Abstract
Background
All studies involving use of ionizing radiation should be performed in accordance with the ALARA (As Low As Reasonably Achievable) principle, especially in children. In this study, the prospective ECG triggering technique with low voltage was used in dual-source computed tomography (DSCT) angiography to investigate if image quality with low radiation dose could be satisfactory in pediatric patients with congenital heart disease.
Methods
Sixty pediatric patients with suspected congenital cardiovascular anomalies were enrolled prospectively in the study. They were randomly assigned to two groups for DSCT angiography. Group A were scanned by prospective ECG-triggering computed tomography angiography (CTA) with 80 kV tube voltage, while group B by used non-ECG-gated CTA with the same tube voltage. The anomaly accuracy was evaluated based on the surgical and/or conventional cardiac angiography findings. The overall image quality was assessed on a five-point scale. And the diagnostic accuracy and radiation dose was evaluated in both groups.
Results
There were 127 cardiovascular anomalies in Group A and 108 in Group B. The mean subjective image quality and diagnostic accuracy between these two groups were significantly different (P = 0.007 and 0.011, respectively). The mean effective dose in Group A and Group B was 0.38 ± 0.13 mSv and 0.35 ± 0.17 mSv, respectively. But there was no significant difference between two groups (P = 0.197).
Conclusions
The prospective ECG triggering technique in DSCT scan can offer better image quality and diagnostic accuracy with low radiation exposure in pediatric patients with congenital heart diseases. This technique has potential to become a new clinical routine in pediatric cardiac computed tomography (CT) imaging.
Keywords: Dual-source CT, Congenital heart disease, Radiation dose
Background
Cardiovascular computed tomography angiography (CTA) performed on multi-detector row scanners is an accurate method for noninvasive detection of congenital cardiovascular abnormalities [1–5]. Compared to retrospective ECG-gated computed tomography (CT), non-ECG-gated scanning technique is usually applied in CTA studies with low radiation dose in pediatric patients with congenital heart disease [6–8]. The non-ECG-gated technique has also been proved to be relatively more diagnostic accurate. However, it still remains difficult to show minor anatomic abnormalities because of motion artifacts according to the literature and also daily clinical experience [8, 9].
Sequential scanning technique with prospective ECG-triggering is a recent algorithm that could help to reduce the radiation exposure in cardiovascular CT [10, 11]. This technique only allows the ionized X-ray radiation to apply at a certain predefined period of the cardiac cycle rather than during the entire cycle as the retrospective ECG-gating technique. Therefore,prospective ECG-triggering can greatly lower radiation dose while ensure the diagnostic image quality of coronary artery [12–14]. Also, the clinical diagnostic demand of CT image quality is lower for congenital heart disease than for coronary artery disease [15]. Therefore, it is essential whether dual source CT (DSCT) cardiovascular angiography using prospective ECG-triggering can be performed in pediatric patients with congenital heart disease. The purpose of this study was to evaluate the image quality and diagnostic accuracy of DSCT cardiac angiography using low-voltage prospective ECG-triggering technique in pediatric patients with congenital heart disease in comparison with non-ECG-gated technique.
Methods
Patients
This prospective study was approved by the institutional review board and written informed consents were obtained from all patients’ guardians. The potential adverse effects of contrast medium injection and radiation exposure were explained to the parents by a cardiovascular radiologist.
A total of 60 consecutive pediatric patients younger than 5 years old were included in this study. All patients were referred to DSCT angiography for evaluation of suspected congenital cardiovascular anomalies for clinical reasons. Surgeries were performed in 47 patients, and 24 patients underwent conventional cardiac angiography (CCA). The final diagnosis of congenital heart disease was based on the surgical and/or conventional cardiac angiography findings. Patients with known hypersensitivity to iodine-containing contrast medium were excluded from this study. The mean age was 2.4 ± 2.1 years (range: 17 days ~ 5 years). The mean body weight was 7.2 ± 6.9 kg (range: 2.1 ~ 15.2 kg).
DSCT protocol
All CT examinations were performed on a DSCT scanner (SOMATOM Definition, Siemens Medical Solutions, Forchheim, Germany). Before the exam, all patients were put under sedation by oral administration of chloral hydrate (50 ~ 75 mg/kg) according to the patient’s body weight and clinical condition. Abdominal bandage was used to reduce the respiratory artifacts during CT scan. All patients were randomly assigned to two groups for DSCT angiography (with 30 patients in each group). Patients in group A were scanned using prospective ECG-triggering. Patients in group B were examined by non-ECG-gated spiral CT scans. The scan parameters for both groups were listed in Table 1. All patients were scanned in a cranio-caudal direction from the lung apex to the liver dome to cover the entire lung parenchyma. Nonionic contrast medium Iopamidol (Iopamiro 370 mg I/mL, Bracco S.p.A.; Milan, Italy) was injected through a peripheral venous line by using a power injection. The injected volume was adjusted according to patients’ body weight: 2 ml/kg contrast medium followed by 20 ml of saline flush, both at a flow rate of 0.5 ~ 2.0 ml/s. For an optimum vascular opacification, a round region of interest (ROI) was placed in the left ventricle. The triggered threshold of ROI was set at 100 HU. Data acquisition was prospectively ECG-triggered, starting at 40 % of the R-R interval. The duration of the CT scans was 3.12 ~ 7.79 s.
Table 1.
Characteristics of Patients and CT Scanning Parameters in Two Groups
| Parameter | Group A | Group B |
|---|---|---|
| Number of children | 30 | 30 |
| Sex (male/female) | 17/13 | 14/16 |
| Mean age (Y) | 2.6 ± 2.4 | 2.2 ± 1.8 |
| Mean weight (Kg) | 7.3 ± 7.1 | 7.1 ± 6.7 |
| Tube voltage (kV) | 80 | 80 |
| Tube current time (mAs) | 250 | 250 |
| Collimation (mm) | 0.6 | 0.6 |
| Rotation time (sec) | 0.33 | 0.50 |
| Pitch | NA | 1.0 |
| Slice thickness (mm) | 1.0 | 1.0 |
| Reconstruction interval (mm) | 0.8 | 0.8 |
CT data postprocessing and image analysis
All reconstructed images were transferred to an external workstation (Leonardo; Siemens Medical Solutions, Forchheim, Germany). Multiplanar reformation (MPR), maximum intensity projection (MIP) and volume rendering technique (VRT) were used to visualize cardiovascular abnormalities. Diagnoses of cardiac abnormalities were proved by the surgical and/or conventional cardiac angiography. Two cardiovascular radiologists (with 7 and 10 years experience, respectively) subjectively interpreted image quality in consensus. A 5-point scale was used to grade the image quality (5 = excellent; 4 = good; 3 = fair; 2 = poor; 1 = not applicable) [16]. Images with score 3 or more were thought to be diagnostic.
The noise and signal-to-noise ratio (SNR) were measured in the ascending aorta and pulmonary trunk by one observe who was blinded to the subjective image quality scores. Image noise was defined as the standard deviation of the attenuation in a 50-mm2 circular ROI on the axial images with care take to avoid the walls [17]. SNR was calculated as the ratio of the attenuation value and the noise.
Radiation dose estimations
The CT volume dose index (CTDIvol) and dose-length-product (DLP) values were recorded from the CT console displays for each scan. The effective dose was derived from the product of DLP and a conversion coefficient of 0.021 mSv/[mGy · cm] for the pediatric chest [18].
Statistical analysis
Statistical analysis was performed on software SPSS (version 14.0, SPSS Inc.; Chicago, IL). Continuous variables were expressed as mean ± SD. The Student t test was used to analyze the difference of subjective image quality score, the image noise, SNR and radiation dose between the two groups. Diagnostic accuracy was compared by chi-square test between the two groups. Interobserver agreement in subjective image quality scoring was evaluated by kappa statistics. A к value of 0.61-0.80 was considered as good. A P value of less than 0.05 was considered to be statistically significant.
Results
Patient characteristics
Patient demographics were also shown in Table 1. No significant difference was found in patient age or weight between two groups (P = 0.375 and 0.631, respectively). The mean heart rates were 124.6 ± 17.3 beats per min (bpm) for group A and 127.9 ± 23.8 bpm for group B (P = 0.310).
Cardiovascular diagnostic accuracy
Anatomical diagnoses of all 60 patients by surgical and/or CCA findings were listed in Table 2.
Table 2.
Anatomical diagnoses of all 60 patients with prospective ECG-triggering DSCT angiography (Group A) and non-ECG-gated DSCT (Group B) with reference to surgical and/or CCA findings
| Diagnosis | Group A /surgery and/or CCA |
Group B /surgery and/or CCA |
|---|---|---|
| Tetralogy of Fallot | 5/5 | 4/4 |
| Aortic pulmonary septal defect | 1/1 | 1/1 |
| Anomalous pulmonary venous return | 5/5 | 4/4 |
| Aortic coarctation | 6/6 | 8/8 |
| Interrupted aortic arch | 2/2 | 2/3 |
| Pulmonary artery atresia with ventricle septal defect | 3/3 | 2/2 |
| Pulmonary artery atresia with intact ventricular septum | 1/1 | 1/1 |
| Anomalous origin of pulmonary artey | 3/3 | 2/2 |
| Transposition of the great arteries | 2/2 | 3/3 |
| Double outlet right ventricle | 2/2 | 2/2 |
| Total | 30/30 | 29/30 |
A total of 106 separate cardiovascular abnormalities were confirmed by surgical and/or CCA findings in Group A, and 102 abnormalities in Group B (Table 3). For group A, prospective ECG-triggering DSCT angiography missed three abnormalities, including one small atrial septal defect and two pulmonary valve stenoses. However, non-ECG-gated DSCT missed ten abnormalities (Table 3) in group B. The total diagnostic accuracy of prospective ECG- triggering scan and non-ECG-gated scan was 97.2 % (103/106) and 90.2 % (92/102), respectively, which was significantly higher in group A than in group B (P = 0.011).
Table 3.
Cardiovascular deformity findings with prospective ECG-triggering DSCT angiography (Group A) and non-ECG-gated DSCT (Group B) with reference to surgical and/or CCA findings
| Abnormalities | Group A /surgery and/or CCA |
Group B /surgery and/or CCA |
|---|---|---|
| Atrial septal defect | 18/19 | 18/21 |
| Ventricular septal defect | 18/18 | 18/19 |
| Patent ductus arteriosus | 16/16 | 14/14 |
| Aortic pulmonary septal defect | 1/1 | 0/1 |
| Anomalous pulmonary venous return | 5/5 | 3/3 |
| Aortic coarctation | 6/6 | 8/8 |
| Interrupted aortic arch | 2/2 | 2/3 |
| Coronary artery anomaly | 2/2 | 0/1 |
| Right aortic arch | 0/0 | 2/2 |
| Pulmonary valve stenosis | 2/4 | 1/2 |
| Pulmonary artery stenosis | 11/11 | 9/9 |
| Pulmonary artery atresia | 4/4 | 2/3 |
| Dilated pulmonary artery | 11/11 | 9/9 |
| Anomalous origin of pulmonary artey | 3/3 | 2/2 |
| Transposition of the great arteries | 2/2 | 3/3 |
| Double outlet right ventricle | 2/2 | 1/2 |
| Total | 103/106 | 92/102 |
In the five patients with tetralogy of Fallot and scanned with prospective ECG- triggering acquisition, two coronary artery anomalies were found. Non-ECG-gated DSCT scan missed only one coronary artery anomaly in 4 patients with tetralogy of Fallot. These coronary artery findings were confirmed by surgery in all the patients with tetralogy of Fallot.
Evaluation of image quality
Interobserver agreement of the image quality was reached in all studies. The average subjective image quality scores of prospective ECG-triggering DSCT and non-ECG-gated DSCT were 4.4 ± 0.1 (range: 3–5) and 3.8 ± 0.3 (range: 2–5), respectively (P = 0.007) (Table 4). There was good agreement (к = 0.73) for overall image quality scoring between the two reviewers. The image quality with prospective ECG-triggering acquisition was found to be significantly better than with non-ECG-gated spiral acquisition (Figs. 1 and 2).
Table 4.
Subjective and objective evaluation of image quality with prospective ECG-triggering DSCT (Group A) and non-ECG-gated DSCT (Group B)
| Group A | Group B | P value | |
|---|---|---|---|
| Subjective image quality scores | 4.4 ± 0.1 | 3.8 ± 0.3 | 0.007 |
| Attenuation in the left atrium (HU) | 409.2 ± 85.5 | 226.4 ± 141.6 | 0.003 |
| Noise in the left atrium (HU) | 40.0 ± 15.8 | 18.46 ± 5.6 | 0.004 |
| SNR in the left atrium | 11.7 ± 4.6 | 13.2 ± 8.9 | 0.638 |
SNR, signal to noise ratio
Fig. 1.
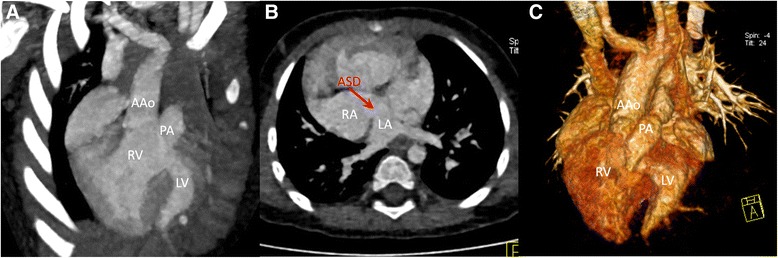
Dual-Source CT imaging with prospective ECG-triggering acquisition for a 15 month-old patient of double outlet right ventricle. Coronal MIP image (a) and coronal VR (c) show the ascending aorta (AAo) and the pulmonary artery (PA) both arise from the right ventricle (RV). Axial MPR image (b) shows this double outlet right ventricle is associated with an atrial septal defect (ASD). LV: left ventricle; RA: right atrium; LA: left atrium
Fig. 2.
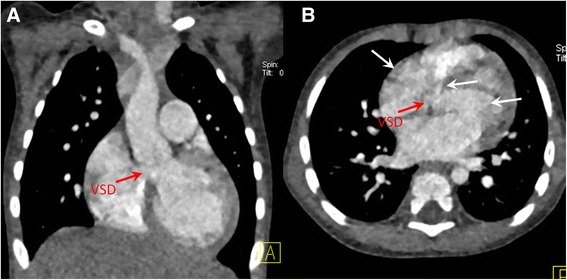
Dual-Source CT imaging with non-ECG-gated spiral acquisition for a 15 month-old patient of ventricular septal defect. Coronal MIP image (a) and axial MPR image (b) show a ventricular septal defect (VSD) with pulsation artifact (white arrows)
The image noise in the left atrium was significantly higher for the prospective ECG triggering CT scan group than that for the non-ECG-gated CT scan group. Also, it showed no significant difference of SNR between two groups (Table 4).
Radiation dose
The mean CTDIvol was 1.58 ± 0.65 mGy (range: 0.39-2.42) and 1.39 ± 0.71 mGy (range: 0.67-2.82) during prospective ECG- triggering acquisition and non-ECG-gated spiral acquisition, respectively. The mean DLP was 19.71 ± 10.56 mGy∙cm (range: 4–37) and 22.29 ± 13.00 mGy∙cm (range: 8–46), respectively, leads to a mean effective dose of 0.41 ± 0.22 mSv (range: 0.084-0.777) and 0.47 ± 0.27 mSv (range: 0.168-0.966), respectively for group A and group B. Although CTDIvol was lower in group A, DLP and the effective radiation dose were higher in group A than that in group B, no significant difference was found between two groups (Table 5).
Table 5.
Radiation dose parameters of prospective ECG-triggering DSCT (Group A) and non-ECG-gated DSCT (Group B)
| Group A | Group B | P value | |
|---|---|---|---|
| CTDIvol (mGy) | 1.58 ± 0.65 | 1.39 ± 0.71 | 0.519 |
| DLP (mGy · cm) | 19.71 ± 10.56 | 22.29 ± 13.00 | 0.560 |
| Effective radiation dose (mSv) | 0.41 ± 0.22 | 0.47 ± 0.27 | 0.560 |
CTDI vol , volume CT dose index; DLP, dose-length product
Discussion
Any diagnostic test with ionizing radiation should be performed in accordance with the ALARA (As Low As Reasonably Achievable) principle, especially in children [19]. With the conventional non-ECG-gated DSCT scan, low dose radiation has been gained. However, for the infants and children who can’t hold their breath during CT scans, motion artifact has always been an issue and can severely impair the image quality and also lower the diagnostic accuracy. In order to reduce radiation dose while maintain the image quality, many dose-saving techniques have been developed, e.g., ECG-controlled dose modulation, tube voltage reduction and prospective-gating sequential scanning mode. Among these strategies, prospective ECG-triggering DSCT is considered one of the most useful methods to reduce radiation dose [20–24].
The reason of radiation dose reduction due to prospective triggering technique is that X-ray exposure only occurs during the selected cardiac phase rather than throughout the entire cardiac cycle (unless functional imaging is required [20]). Huang MP evaluated image quality and radiation dose at weight-based low-dose (80 kV and 60–120 mAs depending on weight) prospectively gated 256-slice MDCT angiography in 64 infants with congenital heart diseases [15]. Diagnostic images were achieved in all cases in Huang’s study, providing a comprehensive three-dimensional evaluation of the cardiac anatomy, including the coronary arteries. Jin KN and his colleagues compared the image quality and radiation dose of retrospective versus prospective ECG-gated dual-source CT imaging in 44 pediatric patients with congenital heart diseases [17]. They found that the image quality was better in the retrospective group than that in the prospective group. However, the mean estimated effective dose was much higher for the retrospective ECG-gated helical scan than that for the prospective non-helical scan, and the retrospective ECG-gated helical scan was definitely unfavorable choice for children. So far, it is known that prospective ECG triggering DSCT angiography can offer a low radiation dose choice. However, very few publications have demonstrated the difference of image quality between prospective ECG triggering and non-ECG-gated DSCT angiography with which low radiation dose can be obtained in both technique. In their study, image quality and the effective radiation dose using these two scan protocols with the same low tube voltage (80 kV) were investigated.
With a gantry rotation time of 330 ms, DSCT has a heart rate-independent temporal resolution of 83 ms with use of a single-segment reconstruction mode, which allows for cardiovascular angiography in patients with high heart rates, especially in infants and children [25]. Some publications [26, 27] reported that at heart rates higher than 85.5 bpm the best reconstruction time shifts to the end systolic phase. Therefore, in this study, 40 % of the R-R interval was used as the center of data acquisition window.
Results from this study showed that with low tube voltage (80 kV) there was no difference of the effective radiation dose between prospective ECG-triggering DSCT scan group (0.41 ± 0.22 mSv) and non-ECG-gated DSCT scan group (0.47 ± 0.27 mSv) (P = 0.560). However, the image quality score of prospective ECG-triggering DSCT scan group (4.4 ± 0.1) is significantly better than that of non-ECG-gated DSCT scan group (3.8 ± 0.3) (P = 0.007). Also, the image noise in the left atrium was significantly higher for the prospective ECG triggering CT scan group than that for the non-ECG-gated CT scan group. In accordance with the image quality, the diagnostic accuracy of prospective ECG-triggering DSCT scan group (97.2 % (103/106)) is also significantly better than that of non-ECG-gated DSCT scan group (90.2 % (92/102)) (P = 0.011).
There is a high incidence (11 %) of coronary artery abnormalities with congenital heart disease [28], especially with complex congenital heart disease. It is essential to evaluate coronary artery variations, because some variations can increase morbidity and even cause death during surgical correction [29, 30]. This study showed that prospective ECG-triggering DSCT scan could depict the coronary artery anomalies clearly, while motion artifact in non-ECG-gated DSCT scan group affected the image quality and led to the missed diagnosis of the only coronary artery anomaly.
Study limitations
This study also has limitations. Firstly, it only included a relatively small group of patients. Future studies with larger patient cohort will be necessary. Secondly, heart beat variability was not considered. And also all the patients in this study showed regular sinus rhythm, however arrhythmia can affect the images massively.
Conclusions
The prospective ECG triggering technique with low tube voltage in DSCT scan can reduce radiation dose and also maintain good image quality in pediatric patients with congenital heart diseases, as compared to a conventional non-ECG-gated DSCT angiography. This promising technique has a potential to become regular clinical method in pediatric CT scans.
Acknowledgments
We would like to thank Dr. Bei E for their help in postprocessing and image reconstruction of the manuscript. The research was supported by the National Natural Science Foundation for the youth of China (Grant No. 81301189).
Abbreviations
- CT
Computed tomography
- CTA
Computed tomography angiography
- DSCT
Dual-source CT
- CCA
Conventional cardiac angiography
- ROI
Region of interest
- MPR
Multiplanar reconstruction
- MIP
Maximum intensity projection
- VRT
Volume rendering technique
- SNR
Signal to noise ratio
- CTDIvol
Volume CT dose index
- DLP
Dose length product
Footnotes
Competing interests
One of the authors Yan Jia is Siemens employee.
Authors’ contributions
YL and MWZ carried out the conception and design. JL and HLZ carried out the analysis and interpretation. JR, JX and YWH participated in the data collection. YL and YJ participated in the writing the article, the critical revision of the article and the statistical analysis. All authors read and approved the final manuscript.
Contributor Information
Ying Liu, Email: yingyinglyly@126.com.
Jian Li, Email: xjyylj@yeah.net.
Hongliang Zhao, Email: zhaohl1980@163.com.
Yan Jia, Email: jiayan@siemens.com.
Jing Ren, Email: jrenmm@126.com.
Jian Xu, Email: xujian@fmmu.edu.cn.
Yuewen Hao, Email: 1982_edifier@163.com.
Minwen Zheng, Phone: +86 029 84775421, Email: zhengmw2007@163.com.
References
- 1.Khatri S, Varma SK, Khatri P, Kumar RS. 64-slice multidetector-row computed tomographic angiography for evaluating congenital heart disease. Pediatr Cardiol. 2008;29:755–762. doi: 10.1007/s00246-008-9196-1. [DOI] [PubMed] [Google Scholar]
- 2.Schroeder S, Achenbach S, Bengel F, Burgstahler C, Cademartiri F, de Feyter P, George R, Kaufmann P, Kopp AF, Knuuti J, Ropers D, Schuijf J, Tops LF, Bax JJ; Working Group Nuclear Cardiology and Cardiac CT; European Society of Cardiology; European Council of Nuclear Cardiology. Cardiac computed tomography: indications, applications, limitations, and training requirements: report of a Writing Group deployed by the Working Group Nuclear Cardiology and Cardiac CT of the European Society of Cardiology and the European Council of Nuclear Cardiology. Eur Heart J. 2008;29:531–56. [DOI] [PubMed]
- 3.Herzog C, Mulvihill DM, Nguyen SA, Savino G, Schmidt B, Costello P, Vogl TJ, Schoepf UJ. Pediatric cardiovascular CT angiography: radiation dose reduction using automatic anatomic tube current modulation. AJR Am J Roentgenol. 2008;190:1232–1240. doi: 10.2214/AJR.07.3124. [DOI] [PubMed] [Google Scholar]
- 4.Mori Y, Takahashi K, Nakanishi T. Complications of cardiac catheterization in adults and children with congenital heart disease in the current era. Heart Vessels. 2013;28:352–59. [DOI] [PubMed]
- 5.Paul JF, Rohnean A, Sigal-Cinqualbre A. Multidetector CT for congenital heart patients: what a paediatric radiologist should know. Pediatr Radiol. 2010;40:869–875. doi: 10.1007/s00247-010-1614-x. [DOI] [PubMed] [Google Scholar]
- 6.Tsai IC, Lee T, Chen MC, Fu YC, Jan SL, Wang CC, Chang Y. Visualization of neonatal coronary arteries on multidetector row CT: ECG-gated versus non-ECG-gated technique. Pediatr Radiol. 2007;37:818–825. doi: 10.1007/s00247-007-0512-3. [DOI] [PubMed] [Google Scholar]
- 7.Goo HW, Suh DS. Tube current reduction in pediatric non-ECG-gated heart CT by combined tube current modulation. Pediatr Radiol. 2006;36:344–351. doi: 10.1007/s00247-005-0105-y. [DOI] [PubMed] [Google Scholar]
- 8.Goo HW, Park IS, Ko JK, Kim YH, Seo DM, Yun TJ, Park JJ. Visibility of the origin and proximal course of coronary arteries on non-ECG-gated heart CT in patients with congenital heart disease. Pediatr Radiol. 2005;35:792–798. doi: 10.1007/s00247-005-1482-y. [DOI] [PubMed] [Google Scholar]
- 9.Shiraishi I, Kajiyama Y, Yamagishi M, Hamaoka K, Yagihara T. The applications of non-ECG-gated MSCT angiography in children with congenital heart disease. Int J Cardiol. 2012;156:309–314. doi: 10.1016/j.ijcard.2010.11.009. [DOI] [PubMed] [Google Scholar]
- 10.Hsieh J, Londt J, Vass M, Li J, Tang X, Okerlund D. Step-and-shoot data acquisition and reconstruction for cardiac x-ray computed tomography. Med Phys. 2006;33:4236–4248. doi: 10.1118/1.2361078. [DOI] [PubMed] [Google Scholar]
- 11.Gopal A, Mao SS, Karlsberg D, Young E, Waggoner J, Ahmadi N, Pal RS, Leal J, Karlsberg RP, Budoff MJ. Radiation reduction with prospective ECG-triggering acquisition using 64-multidetector Computed Tomographic angiography. Int J Cardiovasc Imaging. 2009;25:405–416. doi: 10.1007/s10554-008-9396-z. [DOI] [PubMed] [Google Scholar]
- 12.Alkadhi H. The revival of step-and-shoot computed tomography coronary angiography: benefits and open questions. J Cardiovasc Comput Tomogr. 2008;2:91–92. doi: 10.1016/j.jcct.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 13.Scheffel H, Alkadhi H, Leschka S, Plass A, Desbiolles L, Guber I, Krauss T, Gruenenfelder J, Genoni M, Luescher TF, Marincek B, Stolzmann P. Low-dose CT coronary angiography in the step-and-shoot mode: diagnostic performance. Heart. 2008;94:1132–1137. doi: 10.1136/hrt.2008.149971. [DOI] [PubMed] [Google Scholar]
- 14.Alkadhi H, Stolzmann P, Scheffel H, Desbiolles L, Baumüller S, Plass A, Genoni M, Marincek B, Leschka S. Radiation dose of cardiac dual-source CT: the effect of tailoring the protocol to patient-specific parameters. Eur J Radiol. 2008;68:385–391. doi: 10.1016/j.ejrad.2008.08.015. [DOI] [PubMed] [Google Scholar]
- 15.Huang MP, Liang CH, Zhao ZJ, Liu H, Li JL, Zhang JE, Cui YH, Yang L, Liu QS, Ivanc TB, Vembar M. Evaluation of image quality and radiation dose at prospective ECG-triggered axial 256-slice multi-detector CT in infants with congenital heart disease. Pediatr Radiol. 2011;41:858–866. doi: 10.1007/s00247-011-2079-2. [DOI] [PubMed] [Google Scholar]
- 16.Ben Saad M, Rohnean A, Sigal-Cinqualbre A, Adler G, Paul JF. Evaluation of image quality and radiation dose of thoracic and coronary dual-source CT in 110 infants with congenital heart disease. Pediatr Radiol. 2009;39:668–676. doi: 10.1007/s00247-009-1209-6. [DOI] [PubMed] [Google Scholar]
- 17.Jin KN, Park EA, Shin CI, Lee W, Chung JW, Park JH. Retrospective versus prospective ECG-gated dual-source CT in pediatric patients with congenital heart diseases: comparison of image quality and radiation dose. Int J Cardiovasc Imaging. 2010;26(Suppl 1):63–73. doi: 10.1007/s10554-009-9579-2. [DOI] [PubMed] [Google Scholar]
- 18.Fuchs TA, Stehli J, Bull S, Dougoud S, Clerc OF, Herzog BA, Buechel RR, Gaemperli O, Kaufmann PA. Coronary computed tomography angiography with model-based iterative reconstruction using a radiation exposure similar to chest X-ray examination. Eur Heart J. 2014;35:1131–1136. doi: 10.1093/eurheartj/ehu053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hollingsworth CL, Yoshizumi TT, Frush DP, Chan FP, Toncheva G, Nguyen G, Lowry CR, Hurwitz LM. Pediatric cardiac-gated CT angiography: assessment of radiation dose. AJR Am J Roentgenol. 2007;189:12–18. doi: 10.2214/AJR.06.1507. [DOI] [PubMed] [Google Scholar]
- 20.Milkovic D, Garaj-Vrhovac V, Ranogajec-Komor M, Miljanic S, Gajski G, Knezevic Z, Beck N. Primary DNA damage assessed with the comet assay and comparison to the absorbed dose of diagnostic X-rays in children. Int J Toxicol. 2009;28:405–416. doi: 10.1177/1091581809344775. [DOI] [PubMed] [Google Scholar]
- 21.Ketelsen D, Thomas C, Werner M, Luetkhoff MH, Buchgeister M, Tsiflikas I, Reimann A, Burgstahler C, Brodoefel H, Kopp AF, Claussen CD, Heuschmid M. Dual-source computed tomography: Estimation of radiation exposure of ECG-gated and ECG-triggered coronary angiography. Eur J Radiol. 2010;73:274–279. doi: 10.1016/j.ejrad.2008.10.033. [DOI] [PubMed] [Google Scholar]
- 22.Klass O, Jeltsch M, Feuerlein S, Brunner H, Nagel HD, Walker MJ, Brambs HJ, Hoffmann MH. Prospectively gated axial CT coronary angiography: preliminary experiences with a novel low-dose technique. Eur Radiol. 2009;19:829–836. doi: 10.1007/s00330-008-1222-4. [DOI] [PubMed] [Google Scholar]
- 23.Earls JP, Berman EL, Urban BA, Curry CA, Lane JL, Jennings RS, McCulloch CC, Hsieh J, Londt JH. Prospectively gated transverse coronary CT angiography versus retrospectively gated helical technique: improved image quality and decreased radiation dose. Radiology. 2008;246:742–753. doi: 10.1148/radiol.2463070989. [DOI] [PubMed] [Google Scholar]
- 24.Hausleiter J, Meyer T, Hermann F, Hadamitzky M, Krebs M, Gerber TC, McCollough C, Martinoff S, Kastrati A, Schömig A, Achenbach S. Estimated radiation dose associated with cardiac CT angiography. JAMA. 2009;301:500–507. doi: 10.1001/jama.2009.54. [DOI] [PubMed] [Google Scholar]
- 25.Schoenhagen P. Back to the future: coronary CT angiography using prospective ECG triggering. Eur Heart J. 2008;29:153–154. doi: 10.1093/eurheartj/ehm614. [DOI] [PubMed] [Google Scholar]
- 26.Matt D, Scheffel H, Leschka S, Flohr TG, Marincek B, Kaufmann PA, Alkadhi H. Dual-source CT coronary angiography: image quality, mean heart rate, and heart rate variability. AJR Am J Roentgenol. 2007;189:567–573. doi: 10.2214/AJR.07.2078. [DOI] [PubMed] [Google Scholar]
- 27.Leschka S, Wildermuth S, Boehm T, Desbiolles L, Husmann L, Plass A, Koepfli P, Schepis T, Marincek B, Kaufmann PA, Alkadhi H. Noninvasive coronary angiography with 64-section CT: effect of average heart rate and heart rate variability on image quality. Radiology. 2006;241:378–385. doi: 10.1148/radiol.2412051384. [DOI] [PubMed] [Google Scholar]
- 28.Hong C, Becker CR, Huber A, Schoepf UJ, Ohnesorge B, Knez A, Brüning R, Reiser MF. ECG-gated reconstructed multi-detector row CT coronary angiography: effect of varying trigger delay on image quality. Radiology. 2001;220:712–717. doi: 10.1148/radiol.2203010055. [DOI] [PubMed] [Google Scholar]
- 29.Koifman B, Egdell R, Somerville J. Prevalence of asymptomatic coronary arterial abnormalities detected by angiography in grown-up patients with congenital heart disease. Cardiol Young. 2001;11:614–618. doi: 10.1017/S1047951101000968. [DOI] [PubMed] [Google Scholar]
- 30.Chen SJ, Lin MT, Lee WJ, Liu KL, Wang JK, Chang CI, Li YW, Chiu IS. Coronary artery anatomy in children with congenital heart disease by computed tomography. Int J Cardiol. 2007;120:363–370. doi: 10.1016/j.ijcard.2006.10.013. [DOI] [PubMed] [Google Scholar]


