Abstract
Bertolotti’s syndrome must be considered as a differential diagnosis for lower back pain in young people. Treatment, whether conservative or operative, is still debatable. In this paper, we report a case of a 20-year-old girl presenting with lower back pain for 8 years. We administered injection with local anaesthetic and steroid injections within the pseudo-articulation; however, the pain was relieved for 3 weeks. Surgical excision of the pseudo-articulation successfully treated her back pain and the sciatica.
Keywords: Bertolotti’s syndrome, back pain in young patients, transitional vertebrae
Introduction
Bertolotti’s syndrome is characterised by the presence of a variation of the fifth lumbar (L5) vertebra with a large transverse process, either articulated or fused with the sacral basis or iliac crest, producing a chronic, persistent lower back pain.1 Bertolotti stated as early as in 1917 that these abnormal vertebrae may produce lower back pain due to arthritic changes occurring at the site of pseudarthrosis. We report a case of a young patient presenting with severe chronic back pain, which resolved once the diagnosis of Bertolotti’s syndrome was made and appropriate treatment was instituted.
Case report
A 20-year-old girl presented to us in December 2013 with a history of lower back pain for 8 years. She did not have any co-morbidities. The back pain was associated with right leg radiculopathy. She had been taking of nonsteroidal anti-inflammatory drugs (Voltaren 50 mg tds) and opioids (Tramadol 50 mg tds) for 5 years. She required admission to the accident and emergency department frequently for parenteral analgesia. She regularly was seen by general practitioners (GPs) and was treated for mechanical back pain. A year prior to seeing us, she required intramuscular morphine injections 2–3 times a week. She was unemployed as her pain was debilitating. Between the year 2010 and 2013, the patient underwent three lumbar sacral magnetic resonance imaging (MRI), one cervical spine MRI, one computed tomography (CT) of the lumbar spine and eight plain lumbar sacral radiography. Finally, a nerve conduction study (NCS) was done. The MRI scans reported disc degeneration at L4/L5 with no lateral or central stenosis. CT reported unilateral right sacralisation of the L5 vertebrae. The NCS showed normal results.
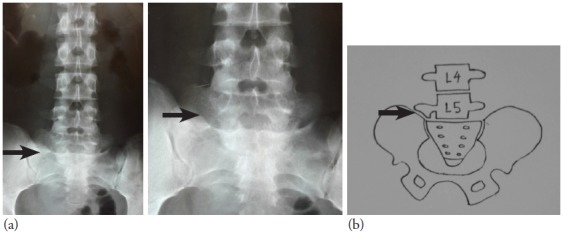
Physical examination revealed a small-built girl with an antalgic gait. There was an area of tenderness at the lower lumbar region and the right posterior iliac and sacrum region. She had guarding of the right paravertebral muscle. Straight leg raising/Lasegue’s sign was positive over the right leg, which suggested that the patient was having lumbar radiculopathy. No motor and sensory deficits were noted. Anterior posterior radiograph of the lumbar sacral spine showed the presence of pseudo articulation of the right L5 transverse process and the sacrum (Figure 1).
Figure 1: (a) Pre-operative anteroposterior (AP) lumbar sacral radiograph showing the enlarged right L5 transverse process forming a pseudo-articulation with the sacrum. The left transverse process and the sacrum are normal. (b) Diagrammatic representation of the radiographs showing these abnormalities.
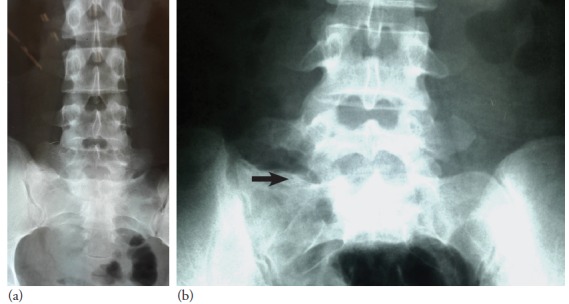
At this juncture, there were two possible pain the back: cause of pseudo-articulation of the right transverse process with the sacrum or the degenerative disc between L4 and L5. We administered an injection with local anaesthetic and steroid at the pseudo-articulation of the transverse process and sacrum. It relieved her back pain and radiculopathy for 3 weeks before the symptoms recurred with greater intensity. The injection identified the pain generator. In view of long-standing debilitating pain with failure of non-surgical treatment, surgical excision of the pseudo-articulation of the right L5 transverse process with the sacrum was performed (Figure 2). The pre and post surgery radiographs showed the recreation of the normal gap between the transverse process and the sacrum (Figure 3 )
Figure 2: Intra-operative picture showing the pseudo-articulation between the transverse process of L5 (superior) and sacrum (inferior).
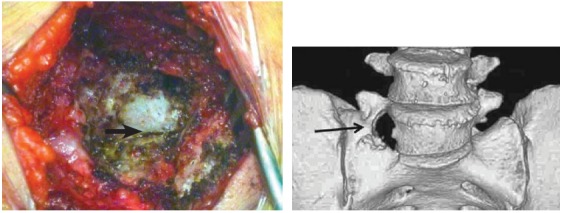
Figure 3: Pre-operative radiograph (a) Post-operative AP lumbar sacral radiographs showing resected area with recreation of the gap between the transverse process of the right L5 vertebrae and the sacrum (b).
Discussion
Lower back pain is the most common reason for seeking medical advice; it occurs in 80% of adults at some stage. Management of lower back pain starts with a thorough history taking. The history should include all the potential red and yellow flags of lower back pain. Most patients have one red flag; however, patients with two or more red flags necessitate an early referral to an orthopaedic surgeon.2 The patient in our study had six red flags: age of 20 years, pain persisting more than 3 months, failure to improve with therapy, pain at rest, severe pain and tenderness of the vertebrae.
In 1917, Bertolotti described unilateral and bilateral enlargement of the transverse process of the most caudal lumbar vertebra, which may articulate or fuse with the sacrum or ilium. The incidence of Bertolotti’s syndrome is 18.5% in individual aged less than 30 years.3 Examining a patient with Bertolotti’s syndrome would reveal little information. There may be mild to moderate tenderness at the lower lumbar region, particularly around the pseudo-articulation. Range of motion of the spine may be limited during periods of acute exacerbation and may be normal when they are not in pain. Occasionally, there may be radicular signs. There are many patients with Bertolotti’s syndrome who would present incidentally during routine radiographic examination. This subset of patients may not have symptoms or signs of this condition. Diagnosis of Bertolotti’s syndrome is based on radiological findings and their correlation with the clinical presentation. Plain radiographs of the lumbar–sacral spine in anterior and posterior views showing the presence of an enlarged transverse process of the L5 vertebrae that forms a joint with the sacrum or the ilium bone would suggest Bertolotti’s syndrome as the diagnosis.
There is controversy with regards to whether such an abnormal vertebra produces symptoms of lower back pain. Many authors have supported a relationship between lumbo-sacral transitional vertebra and lower back pain, while Castellvi et al. found that in patients with back pain and sciatica, the transitional vertebra was prevalence of 30%.4 Till today, there is no consensus on how to treat these patients. Marks and Thulbourne studied 10 patients who received a steroid and local anaesthetic infiltration for their anomalous lumbo-sacral articulations for severe chronic lower back pain. Immediate relief was found in eight, but only one patient remained pain free 2 years later.5 Jonsson et al. also reported symptomatic relief in 9 of 11 patients who had an injection of local anaesthetic into the anomalous articulation. However, these patients subsequently underwent resection of the accessory joint; At a mean follow-up of 17 months, nine patients reported relief from pain.6 For Bertolotti’s syndrome that fails to respond to non-operative treatment, including NSAIDs, activity modification, transcutaneous electrical nerve stimulation therapies and steroid injections, surgical excision is indicated.
Conclusion
Chronic lower back pain in younger patients is a red flag sign. Identifying the pain generator requires a thorough evaluation. The assessment includes history taking, physical examination and radiological imaging. Failure to follow this algorithm will lead to misdiagnosis and sub-optimal management. A plain radiograph of the lumbar sacral spine would confirm the diagnosis of Bertolotti’s syndrome. A diagnostic local anaesthetic injection would identify the pseudo-articulation of the L5 transverse process and sacrum as the pain generator, and appropriate treatment could be introduced.
How does this paper make a difference to general practice?
Back pain is the second most common reason to visit a primary care physician
Back pain in young patients are uncommon and can be a diagnostic dilemma
The present case shows a thorough history taking and physical examination with a simple imaging technique world have ascertained the clinical diagnosis
Early diagnosis and prompt management, as in this case, can benefit the patient economically and socially
This case illustrates perfectly why the first imaging in chronic lower back pain should be a plain radiography of the lumbar sacral region and not an MRI or CT
Footnotes
Conflict of interest: The authors declare that there are no conflicts of interest.
Funding: This research received no specific grant from the government or any other funding agency in the public, commercial or not-for-profit sectors
Manmohan S, Dzulkarnain A, Nor Azlin ZA, Fazir M. Bertolotti’s syndrome: A commonly missed cause of back pain in young patients Malays Fam Physician. 2015;10(2);55-58.
References
- 1.Bertolotti M. Contributo alla conoscenze dei vizi di differenzazione regionale del rachide con speciale riguardo alla assimilazione sacrale della V. lombare. Radio-logique Medica (Torino) 1917;4:113–44. (in Italian) [Google Scholar]
- 2.Underwood M. Diagnosing acute nonspecific low back pain: Time to lower the red flags? Arthritis Rheum. 2009;60(10):2855–7. doi: 10.1002/art.24858. [DOI] [PubMed] [Google Scholar]
- 3.Quinlan JF, Duke D, Eustace S. Bertolotti syndrome: Cause of back pain in young people. J Bone Joint Surg (Br) 2006:88–B:1183–6. doi: 10.1302/0301-620X.88B9.17211. [DOI] [PubMed] [Google Scholar]
- 4.Castellvi AE, Glodstein LA, Chan DPK. Lumbarsacral transitional vertebrae and their relationship with lumbar extradural defects. Spine. 1983;9:493–5. doi: 10.1097/00007632-198407000-00014. [DOI] [PubMed] [Google Scholar]
- 5.Marks RC, Thulbourne T. Infiltration of anomalous articulations: Steroid and anesthetic injections in 10 back-pain patients. Acta Orthop Scand. 1991;62:139–41. doi: 10.3109/17453679108999242. [DOI] [PubMed] [Google Scholar]
- 6.Jonsson B, Stromqvist B, Egund N. Anomalous lumbosacral articulations and low back-pain: Evaluation and treatment. Spine. 1989;14:831–4. doi: 10.1097/00007632-198908000-00009. [DOI] [PubMed] [Google Scholar]


