same address, or younger than 18 years were excluded.
We recruited CO-validated short-term quitters from August 2011, and initially recruited participants only from specialist stop smoking clinics. In May 2012, participant recruitment was expanded to other settings, including pharmacies, general practice, and health trainer services. Smoking cessation advisors in specialist stop smoking centers are more highly trained in delivering smoking cessation interventions. 4 In contrast, smoking cessation counseling is only a small part of the role of practice nurses and pharmacists. Health Trainers also have a wider role, providing general support for health behavioral changes, including stopping smoking, dietary changes, reducing alcohol intake, and increasing physical activity. 11
The trial achieved the recruitment target by June 2013, and included a total of 1407 eligible short-term quitters. Three participants died before the 12-month follow-up and were excluded from the analysis. Of the 1404 participants, there were 1088 participants from specialist stop smoking clinics, and 316 from nonspecialist cessation services (including 220 from general practices, 57 from health trainers, and 39 from pharmacy). The follow-up rate was 86% at 12 months, and the rate of CO verification was 85% for participants who reported abstinence at the 12-month follow-up.
Data Collection and Variables
Four weeks after the quit date, stop smoking advisors gathered baseline information from participants who had consented to participate in the study, including participants’ demographic characteristics and smoking history (including previous quit attempts, number of cigarettes per day, time of the first cigarette after waking up, living with a smoking partner or not). Study participants were then followed up by researchers at 3 and 12 months after quit dates. The follow-up interviews were conducted by telephone and involved researchers administering a questionnaire which asked questions about the participant’s smoking status and process variables. In addition, at the 3 and 12-month follow-up, we asked participants whether they used smoking cessation medications during 2 and 3 months after the quit date (For more details about questions asked and response options, please see the baseline and follow-up questionnaires in an online Supplementary Material.).
The primary outcome in the study was defined as prolonged abstinence from months 4 to 12, with no more than five cigarettes in total, and confirmed by CO < 10 ppm at the 12-month follow-up. 12 At the 12-month follow-up, participants who reported smoking abstinence during the past 7 days were invited to take a CO test. Participants came to a clinic or a researcher visited them at home for this test. To optimize CO test rates, a shopping voucher (£20) was offered to each of the participants who attended the CO test at the 12-month follow-up. Participants who declined biochemical verification or who did not respond to follow-up were classified as relapsed. However, according to the trial protocol 8 and Russell standard, 12 participants who died or were known to have moved away from the study areas were excluded from the numerator and denominator, because their smoking status were not available at the final follow-up.
Statistical Analysis
We used t test for continuous variables and Pearson chi-square test for categorical variables to compare differences between stop smoking services in baseline characteristics and the use of cessation medications. The statistical significance was defined when the P value was at most 5%. We used multivariable logistic regression analyses to investigate the association between continuous smoking abstinence from 4 to 12 months and the type of smoking cessation services participants had accessed, adjusted for possible confounding factors. The confounding factors used in the multivariable analysis were age, sex, married or living with a partner, education level, unemployed or not, receipt of free prescription, previous quit attempts, managed to quit at least 4 weeks before, less than 10 cigarettes per day, first cigarette within 5 minutes after waking, living with a smoking partner, use of nicotine replacement therapy (NRT) or varenicline during 2 to 3 months after the quit date. The dependent variable was the prolonged CO-validated smoking abstinence from 4 to 12 months, and independent variables included type of stop smoking advisors (specialist vs. other), age, gender, marital status, level of education, in receipt of free prescription, previous quit attempts, level of nicotine dependence, and use of smoking cessation medications during 2 to 3 months after the quit date. Statistical analyses were conducted using Stata (version 13.1).
Results
The main characteristics of participants by type of service are shown in Table 1. There were no statistically significant differences between participants from specialist services and nonspecialist services in demographic characteristics and smoking variables at baseline. The average age of participants was 48 years, and 53% were female. The proportion of participants who were unemployed was 10%, and 57% were in receipt of free prescriptions. Most (89%) had previously attempted to quit smoking, and 18% were living with a smoking partner (Table 1).
Table 1.
The Participant Characteristics at Baseline by Service Type
| Specialist smoking cessation services (N = 1088) | Nonspecialist smoking cessation services (N = 316) | P | |
|---|---|---|---|
| Age: mean (SD) | 48.1 (13.9) | 47.0 (13.2) | .182 |
| Female: % (n) | 52.4 (570) | 53.8 (170) | .659 |
| Ethnicity—white: % (n) | 98.6 (1070) | 98.7 (312) | .875 |
| Married or living with a partner: % (n) | 62.6 (680) | 58.5 (185) | .190 |
| Education: % (n) | (N = 1074) | (N = 312) | |
| None | 20.4 (219) | 19.6 (61) | .479 |
| GCSE | 34.5 (371) | 34.9 (109) | |
| A-level | 17.8 (191) | 14.7 (46) | |
| Degree | 14.6 (157) | 18.3 (57) | |
| Unknown | 12.7 (136) | 12.5 (39) | |
| Employment status: % (n) | |||
| Paid employment | 50.9 (554) | 58.9 (186) | .135 |
| Unemployed | 10.5 (114) | 8.5 (27) | |
| Looking after home | 7.8 (85) | 6.0 (19) | |
| Retired | 20.7 (225) | 18.4 (58) | |
| Full time students | 1.5 (16) | 0.3 (1) | |
| Other | 8.6 (94) | 7.9 (25) | |
| Free prescriptiona: % (n) | 58.0 (625/1077) | 53.5 (165/310) | .132 |
| Any previous quit attempts: % (n) | 88.6 (963/1087) | 91.1 (288/316) | .200 |
| Cigarettes <10 per day before quitting: % (n) | 13.5 (147/1087) | 15.8 (50/316) | .300 |
| First cigarette within 5 minutes after waking up: % (n) | 42.9 (466/1087) | 39.9 (126/316) | .342 |
| The longest time managed to stay quit before, >4 weeks: % (n) | 72.6 (756/1041) | 67.8 (213/314) | .099 |
| Living with a smoking partner: % (n) | 18.2 (198) | 19.0 (60) | .750 |
GCSE = General Certificate of Secondary Education.aFree prescription—The charge for a single prescription is £8.05 in the United Kingdom. Some people are entitled to free prescriptions because of their age (60 or over, or under 16, or aged 16 to 18 in full-education), income (on Income Support or qualified via other benefits or tax credits), or medical condition.
Table 2 shows the use of smoking cessation medications during 2 and 3 months after the quit date. There were no statistically significant differences between specialist and nonspecialist services (as a combined category) for the use of any medications (74.2% vs. 72.5%), NRT (36.3% vs. 36.4%), or varenicline (40.6% vs. 36.4%). However, there were statistically significant differences in the use of NRT or varenicline across individual settings (Table 2). For example, participants from pharmacy settings were more likely to use NRT compared to participants from general practice (61.5% vs. 30.9%). The use of varenicline was 0.0% in participants from pharmacy settings, compared to 44.6% in those from general practice settings.
Table 2.
Use of Stop Smoking Medications During 2–3 Months
| Any cessation medications % (n) | Any nicotine replacement therapy % (n) | Varenicline % (n) | Total N | |
|---|---|---|---|---|
| Specialist services | 74.6 (812) | 36.3 (395) | 40.6% (442) | 1088 |
| All nonspecialist services | 72.5 (229) | 36.4 (115) | 36.4 (115) | 316 |
| General practice | 74.6 (164) | 30.9 (68) | 44.6 (98) | 220 |
| Health trainer | 70.2 (40) | 40.4 (23) | 29.8 (17) | 57 |
| Pharmacy | 64.1 (25) | 61.5 (24) | 0 (0) | 39 |
| Total | 74.2 (1041) | 36.3 (510) | 39.7 (557) | 1404 |
| Pearson chi-square test: | ||||
| Specialist services vs. all nonspecialist services | P = .439 | P = .977 | P = .176 | |
| Across different settings (specialist, general practice, health trainer, and pharmacy) | P = .445 | P = .003 | P < .001 | |
Some participants used more than one cessation medication during 2–3 months. The number of participants who did not use any cessation medications was the difference between the total number of participants and the number of participants who used any cessation medications. For example, 276 of the 1088 participants from specialist services did not use any cessation medications (ie, 1088 − 812 = 276).
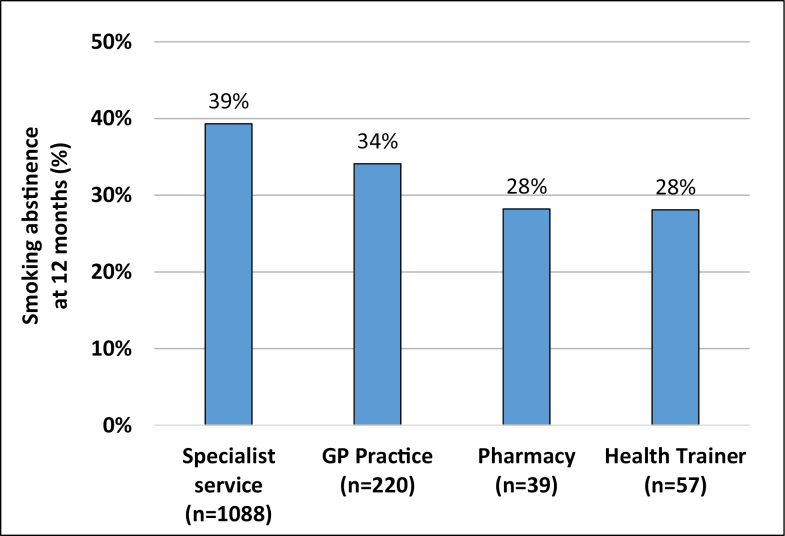
Figure 1 shows the rate of continuous abstinence from 4 to 12 months by type of stop smoking service, which was relatively high for specialist services (39.3%, 95% confidence interval [CI] = 36.5% to 42.3%), low for health trainers (28.1%, 95% CI = 17.7% to 41.5%) or pharmacies (28.2%, 95% CI = 15.9% to 44.9%), and intermediate for GP practices (34.1%, 95% CI = 28.1% to 40.7%). When nonspecialist services were combined, the rate of continuous smoking abstinence was higher in participants recruited from specialist services in comparison to the rate of abstinence in participants from nonspecialist services (39% vs. 32%; P = .023). If the outcome was defined as continuous abstinence from month 2 to 12, the difference in abstinence rate between specialist and nonspecialist services would be similar (34% vs. 27%; P = .018).
Figure 1.
Continuous abstinence from 4 to 12 months in short-term quitters, by type of smoking cessation advisors.
Results of multivariable logistic regression analysis are shown in Table 3. After adjusting for a range of participant characteristics and smoking variables, the specialist service was significantly associated with a higher rate of longer-term smoking abstinence (odds ratio: 1.48, 95% CI = 1.09% to 2.00%; P = .011). The longer-term smoking abstinence rate was positively associated with age (P = .016), married or living with a partner (P = .003), fewer than 10 cigarettes per day before quitting (P = .001), and use of NRT during 2–3 months (P = .001). Unemployment status (P = .056), smoking the first cigarette within 5 minutes after waking up (P = .068), and use of varenicline during 2–3 months (P = .060) tended to be associated with the longer-term smoking outcome, although the association was not statistically significant (Table 3).
Table 3.
Results of Multivariable Logistic Regression for Continuous Smoking Abstinence From 4 to 12 Months
| Odds ratio (95% CI) | P | |
|---|---|---|
| Specialist services vs. nonspecialist services | 1.477 (1.092, 1.997) | .011 |
| Age (y) | 1.013 (1.002, 1.023) | .016 |
| Female vs. male | 0.933 (0.723, 1.205) | .596 |
| Married or living with a partner vs. all other | 1.520 (1.158, 1.995) | .003 |
| Low education (up to GCSE vs. A-level or above) | 0.940 (0.726, 1.218) | .641 |
| Unemployed vs. all other | 0.634 (0.398, 1.012) | .056 |
| Free prescription vs. no free prescription | 0.898 (0.675, 1.195) | .461 |
| Any previous quit attempts vs. no previous quit attempt | 0.702 (0.439, 1.123) | .140 |
| Longest time managed to quit before: >4 weeks vs. ≤4 weeks | 1.770 (1.245, 2.517) | .001 |
| Cigarettes per day before quitting: <10 vs. ≥10 | 0.785 (0.605, 1.018) | .068 |
| First cigarette within 5 minutes after waking vs. >5 minutes | 0.817 (0.586, 1.140) | .235 |
| Living with a smoking partner vs. not living with a smoking partner | 0.888 (0.639, 1.236) | .480 |
| Use of NRT vs. no use of NRT during 2–3 months | 1.652 (1.214, 2.248) | .001 |
| Use of varenicline vs. no use of varenicline during 2–3 months | 1.335 (0.987, 1.805) | .060 |
CI = confidence interval; GCSE = General Certificate of Secondary Education; NRT = nicotine replacement therapy. The multivariable analysis used data from 1154 participants, and data from 250 participants were excluded from the analysis because of missing data from some independent variables. After including the treatment condition as an independent variable, the results of the logistic regression analysis remain materially unchanged.
Discussion
To the best of our knowledge, this is the first large scale study showing that short-term quitters after receiving cessation treatment from specialist advisors were less likely to relapse at 12 months compared to those treated in nonspecialist services. The difference in the proportion of smoking abstinence at 12 months was on average 7% between the specialist and nonspecialist services, which has important public health implications. Assuming the same quit rate (37%) at 4 weeks after the quit date, 3 the corresponding rate of prolonged abstinence from month 4 to 12 in people who set a quit date will be 14.4% and 11.8%, respectively. The difference in prolonged abstinence among people who set a quit date is likely to be larger than 2.6% if the support from specialist advisors is associated with a higher short-term quit rate than the support from nonspecialist advisors. 4
The observed difference in longer-term smoking abstinence between specialist and nonspecialist services in this study is unlikely to be caused by confounding factors. The association between smoking abstinence at 12 months and support from specialist advisors remained statistically significant after adjusting for participant characteristics, smoking history variables, and the use of smoking cessation medications (Table 2).
Previous studies have explored possible reasons for varying short-term outcomes by different smoking cessation settings and type of advisors in the English stop smoking services. Firstly, specialist advisors have received more training in smoking cessation counseling, compared to other health care professionals, 13 and a study found that success rates of smoking cessation treatment were associated with increased uptake of a national evidence-based training programme by advisors. 14 In addition to more extensive training, McDermott and colleagues 4 reported that specialist advisors received more supervision and showed greater adherence to evidence-based practice. Finally, it was found that group based sessions were more common in specialist centers than in other settings, 5 and support provided in specialist clinics may be more intensive, compared to that provided in nonspecialist settings. For example, smoking cessation treatment delivered by pharmacists in Glasgow was considered to be of “medium-intensity”. 15
The above reasons may also be pertinent in explaining the reduced risk of longer-term smoking relapse in short-term quitters who received support in specialist centers. Compared with nonspecialist support, behavioral support from specialist advisors might have provided more effective knowledge and skills for clients to cope with urges to smoke. It was found that reported attempts by participants to do something to cope with urges were associated with a lower risk of smoking relapse. 9 We further analyzed data and found that the proportion of participants who attempted to do something to cope with urges was 89.9% in participants from the specialist services and 84.5% in those from nonspecialist services.
Limitations
This was a secondary analysis of data from a trial, and it is possible that the effects observed are due to confounding factors that were not measured or adjusted for. The study recruited many more short-term quitters from specialist services (n = 1088) than from nonspecialist services (n = 316). Therefore, quitters from pharmacies, general practice, and health trainer services were combined in the main analysis and a comparison between different nonspecialist settings could not be conducted because of the small sample size. It also raises a question about the sample’s representativeness to all short-term quitters from nonspecialist smoking cessation services. In addition, the level of training and experience amongst staff who provide smoking cessation support in pharmacies, general practice, and health trainer services may be very different.
Implications for Practice and Research
Findings from this study suggest that support from specialist smoking cessation advisors is associated with not only an increased short-term quit success, but also a reduced longer-term smoking relapse risk among short-term quitters. The most meaningful public health target of smoking cessation programmes is a lowered prevalence of smoking in population, rather than simply a counting of short-term quitters most of whom will relapse in 12 months. Although smoking cessation support in any setting is cost-effective, 16 specialist counseling, as an intervention that improves longer-term outcomes, should be emphasized.
Findings from this study have important public health and clinical implications, as currently there is a lack of cost-effective interventions for the prevention of smoking relapse in short-term quitters. 17,18 In the English stop smoking services in 2012/2013, 33% of smokers motivated to quit received support in specialist clinics, 39% in primary care, 21% in pharmacy, and 7% in other settings. 3 The total number of people who set a quit date in nonspecialist services was 485 245 in 2012/2013 in England. 3 If the rate of prolonged abstinence was increased by 2.6%, there would be 12 616 more people who were abstinent at 12 months. Therefore the use of specialist smoking cessation services should be encouraged to result in more quitters with longer-term abstinence. However, it should be stressed that smoking cessation support from nonspecialist advisors is still cost-effective. 16 A large proportion of smokers motivated to quit have chosen to receive cessation support from general practice, pharmacy, and other nonspecialist advisors, based on individual preferences, such as perceived convenience. Health care professionals who provide smoking cessation counseling in nonspecialist settings should receive more training, or be allowed more time to provide smoking cessation counseling, in order to improve short-term and longer-term outcomes. Further research is needed to investigate reasons for the difference in longer term outcomes between specialist and nonspecialist cessation support, and whether enhancing generalist skills in nonspecialist advisors can reduce longer term relapse.
In summary, longer-term smoking relapse appeared to be reduced in smokers who received support from specialist smoking cessation advisors, compared with those who received support from nonspecialist advisors.
Supplementary Material
Supplementary Material can be found online at http://www.ntr.oxfordjournals.org
Funding
This project was funded by the NIHR Health Technology Assessment programme (Project HTA09/91/36). Visit the HTA programme website for more details www.hta.ac.uk/link to project page. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Department of Health. We acknowledge the support of the National Institute for Health Research, through the Primary Care Research Network. PA is funded by UK Centre for Tobacco Control Studies (a UKCRC Public Health Research Centre of Excellence) which receives funding from British Heart Foundation, Cancer Research UK, Economic and Social research Council, Medical Research Council, and the Department of Health (grant number MR/K23195/1).
Declaration of Interests
PA has done ad hoc consultancy and research for the pharmaceutical industry on smoking cessation. THB has received research funding and study medication from Pfizer, Inc. No other competing interest declared; no other relationships or activities that could appear to have influenced the submitted work.
Supplementary Material
Acknowledgments
FS, PA, THB, RH, GRB, MOB, and SS designed the trial and developed study protocol. VM and AB coordinated the trial and contributed to project management. AB, VM, TJB and CN contributed to participant recruitment, follow-up interviews, and data collection. FS analyzed data and drafted the manuscript. All authors contributed to the interpretation of results, and commented on the draft manuscript. We thank staff from NHS Norfolk and Norfolk Community Health & Care NHS Trust for providing advice on the development of the trial protocol. We thank stop smoking advisors from NHS stop smoking services in Norfolk, Lincolnshire, Suffolk, Hertfordshire, Great Yarmouth, and Waveney for recruiting quitters to the study. The trial was conducted in collaboration with the Norwich Clinical Trials Unit whose staff provided input into the design, conduct and analysis (Tony Dyer—randomization and data management, Garry Barton—health economics). We thank Laura Vincent for providing administrative support, data entering and data checking.
References
- 1. Zwar NA, Mendelsohn CP, Richmond RL. Supporting smoking cessation. BMJ. 2014;348:f7535. doi:10.1136/bmj.f7535. [DOI] [PubMed] [Google Scholar]
- 2. West R, May S, West M, Croghan E, McEwen A. Performance of English stop smoking services in first 10 years: analysis of service monitoring data. BMJ. 2013;347:f4921. doi:10.1136/bmj.f4921. [DOI] [PubMed] [Google Scholar]
- 3. NHS. Statistics on NHS Stop Smoking Services: England, April 2012–March 2013. Lifestyle Statistics, Health and Social Care Information Centre; 2013. http://whyquit.com/NRT/UK/2012_NHS_SSS_Statistics.pdf. Accessed March 16, 2015. [Google Scholar]
- 4. McDermott MS, Beard E, Brose LS, West R, McEwen A. Factors associated with differences in quit rates between “specialist” and “community” stop-smoking practitioners in the english stop-smoking services. Nicotine Tob Res. 2013;15(7):1239–1247. doi:10.1093/ntr/nts262. [DOI] [PubMed] [Google Scholar]
- 5. McEwen A, West R, McRobbie H. Effectiveness of specialist group treatment for smoking cessation vs. one-to-one treatment in primary care. Addict Behav. 2006;31(9):1650–1660. doi:10.1016/j.addbeh.2005.12.014. [DOI] [PubMed] [Google Scholar]
- 6. Hiscock R, Murray S, Brose LS, et al. Behavioural therapy for smoking cessation: the effectiveness of different intervention types for disadvantaged and affluent smokers. Addict Behav. 2013;38(11):2787–2796. doi:10.1016/j.addbeh.2013.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hughes JR, Keely J, Naud S. Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction. 2004;99(1):29–38. doi:10.1111/j.1360-0443.2004.00540.x. [DOI] [PubMed] [Google Scholar]
- 8. Song F, Holland R, Barton GR, et al. Self-help materials for the prevention of smoking relapse: study protocol for a randomized controlled trial. Trials. 2012;13:69. doi:10.1186/1745-6215-13-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Blyth A, Maskrey V, Notley C, et al. Effectiveness and economic evaluation of self-help educational materials for the prevention of smoking relapse: randomised controlled trial (SHARPISH). Health Technol Assess. 2015;19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Department of Health. NHS Stop Smoking Services: Service and Monitoring Guidance 2010/11. London, United Kingdom: Department of Health; 2009. http://webarchive.nationalarchives.gov.uk/20130107105354/http://dh.gov.uk/en/publicationsandstatistics/publications/publicationspolicyandguidance/dh_109696. Accessed March 16, 2015. [Google Scholar]
- 11. Michie S, Rumsey N, Fussell A, et al. Improving Health: Changing Behaviour. NHS Health Trainer Handbook. London, United Kingdom: Department of Health; 2008. http://healthtrainersengland.com/wp-content/uploads/2014/05/NHSHealthTrainerHandbook.pdf. Accessed March 16, 2015. [Google Scholar]
- 12. West R, Hajek P, Stead L, Stapleton J. Outcome criteria in smoking cessation trials: proposal for a common standard. Addiction. 2005;100(3):299–303. doi:10.1111/j.1360-0443.2004.00995.x. [DOI] [PubMed] [Google Scholar]
- 13. McDermott MS, West R, Brose LS, McEwen A. Self-reported practices, attitudes and levels of training of practitioners in the English NHS Stop Smoking Services. Addict Behav. 2012;37(4):498–506. doi:10.1016/j.addbeh.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 14. Brose LS, West R, Michie S, McEwen A. Changes in success rates of smoking cessation treatment associated with take up of a national evidence-based training programme. Prev Med. 2014;69C:1–4. doi:10.1016/j.ypmed.2014.08.021. [DOI] [PubMed] [Google Scholar]
- 15. Bauld L, Boyd KA, Briggs AH, et al. One-year outcomes and a cost-effectiveness analysis for smokers accessing group-based and pharmacy-led cessation services. Nicotine Tob Res. 2011;13(2):135–145. doi:10.1093/ntr/ntq222. [DOI] [PubMed] [Google Scholar]
- 16. Godfrey C, Parrott S, Coleman T, Pound E. The cost-effectiveness of the English smoking treatment services: evidence from practice. Addiction. 2005;100(suppl 2):70–83. doi:10.1111/j.1360-0443.2005.00916.x. [DOI] [PubMed] [Google Scholar]
- 17. Hajek P, Stead LF, West R, Jarvis M, Hartmann-Boyce J, Lancaster T. Relapse prevention interventions for smoking cessation. Cochrane Database Syst Rev. 2013;8:CD003999. doi:10.1002/14651858.CD003999.pub4. [DOI] [PubMed] [Google Scholar]
- 18. Coleman T, Agboola S, Leonardi-Bee J, Taylor M, McEwen A, McNeill A. Relapse prevention in UK Stop Smoking Services: current practice, systematic reviews of effectiveness and cost-effectiveness analysis. Health Technol Assess. 2010;14:1–152, iii-iv. doi:10.3310/hta14490. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.