Abstract
Background
Readmission rates of psychiatric inpatients are higher in South Korea than other Organization for Economic Co-operation and Development (OECD) countries. In addition, the solution for readmission control is deficient based on the characteristics of the South Korean National Health Insurance (NHI) system. Therefore, it is necessary to identify ways to reduce psychiatric inpatient readmissions. This study investigated the relationship between inpatient volume per psychiatrist and the readmission rate of psychiatric inpatients in South Korea.
Method
We used NHI claim data (N = 37,796) from 53 hospitals to analyze readmission within 30 days for five diagnosis (organic mental disorders, mental and behavioral disorders due to psychoactive substance use, schizophrenia, mood disorders, neurotic disorders, and stress-related and somatoform disorders) between 2010 and 2013. We performed χ2 and analysis of variance tests to investigate associations between patient and hospital-level variables and readmission within 30 days. Finally, generalized estimating equation (GEE) models were analyzed to examine possible associations with readmission.
Results
Readmissions within 30 days accounted for 1,598 (4.5 %) claims. Multilevel analysis demonstrated that inpatient volume per psychiatrist were inversely related with readmission within 30 days (low odds ratio [OR]: 0.38, 95 % confidence interval [CI]: 0.28–0.51; mid-low OR: 0.48, 95 % CI: 0.36–0.63; mid-high OR: 0.55, 95 % CI: 0.44–0.69; Q4 = ref). The subgroup analysis by diagnosis revealed that both “schizophrenia, schizotypal, and delusional disorders” and “mood disorders” had inverse relationships with readmission risk for all volume groups.
Conclusions
We observed an inverse association between inpatient volume per psychiatrist and the 30-day readmission rate of psychiatric inpatients, suggesting that it could be a useful quality indicator in mental health care.
Keywords: Patient volume, Quality of care, Readmission, Psychiatric care
Background
In South Korea, readmission is a key issue for controlling health care costs from increasing. However, readmission rates have gradually increased, especially for mental health care. It adversely affects patients and increases the cost burden on National Health Insurance (NHI) systems. Thus, readmission is considered a quality indicator for inpatient services [1]. Based on the Organization for Economic Co-operation and Development (OECD) Health at a Glance 2013 data, the readmission rate of psychiatric inpatients in South Korea was greater than those in other OECD countries (readmissions for schizophrenia in South Korea, 2011: 19.4 %; OECD average: 12.3 %) [2].
Many health care professionals and researchers have investigated ways to reduce inpatient readmission. These studies reported that risk of readmission in this patient group is positively associated with a history of previous readmission, length of stay (LOS), and comorbidity, but were inversely associated with substance abuse, and hospital volume [3–9]. Among those, hospital volume was generally considered to be associated with better health care quality. Regarding the volume-outcome relationship, higher volume could be helpful in the improvement of skills and the outcomes were improved [10, 11]. However, excessive volume may be a cause of overload in hospital staffing, and most publications that describe a volume-outcome relationship only analyzed health care requiring surgical procedures; they did not assess psychiatric health care. The characteristics of medical treatment in mental health services are different from other specialties. Given that psychiatrist treatment largely involves patient interview sessions rather than surgical procedures, such treatments would differently affect psychiatrist`s workload compared to other specialty areas. Consequently, the reduction in the quality of care for psychiatric disorder can be caused by such association. Hence readmission, a healthcare quality indicator, can increase because patients are unable to receive appropriate treatment due to a reduction in the quality of care [12–15]. This suggests that the volume-outcome relationship is not applicable to all areas of medical treatment.
Although the problem of psychiatric readmission rates in South Korea was worse than other countries, since South Korea had FFS (fee for service) payment system for psychiatric disorder, the solution for control of the readmission of psychiatric inpatients were deficient by the characteristics of NHI system in South Korea [16, 17]. To the best of our knowledge, no studies about patient volume per psychiatrist have been conducted in South Korea. Therefore, it is necessary to investigate how patient volumes per psychiatrist affect psychiatric inpatient admissions in order to improve outcomes and reduce medical costs.
Methods
Study population
There were about 1,730 hospitals including 39 public hospitals during 2010–2013 in South Korea. We projected that this might cause baseline imbalances due to differences in hospital characteristics because the number of public hospitals was only about 2.3 % among the total number of hospitals in South Korea. To reduce bias caused by the observed covariates and to deal with the usual baseline imbalances across hospitals, the data used in this study only included 156 hospitals (117 private vs 39 public) that were extracted using the propensity score matching-methods (1:3), conducted based on the nearest neighbor methods while adjusting for hospital characteristics including hospital location, nursing staffing level, number of total beds, number of intensive care unit beds, number of emergency room beds, and number of doctors [18]. Among 156 hospitals, we only analyzed hospitalization cases of the five most frequent diagnostic categories among overall psychiatric disorder that classified diagnoses according to International Classification of Diseases groupings (ICD-10: F0.x-F4.x) to reflect specific clinical mechanisms as follows: “organic, including symptomatic, mental disorders (F0.x)”, “mental and behavioral disorders due to psychoactive substance use (F1.x)”, “schizophrenia, schizotypal, and delusional disorders (F2.x)”, “mood disorders (F3.x)”, and “neurotic, stress-related and somatoform disorders (F4.x)”. Therefore, we excluded the 103 hospitals without hospitalization cases for the major five psychiatric disorders. Then, we excluded 3,014 cases with missing values for the variables of interest. Finally, we used NHI claim data from 53 hospitals to analyze readmission rates of psychiatric inpatients within 30 days of discharge. These data were collected between 2010 and 2013 and included 37,796 hospitalizations in 53 hospitals. The unit of analysis was hospitalization rather than patient (Fig. 1).
Fig. 1.
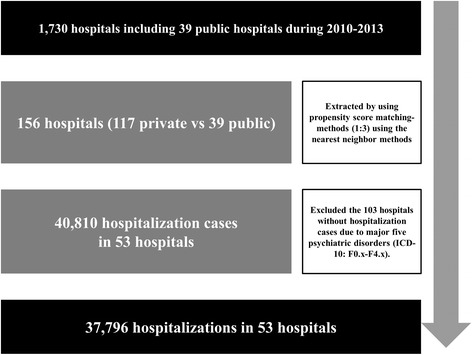
Selection of study population
Ethics statement
Out study utilized secondary data reported on the aggregate level, and each case in our dataset was converted to random number for preventing identification. Therefore, it was not necessary to obtain research ethics approval.
Variables
The outcome variable in this study was readmission within 30 days due to same diagnosis after discharge for psychiatric disorders, were included in this study (F0.x-F4.x). Each patient’s first discharge in a given calendar date was considered the index discharge, and readmissions due to same diagnosis within 30 calendar days from the index discharge were defined as readmission.
The primary variable of interest in relation to readmission within 30 days of discharge was inpatient volume per psychiatrist, which was defined as the sum of LOS for all mental disorders per hospital/number of psychiatrists per hospital [19]. We assumed that there were substantial differences in risk of readmission, the outcome variable, by inpatient volume per psychiatrist in a U-shape curve. This is because higher volume in hospital could have a positive role on patient`s outcomes by increasing experiences and developing medical skills in doctors based on a volume-outcome relationship, but excessive patient volume also could negatively affect patient outcomes [12, 20, 21]. Thus, inpatient volume per psychiatrist was categorized into quartiles for analysis to reflect differences by variation of inpatient volume per psychiatrist (Q1 = low inpatient volume per psychiatrist; < 1282.0 days, Q2 = mid-low inpatient volume per psychiatrist; 1282.0–1927.2 days, Q3 = mid-high inpatient volume per psychiatrist; 1927.3–3494.9 days, Q4 = high inpatient volume per psychiatrist; more than 3495.0 days per 1 psychiatrist for 1 year) [15, 22].
We adjusted for both patient and hospital-level variables when analyzing the relationship between inpatient volume per psychiatrist and psychiatric inpatient readmission. To adjust patient demographic and clinical characteristics, patient-level variables included in the analysis were: diagnosis, LOS, sex, age, and year. Age was classified into 10-years intervals. Diagnoses were classified using ICD-10 codes F0.x-F4.x to reflect specific clinical mechanisms. LOS was included to reflect severity of each patient. We categorized it based on its median value in our study (median: 14 days, interquartile range [IQR]: 25 days) [23].
Hospital-level variables encompassed both human resource variables and structural characteristics: numbers of psychiatrists, pharmacists, nurses, and beds; proportion and occupancy rate of psychiatric beds; teaching and ownership status; and type of medical institution. The proportion of psychiatric beds was defined as a percentage of the number of psychiatric beds among the number of total beds.
The occupancy rate of psychiatric beds was calculated as the total number of inpatients days due to psychiatric disorder (ICD-10: Fx.x) for each year divided by the number of available psychiatric beds for each year [24]. This indicator was used to consider situations related to economic issues which could affect to readmission for profit in each hospital, and was calculated as shown in the following equations:
In addition, teaching status, ownership status, and type of medical institution were included to reflect the differences by hospital structural characteristics [25, 26].
Statistical analysis
We first examined the distribution of each categorical variable by examining frequencies and percentages and performing χ2 tests to investigate associations with psychiatric inpatient readmission within 30 days. These analyses were performed for both patient- and hospital-level variables. Next, analyses of variances (ANOVAs) were carried out to compare the average values and standard deviations for continuous hospital-level variables. Third, to examine associations with readmission within 30 days after discharge for 5 types of psychiatric disorder, we performed logistic regression analysis using generalized estimating equation (GEE) model with link logit including both inpatient- and hospital-level variables, because the data used in this study was hierarchically structured and had binary outcome variables. This GEE model assumed that with proper distributions for each hospitalization case while taking into account the correlation among hospitalization cases within the hospitals. In this study, the correlation structure was modeled as exchangeable correlation structure [27, 28]. Finally, subgroup analyses for associations with readmission within 30 days were also performed according to diagnosis. All statistical analyses were performed using SAS statistical software version 9.2 (SAS Institute Inc., Cary, NC). All P-values were two-sided and considered significant at P < 0.05.
Results
The data used in this analysis included 35,884 hospitalizations. Among them, 1,598 (4.5 %) were psychiatric inpatient readmissions within 30 days. Table 1 shows univariate associations between various patient-level variables and readmission within 30 days. In terms of diagnoses, “schizophrenia, schizotypal, and delusional disorders” were the most frequent causes of readmission within 30 days (10.5 %) compared to other mental disorders. Patients hospitalized for more than 14 days had higher readmission rates than those with shorter hospitalizations (<14 days: 1.8 %, ≥14 days: 6.6 %). The readmission rate for males was higher than that for females (males: 6.5 %, females: 2.8 %). Finally, readmission rates gradually increased over time. The high inpatient volume group’s psychiatric inpatients had higher readmission rates than the other inpatient volume groups (low: 1.7 %, mid-low: 1.8 %, mid-high: 2.6 %, 10 high: 11.5 %).
Table 1.
Univariate associations between readmission within 30 days of discharge and various patient-level variables
| Variables | Total (N = 35,884) | Low inpatient volumes per psychiatrist (n = 8,969) | Mid-low inpatient volumes per psychiatrist (n = 8,909) | Mid-high inpatient volumes per psychiatrist (n = 9,186) | High inpatient volumes per psychiatrist (n = 9,042) | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Readmission | No readmission | P-value | Readmission | No readmission | P-value | Readmission | No readmission | P-value | Readmission | No readmission | P-value | Readmission | No readmission | P-value | |||||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | ||||||
| Diagnosis | |||||||||||||||||||||||||
| Organic, including symptomatic, mental disorders | 121 | 3.2 | 3,690 | 96.8 | <.0001 | 6 | 0.5 | 1,173 | 99.5 | <.0001 | 11 | 1.5 | 738 | 98.5 | 0.1191 | 25 | 3.0 | 815 | 97.0 | <.0001 | 79 | 7.6 | 964 | 92.4 | <.0001 |
| Mental and behavioral disorders due to psychoactive substance use | 288 | 4.7 | 5,875 | 95.3 | 30 | 1.7 | 1,713 | 98.3 | 40 | 2.5 | 1,542 | 97.5 | 38 | 3.2 | 1,143 | 96.8 | 180 | 10.9 | 1,477 | 89.1 | |||||
| Schizophrenia, schizotypal, and delusional disorders | 797 | 10.5 | 6,802 | 89.5 | 37 | 3.1 | 1,148 | 96.9 | 35 | 2.0 | 1,759 | 98.0 | 94 | 4.7 | 1,918 | 95.3 | 631 | 24.2 | 1,977 | 75.8 | |||||
| Mood disorders | 274 | 2.1 | 12,603 | 97.9 | 50 | 1.6 | 3,067 | 98.4 | 50 | 1.5 | 3,329 | 98.5 | 63 | 1.8 | 3,514 | 98.2 | 111 | 4.0 | 2,693 | 96.0 | |||||
| Neurotic, stress-related, and somatoform disorders | 118 | 2.2 | 5,316 | 97.8 | 30 | 1.7 | 1,715 | 98.3 | 26 | 1.9 | 1,379 | 98.1 | 23 | 1.7 | 1,331 | 98.3 | 39 | 4.2 | 891 | 95.8 | |||||
| Length of stay (days) | |||||||||||||||||||||||||
| < 14 | 292 | 1.8 | 15,895 | 98.2 | <.0001 | 74 | 1.4 | 5,106 | 98.6 | 0.0177 | 74 | 1.8 | 3,927 | 98.2 | 0.8425 | 64 | 1.8 | 3,452 | 98.2 | <.0001 | 80 | 2.3 | 3,410 | 97.7 | <.0001 |
| ≥ 14 | 1,306 | 6.6 | 18,391 | 93.4 | 79 | 2.1 | 3,710 | 97.9 | 88 | 1.8 | 4,820 | 98.2 | 179 | 3.3 | 5,269 | 96.7 | 960 | 17.3 | 4,592 | 82.7 | |||||
| Sex | |||||||||||||||||||||||||
| Male | 1,029 | 6.5 | 14,807 | 93.5 | <.0001 | 70 | 1.9 | 3,610 | 98.1 | 0.2311 | 74 | 2.0 | 3,660 | 98.0 | 0.3268 | 157 | 4.3 | 3,518 | 95.7 | 0.3268 | 728 | 15.3 | 4,019 | 84.7 | <.0001 |
| Female | 569 | 2.8 | 19,479 | 97.2 | 83 | 1.6 | 5,206 | 98.4 | 88 | 1.7 | 5,087 | 98.3 | 86 | 1.6 | 5,203 | 98.4 | 312 | 7.3 | 3,983 | 92.7 | |||||
| Age (years) | |||||||||||||||||||||||||
| ≤ 29 | 124 | 2.0 | 6,150 | 98.0 | <.0001 | 28 | 1.7 | 1,593 | 98.3 | 0.0156 | 27 | 1.5 | 1,828 | 98.5 | 0.1145 | 31 | 1.9 | 1,582 | 98.1 | <.0001 | 38 | 3.2 | 1,147 | 96.8 | <.0001 |
| 30–39 | 228 | 4.4 | 4,919 | 95.6 | 31 | 2.7 | 1,120 | 97.3 | 32 | 2.3 | 1,375 | 97.7 | 51 | 4.0 | 1,216 | 96.0 | 114 | 8.6 | 1,208 | 91.4 | |||||
| 40–49 | 369 | 5.8 | 6,029 | 94.2 | 29 | 2.0 | 1,444 | 98.0 | 34 | 2.1 | 1,564 | 97.9 | 35 | 2.3 | 1,461 | 97.7 | 271 | 14.8 | 1,560 | 85.2 | |||||
| 50–59 | 345 | 4.9 | 6,701 | 95.1 | 25 | 1.4 | 1,736 | 98.6 | 36 | 2.2 | 1,635 | 97.8 | 52 | 2.9 | 1,745 | 97.1 | 232 | 12.8 | 1,585 | 87.2 | |||||
| 60–69 | 345 | 6.5 | 4,946 | 93.5 | 25 | 1.8 | 1,333 | 98.2 | 20 | 1.7 | 1,136 | 98.3 | 52 | 3.8 | 1,317 | 96.2 | 248 | 17.6 | 1,160 | 82.4 | |||||
| 70–79 | 187 | 3.3 | 5,541 | 96.7 | 15 | 0.9 | 1,590 | 99.1 | 13 | 1.1 | 1,209 | 98.9 | 22 | 1.5 | 1,400 | 98.5 | 137 | 9.3 | 1,342 | 90.7 | |||||
| Year | |||||||||||||||||||||||||
| 2010 | 120 | 2.3 | 5,124 | 97.7 | <.0001 | 17 | 0.7 | 2,396 | 99.3 | <.0001 | 27 | 1.4 | 1,837 | 98.6 | <.0001 | 8 | 1.4 | 561 | 98.6 | <.0001 | 68 | 17.1 | 330 | 82.9 | <.0001 |
| 2011 | 363 | 3.1 | 11,385 | 96.9 | 16 | 1.0 | 1,618 | 99.0 | 31 | 1.1 | 2,762 | 98.9 | 46 | 1.1 | 4,224 | 98.9 | 270 | 7.3 | 3,408 | 92.7 | |||||
| 2012 | 702 | 5.4 | 12,242 | 94.6 | 15 | 1.0 | 1,442 | 99.0 | 43 | 1.7 | 2,494 | 98.3 | 66 | 1.8 | 3,597 | 98.2 | 578 | 12.4 | 4,082 | 87.6 | |||||
| 2013 | 413 | 6.9 | 5,535 | 93.1 | 105 | 3.0 | 3,360 | 97.0 | 61 | 3.6 | 1,654 | 96.4 | 123 | 18.0 | 561 | 82.0 | 124 | 40.5 | 182 | 59.5 | |||||
| Total | 1,598 | 4.5 | 34,286 | 95.5 | 153 | 1.7 | 8,816 | 98.3 | 162 | 1.8 | 8,747 | 98.2 | 243 | 2.6 | 8,943 | 97.4 | 1,040 | 11.5 | 8,002 | 88.5 | |||||
Table 2 shows the distribution of hospital-level variables. The average number of psychiatrists, nurses, and pharmacists were 2.9 (SD: 1.6), 8.6 (SD: 9.1), and 224.4 (SD: 165.7), respectively. The mean number of total beds was 461.5 (SD: 208.8), and the average occupancy rate of psychiatric beds was 20.1 % (SD: 47.2). There were fewer nonteaching hospitals in our sample (n = 17) than teaching hospitals (n = 36), and there were more private hospitals (n = 39) than public hospitals (n = 14). Finally, there were more general hospitals (n = 48) than hospitals (n = 5).
Table 2.
Hospital-level characteristics
| n/Mean | %/SD | |
|---|---|---|
| Number of psychiatrists | 2.9 | ±1.6 |
| Number of pharmacists | 8.6 | ±9.1 |
| Number of nurses | 222.4 | ±165.7 |
| Number of beds | 461.5 | ±208.8 |
| Proportion of psychiatric beds (%) | 8.3 | ±14.2 |
| Psychiatric bed occupancy rate (%) | 20.1 | ±47.2 |
| Teaching status | ||
| Nonteaching hospital | 17 | 32.1 % |
| Teaching hospital | 36 | 67.9 % |
| Ownership | ||
| Public | 14 | 26.4 % |
| Private | 39 | 73.6 % |
| Type of medical institution | ||
| Hospital | 5 | 9.4 % |
| General hospital | 48 | 90.6 % |
| Total | 53 | 100.0 |
A logistic regression analysis using GEE model considering both patient- and hospital-level variables revealed that patients with diagnoses of “schizophrenia, schizotypal, and delusional disorders (ICD-10: F2.x)” had a higher risk of readmission within 30 days compared to other mental disorders (odds ratio [OR]: 3.86, 95 % confidence interval [CI]: 2.78–5.36). Patients hospitalized for more than 14 days had a lower risk of readmission within 30 days than those hospitalized for shorter periods (OR: 0.40, 95 % CI: 0.33–0.49). Females had a lower risk of readmission than males (OR: 0.63, 95 % CI: 0.54–0.74). Over the 4 years of data included in the study, the risk for readmission gradually increased. In terms of hospital-level variables, inpatients at hospitals with low inpatient volume per psychiatrist had low risk of readmission than those with high inpatient volume (low OR: 0.38, 95 % CI: 0.28–0.51; mid-low OR: 0.48, 95 % CI: 0.36–0.63; mid-high OR: 0.55, 95 % CI: 0.44–0.69; Q4 = ref). In addition, risk of readmission had a positive trend with inpatient volume (P for trend < .001). Patients treated at hospitals with more psychiatrists or more pharmacists had a lower risk of readmission within 30 days (number of psychiatrists OR: 0.87, 95 % CI: 0.80–0.95 per psychiatrist; number of pharmacists OR: 0.94, 95 % CI: 0.92–0.96 per pharmacist). Similarly, the number of nurses was associated with a lower risk of 30-day readmission (number of nurses OR: 0.98, 95 % CI: 0.96–0.99 per 10 nurses). A higher number of total beds and greater proportion of psychiatric beds were both associated with a higher risk of readmission within 30 days (number of beds OR: 1.48, 95 % CI: 1.35–1.63 per 100 increase in the number of beds; proportion of psychiatric beds OR: 1.08, 95 % CI: 1.02–1.15 per 10 % increase in the proportion of psychiatric beds). With regard to structural characteristics, patients at private hospitals had a higher readmission risk than those at public hospitals (OR: 3.00, 95 % CI: 2.41–3.74). In contrast, patients treated at general hospitals had a lower risk of readmission within 30 days than patients at hospitals among types of medical institution (OR: 0.35, 95 % CI: 0.27–0.47) (Table 3).
Table 3.
Factors associated with readmission within 30 days of discharge for 5 types of psychiatric disorder, derived from a GEE model
| OR | 95 % CI | ||
|---|---|---|---|
| Patient-level | |||
| Diagnosis | |||
| Organic, including symptomatic, mental disorders | 1.00 | – | – |
| Mental and behavioral disorders due to psychoactive substance use | 1.56 | 1.10 | 2.22 |
| Schizophrenia, schizotypal, and delusional disorders | 3.86 | 2.78 | 5.36 |
| Mood disorders | 1.10 | 0.79 | 1.54 |
| Neurotic, stress-related, and somatoform disorders | 1.35 | 0.92 | 2.00 |
| Length of stay (days) | |||
| < 14 | 1.00 | – | – |
| ≥ 14 | 0.40 | 0.33 | 0.49 |
| Sex | |||
| Male | 1.00 | – | – |
| Female | 0.63 | 0.54 | 0.74 |
| Age (years) | |||
| ≤ 29 | 1.00 | – | – |
| 30–39 | 1.37 | 1.00 | 1.86 |
| 40–49 | 1.56 | 1.17 | 2.07 |
| 50–59 | 1.82 | 1.36 | 2.43 |
| 60–69 | 2.27 | 1.69 | 3.05 |
| 70–79 | 1.28 | 0.91 | 1.81 |
| Year | |||
| 2010 | 1.00 | – | – |
| 2011 | 1.26 | 0.92 | 1.74 |
| 2012 | 1.97 | 1.45 | 2.68 |
| 2013 | 4.61 | 3.35 | 6.35 |
| Hospital-level | |||
| Inpatient volumes per psychiatrist | |||
| Low | 0.38 | 0.28 | 0.51 |
| Mid-low | 0.48 | 0.36 | 0.63 |
| Mid-high | 0.55 | 0.44 | 0.69 |
| High | 1.00 | – | – |
| Number of psychiatrists | 0.87 | 0.80 | 0.95 |
| Number of pharmacists | 0.94 | 0.92 | 0.96 |
| Number of nurses (per 10 nurse increase) | 0.98 | 0.96 | 0.99 |
| Number of beds (per 100 bed increase) | 1.48 | 1.35 | 1.63 |
| Proportion of psychiatric beds (per 10 % increase) | 1.08 | 1.02 | 1.15 |
| Psychiatric bed occupancy rate (per 10 % increase) | 0.99 | 0.97 | 1.00 |
| Teaching status | |||
| Nonteaching hospital | 1.39 | 1.00 | 1.91 |
| Teaching hospital | 1.00 | – | – |
| Ownership | |||
| Public | 1.00 | – | – |
| Private | 3.00 | 2.41 | 3.74 |
| Type of medical institution | |||
| Hospital | 1.00 | – | – |
| General hospital | 0.35 | 0.27 | 0.47 |
Abbreviations: CI confidence interval, OR odds ratio
We performed an additional analysis investigating the association between inpatient volume per psychiatrist and patient readmission within 30 days after stratifying by each diagnosis. We observed a general positive association between inpatient volume per psychiatrist and readmission risk in all diagnosis groups. In particular, higher inpatient volume per psychiatrist group had higher risk for readmission due to “schizophrenia, schizotypal, and delusional disorders” and “mood disorders” diagnostic groups (“schizophrenia, schizotypal, and delusional disorders”: low OR: 0.29, 95 % CI: 0.15–0.56; mid-low OR: 0.27, 95 % CI: 0.15–0.50; mid-high OR: 0.45, 95 % CI: 0.29–0.70, Q4 = ref) (“mood disorders”: low OR: 0.28, 95 % CI: 0.14–0.53; mid-low OR: 0.47, 95 % CI: 0.27–0.84; mid-high OR: 0.49, 95 % CI: 0.32–0.77, Q4 = ref) (Fig. 2).
Fig. 2.
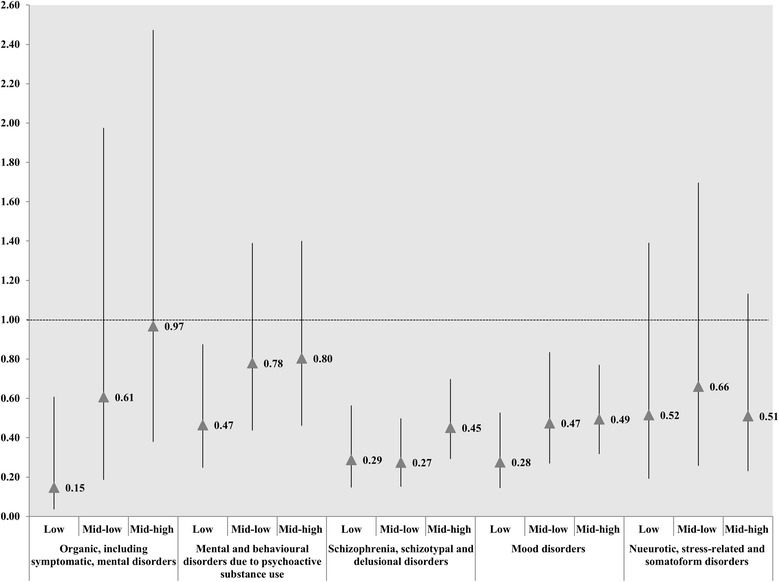
Odds ratios for inpatient volumes per psychiatrist associated with readmission within 30 days of discharge, stratified by diagnosis * High inpatient volumes per psychiatrist was reference group. † the OR is marked as triangle point; and results were statistically significant if each bar as marked to SD is not reached the cutoff line in 1.00
Discussion
Readmission is considered a quality indicator for treatment, and high levels of readmission increase cost. Many studies have been conducted to assess the reasons for readmission, which is a major contributor to health care cost. In particular, the readmission of psychiatric inpatients in South Korea was higher than that of other OECD countries [2]. In the present study, we analyzed the relationship between readmission within 30 days of discharge for psychiatric disorders and inpatient volume per psychiatrist, hospital characteristics, and human resource variables. We found evidence that inpatient volume per psychiatrist was positively associated with psychiatric inpatient readmission within 30 days (Q1 OR: 0.38, 95 % CI: 0.29–0.50; Q2 OR: 0.44, 95 % CI: 0.34–0.59; Q3 OR: 0.57, 95 % CI: 0.46–0.71; Q4 = ref), not volume-outcome relationship in any level. Generally, psychiatrists with low inpatient volume (less than 1282.0 days for 1 year) had better quality in psychiatric inpatient care except patient with “neurotic, stress-related, and somatoform disorders”. In particular, those relationships were statistically significant in “schizophrenia, schizotypal, and delusional disorders” and “mood disorders”. However, in other diagnostic groups, there were just positive trends rather than statistically significant associations. It may be caused by a lack of statistical power.
Many previous studies that examined volume-outcome relationships found that better health care outcomes were associated with many patient volumes in hospitals [29, 30]. However, such studies were performed by subjecting surgical patients in surgical field. In those health care fields including surgery, physicians with high inpatient volume were found to have higher skill levels. On the other hand, psychiatrist treatment largely involves patient interview session rather than surgical procedure. Therefore, a high patient volume could cause mental fatigue for psychiatrists [31–34]. Higher level of psychiatrist burnout could contribute to poorer mental health care outcome. Although previous study in nonsurgical field demonstrated that high volume was positively associated with the risk in adverse events as readmission, our findings focused to psychiatric inpatient care in contrast with those of previous studies [35].
A few studies outside of South Korea have assessed the relationship between inpatient volume per psychiatrist and readmission within 30 days [13, 14, 36]. In those studies, similar results with our findings were shown. However, they were just analyzed in other countries, not South Korea. Thus, our results provide information that health policy makers and health care providers could use to reduce the readmission rate of psychiatric inpatients in South Korea.
Based on our findings, health policy makers should consider how to improve mental health care quality. Due to health care system characteristics like FFS, there are limited ways to control readmission [37]. Because health care providers receive payment for each treatment they provide, there is limited incentive to reduce readmission. As a result, inpatient readmission in South Korea has been difficult to control. However, our findings provide new evidence that health policy makers can use to revise policies. Our results suggest that the inpatient volume had an inverse association with patient`s outcome. We are not sure about the optimal values of inpatient volume per psychiatrist for maximizing the efficiency of psychiatric care, but there is a need to manage psychiatrist`s workload as appropriately. However, reducing inpatient volumes per psychiatrist mean either increasing psychiatry staffing or decreasing inpatient volume. Such strategies would accompany additional cost burden in psychiatric care. Therefore, health policy makers and decision makers have to first consider the tradeoff relationship between quality and cost, and then make efficient alternatives for improving psychiatric care in the near future. In addition, health policy makers should consider developing incentive programs to ensure a superior quality of care. Thus, such programs or alternatives would prevent inadequate psychiatric treatment and it could also be helpful in reducing the cost burden caused by adverse events such as readmission. This would eventually increase the accessibility of patients by reducing the cost barrier for using psychiatric care in South Korea, and then could improve the mental health of South Koreans.
Our study has several strengths compared to previous investigations. First, we used NHI claim data to analyze both patient- and hospital-level characteristics. Thus, our models reflect the diversity of patients and hospitals in South Korea, and the results will be helpful in establishing evidence-based health policies. Second, we considered hospital characteristics such as ownership status, teaching status, type of medical institution, and human resource availability. In previous studies on readmission, public hospitals have had higher readmission rates than private hospitals. However, we found higher readmission rates in private hospitals. We hypothesize that this is because private hospitals to occupy beds in order to make more profits, but such motivation was relatively less in public hospital based on ownership status [38]. Our results demonstrate that staff levels affect psychiatric inpatient care; in particular, the readmission rate is associated with the numbers of psychiatrists and pharmacists. This finding suggests that better quality care requires an appropriate balance of health care staff to deliver effective treatment. To test this hypothesis, it would be necessary to perform further analyses of detailed hospital data. Third, to our knowledge, this is the first study on the relationship between psychiatric inpatient readmission and inpatient volume per psychiatrist in South Korea, where readmissions are a major expense. Given the paucity of existing data, our results may prove helpful in managing South Korean mental health readmissions. Finally, our study employed LOS per psychiatrist to measure inpatient volume per psychiatrist. Thus, our results could be considered to provide more detailed inpatient volume per psychiatrist (as opposed to only examining patient volume).
Our study also has some limitations. First, substance use, an important indicator of mental health care quality, was not considered in our analysis because the relevant details were not included in our dataset. In addition, we only focused on five diagnostic groups, not all psychiatric disorders. As a result, these findings may not be generalizable to all psychiatric disorders. Also, we just consider repeat admission for same diagnosis rather than readmission due to any of the psychiatric diagnoses, because there were some limitations for accessibility of data. Next, we only analyzed cases with readmissions that took place in the same hospital. This was best way to include cross-hospital readmission in this study. However, we were unable to determine whether the each inpatient was hospitalized multiple times, as the data used in our study was based on only hospitalization cases, not inpatients details. In addition, the details about whether patients transferred to other hospitals could not be considered in this study, because such information were unavailable in the data used. Third, the NHI claim data we used included information from 53 hospitals. Thus, it may be difficult to generalize our results to South Korea as a whole, and we could not account for cases transferred from other hospitals. In addition, in the process of selecting the study population, we first performed the propensity score matching and excluded hospitals without hospitalization cases for the major five psychiatric disorders. Although it would be ideal to first exclude inappropriate hospitals which do not provide psychiatric care among total hospitals in South Korea and then perform the selection of the study population using the propensity score matching methods, there were limitations in conducting this as there are difficulties in accessing patient information due to issues such as ethics. Fourth, our results do not address cost because financial information was not included in our dataset. Also, our study could not assess the effects of comorbid mental disorders including depression. Fifth, the inpatient volume per psychiatrist as an outcome variable used in this study defined as an average of sum of LOS per each psychiatrist in each hospital. Therefore, we could not consider difference for workload each psychiatrist in each hospital by calculating method and limitation of data.
Despite these limitations, our results suggest that inpatient volume per psychiatrist substantially impacts the risk of psychiatric inpatient readmission within 30 days. These findings could be used by health policy makers and the government to identify potential solutions for controlling psychiatric inpatient readmission rates. However, further studies are needed to determine effective strategies to reduce psychiatric inpatient readmission rates.
Conclusions
Psychiatric inpatient readmission rates within 30 days of release were lower in hospitals with lower inpatient volume per psychiatrist, especially for those patients hospitalized for “schizophrenia, schizotypal, and delusional disorders” and “mood disorders.” There need more further study which investigating more detailed relationship, so the health policy makers and hospital managers could reduce readmissions for psychiatric disorders and other diseases in the future.
Ethics approval and consent to participate
Out study utilized secondary data reported on the aggregate level and each case in our dataset was converted to random number for avoiding identification. Thus, it was not necessary to obtain research ethics approval and informed consents from the patients.
Consent for publication
Not applicable.
Availability of data and materials
The data used in this study were obtained from the Health Insurance Claim data, it can only be disclosed to the people who had authorized.
Acknowledgement
No specific funding supported this study.
Abbreviations
- ANOVAs
analysis of variances
- CI
confidence interval
- FFS
fee for service
- GEE
generalized estimating equation
- ICD
International classification of diseases groupings
- LOS
length of stay
- NHI
National Health Insurance
- OECD
Organization for Economic Co-operation and Development
- OR
odds ratio
- SD
standard deviation
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
KTH designed the study, researched data, performed statistical analyses and wrote the manuscript. SYL, SJK, MIH, SIJ, SJK, and ECP contributed to the discussion and reviewed and edited the manuscript. E.C.P. is the guarantor of this work and as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. In addition, W.K. provided re-editing services for our manuscript to improve the quality of scientific writing. All authors read and approved the final manuscript.
Contributor Information
Kyu-Tae Han, Email: kthan@yuhs.ac.
Seo Yoon Lee, Email: Sunjung5958@yuhs.ac.
Sun Jung Kim, Email: sunjkim0623@gmail.com.
Myung-Il Hahm, Email: hmi@sch.ac.kr.
Sung-In Jang, Email: JANGSI@yuhs.ac.
Seung Ju Kim, Email: yuwooki@yuhs.ac.
Woorim Kim, Email: woorimk@yuhs.ac.
Eun-Cheol Park, Phone: 82-2-2228-1862, Email: ecpark@yuhs.ac.
References
- 1.Zhang J, Harvey C, Andrew C. Factors associated with length of stay and the risk of readmission in an acute psychiatric inpatient facility: a retrospective study. Aust N Z J Psychiatry. 2011;45:578–85. doi: 10.3109/00048674.2011.585452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.OECD. Health at a Glance 2013: OECD Indicators. 2013.
- 3.Yellowlees P. Psychiatric and social reasons for frequent rehospitalization. Hosp Community Psychiatry. 1994;45:347. doi: 10.1176/ps.45.4.347. [DOI] [PubMed] [Google Scholar]
- 4.Epstein SA, Gonzales JJ, Weinfurt K, Boekeloo B, Yuan N, Chase G. Are Psychiatrists’ Characteristics Related to How They Care for Depression in the Medically Ill?:< i > Results From a National Case-Vignette Survey</i>. Psychosomatics. 2001;42:482–9. doi: 10.1176/appi.psy.42.6.482. [DOI] [PubMed] [Google Scholar]
- 5.Callaly T, Trauer T, Hyland M, Coombs T, Berk M. An examination of risk factors for readmission to acute adult mental health services within 28 days of discharge in the Australian setting. Australas Psychiatry. 2011;19:221–5. doi: 10.3109/10398562.2011.561845. [DOI] [PubMed] [Google Scholar]
- 6.Callaly T, Hyland M, Trauer T, Dodd S, Berk M. Readmission to an acute psychiatric unit within 28 days of discharge: identifying those at risk. Aust Health Rev. 2010;34:282–5. doi: 10.1071/AH08721. [DOI] [PubMed] [Google Scholar]
- 7.Bobier C, Warwick M. Factors associated with readmission to adolescent psychiatric care. Aust N Z J Psychiatry. 2005;39:600–6. doi: 10.1080/j.1440-1614.2005.01632.x. [DOI] [PubMed] [Google Scholar]
- 8.Boaz TL, Becker MA, Andel R, Van Dorn RA, Choi J, Sikirica M. Risk factors for early readmission to acute care for persons with schizophrenia taking antipsychotic medications. Psychiatr Serv. 2013;64:1225–9. doi: 10.1176/appi.ps.003382012. [DOI] [PubMed] [Google Scholar]
- 9.Bernardo AC, Forchuk C. Factors associated with readmission to a psychiatric facility. Psychiatr Serv. 2001;52:1100–2. doi: 10.1176/appi.ps.52.8.1100. [DOI] [PubMed] [Google Scholar]
- 10.Christian CK, Gustafson ML, Betensky RA, Daley J, Zinner MJ. The volume–outcome relationship: don’t believe everything you see. World J Surg. 2005;29:1241–4. doi: 10.1007/s00268-005-7993-8. [DOI] [PubMed] [Google Scholar]
- 11.Hamilton BH, Hamilton VH. Estimating surgical volume—outcome relationships applying survival models: accounting for frailty and hospital fixed effects. Health Econ. 1997;6:383–95. doi: 10.1002/(SICI)1099-1050(199707)6:4<383::AID-HEC278>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 12.Heggestad T. Operating conditions of psychiatric hospitals and early readmission—effects of high patient turnover. Acta Psychiatr Scand. 2001;103:196–202. doi: 10.1034/j.1600-0447.2001.00166.x. [DOI] [PubMed] [Google Scholar]
- 13.Lee H-C, Lin H-C. Is the volume-outcome relationship sustained in psychiatric care? Soc Psychiatry Psychiatr Epidemiol. 2007;42:669–72. doi: 10.1007/s00127-007-0214-z. [DOI] [PubMed] [Google Scholar]
- 14.Lin H-C, Lee H-C. Psychiatrists’ caseload volume, length of stay and mental healthcare readmission rates: A three-year population-based study. Psychiatry Res. 2009;166:15–23. doi: 10.1016/j.psychres.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 15.Hughes RG, Carayon P, Gurses AP. Nursing workload and patient safety—a human factors engineering perspective. 2008. [PubMed]
- 16.Hsiao WC. Design and implementation of social health insurance. In Social health insurance for developing nations. 2007. pp.21.
- 17.Hamada H, Sekimoto M, Imanaka Y. Effects of the per diem prospective payment system with DRG-like grouping system (DPC/PDPS) on resource usage and healthcare quality in Japan. Health Policy (New York) 2012;107:194–201. doi: 10.1016/j.healthpol.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 18.Schreyögg J, Stargardt T, Tiemann O. Costs and quality of hospitals in different health care systems: a multi‐level approach with propensity score matching. Health Econ. 2011;20:85–100. doi: 10.1002/hec.1568. [DOI] [PubMed] [Google Scholar]
- 19.Safeek YM, Padaco GS. Red plan, white boards, blue huddles, & clear pathways: Synopsis of a length of stay reduction strategy. Physician Exec. 2010;36:34. [PubMed] [Google Scholar]
- 20.Tarnow-Mordi W, Hau C, Warden A, Shearer A. Hospital mortality in relation to staff workload: a 4-year study in an adult intensive-care unit. Lancet. 2000;356:185–9. doi: 10.1016/S0140-6736(00)02478-8. [DOI] [PubMed] [Google Scholar]
- 21.Group UNSS. Patient volume, staffing, and workload in relation to risk-adjusted outcomes in a random stratified sample of UK neonatal intensive care units: a prospective evaluation. Lancet. 2002;359:99–107. doi: 10.1016/S0140-6736(02)07366-X. [DOI] [PubMed] [Google Scholar]
- 22.Marks FE. Refining a classification system for fiscal and staffing management. J Nurs Adm. 1987;17:39. doi: 10.1097/00005110-198701000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Thompson EE, Neighbors HW, Munday C, Trierweiler S. Length of stay, referral to aftercare, and rehospitalization among psychiatric inpatients. Psychiatr Serv. 2003; 54:1271–6. [DOI] [PubMed]
- 24.Forster AJ, Stiell I, Wells G, Lee AJ, Van Walraven C. The effect of hospital occupancy on emergency department length of stay and patient disposition. Acad Emerg Med. 2003;10:127–33. doi: 10.1111/j.1553-2712.2003.tb00029.x. [DOI] [PubMed] [Google Scholar]
- 25.Schultz M, Van Servellen G, Chang B, McNeese-Smith D, Waxenberg E. The relationship of hospital structural and financial characteristics to mortality and length of stay in acute myocardial infarction patients. Outcomes Manag Nurs Pract. 1997;2:130–6. [PubMed] [Google Scholar]
- 26.Han K-T, Park E-C, Kim SJ, Kim W, Hahm M-I, Jang S-I, Lee SG. Effective strategy for improving health care outcomes: Multidisciplinary care in cerebral infarction patients. Health Policy (New York) 2015;119:1039–45. doi: 10.1016/j.healthpol.2015.06.005. [DOI] [PubMed] [Google Scholar]
- 27.Hanley JA, Negassa A, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 2003;157:364–75. doi: 10.1093/aje/kwf215. [DOI] [PubMed] [Google Scholar]
- 28.Stawski RS. Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modeling. Structural Equation Modeling: A Multidiscip J. 2013;20:541–50.
- 29.Boudourakis LD, Wang TS, Roman SA, Desai R, Sosa JA. Evolution of the surgeon-volume, patient-outcome relationship. Ann Surg. 2009;250:159–65. doi: 10.1097/SLA.0b013e3181a77cb3. [DOI] [PubMed] [Google Scholar]
- 30.Nathens A, Maier R. The relationship between trauma center volume and outcome. Adv Surg. 2000;35:61–75. [PubMed] [Google Scholar]
- 31.Huxley P. Mental illness in the community: the Goldberg-Huxley model of the pathway to psychiatric care. Nord J Psychiatry. 1996;50:47–53.
- 32.Bertram DA, Opila DA, Brown JL, Gallagher SJ, Schifeling RW, Snow IS, Hershey CO. Measuring physician mental workload: reliability and validity assessment of a brief instrument. Med Care. 1992;30:95–104. doi: 10.1097/00005650-199202000-00001. [DOI] [PubMed] [Google Scholar]
- 33.Kumar S. Burnout in psychiatrists. World Psychiatry. 2007;6:186. [PMC free article] [PubMed] [Google Scholar]
- 34.Rathod S, Roy L, Ramsay M, Das M, Birtwistle J, Kingdon D. A survey of stress in psychiatrists working in the Wessex Region. Psychiatric Bulletin. 2000;24:133–6. doi: 10.1192/pb.24.4.133. [DOI] [Google Scholar]
- 35.Horwitz LI, Lin Z, Herrin J, Bernheim S, Drye EE, Krumholz HM, Ross JS. Association of hospital volume with readmission rates: a retrospective cross-sectional study. BMJ. 2015;350:h447. doi: 10.1136/bmj.h447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Druss BG, Miller CL, Pincus HA, Shih S. The volume-quality relationship of mental health care: does practice make perfect? Am J Psychiatry. 2004;161:2282–6. doi: 10.1176/appi.ajp.161.12.2282. [DOI] [PubMed] [Google Scholar]
- 37.Experton B, Ozminkowski RJ, Pearlman DN, Li Z, Thompson S. How does managed care manage the frail elderly?: the case of hospital readmissions in fee-for-service versus HMO systems. Am J Prev Med. 1999;16:163–72. doi: 10.1016/S0749-3797(98)00098-1. [DOI] [PubMed] [Google Scholar]
- 38.Kessler DP, McClellan MB. The effects of hospital ownership on medical productivity. Rand J Econ. 2002;33:488–506. [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used in this study were obtained from the Health Insurance Claim data, it can only be disclosed to the people who had authorized.


