Abstract
Objective
To evaluate the impact of integrating a handoff tool into the electronic medical record (EMR) on sign-out accuracy, satisfaction and workflow in a neonatal intensive care unit (NICU).
Study Design
Prospective surveys of neonatal care providers in an academic children’s hospital 1 month before and 6 months following EMR integration of a standalone Microsoft Access neonatal handoff tool.
Result
Providers perceived sign-out information to be somewhat or very accurate at a rate of 78% with the standalone handoff tool and 91% with the EMR-integrated tool (P < 0.01). Before integration of neonatal sign-out into the EMR, 35% of providers were satisfied with the process of updating sign-out information and 71% were satisfied with the printed sign-out document; following EMR integration, 92% of providers were satisfied with the process of updating sign-out information (P < 0.01) and 98% were satisfied with the printed sign-out document (P < 0.01). Neonatal care providers reported spending a median of 11 to 15 min/day updating the standalone sign-out and 16 to 20 min/day updating the EMR-integrated sign-out (P = 0.026). The median percentage of total sign-out preparation time dedicated to transcribing information from the EMR was 25 to 49% before and <25% after EMR integration of the handoff tool (P < 0.01).
Conclusion
Integration of a NICU-specific handoff tool into an EMR resulted in improvements in perceived sign-out accuracy, provider satisfaction and at least one aspect of workflow.
Keywords: health information technology, communication, NICU, clinical informatics
Introduction
Physician handoffs have been described as a “precarious exchange” often fraught with preventable errors that have the potential to cause patient harm.1,2 In an era of trainee duty hour restrictions, patient care handoffs are occurring with increased frequency. Accordingly, both the Institute of Medicine and the Joint Commission identify implementation of a standardized approach to patient handoffs (including transfer of up-to-date information regarding a patient’s condition, care and treatment), as one aspect of achieving more effective communication in an effort to improve patient safety.3,4
Computerized sign-out systems, such as those that employ word processor documents, have been associated with improved continuity of care and a reduction in adverse events at the time of patient handoffs.5 These standalone electronic sign-out systems require significant manual data transcription, which represents a potential source of error.5 In addition to the potential for containing inaccuracies, standalone sign-out systems require time and effort to create and maintain.2 Systems integrated within a hospital’s electronic medical record (EMR), on the other hand, have the ability to automate the retrieval of pertinent patient information from the EMR. Furthermore, EMR-integrated handoff systems have been shown to facilitate patient care handoffs, which might otherwise be “haphazard and error prone.”2,6,7
In June 2006, Bernstein et al.8 implemented an EMR-integrated electronic handoff tool on the medical/surgical wards at Lucile Packard Children’s Hospital (LPCH) and documented its rapid adoption, improved physician workflow and improved physician satisfaction. The handoff tool was not adopted in the LPCH neonatal intensive care unit (NICU), where the layout of a well-established standalone Microsoft Access sign-out database better addressed the needs of the unit.
EMRs have been shown to improve clinical practice in the NICU,9 but standalone sign-out systems specific to neonatal care remain barriers to adoption of EMR-based handoff tools. To date, the customization of a commercial EMR for NICU-specific handoffs has not been documented. The purpose of this study is to evaluate the impact of implementation of an EMR-integrated NICU-specific handoff tool on sign-out accuracy, provider satisfaction, and workflow.
Methods
Before the study period, a Microsoft Access-based handoff tool was used to facilitate sign-out in the NICU at LPCH. Care providers in neonatal units at LPCH were surveyed 1 month pre- and 6 months post-implementation of the NICU-specific electronic handoff tool integrated within the hospital’s EMR. LPCH is a 304-bed quaternary care women and children’s hospital in Palo Alto, CA, USA; it is the principal academic children’s hospital affiliated with Stanford University. The NICU at the main campus of LPCH is comprised of 74 beds. The EMR at LPCH includes laboratory, radiology, and transcription results, computerized provider order entry, and clinical nursing documentation, which corresponds to Stage 4 of the Healthcare Information and Management Systems Society Analytics EMR adoption model.10
The EMR-integrated neonatal handoff tool was implemented on 30 October 2008. Pre-implementation survey data were collected during the month of October 2008 and 6-month post-implementation survey data were collected in April and May 2009. This project was reviewed and approved by the Stanford University School of Medicine Institutional Review Board.
Participants
All neonatal care faculty, hospitalists, fellows, and nurse practitioners who work in the LPCH NICU were invited to participate in the surveys. In addition, pediatric residents who rotated through the NICU between 1 July 2008 to 31 October 2008 and 1 November 2008 to 1 May 2009 were invited to complete the pre- and post-implementation surveys, respectively.
Intervention
A neonatal-specific electronic handoff tool, including both a printed neonatal sign-out document and a neonatal sign-out data entry form, was implemented within a commercial EMR (Millenium, Cerner, Kansas City, MO, USA) on 30 October 2008.
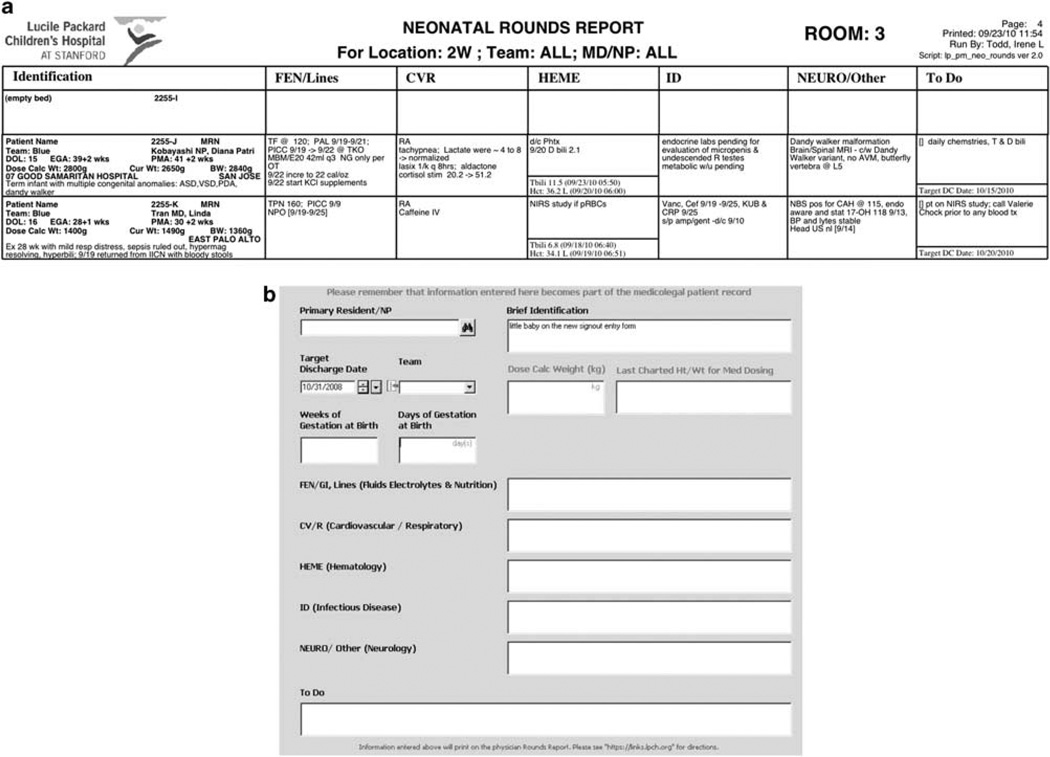
The EMR-integrated neonatal sign-out document (Figure 1a) is organized by bed location and is populated automatically by information from the EMR, including patient demographics, measurements and laboratory data. A patient description, a systems-based summary of active medical issues and ongoing care and a ‘To Do’ list are entered as free text on the neonatal-specific sign-out entry form (Figure 1b) within each patient’s electronic chart. Because the form’s structure is based upon the entry form used for the previously implemented medical/surgical EMR-integrated handoff tool, the sign-out information it contains is not restricted to the neonatal sign-out document. Rather, it is patient-specific and is available to populate the EMR-integrated medical/surgical sign-out document as well (for instance, when a patient is transferred out of the NICU to another unit).
Figure 1.
Electronic medical record (EMR)-integrated neonatal handoff tool. (a) Excerpt from the sign-out document and (b) sign-out data entry form.
Training
Before implementation of the neonatal-specific EMR-integrated handoff tool, an email containing instructions was sent to neonatal care providers caring for patients in the LPCH NICU (attendings, neonatal nurse practitioners (NNPs), fellows, charge nurses and nurse managers) and house staff. Pediatric residents required minimal training because the format and functionality of the EMR-integrated neonatal sign-out entry form are based upon the previously implemented medical/surgical handoff tool they use when rotating throughout other areas of LPCH. Informal instructional sessions were provided to attendings, fellows, NNPs and nurses in neonatal care areas at the time of go-live.
Survey
The same multiple-choice eight-item survey was administered to providers caring for patients in the LPCH NICU 1 month pre- and 6 months post-integration of the neonatal handoff tool into the EMR (Appendix 1). One additional item, a free-response area, was provided for comments and other feedback. Survey data were collected anonymously using an online survey engine (Stanford Surveyor v1.0, Stanford University, Palo Alto, CA, USA).
The primary outcome was provider reported accuracy of sign-out information. Secondary outcomes were provider reported satisfaction with the process of updating sign-out information, satisfaction with the printed sign-out document, and provider reported sign-out workflow (time spent updating sign-out information, and the percentage of total sign-out preparation time dedicated to transcribing information from the EMR). Providers also reported use of either the standalone or EMR-integrated neonatal handoff tool.
EMR run reports
Each run of the EMR-integrated neonatal sign-out report was tracked systematically using logs within the EMR. The logs included information about provider position: medical (MDs, NNPs), nursing, or ancillary (pharmacists, unit secretaries, case managers, nutritionists, and audiologists).
Statistical analysis
Descriptive summary of the data consisted of frequency counts, percentages, mean values and median values. The Wilcoxon rank-sum test was used for comparison of ordinal variables, and the Fisher’s exact test for independence was used for categorical variables. R statistical package (version 2.10 for Windows) was used (The R Foundation for Statistical Computing, Vienna, Austria).
Results
Survey results: impact on accuracy, satisfaction and workflow
Fifty-two providers caring for patients in the LPCH NICU responded to the pre-implementation survey, and 46 responded to the 6- month post-implementation survey. The composition of pre-implementation and post-implementation respondents was similar (Table 1). Before the introduction of the neonatal-specific EMR-integrated handoff tool, 93% of respondents who used a sign-out document in the NICU reported using the standalone Microsoft Access-based solution, while 7% reported use of the EMR-integrated medical/surgical sign-out (Table 2). Six months following the introduction of the neonatal-specific EMR-integrated handoff tool, 98% of respondents who used a sign-out document reported using the neonatal-specific EMR-integrated sign-out, and one respondent reported use of the standalone Microsoft Access-based solution (P < 0.0001).
Table 1.
Survey respondents
| Pre- intervention |
Post- intervention |
P-value | |
|---|---|---|---|
| Number of respondents | 52 | 46 | |
| Position | 0.7094 | ||
| Neonatologist (%) | 10 (19) | 5 (11) | |
| General pediatrician/hospitalist (%) | 6 (12) | 4 (9) | |
| Neonatal nurse practitioner (%) | 12 (23) | 10 (22) | |
| Nurse (%) | 4 (8) | 3 (7) | |
| Neonatology fellow (%) | 4 (8) | 3 (7) | |
| Resident (%) | 16 (31) | 18 (39) | |
| Othera (%) | 0 (0) | 3 (7) | |
| Unit | 0.8363 | ||
| Well baby nursery (%) | 1 (2) | 0 (0) | |
| Packard special care nursery (%) | 5 (10) | 6 (13) | |
| Intermediate intensive care nursery (%) | 2 (4) | 3 (7) | |
| Neonatal intensive care unit (%) | 44 (85) | 37 (80) |
Three registered dieticians responded to the post-implementation survey.
Table 2.
Survey resultsa
| Pre- intervention |
Post- intervention |
P-value | |
|---|---|---|---|
| Handoff tool used | <0.0001 | ||
| Number of respondents | 52 | 46 | |
| Microsoft Access-based (%) | 40 (77) | 1 (2) | |
| EMR-integrated (%) | 3 (6) | 43 (94) | |
| None (%) | 9 (17) | 2 (4) | |
| Perceived accuracy of sign-out document | 0.0025 | ||
| Number of respondents | 45 | 46 | |
| Very accurate (%) | 6 (13) | 17 (37) | |
| Somewhat accurate (%) | 29 (64) | 25 (54) | |
| Somewhat inaccurate (%) | 10 (22) | 4 (9) | |
| Very inaccurate (%) | 0 (0) | 0 (0) | |
| Satisfaction with sign-out process | <0.0001 | ||
| Number of respondents | 43 | 36 | |
| Very satisfied (%) | 4 (9) | 12 (33) | |
| Somewhat satisfied (%) | 11 (26) | 21 (58) | |
| Neutral (%) | 12 (28) | 0 (0) | |
| Somewhat dissatisfied (%) | 16 (37) | 2 (6) | |
| Very dissatisfied (%) | 0 (0) | 1 (3) | |
| Satisfaction with sign-out document | 0.0003 | ||
| Number of respondents | 45 | 46 | |
| Very satisfied (%) | 8 (18) | 18 (39) | |
| Somewhat satisfied (%) | 24 (53) | 27 (59) | |
| Neutral (%) | 7 (16) | 0 (0) | |
| Somewhat dissatisfied (%) | 6 (13) | 1 (2) | |
| Very dissatisfied (%) | 0 (0) | 0 (0) | |
| Time updating sign-out document | 0.026 | ||
| Number of respondents | 38 | 33 | |
| <5 min/day (%) | 1 (3) | 0 (0) | |
| 5–10 min/day (%) | 11 (29) | 5 (15) | |
| 11–15 min/day (%) | 10 (26) | 10 (30) | |
| 16–20 min/day (%) | 15 (39) | 11 (33) | |
| 21–25 min/day (%) | 0 (0) | 3 (10) | |
| 26–30 min/day (%) | 1 (3) | 3 (10) | |
| >30 min/day (%) | 0 (0) | 1 (3) | |
| Percent of time transcribing from EMR | 0.0006 | ||
| Number of respondents | 38 | 33 | |
| <25% (%) | 6 (16) | 17 (52) | |
| 25–49% (%) | 17 (45) | 10 (30) | |
| 50–74% (%) | 11 (29) | 6 (18) | |
| >75% (%) | 4 (11) | 0 (0) |
Abbreviation: EMR, electronic medical record.
Excludes responses indicating ‘not enough information to respond’.
Provider perceived accuracy, satisfaction, and workflow data are reported in Table 2. Before introduction of the neonatal-specific EMR-integrated handoff tool, 78% of respondents reported the sign-out document to be somewhat or very accurate, compared with 91% 6 months following its introduction (P = 0.0025). Before implementation of the neonatal-specific EMR-integrated handoff tool, 35% of respondents reported being somewhat or very satisfied with the process of updating sign-out information, and 71% were somewhat or very satisfied with the printed sign-out document. Six months post-implementation, 92% of respondents reported being somewhat or very satisfied with the process of updating sign-out information (P < 0.0001), and 98% were somewhat or very satisfied with the printed sign-out document (P = 0.0003).
The median reported time spent updating sign-out information was 11 to 15 min/day before implementation of the neonatal-specific EMR-integrated handoff tool, and 16 to 20 min/day following its implementation (P = 0.026). The median reported percentage of total sign-out preparation time dedicated to transcribing data from the EMR was 25 to 49% before implementation of the neonatal-specific EMR-integrated handoff tool, and <25% following its introduction (P = 0.0006).
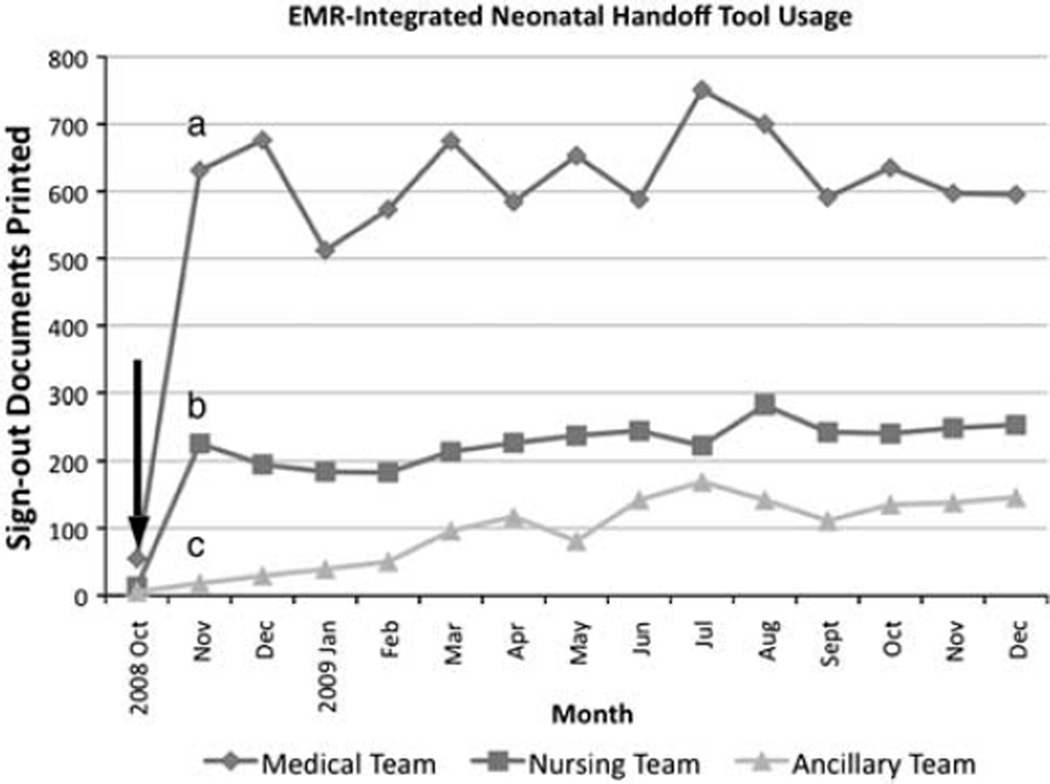
EMR run reports: usage data
Run reports from the EMR demonstrate usage of the neonatal-specific EMR-integrated sign-out since its introduction on 30 October 2008 (Figure 2). During the study period, the sign-out was run 872 times/month (mean), 609 times/month by medical providers, 205 times/month by nurses and 58 times/month by ancillary staff.
Figure 2.
Monthly usage of the electronic medical record (EMR)-integrated neonatal handoff tool since the intervention on 30 October 2008 (arrow) by (a) MDs, neonatal nurse practitioners (NNPs), (b) nursing (including charge nurses) and (c) ancillary staff (pharmacists, unit secretaries, case managers, nutritionists and audiologists).
Discussion
Following implementation of the NICU-specific handoff tool within our EMR, we demonstrated improved provider reported sign-out accuracy and satisfaction with both the electronic sign-out process and the printed sign-out document. Although providers reported increased total time spent updating sign-out information, they also reported spending a smaller percentage of time transcribing data from the EMR.
To date, customization of a commercial EMR to address handoff needs specific to neonatal care has not been documented. Our results showing increased perceived accuracy of sign-out information following EMR integration of the NICU-specific handoff tool suggests EMR integration has the potential to improve handoff communication, and thus has the potential to reduce errors that can lead to patient harm. Customizing EMR functionality to address discipline-specific handoff workflow concerns can increase efficiency, physician satisfaction and acceptance of electronic health information systems.2
The increased perceived accuracy of the EMR-integrated handoff tool is likely a direct result of the automation of both sign-out list maintenance tasks and data retrieval by the EMR. These results are consistent with a previous study of NICU documentation that suggested EMR integration has the potential to decrease documentation errors by reducing redundant data transcription.11 When a patient is admitted, discharged, or transferred, the sign-out document is updated automatically. Similarly, if a patient’s location changes within the unit, the sign-out document reflects the change without requiring input from providers. Because list maintenance is automated by the tool, increased provider time can be dedicated to keeping sign-out information accurate and current. Benefits of integrating a NICU-specific handoff tool within an EMR are achievable at a relatively early stage of EMR adoption because the automation of list maintenance tasks relies primarily upon registration data. In addition to registration information, the accuracy of our EMR-integrated NICU-specific handoff tool is supported by automatic retrieval of laboratory data and clinical information documented electronically by nurses.
Improved provider satisfaction with the EMR-integrated handoff tool is likely related to both quantitative and qualitative workflow factors. Providers spent a smaller percentage of time transcribing data already contained within the EMR following introduction of the EMR-integrated tool, indicating a decrease in redundant manual data entry. Qualitative benefits of EMR integration likely having a role in the tool’s success include elimination of the standalone sign-out database, resulting in a Health Insurance Portability and Accountability Act (HIPAA)-compliant single source of truth for neonatal sign-out information; availability of remote access to sign-out information; and establishment of patient-centric (rather than location-based) sign-out data that is available to consultants outside the NICU and flows with patients as they move between units.
Despite these workflow improvements, providers reported spending more total time updating the EMR-integrated neonatal sign-out. The informatics literature acknowledges more/new work for clinicians as an unintended adverse consequence of computerized provider order entry implementations.12,13 With integration of the neonatal-specific sign-out tool into the EMR, providers were no longer able to update sign-out information for multiple patients on a single database file; rather, sign-out information was accessed within each patient’s electronic chart. The less efficient interface of the EMR-integrated sign-out tool likely had a role in the increased time spent updating sign-out information following its implementation. In addition, the EMR-integrated sign-out contains more space for sign-out information, so providers might have spent more time updating the sign-out because they were able to communicate more information. It is also possible that respondents underestimated the time required to perform list maintenance tasks on the standalone sign-out database.
Following incorporation of the sign-out tool into the EMR, system logs demonstrated nearly 25% of total usage was by nursing staff, including charge nurses. Furthermore, because neonatal sign-out information was no longer limited to workstations in the NICU, other staff began to make use of the report as well: over 10% of neonatal sign-out reports were printed by pharmacists, unit secretaries, case managers, nutritionists, and audiologists seeking neonatal patient information. Although the sign-out tool was designed for MDs and NNPs, integration of the tool within the EMR resulted in increased access to and communication of sign-out information to staff within neonatal care areas and throughout the hospital. This asynchronous, non-interruptive communication can improve the exchange of information.14
Study limitations include those inherent to a self-reported survey method of data collection (poor memory, misinterpretation of a question and intentional deception). Because survey data is descriptive, it is also not possible to draw cause and effect conclusions based upon the responses. The survey might have been more sensitive to differences pre- and post-EMR integration of the handoff tool if continuous rather than ordinal data were collected. Finally, a time and motion study could have more accurately assessed sign-out workflow.
In future versions of the EMR-integrated handoff tool, we hope to increase efficiency by improving the interface for sign-out data entry, as demonstrated in the electronic handoff tool at the University of Washington,3 which has since been integrated within the EMR (Thomas Payne, MD, personal communication). There are also opportunities to automate the retrieval of additional clinical information from the electronic chart, including more laboratory, pharmacy, and radiology information. Finally, using logic that considers electronic provider orders and documentation, we envision the EMR-integrated neonatal sign-out document as a tool for facilitating clinical decision support. It will be important to evaluate the effects of future enhancements to the handoff tool on accuracy, provider workflow, adverse events, patient harm, and the clinical outcomes the decision support functions are designed to affect.
Conclusion
In conclusion, we were able to show that integration of a handoff tool specific to neonatal care within an EMR resulted in improvements in perceived sign-out accuracy, satisfaction, and at least one aspect of workflow. Customization of commercially available EMRs to meet the unique demands of the NICU is possible; we demonstrated specifically the potential to improve handoff communication, an important aspect of patient safety.
Acknowledgments
We acknowledge all the members of the LPCH Information Services department who played a role in the development and implementation of the EMR-based neonatal handoff tool, with special thanks to Margie Godin, RN (Clinical Informatics manager for newborn care and obstetrics), Kiran Pandher (systems architect) and Irene Todd (programmer analyst) for their contributions to the project. We also thank Matthew Wood (clinical informatics, LPCH) for his assistance in the statistical analysis. Finally, we acknowledge Ashvin Sangoram, MD, PhD (former neonatal-perinatal medicine fellow, Stanford University School of Medicine), who developed the standalone Microsoft Access neonatal handoff tool that informed several design aspects of the EMR-integrated handoff tool.
Appendix 1
NICU sign-out survey
- What is your primary clinical role in newborn care?a
- Neonatologist
- General Pediatrician or Hospitalist
- NNP
- Nurse
- NICU fellow
- Resident
- Other (please specify)
- In which unit do you primarily provide care?a
- WBN
- PSCN
- IICN
- NICU
- Do you use printed sign-out information as part of your daily routine?a
- Yes-from Microsoft Access
- Yes-from Powerchart
- No
- Approximately how much time each day do you spend updating sign-out information? Please consider both time updating clinical information and patient location.a
- I do not update sign-out information routinely.
- <5 min/day
- 6–10 min/day
- 11–15 min/day
- 16–20 min/day
- 21–25 min/day
- 26–30 min/day
- >30 min/day
- When updating the sign-out report, what percentage of your time is spent transcribing information from the electronic medical record (Powerchart), including clinical data (weights, labs, etc) and patient location?a
- I do not update sign-out information routinely.
- <25%
- 25–49%
- 50–75%
- >75%
- How accurate/current is the information contained in the sign-out, including clinical data (weights, labs, etc) and patient location?a
- I do not review the printed sign-out information routinely.
- Very inaccurate
- Somewhat inaccurate
- Somewhat accurate
- Very accurate
- How satisfied are you with the current sign-out process?a
- I do not use the current sign-out routinely.
- Very dissatisfied
- Somewhat dissatisfied
- Neither satisfied nor dissatisfied
- Somewhat satisfied
- Very satisfied
- How satisfied are you with the current sign-out printed document?a
- I do not use the current sign-out routinely.
- Very dissatisfied
- Somewhat dissatisfied
- Neither satisfied nor dissatisfied
- Somewhat satisfied
- Very satisfied
Comments:
aRequired.
Footnotes
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Mukherjee S. A precarious exchange. N Engl J Med. 2004;351:1822–1824. doi: 10.1056/NEJMp048085. [DOI] [PubMed] [Google Scholar]
- 2.Frank G, Lawless ST, Steinberg TH. Improving physician communication through an automated, integrated sign-out system. J Healthc Inf Manag. 2005;19:68–74. [PubMed] [Google Scholar]
- 3.Institute of Medicine (US) Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. Committee on Quality of Health Care in America. [PubMed] [Google Scholar]
- 4.The Joint Commission 2006 Critical Access Hospital and Hospital National Patient Safety Goals. 2006 [cited]Available from: http://www.jointcommission.org/GeneralPublic/NPSG/06_npsg_dsc.htm. [Google Scholar]
- 5.Petersen LA, Orav EJ, Teich JM, O’Neil AC, Brennan TA. Using a computerized sign-out program to improve continuity of inpatient care and prevent adverse events. Jt Comm J Qual Improv. 1998;24:77–87. doi: 10.1016/s1070-3241(16)30363-7. [DOI] [PubMed] [Google Scholar]
- 6.Van Eaton EG, Horvath KD, Lober WB, Pellegrini CA. Organizing the transfer of patient care information: the development of a computerized resident sign-out system. Surgery. 2004;136:5–13. doi: 10.1016/j.surg.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 7.Van Eaton EG, McDonough K, Lober WB, Johnson EA, Pellegrini CA, Horvath KD. Safety of using a computerized rounding and sign-out system to reduce resident duty hours. Acad Med. 2010;85:1189–1195. doi: 10.1097/ACM.0b013e3181e0116f. [DOI] [PubMed] [Google Scholar]
- 8.Bernstein JA, Imler DL, Sharek P, Longhurst CA. Improved physician work flow after integrating sign-out notes into the electronic medical record. Jt Comm J Qual Patient Saf. 2010;36:72–78. doi: 10.1016/s1553-7250(10)36013-2. [DOI] [PubMed] [Google Scholar]
- 9.Cordero L, Kuehn L, Kumar RR, Mekhjian HS. Impact of computerized physician order entry on clinical practice in a newborn intensive care unit. J Perinatol. 2004;24:88–93. doi: 10.1038/sj.jp.7211000. [DOI] [PubMed] [Google Scholar]
- 10.HIMSS Analytics: Healthcare IT Data, Research, and Analysis. 2010 [cited]Available from: http://www.himssanalytics.org/hc_providers/emr_adoption.asp. [Google Scholar]
- 11.Carroll AE, Tarczy-Hornoch P, O’Reilly E, Christakis DA. Resident documentation discrepancies in a neonatal intensive care unit. Pediatrics. 2003;111:976–980. doi: 10.1542/peds.111.5.976. [DOI] [PubMed] [Google Scholar]
- 12.Campbell EM, Sittig DF, Ash JS, Guappone KP, Dykstra RH. Types of unintended consequences related to computerized provider order entry. J Am Med Inform Assoc. 2006;13:547–556. doi: 10.1197/jamia.M2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Poissant L, Pereira J, Tamblyn R, Kawasumi Y. The impact of electronic health records on time efficiency of physicians and nurses: a systematic review. J Am Med Inform Assoc. 2005;12:505–516. doi: 10.1197/jamia.M1700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sidlow R, Katz-Sidlow RJ. Using a computerized sign-out system to improve physician-nurse communication. Jt Comm J Qual Patient Saf. 2006;32:32–36. doi: 10.1016/s1553-7250(06)32005-3. [DOI] [PubMed] [Google Scholar]