Abstract
Background and aims
Drinking urges during treatment for alcohol use disorders (AUDs) are common, can cause distress, and predict relapse. Clients may have little awareness of how their drinking urges might be expected to change during AUD treatment in general and in response to initiating abstinence. The aim of the present study was to test whether drinking urges change on a daily level during treatment and after initiating abstinence.
Design
Secondary data analysis was performed using daily drinking urge ratings from two randomized clinical trials.
Setting and Participants
Women (N=98) and men (N=79) with AUDs in separate clinical trials of outpatient AUD-focused cognitive-behavioral therapy.
Measurements
Daily dichotomous indicators of any drinking urges or acute escalations in urges (i.e., at least two more urges compared with the previous day) were examined using generalized linear mixed growth-curve modeling.
Findings
Participants who initiated abstinence reported reductions in urges immediately thereafter (log odds ratios: women B=−0.701, p<.001; men B=−0.628, p=0.018), followed by additional, gradual reductions over time (women B=−0.118, p<.001; men B=−0.141, p<.001). Participants who entered treatment abstaining from alcohol also reported significant reductions in urges over time (women B=−0.147, p<.001; men B=−0.142, p<.001). Participants who drank throughout treatment had smaller (women B=−0.042, p =.012) or no reductions in urges (men B=0.015, p=.545). There was no evidence that urges systematically increased in response to initiating abstinence.
Conclusions
Drinking urges during outpatient behavioral treatment for alcohol use disorders may be maintained in part by alcohol consumption. Initiating abstinence is associated with reductions in drinking urges immediately and then more gradually over time.
Keywords: abstinence initiation, alcohol, alcohol use disorder treatment, cognitive-behavioral therapy, craving, drinking urges, process of change, quit date
Individuals with alcohol use disorders (AUDs) commonly experience urges to drink despite wanting to reduce their alcohol use. This phenomenon is now recognized as a core feature of AUDs [1-2] and is increasingly studied in clinical research [3]. Drinking urges in AUD treatment predict subsequent alcohol use and relapse [4-9] from a single day [10-11] to three years later [7]. Conversely, alcohol use also appears to intensify or increase urges based on cross-sectional [12-13] and prospective measurements spanning from single day [10] to two-months [14].
A bidirectional association between urges and alcohol consumption is consistent with contemporary cognitive-behavioral models of addiction [15-18]. These models generally posit that urges are elicited by cues, and when followed by drinking the associations between cue, urge, and drinking are strengthened. The likelihood of subsequent cue-urge patterns increases, which helps maintain urges. In contrast, abstaining from alcohol should weaken these associations and remove a source of urge cues, but also may cause withdrawal symptoms that could increase urges.
Clients often report worrying that initiating abstinence will increase their urges [19-20]. This fear is clinically relevant since urges are reported as distressing, potentially reducing motivation for abstinence or creating negative treatment expectancies. Clients also may lack clarity about if, when, and how much their urges may change during treatment or when initiating abstinence. Providing evidence-based information about individual differences in urges and changes in urges over time may help clients make better-informed treatment decisions, reduce ambivalence, and promote positive treatment expectancies. Measured on a weekly or daily basis, urges have been shown to decrease during behavioral treatment [5, 21-22]. However, there is little research on trajectories of daily urges during behavioral treatment before and after initiating abstinence.
The present study aims to (1) provide descriptive statistics on between-individual variability in daily drinking urges during two behavioral treatment studies, and (2) model patterns of change over time in daily drinking urges during treatment. Patterns of drinking urges were modeled in relation to two factors that were hypothesized to affect drinking urges, namely (1) initiating abstinence and (2) history of alcohol withdrawal symptoms.
Method
Participants
The present study is a secondary analysis of data from two randomized clinical trials testing alcohol behavioral couple therapy (ABCT) with women (“women’s study” [23]) and men (“men’s study” [24]). The women’s study compared individual cognitive-behavioral therapy to ABCT and the men’s study compared ABCT, ABCT with Alcoholics Anonymous components, and ABCT with relapse prevention components.
Participants met DSM-III or DSM-IV criteria for alcohol abuse or dependence, consumed alcohol within 60 days before contacting the treatment team, were in committed heterosexual relationships, and had partners who were willing to attend treatment sessions. Exclusionary criteria included current drug dependence with physiological dependence (assessed via the Structured Clinical Interview for DSM-IV [SCID] [25]), current psychotic disorder (assessed via the SCID in the women’s study and the Symptom Checklist-90 [26] in the men’s study), or significant cognitive impairment (<25 on Mini-Mental Status Exam [27]). The men’s study excluded participants with partners who had a current alcohol use disorder.
Among 102 participants in the original women’s study, 98 had enough daily drinking recordings to determine abstinence status (i.e., at least 14 days, described below) and were included here. The men’s study originally included 90 participants; 79 met identical criteria and were included here. Participant descriptive statistics are presented in Table 1.
Table 1.
Participant Demographics
| Women's Study
(N = 98) N (%) |
Men's Study
(N = 79) N (%) |
|||
|---|---|---|---|---|
|
|
||||
| Race and Ethnicity | ||||
| White/Caucasian | 94 | (95.92) | 71 | (91.03) |
| Black/African American | 4 | (4.08) | 3 | (3.85) |
| American Indian/Alaskan Native | 0 | 3 | (3.85) | |
| Hispanic/Latino | 0 | 1 | (1.28) | |
| Not reported | 0 | 1 | (1.28) | |
| Percent Endorsing Alcohol Withdrawal | 53 | (54.08) | 40 | (50.63) |
| M | (SD) | M | (SD) | |
|
|
||||
| Age | 45.17 | (9.25) | 39.85 | (10.75) |
| Education (Years) | 14.61 | (2.58) | 13.46 | (2.41) |
| Alcohol Dependence Symptoms | ||||
| SCID | 4.70 | (1.29) | ||
| CIDI-SAM | 25.37 | (7.76) | ||
Note. SCID = Structured Clinical Interview for DSM-IV Disorders, CIDI-SAM = Composite International Diagnostic Interview, Substance Abuse Module. The SCID-IV assessed 7 DSM-IV alcohol dependence symptoms. The CIDI-SAM assessed responses to 47 yes/no items assessing alcohol dependence symptoms.
Measures
Alcohol dependence
Alcohol dependence and history of withdrawal were assessed using the Composite International Diagnostic Interview, Substance Abuse Module [28] (men’s study) and the SCID (women’s study).
Daily drinking and urge logs
As part of treatment, participants recorded daily drinking urges and alcohol consumption using self-monitoring cards. Cards included fields to record triggering situations, times, and intensities of urges, with room to record multiple urges per day. Urges were not assessed before or after the treatment period. There were 11,456 self-monitoring cards with drinking urge data in the women’s study and 7,221 in the men’s study.
The number of urges per day and urge intensity ratings were highly non-normally distributed and were dichotomized to facilitate statistical analysis. Dichotomous variables indicated (1) the presence or absence of any urges each day and (2) the presence or absence of an acute escalation of two or more urges within a single day compared to number of urges the day before [29]. Together, these indices captured both the presence vs. absence of urges and sudden increases in urges relative to prior days. These variables were modestly correlated, r=0.32, p<.001, indicating some overlap but a likelihood of measuring separate aspects of urges.
Procedures
Participants received manual-guided cognitive-behavioral AUD treatment in individual or couples format. Treatments were abstinence-oriented and clients agreed to this goal at the onset of treatment. Therapists were trained in the treatment protocols and received regular supervision. Treatment consisted of up to 20 sessions in 6 months (women’s study) or 15 sessions with up to two emergency sessions with no limited time period (men’s study). Individual therapy sessions were 60 minutes; couple sessions were 90 minutes. Treatment fidelity was rated for a subset of first- and mid-treatment sessions and indicated adequate treatment delivery [30].
Instructions and a rationale for self-monitoring were provided in the first session. Participants were asked to carry monitoring cards each day and to record urges in real time. Urges were defined as any thought, desire, or craving to drink, and participants were encouraged to use a low threshold by noting even small thoughts and desires and any urges that preceded drinking. At the beginning of all subsequent treatment sessions, urge recordings were reviewed, graphed, and discussed. When self-monitoring cards were missing or incomplete, therapists were instructed to fill in this information with the clients through retrospective recall. Fidelity ratings indicated that cards were reviewed in 93.7% of the 79 mid-treatment sessions available for rating [30].
Analytic Plan
Men’s and women’s study data were analyzed separately to test the replicability of the results, except when combining the two samples facilitated statistical modeling (e.g., small n’s preventing model convergence). Analyses aimed to (1) describe between-subject variability in urges using descriptive statistics and (2) identify systematic changes in urges over time using growth curve models. Participants were classified as either “quitters,” “abstainers,” or “continued drinkers” depending on if and when the first 14 days of continuous abstinence occurred in treatment. “Quitters” had some alcohol consumption during the first 14 days of treatment but eventually obtained at least 14 days of continuous abstinence. “Abstainers” were abstinent for the first 14 days of treatment, and “continued drinkers” never obtained 14 days of continuous abstinence. Classification status was not affected by drinking beyond the initial 14-day abstinence period. In the women’s and men’s studies, respectively, there were 44 and 30 quitters, 34 and 33 abstainers, and 20 and 16 continued drinkers. Classification based on a 14-day abstinence period informed by previous research suggesting a low likelihood of 14 or more consecutive abstinent days between drinking episodes before and during alcohol treatment [31]. Likewise, only 9% of participants in the present samples (women’s n=9; men’s n=7) had any abstinence period of 14 days or longer between drinking episodes for the 90 days before baseline interview.
Growth curve models identified systematic changes in urges for each group. Moderation by alcohol withdrawal symptom status also was examined. Data were utilized from 28 days before through 120 days after abstinence was initiated for quitters, after which point urge data was available for less than half of the participants. Data were utilized from the 1st to the 120th day of treatment for abstainers and continued drinkers. Time variables were centered in relation to the day abstinence was initiated (quitters) or the first day of treatment (abstainers and continued drinkers). Growth curves were estimated using generalized linear mixed models [32-33] using lme4 in R [34] with maximum likelihood to reduce bias from missing data [35].
Results
Daily Drinking Urges: Between-Participant Variability
The proportion of days with at least one drinking urge varied considerably by participant. Intra-class correlations (ICCs) for intercept-only GLMMs for drinking urges were 0.44 and 0.55 for the women’s and men’s studies, respectively, indicating that approximately half of the variability in all observed daily drinking urges was accounted for by between-individual differences [36]. Median odds ratios (i.e., the median value of all pairwise odds ratio comparisons between subjects [36]), which also describe between-individual variability, were 4.63 and 6.79 for the women’s and men’s studies, respectively. These values mean that for two randomly sampled individuals from the study populations, their individual odds of experiencing daily drinking urges would typically differ by an odds ratio of 4.37, suggesting considerable heterogeneity.
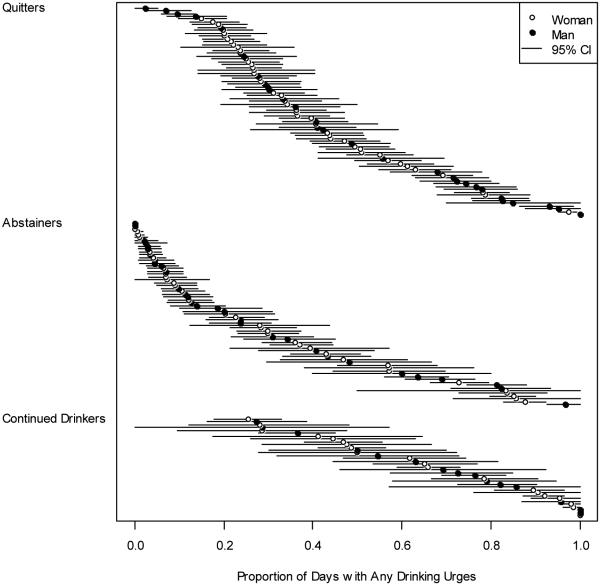
The proportions of days with drinking urges for each individual and 95% confidence intervals for these estimates are shown in Figure 1. Substantial variability was present for all three drinking status groups, with participants experiencing urges in the full range of 0% to 100% of days. The quitter and abstainer groups had a lower prevalence of urges than the continued drinking group (ps<.001); however, even in these groups many individuals had a high proportion of days with urges.
Figure 1.
Dot chart of the proportions of days with drinking urges by participant (dots) with 95% confidence interval estimates (lines).
Daily Drinking Urges: Growth Curves
Urge growth curves by drinking status
Omnibus testing indicated significant drinking status × time interactions (ps<.001) supporting the hypothesis of different growth trajectories for different drinking groups. Results for each group are reported in Table 2 (women’s study) and Table 3 (men’s study). In both studies, quitters experienced immediate reductions in urges after initiating abstinence. Quitters in both studies had further decreases in urges over time after abstinence was initiated. In the women’s study, urges declined over time before initiating abstinence (p=0.03); this effect was similar in direction and magnitude but was not significant (p=0.08) for the men’s study.
Table 2.
Daily Drinking Urges Growth Curve Models by Group, Women's Study
| Quitters | Estimate | 95% CI | p |
|---|---|---|---|
|
|
|||
| Intercept | 0.535 | 0.082 , 0.990 | .020 |
| Post-abstinence immediate change | −0.701 | −1.042 , −0.364 | <.001 |
| Pre-abstinence change over time | −0.156 | −0.299 , −0.014 | .032 |
| Post-abstinence change over time | −0.118 | −0.136 , −0.102 | <.001 |
| Intercept variance | 1.188 | 0.763 , 1.943 | |
| Abstainers | |||
| Intercept | −0.193 | −0.935 , 0.538 | .595 |
| Change over time | −0.147 | −0.171 , −0.123 | <.001 |
| Intercept variance | 4.157 | 2.520 , 7.347 | |
| Drinkers | |||
| Intercept | 1.256 | 0.472 , 2.083 | .001 |
| Change over time | −0.042 | −0.076 , −0.009 | .012 |
| Intercept variance | 2.666 | 1.362 , 5.834 | |
Note. Post-abstinence immediate change is a dummy variable equal to 0 before abstinence was initiated and 1 after abstinence was initiated; pre-abstinence and post-abstinence change over time are piecewise linear growth terms for the periods before and after abstinence was initiated. All variables for change over time are scaled such that a one-unit change in the predictor corresponds to a time period of one week. Estimates are conditional log-odds ratios.
Table 3.
Daily Drinking Urges Growth Curve Models by Group, Men's Study
| Quitters | Estimate | 95% CI | p |
|---|---|---|---|
|
|
|||
| Intercept | 1.085 | 0.290 , 1.898 | .007 |
| Post-abstinence immediate change | −0.628 | −1.154 , −0.106 | .018 |
| Pre-abstinence change over time | −0.196 | −0.418 , 0.023 | .081 |
| Post-abstinence change over time | −0.141 | −0.173 , −0.109 | <.001 |
| Intercept variance | 3.039 | 1.799 , 5.556 | |
| Abstainers | |||
| Intercept | −0.835 | −1.595 , −0.102 | .023 |
| Change over time | −0.142 | −0.169 , −0.115 | <.001 |
| Intercept variance | 3.726 | 2.176 , 6.906 | |
| Drinkers | |||
| Intercept | 0.990 | 0.163 , 1.928 | .015 |
| Change over time | 0.015 | −0.034 , 0.065 | .545 |
| Intercept variance | 1.980 | 0.768 , 5.830 | |
Note. See Table 2 footnote for additional information on growth-curve model terms.
Abstainers in both studies showed significant reductions in urges over the time during treatment. Continued drinkers in the women’s study showed significant reductions in urges over time, but to a significantly smaller degree (ps<.001) than abstainers or quitters. This effect was not replicated in the men’s study, where continued drinkers experienced no change over time (p=0.54). However, daily urge data were particularly sparse for male continued drinkers, (627 days available) compared to male quitters (3093) and abstainers (3501), especially after the 7th week of treatment.
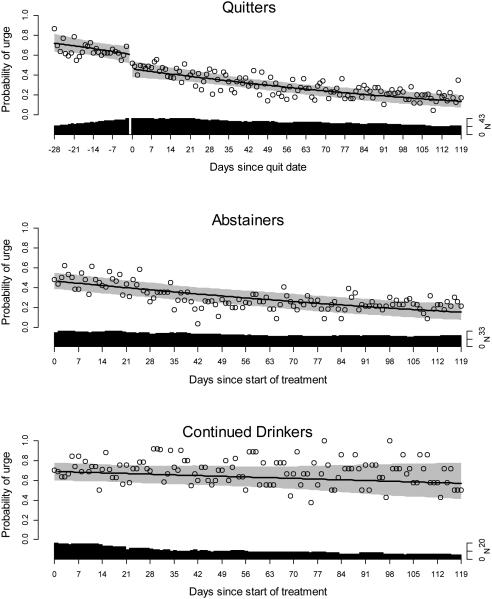
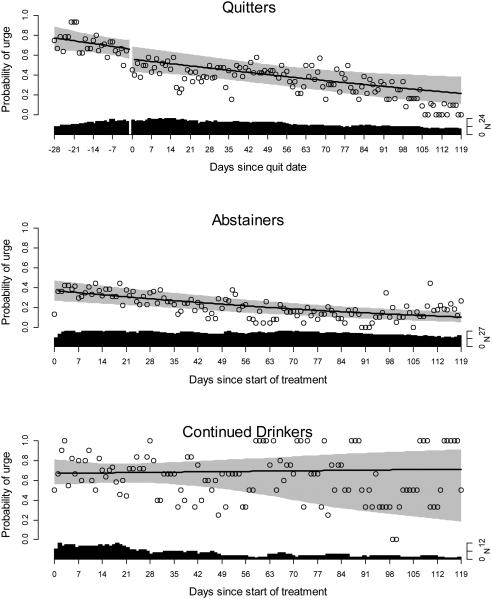
Growth curves are illustrated in Figures 2 (women’s study) and 3 (men’s study), which show model-predicted trajectories of the probability of experiencing any urges on a particular day (lines) with bootstrapped 95% confidence intervals (gray regions), observed proportions of participants who reported urges each day (dots), and the number of days with valid urge data (black regions). These figures show that urges were quite frequent during periods of drinking (i.e., continued drinkers and quitters prior to initiating abstinence), then suddenly decreased when abstinence was initiated (day zero for quitters), and continued to decrease gradually over time after abstinence was initiated (i.e., abstainers and quitters after initiating abstinence). For example, during periods of drinking, urges were typically reported on about 60-85% of days. Then, when abstinence was initiated, urges occurred approximately 40-60% of days, but continued to decline over treatment and occurred around 20-40% of days near the end of the 120 day period.
Figure 2.
Drinking urge trajectories for women’s study by drinking category. Lines represent model-estimated probabilities of daily drinking urges, gray regions represent 95% confidence intervals for model estimates, dots represent observed proportions of participants reporting any urge on each day, black regions represent the number of days with valid urge data present for analysis. Modeled values are based on marginal mean estimates [33].
Figure 3.
Drinking urge trajectories for men’s study by drinking category. See Figure 2 for detailed figure explanation.
Urge growth curves by withdrawal status
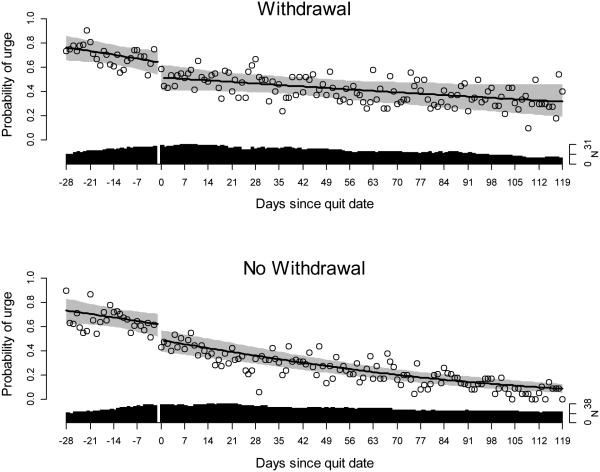
Differences in urge trajectories based on the presence or absence of past alcohol withdrawal symptoms were examined specifically for quitters because their urge data could be calibrated to their exact quit date. Data from the women’s and men’s studies were combined to increase statistical power due to the smaller sample sizes from dividing quitters into withdrawal and non-withdrawal groups.
Results in Table 4 show that for both groups, urges decreased immediately after initiating abstinence, and then continued to decrease over time. However, urges decreased considerably less over time for individuals with a history of withdrawal (difference in slopes, B=0.10, SE=0.02, z=6.47, p<.001).
Table 4.
Daily Drinking Urges Growth Curve Models by Withdrawal Symptoms, Quitters Only, Men's and Women's Studies Combined
| Withdrawal Symptoms Present | Estimate | 95% CI | p |
|---|---|---|---|
|
|
|||
| Intercept | 0.876 | 0.246 , 1.520 | .006 |
| Post-abstinence immediate change | −0.662 | −1.092 , −0.236 | .002 |
| Pre-abstinence change over time | −0.184 | −0.363 , −0.006 | .043 |
| Post-abstinence change over time | −0.070 | −0.092 , −0.048 | <.001 |
| Intercept variance | 2.020 | 1.214 , 3.605 | |
| Withdrawal Symptoms Absent | |||
| Intercept | 0.591 | 0.060 , 1.126 | .028 |
| Post-abstinence immediate change | −0.671 | −1.054 , −0.293 | .001 |
| Pre-abstinence change over time | −0.172 | −0.334 , −0.011 | .037 |
| Post-abstinence change over time | −0.168 | −0.189 , −0.147 | <.001 |
| Intercept variance | 1.637 | 1.034 , 2.733 | |
Note. See Table 2 footnote for additional information on growth-curve model terms.
Growth curves are illustrated in Figure 4. In both groups, drinking urges were initially high, then decreased immediately once abstinence was initiated and continued to decline, but to a lesser degree for individuals with a history of withdrawal.
Figure 4.
Drinking urge trajectories for men’s and women’s study by withdrawal status. See Figure 2 for detailed figure explanation.
Acute Escalations of Urges: Between-Participant Variability
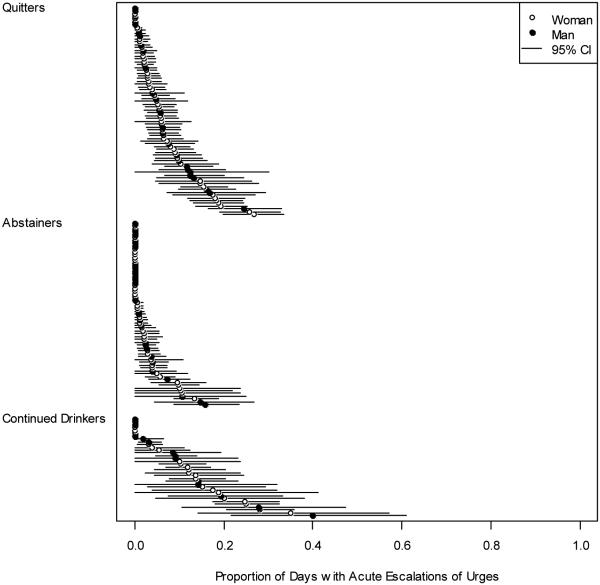
An intercept-only model of acute escalations in urges (increase by two or more urges within a day compared to the previous day) yielded ICCs of 0.30 and 0.41 for the women’s and men’s studies, respectively. Mean odds ratios were 3.06 and 4.25, respectively, indicating substantial between-individual variability as illustrated by drinking status group in Figure 5. Continued drinkers had more frequent acute escalations than abstainers (p<.001) and quitters (p=.01). Several participants in each group experienced no acute escalations, while several participants experienced them relatively frequently, for example, on 10-40% of days.
Figure 5.
Dot chart of the proportions of days with acute escalations of drinking urges by participant (dots) with 95% confidence interval estimates (lines).
Acute Escalations of Urges: Growth Curves
Acute escalations of urges by drinking status
Growth curve models of acute escalations of urges are presented in Table 5 with data from the women’s and men’s studies combined due to the lower prevalence of acute escalations. For quitters, the likelihood of experiencing an acute escalation of urges was significantly reduced immediately after abstinence was initiated, then continued to decline over time. Quitters did not experience significant change in acute escalations before abstinence was initiated. Abstainers and continued drinkers experienced gradual reductions in acute escalations over time during treatment. At the beginning of treatment, abstainers had significantly fewer acute urge escalations compared to continued drinkers, difference in intercepts B=−1.82, SE=0.32, z=−5.65, p<.001, although the amount of reduction over time was not significantly different between abstainers and continued drinkers, difference in slopes B=−0.02, SE=0.02, z=−0.92, p=.36.
Table 5.
Acute Escalations of Urges Growth Curve Models by Group, Women's and Men's Studies Combined
| Quitters | Estimate | 95% CI | p |
|---|---|---|---|
|
|
|||
| Intercept | −2.158 | −2.575 , −1.763 | <.001 |
| Post-abstinence immediate change | −0.808 | −1.192 , −0.419 | <.001 |
| Pre-abstinence change over time | 0.090 | −0.062 , 0.243 | .242 |
| Post-abstinence change over time | −0.047 | −0.075 , −0.021 | .001 |
| Intercept variance | 0.943 | 0.596 , 1.530 | |
| Abstainers | |||
| Intercept | −4.079 | −4.693 , −3.575 | <.001 |
| Change over time | −0.058 | −0.097 , −0.020 | .003 |
| Intercept variance | 1.967 | 1.062 , 3.761 | |
| Drinkers | |||
| Intercept | −1.971 | −2.395 , −1.605 | <.001 |
| Change over time | −0.049 | −0.083 , −0.015 | .005 |
| Intercept variance | 0.714 | 0.334 , 1.561 | |
Note. See Table 2 footnote for additional information on growth-curve model terms.
Acute escalations of urges by history of withdrawal
The patterns of acute urge escalations for quitters with and without histories of withdrawal are presented in Table 6. Participants with histories of withdrawal did not have significant immediate reductions in acute urge escalations after initiating abstinence (p=0.052), and had no changes over time in acute escalations before or after abstinence was initiated. Participants without withdrawal symptoms experienced significant reductions in acute escalations immediately after initiating abstinence (p<.001), which continued to significantly decrease over time. Neither group experienced reductions in acute escalations of urges prior to initiating abstinence. Additional analyses that modeled days with “strong urges” (i.e., mean daily urge ratings ≥ the scale midpoint) produced an identical pattern of results as acute urge escalations, with the exception that withdrawers experienced decreases in strong urges over time before and after initiating abstinence.
Table 6.
Acute Escalations of Growth Curve Models by Withdrawal Symptoms, Quitters Only, Men's and Women's Studies Combined
| Withdrawal Symptoms Present | Estimate | 95% CI | p |
|---|---|---|---|
|
|
|||
| Intercept | −2.389 | −3.061 , −1.767 | <.001 |
| Post-abstinence immediate change | −0.581 | −1.168 , 0.025 | .052 |
| Pre-abstinence change over time | 0.099 | −0.147 , 0.350 | .427 |
| Post-abstinence change over time | 0.005 | −0.030 , 0.041 | .768 |
| Intercept variance | 1.023 | 0.525 , 2.086 | |
| Withdrawal Symptoms Absent | |||
| Intercept | −1.965 | −2.499 , −1.466 | <.001 |
| Post-abstinence immediate change | −0.864 | −1.374 , −0.349 | .001 |
| Pre-abstinence change over time | 0.084 | −0.109 , 0.279 | .388 |
| Post-abstinence change over time | −0.122 | −0.169 , −0.078 | <.001 |
| Intercept variance | 0.827 | 0.425 , 1.657 | |
Note. See Table 2 footnote for additional information on growth-curve model terms.
Discussion
The present study examined how drinking urges vary between individuals and over time during cognitive-behavioral AUD treatment. The prevalence of daily drinking urges and acute escalations of urges was highly variable between individuals. In fact, between-individual differences accounted for approximately one-third to one-half of the overall variance in all observed daily urges during treatment.
Participants in both studies had reductions in daily urges immediately after initiating abstinence and additionally over time after initiating abstinence or entering treatment already abstaining. In contrast, participants who did not initiate abstinence experienced, on average, slower declines in drinking urges (women’s study) or no decrease (men’s study). Participants with and without histories of alcohol withdrawal experienced significant reductions in drinking urges immediately or gradually over time after initiating abstinence. Acute escalations of urges declined over time before and after initiating abstinence for participants without withdrawal but not for participants with withdrawal. Continued drinkers and abstainers both had significant reductions in acute urge escalations during treatment.
Clinical Implications
Treatment providers may inform clients that people in AUD treatment vary highly in the amount of daily urges and acute escalations of urges they experience. This may help normalize clients’ experiences, for example, by knowing that it is not unusual to experience very many or very few urges. This could lead into discussions of clients’ unique antecedents and consequences of urges [37], and such discussions could continue throughout treatment as urge patterns change.
The current findings are promising for clients who hope that their drinking urges will decrease. Clients may benefit from knowing that initiating abstinence is likely to be accompanied by an immediate decrease in drinking urges, followed by additional gradual decreases in urges over time. This is contrary to concerns of some clients that initiating abstinence may cause an increase in urges. Treatment providers may inform clients that, for most people, drinking urges decrease rather than increase upon initiating abstinence, potentially shifting expectancies, providing incentive for initiating abstinence, and instilling hope that discomfort caused by urges is likely to decrease.
Clients with alcohol withdrawal symptoms likewise can be reassured that they are likely to experience reductions in drinking urges upon the initiation of abstinence, although slower reductions may be expected. A history of withdrawal symptoms may warrant more in-depth monitoring and discussion of urges, for example, since a higher prevalence of urges can predict relapse [8], create discomfort and demoralization, and reduce self-regulation capacity [38-39].
Theoretical Implications
Contemporary cognitive-behavioral models posit that learned cues elicit motivational states to drink (i.e., drinking urges), and that drinking in these contexts strengthens the associations between cues, urges, and drinking [15-18]. The results of the present study are consistent with this hypothesis, such that periods of drinking were associated with a high frequency of urges, potentially reflecting the maintenance of urge-cue associations. Decreases in urges after initiating abstinence may reflect a weakening of these associations. Moreover, drinking or anticipating drinking itself may elicit urges to drink, and initiating abstinence may have the immediate effect of removing that salient urge cue [40]. Alcohol withdrawal symptoms also may cue urges, which is consistent with the finding of greater maintenance of urges for participants with past withdrawal symptoms even after initiating abstinence. Alternatively, withdrawal symptoms may have served as a proxy for heavier pre-treatment drinking, such that participants with withdrawal had stronger associations between cue, urge, and drinking that weakened over time more slowly.
Urge reductions in alcohol treatment may be partly facilitated by alcohol cessation, which is consistent with previous research showing bidirectional relationships between urges and alcohol use [10-11,14]. If urges and alcohol use are related reciprocally, targeting either variable in treatment may cause improvements in the other, providing multiple entry points for interventions.
Although abstinence was associated with reduced urges, many abstaining individuals still experienced a high prevalence of urges. It may be beneficial to directly target reducing both alcohol use and drinking urges simultaneously [41-42] and to monitor drinking urges as key outcomes even among individuals who are abstinent. Future research may shed light on how to most effectively target alcohol use and drinking urges separately or concurrently among different individuals. Because many individuals reduce or abstain from alcohol use before treatment, future studies may also monitor how urges change before treatment, which was not done in the present study.
Limitations and Strengths
The present study has several limitations. First, there are measurement limitations. Urges were recorded using daily diary cards which were not electronically verified in real-time, and the number of urges recalled retrospectively during sessions (instead of in real-time) was not recorded. Also, drinking urges and cravings are complex constructs with many definitions, conceptualizations, and self-report measures, and the present study used a relatively simple definition of urges as subjective thoughts, desires, or cravings to use alcohol, which does not allow for more nuanced analyses.
Second, there are design limitations that reduced the ability to make causal inferences. For example, participants could not be randomly assigned to abstinence or withdrawal symptom categories, so differences between groups could be influenced by third variables, including differences at baseline or during treatment. The imbalance in data points between groups also led to limitations in the precision of some estimates.
Third, there are analytic limitations. Urge variables were simplified into dichotomous indicators due to statistical violations. Drinking groups were defined based on the presence of 14 days of continuous abstinence, but other classification schemes based on moderated drinking could also be defined and tested. Moderate drinking classifications could be examined in subsequent research but would require careful consideration of clients’ unique criteria for what constitutes successful moderated drinking. Such work also may be more appropriate in treatment settings that include moderated drinking, rather than abstinence, as a primary goal.
The present study also has several strengths. Daily collection of drinking urge data yielded over 18,000 data points. Drinking urges were monitored during a critical period of significant change. The sample was treatment-seeking, improving its clinical relevance, and it had a high percentage of women, who are often under-represented in clinical AUD research. Data were available from two randomized clinical trials, allowing the replicability of the findings to be tested, and the treatments themselves were evidence-based and delivered with good fidelity.
Conclusions
Drinking urges are key components in the maintenance, treatment, and relapse of AUDs and are increasingly of interest in treatment research. Yet, the definition of urges, the manner in which they change over time, and their dynamic relationship with alcohol use are only beginning to be understood by researchers, and clients may have even less understanding of drinking urges. Increased understanding of drinking urges may facilitate improved theoretical models of AUD treatment and allow clients to be better informed about their treatment goals and their day-to-day experiences with this distressing and complicated phenomenon.
Acknowledgement
This research was funded by NIAAA grant numbers T32007455, R01AA007070, R37AA007070. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Alcohol Abuse and Alcoholism or the National Institutes of Health.
Footnotes
Declarations of competing interests: None
References
- 1.Murphy CM, Stojek MK, Few LR, Rothbaum AO, MacKillop J. Craving as an alcohol use disorder symptom in DSM-5: an empirical examination in a treatment-seeking sample. Exp Clin Psychopharmacol. 2014 Feb;22(1):43–9. doi: 10.1037/a0034535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 5th Author; Washington, DC: 2013. [Google Scholar]
- 3.Kavanagh DJ, Statham DJ, Feeney GFX, Young RM, May J, Andrade J, Connor JP. Measurement of alcohol craving. Addict Behav. 2013;38(2):1572–84. doi: 10.1016/j.addbeh.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 4.Flannery BA, Poole SA, Gallop RJ, Volpicelli JR. Alcohol craving predicts drinking during treatment: an analysis of three assessment instruments. J Stud Alcohol Drugs. 2003;64(1):120–6. doi: 10.15288/jsa.2003.64.120. [DOI] [PubMed] [Google Scholar]
- 5.Flannery BA, Volpicelli JR, Pettinati HM. Psychometric properties of the Penn Alcohol Craving Scale. Alcohol Clin Exper Res. 1999;23(8):1289–95. [PubMed] [Google Scholar]
- 6.Subbaraman MS, Lendle S, van der Laan M, Kaskutas LA, Ahern J. Cravings as a mediator and moderator of drinking outcomes in the COMBINE study. Addiction. 2013;108(10):1737–44. doi: 10.1111/add.12238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Witkiewitz K. Predictors of heavy drinking during and following treatment. Psychol Addict Behav. 2011;25(3):426–38. doi: 10.1037/a0022889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Witkiewitz K. Temptation to drink as a predictor of drinking outcomes following psychosocial treatment for alcohol dependence. Alcohol Clin Exper Res. 2012;37(3):529–37. doi: 10.1111/j.1530-0277.2012.01950.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yoon G, Won Kim S, Thuras P, Grant JE. Alcohol craving in outpatients with alcohol dependence: rate and clinical correlates. J Stud Alcohol. 2006;67:770–7. doi: 10.15288/jsa.2006.67.770. [DOI] [PubMed] [Google Scholar]
- 10.Fazzino TL, Harder VS, Rose GL, Helzer JE. A daily process examination of the bidirectional relationship between craving and alcohol consumption as measured via interactive voice response. Alcohol Clin Exper Res. 2013;37(12):2161–7. doi: 10.1111/acer.12191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moore TM, Seavey A, Ritter K, McNulty JK, Gordon KC, Stuart GL. Ecological momentary assessment of the effects of craving and affect on risk for relapse during substance abuse treatment. Psychol Addict Behav. 2014;28(2):619–24. doi: 10.1037/a0034127. [DOI] [PubMed] [Google Scholar]
- 12.Day AM, Celio MA, Lisman SA, Spear LP. Gender, history of alcohol use, and number of drinks consumed predict craving among drinkers in a field setting. Addict Behav. 2014;39:354–7. doi: 10.1016/j.addbeh.2013.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pasche SC, Garner M, Baldwin DS, Sinclair JMA. “Craving”: exploring the components of the Desires for Alcohol Questionnaire (DAQ) and the relation to the severity of alcohol problems. J Stud Alcohol Drugs. 2013 Nov;74(6):950–5. doi: 10.15288/jsad.2013.74.950. [DOI] [PubMed] [Google Scholar]
- 14.Schlauch RC, Levitt A, Bradizza CM, Stasiewicz PR, Lucke JF, Maisto SA, et al. Alcohol craving in patients diagnosed with a severe mental illness and alcohol use disorder: bidirectional relationships between approach and avoidance inclinations and drinking. J Consult Clin Psychol. 2013 Dec;81(6):1087–99. doi: 10.1037/a0033914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cox WM, Fadardi JS, Klinger E. Motivational processes underlying implicit cognition in addiction. In: Wiers RW, Stacy AW, editors. Handbook of implicit cognition and addiction. Sage; Thousand Oaks, CA: 2006. [Google Scholar]
- 16.Köpetz CE, Lejuez CW, Wiers RW, Kruglanski AW. Motivation and self-regulation in addiction: a call for convergence. Perspectives Psychol Sci. 2013;8(1):3–24. doi: 10.1177/1745691612457575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tiffany ST. A cognitive model of drug urges and drug-use behavior: role of automatic and nonautomatic processes. Psychol Rev. 1990;97(2):147–68. doi: 10.1037/0033-295x.97.2.147. [DOI] [PubMed] [Google Scholar]
- 18.Wiers RW, Bartholow BD, van den Wildenberg E, Thush C, Engels RCME, Sher KJ, et al. Automatic and controlled processes and the development of addictive behaviors in adolescents: a review and a model. Pharmacol Biochem Behav. 2007 Feb;86(2):263–83. doi: 10.1016/j.pbb.2006.09.021. [DOI] [PubMed] [Google Scholar]
- 19.McKee SA, O’Malley SS, Salovey P, Krishnan-Sarin S, Mazure CM. Perceived risks and benefits of smoking cessation: gender-specific predictors of motivation and treatment outcome. Addict Behav. 2005;30:423–35. doi: 10.1016/j.addbeh.2004.05.027. [DOI] [PubMed] [Google Scholar]
- 20.Weinberger AH, Krishnan-Sarin S, Mazure CM, McKee SA. Relationship of perceived risks of smoking cessation to symptoms of withdrawal, craving, and depression during short-term smoking abstinence. Addict Behav. 2008;33:960–3. doi: 10.1016/j.addbeh.2008.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fatseas M, Serre F, Alexandre J, Debrabant R, Auriacombe M, Swndsen J. Craving and substance use among patients with alcohol, tobacco, cannabis or heroin addiction: a comparison of substance- and person-specific cues. Addiction. 2015;110:1035–42. doi: 10.1111/add.12882. [DOI] [PubMed] [Google Scholar]
- 22.Cooney NL, Litt MD, Sevarino KA, Levy L, Kranitz LS, Sackler H, Cooney JL. Concurrent alcohol and tobacco treatment: effect on daily process measures of alcohol relapse risk. J Consult Clin Psychol. 2015;83(2):346–58. doi: 10.1037/a0038633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McCrady BS, Epstein EE, Cook S, Jensen NK, Hildebrandt T. A randomized trial of individual and couple behavioral alcohol treatment for women. J Consult Clin Psychol. 2009;77(2):243–56. doi: 10.1037/a0014686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McCrady BS, Epstein EE, Hirsch LS. Maintaining change after conjoint behavioral alcohol treatment for men: outcomes at 6 months. Addiction. 1999;94(9):1381–96. doi: 10.1046/j.1360-0443.1999.949138110.x. [DOI] [PubMed] [Google Scholar]
- 25.First MB, Gibbon M, Spitzer RL, Williams JBW. User’s guide for the Structured Clinical Interview for DSM–IV axis I disorders - research version. Biometrics Research Department, New York State Psychiatric Institute; New York: 1996. [Google Scholar]
- 26.Derogatis L. SCL-90-R. Administration scoring and procedures manual-II. Clinical Psychometric Research; Towson, MD: 1983. [Google Scholar]
- 27.Folstein MF, Folstein SE, McHugh PR. Mini”-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 28.Robins LN, Wing J, Wittchen HU, Helzer JE, Babor TF, Burke J, et al. The Composite International Diagnostic Interview: an epidemiologic instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Arch Gen Psychiat. 1988;45(12):1069–77. doi: 10.1001/archpsyc.1988.01800360017003. [DOI] [PubMed] [Google Scholar]
- 29.Jahng S, Wood PK, Trull TJ. Analysis of affective instability in ecological momentary assessment: indices using successive difference and group comparison via multilevel modeling. Psychol Meth. 2008;13:354–75. doi: 10.1037/a0014173. [DOI] [PubMed] [Google Scholar]
- 30.Hallgren KA, Crotwell SS, Muñoz RE, Guis BK, McCrady BS, Ladd BO, Epstein EE. Assessing treatment integrity in alcohol behavioral couple therapy. Under review. [DOI] [PMC free article] [PubMed]
- 31.Epstein EE, Labouvie E, McCrady BS, Swingle J, Wern J. Development and validity of drinking pattern classification: binge, episodic, sporadic, and steady drinkers in treatment for alcohol problems. Addict Behav. 2004:1745–61. doi: 10.1016/j.addbeh.2004.03.040. [DOI] [PubMed] [Google Scholar]
- 32.Breslow NE, Clayton DG. Approximate inference in generalized linear mixed models. J Am Stat Assoc. 1993;88(421):9–25. [Google Scholar]
- 33.Diggle PJ, Heagerty P, Liang K, Zeger SL. Analysis of longitudinal data. second Oxford University Press; Oxford, UK: 2013. [Google Scholar]
- 34.Bates D, Mächler M, Bolker BM, Walker SC. Fitting linear mixed-effects models using lme4. 2014 [cited April 21, 2015]. Available from: http://arxiv.org/abs/1406.5823.
- 35.Hallgren KA, Witkiewitz K. Missing data in alcohol clinical trials: a comparison of methods. Alcohol Clin Exper Res. 2013;37(12):2152–60. doi: 10.1111/acer.12205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Merlo J, Chaix B, Ohlsson H, Beckman A, Johnell K, Hjerpe P, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epid Comm Health. 2006;60:290–7. doi: 10.1136/jech.2004.029454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marinchak JS, Morgan TJ. Behavioral treatment techniques for psychoactive substance use disorders. In: Walters ST, Rotgers F, editors. Treating substance abuse: theory and technique. 3rd Guilford; New York: 2012. [Google Scholar]
- 38.Hagger MS, Leaver E, Esser K, Leung C, Te Pas N, Keatley DA, et al. Cue-induced smoking urges deplete cigarette smokers’ self-control resources. Ann Beh Med. 2013;46:394–400. doi: 10.1007/s12160-013-9520-8. (33) [DOI] [PubMed] [Google Scholar]
- 39.Liu X, Li R, Lanza ST, Vasilenko SA, Piper M. Understanding the role of cessation fatigue in the smoking cessation process. Drug Alcohol Depen. 2013;133:548–55. doi: 10.1016/j.drugalcdep.2013.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kavanaugh DJ, Andrade J, May J. Imaginary relish and exquisite torture: the elaborated intrusion theory of desire. Psychol Rev. 2005;112(2):446–67. doi: 10.1037/0033-295X.112.2.446. [DOI] [PubMed] [Google Scholar]
- 41.Dolan SL, Rohsenow DJ, Martin RA, Monti PM. Urge-specific and lifestyle coping strategies of alcoholics: relationships of specific strategies to treatment outcome. Drug Alcohol Depen. 2013;128:8–14. doi: 10.1016/j.drugalcdep.2012.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Unrod M, Drobes DJ, Stasiewicz PR, Ditre JW, Heckman B, Miller RR, et al. Decline in cue-provoked craving during cue exposure therapy for smoking cessation. Nicotine Tobac Res. 2014;16(3):306–15. doi: 10.1093/ntr/ntt145. [DOI] [PMC free article] [PubMed] [Google Scholar]