Abstract
Background
Despite the known benefits of medication therapy for secondary prevention of coronary artery disease (CAD), many patients do not adhere to prescribed medication regimens. Medication nonadherence is associated with poor health outcomes and higher health care cost.
Objective
The purpose of this meta-analysis was to determine the overall effectiveness of interventions designed to improve medication adherence (MA) among adults with CAD. Additionally, sample, study design, and intervention characteristics were explored as potential moderators to intervention effectiveness.
Methods
Comprehensive search strategies facilitated identification of two-group, treatment versus control design studies testing MA interventions among patients with CAD. Data were independently extracted by two trained research specialists. Standardized mean difference effect sizes were calculated for eligible primary studies, adjusted for bias, then synthesized under a random effects model. Homogeneity of variance was explored using a conventional heterogeneity statistic. Exploratory moderator analyses were conducted using meta-analytic analogues for ANOVA and regression for dichotomous and continuous moderators, respectively.
Results
Twenty-four primary studies were included in this meta-analysis. The overall effect size of MA interventions, calculated from 18,839 participants, was 0.229 (p<.001). The most effective interventions utilized nurses as interventionists, initiated interventions in the inpatient setting, and informed providers of patients' medication adherence behaviors. MA interventions tested among older patients were more effective than those among younger patients. Interventions were equally effective regardless of number of intervention sessions, targeting MA behavior alone or with other behaviors, and the use of written instructions only.
Conclusions
Interventions to increase medication adherence among patients with CAD were modestly effective. Nurses can be instrumental in improving MA among these patients. Future research is needed to investigate nurse-delivered MA interventions across varied clinical settings. Additionally, more research testing MA interventions among younger populations and more racially diverse groups is needed.
Keywords: medication adherence, patient compliance, coronary artery disease, meta-analysis
Introduction
Heart disease is the leading cause of death among adults in the United States.1,2 Coronary artery disease (CAD), the most common form of heart disease, is responsible for 385,000 deaths and $108.9 billion in health care expenditures annually.1,2 Secondary prevention for CAD is a multi-intervention approach involving therapeutic lifestyle changes and evidence-based medical therapies, such as prescribed medications. Between 1980 and 2000, these therapies have contributed to a 50% reduction in CAD-related deaths.3 Research suggests the greatest contributor to this reduction is medications for secondary prevention of CAD.3
Unfortunately, medication nonadherence is highly prevalent.4 Approximately one-third of patients who have had a myocardial infarction do not adhere to prescribed medication regimens.5 Nonadherence is associated with increased risk of all-cause and cardiovascular mortality, revascularization procedures, hospitalization, and higher health care cost.6–8 Effective interventions to improve medication adherence (MA) in this population are critically needed.
Efficacy of MA interventions varies.9–14 Few systematic reviews have focused on MA interventions among CAD patients.15–18 Prior reviews have been limited by narrow search strategies, unclear inclusion criteria, lack of a quantitative synthesis, or absent exploration of potential moderating variables.16 To date, no current meta-analyses exist addressing MA intervention effectiveness among patients with CAD. Thus the overall effectiveness of MA interventions in this population is unclear; furthermore, the most effective types of interventions are yet unknown.
A meta-analysis and moderator analysis of MA interventions among CAD patients could promote efficiency in developing future interventions and provide clinicians with guidance to promote MA in clinical practice. The purpose of this systematic review and meta-analysis was to describe and quantify the overall effectiveness of the body of MA intervention research among CAD patients, and to explore potential moderators of intervention effectiveness. Additionally, we identified limitations in the extant research and suggested areas for future study.
The following research questions guided this study:
What is the overall effectiveness of MA interventions on MA outcomes among patients with CAD?
Does intervention effectiveness vary based on intervention, sample, or design characteristics?
Methods
This systematic review and meta-analysis was performed using standard meta-analysis techniques and PRISMA guidelines.19, 20 This project was part of a larger parent study examining MA outcomes of MA interventions across multiple chronic and acute illnesses.
Search Strategies
We consulted an expert health sciences reference librarian to ensure comprehensive search strategies.21 Databases searched included: MEDLINE, PubMED, PsychINFO, CINAHL, EBSCO, PQDT, Cochrane Central Trials Register, Cochrane Database of Systematic Reviews, IndMed, ERIC, International Pharmaceutical Abstracts, EBM Reviews - Database of Abstracts of Reviews of Effects, and Communication and Mass Media. Broad MeSH terms were used including: patient compliance, medication adherence, drugs, prescription drugs, pharmaceutical preparations, generic, dosage, compliant, compliance, adherent, adherence, noncompliant, noncompliance, nonadherent, nonadherence, medication(s), regimen(s), prescription(s), prescribed, drug(s), pill(s), tablet(s), agent(s), improve, promote, enhance, encourage, foster, advocate, influence, incentive, ensure, remind, optimize, increase, impact, prevent, address, decrease. Fifty-seven relevant journals were hand searched, and author searches and ancestry searches of prior reviews' bibliographies were conducted to identify additional potentially eligible studies.
Inclusion Criteria
We included 2-group, treatment versus control comparison studies testing interventions to increase MA in patients ≥18 years old with a diagnosis of CAD, defined by the primary studies. MA interventions are deliberate actions performed or directed by investigators to increase adherence to specified medication regimens. Examples include education, reminders, and special packaging. Studies with varied types of MA measurement (e.g., electronic monitoring devices, pharmacy refills, self-report) were included given the diversity of MA measures in this research area. Eligible studies needed to contain enough data to calculate an effect size (ES). The research team attempted to contact corresponding authors to obtain missing outcome data.
Data Extraction
To extract relevant data from primary studies, a coding strategy was developed from prior research and expert consultations. The codebook was developed through an iterative process and pilot tested. Data extracted included the primary study source, publication date, dissemination type (e.g., journal article, dissertation), presence of funding, participant demographics (e.g., age, gender, ethnicity, comorbidities), research methods, intervention details, and MA outcomes. Multiple descriptors of primary study research methods were coded, such as sample size, randomization, and intention-to-treat analyses. Method of MA measurement and follow-up interval were recorded. Varied intervention characteristics were coded, including content (e.g., problem solving, self-monitoring, goal setting), delivery (e.g., face-to-face, telephone), dose (e.g., length/number of sessions), and setting (e.g., clinic, home).
Included studies were independently coded by two extensively trained research specialists, then compared and discussed until consensus was reached. A doctorally-prepared senior research specialist supervised the coding process to ensure coding integrity, and reviewed all ES data. Questionable items were resolved in team meetings with the study principal investigator.
Data Analysis
All data were analyzed using Comprehensive Meta-Analysis Software.22 Standardized mean difference effect sizes (d, ES) were calculated for each 2-group treatment versus control posttest comparison. The standardized mean difference ES between groups was calculated by dividing the difference between treatment and control group post-intervention means by the pooled standard deviation. Additional ES analyses were conducted within groups by subtracting the outcome scores from the baseline scores and dividing by the baseline standard deviation. ESs were weighted by the inverse of variance to account for sample size and adjust for bias, then synthesized using a random-effects model.23 A random-effects model was chosen a priori given the expected within- and between-study variance across primary studies. Data were examined for possible outliers based on standardized residuals of each primary study's ES. Publication bias was examined by assessing the symmetry of a funnel plot constructed by plotting each primary study's standard error against its ES.23
Homogeneity of variance was tested using a conventional heterogeneity statistic (Q), to quantify observed heterogeneity across studies, and I2, to determine the proportion of observed heterogeneity due to true differences in effects across studies.23 Exploratory moderator analyses were used to examine possible associations between study characteristics and intervention effectiveness. Dichotomous variables were evaluated using subgroup analysis, and continuous variables were evaluated using meta-regression.23
Results
Twenty-four primary reports were eligible for analysis.9–14,24–41 Additional coding information was found in 4 companion reports about the same primary studies.42–45 Three primary study reports contained multiple comparison groups.33,36,37 There were 28 treatment versus control group posttest comparisons, 9 treatment group pretest-posttest comparisons, and 6 control group pretest-posttest comparisons. Few smaller studies with negative findings were included, indicating evidence of publication bias.
Primary Study Characteristics
The primary studies included in this meta-analysis included 24 journal articles, 3 dissertations, and 1 presentation. Six studies were disseminated prior to 2000. Seventeen studies were supported by funding.
Primary study characteristics are presented in Table 1. Samples were majority male. The median of the mean age for participants was 62.9 years. Only 7 studies reported data on ethnicity. Of those, most subjects were Caucasian. Some studies reported additional chronic diseases among their subjects including: hypertension (k=17), undifferentiated diabetes (k=16), hyperlipidemia (k=12), heart failure (k=4), stroke (k=3), lung disease (k=3), renal disease (k=2), osteoarthritis (k=1), asthma (k=1), atrial fibrillation (k=1), nephritic syndrome (k=1), thyroid disorder (k=1), and cerebral vascular disease (k=1).
Table 1. Characteristics of Primary Studies Included in Medication Adherence Meta-analyses.
| Characteristic | k | Min | Q1 | Median | Q3 | Max |
|---|---|---|---|---|---|---|
| Treatment group sample size | 28 | 4 | 18.75 | 86.5 | 246.5 | 3635 |
| Control group sample size | 24 | 5 | 21 | 82 | 562 | 3010 |
| Percentage attrition | 23 | 0 | 0 | 4.545 | 14.646 | 65.282 |
| Percentage female | 23 | 0 | 25 | 40 | 51.05 | 67.4 |
| Percentage underrepresented group subjects | 7 | 7 | 24.1 | 48 | 90.4 | 92.9 |
| Mean age (years) | 21 | 53.7 | 58.4 | 62.9 | 64 | 72.22 |
| Median number of intervention sessions | 17 | 1 | 1 | 2 | 5 | 12 |
| Median duration of interventions (days) | 23 | 1 | 1 | 35 | 126 | 365 |
| Median duration post-intervention for MA outcome data collection (days) | 14 | 12 | 40.25 | 124.5 | 175.5 | 700 |
Note. k=number of comparisons in which characteristic was reported; Q1=first quartile, Q3=third quartile.
Primary studies reported diverse methods. The median number of intervention sessions was two (k=17). The median number of days for MA intervention duration was 35 (k=23). Only one study reported intervention session duration. MA outcome data were collected a median of 124.5 days post-intervention (k=14). Studies reported diverse methods of collecting MA outcomes including pharmacy refill (k=7), self-report (k=18), biological measures (k=2), and pill counts (k=1).
Overall Effects of MA Interventions of MA Outcomes
Overall MA ESs are presented in Table 2. ESs were calculated for 28 treatment vs. control group comparisons containing 18,839 subjects. The overall ES for these comparisons was 0.229 (p<.001), indicating significant improvements in MA outcomes in the treatment over the control group (Figure 1). When the 3 largest sample studies were excluded, the ES for these comparisons demonstrated minimal change (d=0.269, p<.001). ESs were significantly heterogeneous.
Table 2. Overall Effects of Medication Adherence Interventions among Patients with Coronary Artery Disease.
| Comparison | k | d | p (d) | 95% Confidence interval | SE | Q | I2 | p (Q) |
|---|---|---|---|---|---|---|---|---|
| Treatment vs. control groups at post-testa | 28 | 0.229 | <.001 | 0.138, 0.321 | 0.047 | 78.201 | 65.474 | <.001 |
| Treatment vs. control groups at post-testb | 25 | 0.269 | <.001 | 0.135, 0.403 | 0.068 | 65.384 | 63.294 | <.001 |
| Treatment group pre- vs. post-test | 9 | 0.183 | 0.106 | -0.039, 0.405 | 0.113 | 69.462 | 88.483 | <.001 |
| Control group pre- vs. post-test | 6 | -0.014 | 0.887 | -0.208, 0.180 | 0.099 | 11.124 | 55.052 | 0.049 |
Note. k=number of comparisons; d=standardized mean difference effect size; SE=standard error; Q=conventional homogeneity statistic; I2 =proportion of observed variance across effect size due to true differences in effects.
all studies included
three larger sample studies excluded
Figure 1. Forest Plot of Main Effects.
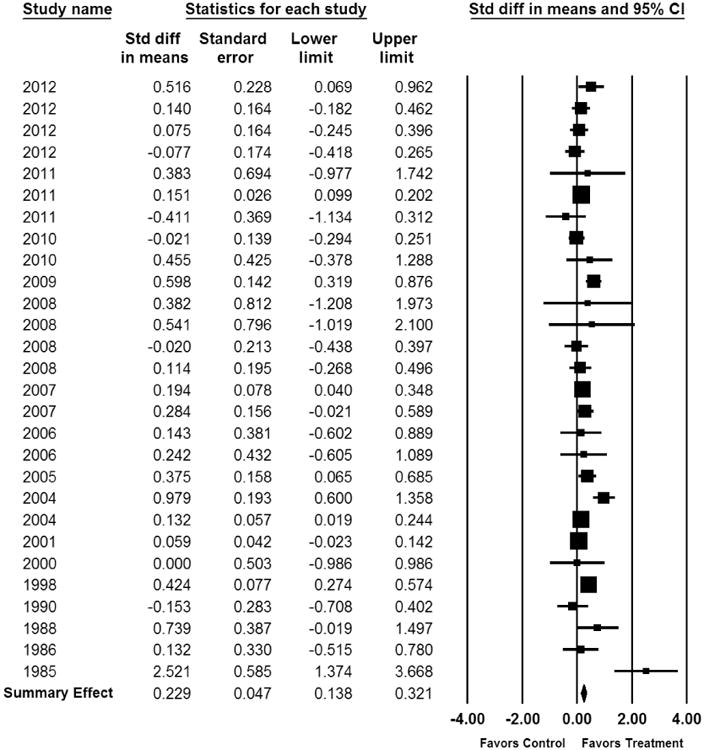
Forest plot of meta-analysis of two-group posttest comparisons of medication adherence outcomes listed by year of publication. Effect sizes calculated using a random effects model. Study weight is proportional to the area of each square.
We also calculated overall ESs for the 9 treatment group pre- vs. post-test comparisons and the 6 for control group pre- vs. post-test comparisons. While the former ES was positive (0.183) and the latter negative (-0.014), neither were statistically significant. Lack of statistical significance may reflect low power from the small number of comparisons.
Moderator Analyses
Continuous and dichotomous moderator analyses are displayed in Tables 3 and 4, respectively. Although all studies from the main analysis were examined for moderating variables, only those moderators reported for a sufficient number of comparisons were included in the analyses.
Table 3. Continuous Moderator Results.
| Moderator | k | B | SE | p |
|---|---|---|---|---|
| Report and Methods Moderators | ||||
| Year of publication | 28 | -0.005 | 0.004 | 0.205 |
| Sample size | 28 | -0.000 | 0.000 | 0.004 |
| Sample Attribute Moderators | ||||
| Age | 21 | 0.014 | 0.004 | 0.001 |
| Percent women | 23 | -0.000 | 0.002 | 0.968 |
| Underrepresented groups | 7 | 0.000 | 0.001 | 0.810 |
| Intervention Feature Moderator | ||||
| Number of sessions | 17 | -0.013 | 0.013 | 0.304 |
| Duration of intervention | 23 | -0.000 | 0.000 | 0.972 |
| Time point for MA outcome data collection | 14 | -0.000 | 0.000 | 0.213 |
Note. k=number of comparisons; B=meta-regression coefficient (unstandardized); SE=standard error; p is value for B
Table 4. Dichotomous Moderator Results.
| Moderator | k | d | SE | QB | p |
|---|---|---|---|---|---|
| Report Moderators | |||||
| Publication status | 1.267 | 0.260 | |||
| Unpublished (e.g. dissertation, presentation) | 4 | 0.724 | 0.474 | ||
| Published article | 24 | 0.189 | 0.037 | ||
| Presence of funding for research | 1.911 | 0.167 | |||
| Unfunded | 11 | 0.452 | 0.192 | ||
| Funded (any funding reported or acknowledged) | 17 | 0.182 | 0.040 | ||
| Socioeconomic status | 0.194 | 0.660 | |||
| Not reported as low income | 24 | 0.237 | 0.046 | ||
| Reported as low income | 4 | 0.352 | 0.259 | ||
| Location | 0.531 | 0.466 | |||
| Not North America | 7 | 0.380 | 0.125 | ||
| North America | 21 | 0.182 | 0.045 | ||
| Research Methods Moderators | |||||
| Allocation to treatment and control groups | 0.200 | 0.655 | |||
| Not random assignment | 8 | 0.199 | 0.068 | ||
| Random assignment | 20 | 0.244 | 0.072 | ||
| Allocation concealment | 1.222 | 0.269 | |||
| Allocation not concealed | 15 | 0.188 | 0.050 | ||
| Allocation concealed | 13 | 0.319 | 0.108 | ||
| Theory | 0.167 | 0.683 | |||
| No theory | 23 | 0.239 | 0.050 | ||
| Any theory | 5 | 0.184 | 0.124 | ||
| Data collectors blinded | 0.481 | 0.488 | |||
| Data collectors not blinded | 18 | 0.207 | 0.052 | ||
| Data collectors blinded | 10 | 0.293 | 0.112 | ||
| Intention-to-treat | 0.000 | 0.997 | |||
| No intention-to-treat | 23 | 0.236 | 0.063 | ||
| Intention-to-treat | 5 | 0.237 | 0.097 | ||
| Intervention Feature Moderators | |||||
| Goal Setting | 0.095 | 0.758 | |||
| No goal setting | 23 | 0.227 | 0.050 | ||
| Goal setting | 5 | 0.183 | 0.135 | ||
| Health care provider given information about MA | 3.899 | 0.048 | |||
| Health care provider NOT given information about MA | 20 | 0.151 | 0.042 | ||
| Health care provider given information about MA | 8 | 0.387 | 0.112 | ||
| Intervention delivered at home | 0.676 | 0.411 | |||
| Not at home | 23 | 0.254 | 0.053 | ||
| At home | 5 | 0.129 | 0.143 | ||
| Intervention delivered at clinic | 0.705 | 0.401 | |||
| Not at clinic | 23 | 0.213 | 0.049 | ||
| At clinic | 5 | 0.320 | 0.118 | ||
| Intervention started while subjects were inpatients | 8.448 | 0.004 | |||
| Not inpatients | 19 | 0.141 | 0.037 | ||
| Inpatients | 9 | 0.590 | 0.150 | ||
| Problem solving | 0.307 | 0.580 | |||
| No problem solving | 22 | 0.245 | 0.054 | ||
| Problem solving | 6 | 0.188 | 0.088 | ||
| Self-monitoring of medications | 1.198 | 0.274 | |||
| No self-monitoring | 25 | 0.195 | 0.045 | ||
| Self-monitoring | 3 | 0.492 | 0.267 | ||
| Succinct written instructions | 1.820 | 0.177 | |||
| No succinct written instructions | 22 | 0.255 | 0.054 | ||
| Succinct written instructions | 6 | 0.124 | 0.080 | ||
| Any written instructions | 2.868 | 0.090 | |||
| No written instructions | 19 | 0.287 | 0.065 | ||
| Any written instructions | 9 | 0.149 | 0.049 | ||
| Behavior target | 1.212 | 0.271 | |||
| Multiple behaviors | 11 | 0.306 | 0.109 | ||
| MA only | 17 | 0.179 | 0.038 | ||
| Part of intervention delivered to providers | 0.476 | 0.490 | |||
| Not delivered to providers | 24 | 0.213 | 0.053 | ||
| Delivered to providers | 4 | 0.311 | 0.131 | ||
| Nurse interventionist | 6.502 | 0.011 | |||
| No nurse | 18 | 0.127 | 0.020 | ||
| Any nurse | 10 | 0.428 | 0.116 | ||
| Physician interventionist | 0.397 | 0.529 | |||
| No physician | 21 | 0.223 | 0.050 | ||
| Physician | 7 | 0.322 | 0.148 | ||
| Pharmacist interventionist | 0.310 | 0.578 | |||
| No pharmacist | 21 | 0.240 | 0.056 | ||
| Pharmacist | 7 | 0.193 | 0.062 | ||
| Mail delivery | 10.845 | 0.001 | |||
| No mail delivery | 23 | 0.292 | 0.059 | ||
| Mail delivery | 5 | 0.060 | 0.038 | ||
| Telephone delivery | 0.701 | 0.403 | |||
| No telephone delivery | 14 | 0.192 | 0.065 | ||
| Telephone delivery | 14 | 0.280 | 0.082 | ||
| Written materials ONLY | 2.985 | 0.084 | |||
| No written intervention | 26 | 0.248 | 0.049 | ||
| Written intervention | 2 | 0.008 | 0.130 | ||
| Face-to-face delivery | 2.604 | 0.107 | |||
| No face-to-face | 7 | 0.143 | 0.048 | ||
| Face-to-face | 21 | 0.288 | 0.076 | ||
Note. k=number of comparisons; d=standardized mean difference effect size; SE=standard error; QB=sum of weighted sum of squares of subgroup means about overall mean; p is value for QB
Intervention Moderators
Studies in which health care providers were given information about subjects' MA revealed a significantly greater ES (0.387) than when the providers were not given information on MA (0.151). An example of this type of intervention component could involve using a questionnaire on participants' baseline MA and barriers to MA.24 Studies with nurse interventionists (0.428) reported significantly higher MA than studies without nurse interventionists (0.127). Studies with and without physician and pharmacist interventionists had similar ESs. Interventions started when participants were inpatients had significantly larger effects (0.590) than interventions that did not start with inpatients (0.141); however, there was little difference when the intervention was delivered at home versus in the clinic. With regards to the mode of intervention delivery, we saw no significant differences among telephone, written materials only, or face-to-face delivery. Interventions using mail delivery were less effective (0.060) than interventions without mail delivery interventions(0.292). There were several nonsignificant variables, including: utilization of theory, number of sessions, duration of intervention, time point for measuring outcome MA, goal setting, interventions delivered at home, interventions delivered in clinic, problem solving, succinct written instructions, any written instructions, behavior target (MA or multiple behaviors), physician or pharmacist interventionists, telephone and face-to-face delivery, and written instructions only.
Report and Sample Moderators
Age of subjects had a significant positive slope (0.014), revealing that MA interventions led to greater adherence improvement in samples of older patients. Interventions were equally effective regardless of publication status, funding, and location. Other nonsignificant moderators included year of publication, percentage of women and underrepresented groups, and socioeconomic status (SES).
Design and Methods Moderators
Although sample size had a statistically significant negative slope, this finding is not clinically substantive. Other potential moderators related to design, such as blinding, allocation concealment, random assignment, and intention-to-treat analyses were not associated with MA effectiveness.
Discussion
Findings from this meta-analysis, the first of its kind, suggest interventions to increase MA among participants with CAD were significantly effective. These positive findings are similar to prior meta-analyses examining MA outcomes from MA interventions among underrepresented groups and from packaging intervention effects.46,47 Although poor MA has been linked to negative health outcomes in patients with CAD,4,6,7 consensus on the how much MA is needed to improve varied CAD-related outcomes is not yet clear. Prior research exists exploring MA and blood pressure outcomes48, 49 and cardiovascular disease risk.49 However, further research is needed to quantify the amount of MA needed to mitigate additional CAD-related outcomes. Moreover, the dose of MA intervention needed to change MA behavior among patients with CAD is yet to be determined. Due to the small number of comparisons employing similar measures of MA, we were unable to convert the ES to a clinical metric of adherence. Future MA intervention research among CAD patients should include explicit information regarding intervention dose.
Moderator findings
We found several interesting moderators. Interventions in which health care providers were given information regarding participants' MA were more effective than interventions without this component. Awareness of patients' MA behavior can motivate and guide providers to address issues related to MA. Clinicians working with patients with CAD should assess issues with or barriers to MA to identify the possible need to intervene. Future research might directly compare an intervention that provides patient MA status to health care providers to a similar intervention without this provision.
MA interventions delivered by nurses were especially effective. Nurses have considerable access to patients with CAD in outpatient settings, such as cardiac rehabilitation and clinics. Additionally, nurses working in the inpatient setting spend approximately 25%-37% of their time providing direct patient care and 11%-21% of their time in medication-related tasks.50,51 In addition to substantial access to this patient population, nurses also have clinical skills to promote MA. For example, nurses have delivered efficacious MA interventions through counseling, 52 follow up communication, 27, 53, 54 and case management.55, 56 Nurses should play an active role in developing and implementing MA interventions among patients with CAD. Research exploring nursing interventions to increase MA among CAD patients could focus on testing or comparing specific intervention strategies such as education, counseling, and managing barriers. Specific nurse type and training were not clearly reported among studies, hindering the comparison of MA intervention effectiveness across different types of nurses. Future studies should explicitly identify types of nurses delivering MA interventions among patients with CAD.
MA interventions initiated in the inpatient setting were more effective. The inpatient setting may provide an opportunity for clinicians to inform patients and families about the importance of medications for secondary prevention of CAD, as well as strategies for MA. Moreover, the dire nature of hospitalization may influence patient and family receptivity to MA interventions. Most MA interventions initiated in the inpatient setting included follow up intervention content post-discharge. Continued reinforcement of MA post-discharge may positively affect MA outcomes. For those patients who may start medications outside of the hospital, interventions delivered at home or in the clinic were equally effective. Future research might directly compare MA interventions initiated in the inpatient setting to MA interventions initiated post hospitalization.
Regarding sample characteristics, only age appeared to impact intervention effectiveness. As the age of the sample increased, so did the intervention effectiveness. These findings support prior research related to statin MA and LDL goal attainment.57,58 Chi and colleagues57 postulated that older individuals are more likely to have multiple comorbidities and may be more attentive to prescribed medication regimens. Additional primary research is needed to identify effective MA interventions among younger populations with CAD. Furthermore, more primary research involving more diverse samples is needed. CAD-related deaths are higher among African-Americans than Caucasians and other groups.2,59 Rates of MA for various chronic diseases also differ across race and ethnicity, with minority groups being less adherent to prescribed medications.60,61 However, few primary studies included in this meta-analysis reported racially or ethnically diverse groups. Thus future primary research testing MA interventions among patients with CAD must strive to include minority groups to reduce this disparity.
We found some interesting nonsignificant moderators. Interventions focusing solely on MA were as effective as interventions that had multiple behavioral foci. Thus clinicians may take the opportunity to introduce strategies for MA while discussing other health behaviors with CAD patients. The use of only written material did not impact intervention effectiveness, suggesting providers should consider using more than this type of delivery when promoting MA among patients with CAD. Future MA intervention research among CAD patients should incorporate additional forms of intervention delivery beyond written materials. Number of intervention sessions did not appear to be a significant moderator. It is possible that even one or two intervention sessions may be effective in changing MA behavior among CAD patients. However, additional research testing or comparing various aspects of intervention dose could help identify the most effective dose needed to change MA behavior. We did not identify any specific intervention strategy that increased MA intervention effectiveness; however, lack of statistical significance of these moderators may be related to the small number of comparisons.
MA interventions delivered by physicians or pharmacists were equally effective as interventions not delivered by these providers. Although these findings suggest involving these providers may not increase MA intervention effectiveness, the number of studies incorporating these types of interventionists was small. Future research could directly compare similar MA interventions among CAD patients delivered by different clinicians. Additional research may also explore variations in MA intervention delivery across diverse health care providers.
This meta-analysis was limited by some primary study characteristics. Although efforts were made to contact corresponding authors, some studies were excluded because critical data were missing from primary study reports. Primary study reporting limits generalizability of this study's findings to more diverse populations. Primary study quality is an important issue in meta-analysis work. Multiple strategies are recommended to manage primary study quality.62,63 We used specific inclusion criteria to capture reports with more rigorous study designs, employed analysis techniques accounting for study heterogeneity, and explored study quality empirically through moderator analyses. Some publication bias was present. Smaller, negative studies are less likely to be published; therefore, access to these studies is limited. Despite extensive search strategies, capturing these relevant studies was a challenge.
Primary study reporting affected the ability to identify effective combinations of MA components. Several studies employed multiple intervention strategies; however, combinations of strategies were inconsistent. Thus determining the most effective combination of MA intervention strategies was not possible.
Measurement error within the primary studies could have introduced bias towards overestimation of MA intervention effects. Objective measures are the most sensitive and specific means of measuring MA;64,65 however, most included studies utilized self-reported MA, which is known to overestimate patients' MA.66 Future MA intervention research conducted among patients with CAD should consider using objective measures of MA to reduce bias.
Meta-analyses are observational studies. The moderator findings of this study are intended to promote additional exploration in this area of study. The scope of this meta-analysis is limited to MA among patients with CAD. Therefore, interpretation of these findings may not be possible among patients with other chronic illnesses or other forms of heart disease.
Conclusion
Medication management is an important aspect of secondary prevention for CAD. Nonadherence to prescribed medications for CAD has been linked with multiple poor outcomes. Findings from this meta-analysis suggest MA interventions among patients with CAD are effective, especially among older patients. Clinicians working with patients with CAD evaluate patients' MA behavior prior to initiating interventions to improve MA. Nurses are on the front lines of health behavior promotion among these patients and can be effective MA interventionists. Future research is needed to explore MA interventions among younger populations and more racially diverse groups.
Acknowledgments
The project described was supported by Award Number R01NR011990 (Conn-PI) from the National Institute of Nursing Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health.
Contributor Information
Jo-Ana D. Chase, Email: chasej@missouri.edu, S343 School of Nursing, University of Missouri, Columbia, MO 65211.
Jennifer L. Bogener, Email: jenniferbogener@gmail.com, University of Missouri, School of Nursing, School of Health Professions, 100 E. Green Meadows Rd. Ste. 10, Columbia, MO 65203.
Todd M. Ruppar, Email: RupparT@missouri.edu, S423 School of Nursing, University of Missouri, Columbia, MO 65211.
Vicki S. Conn, Email: conn@missouri.edu, S317 School of Nursing, University of Missouri, Columbia, MO 65211.
References
- 1.Centers for Disease Control and Prevention. Heart Disease Facts. 2014 http://www.cdc.gov/heartdisease/facts.htm.
- 2.National Heart Lung, and Blood Institute. Morbidity and Mortality: 2012 Chart Book on Cardiovascular, Lung, and Blood Diseases. National Institutes of Health; 2012. [Google Scholar]
- 3.Ford ES, Ajani UA, Croft JB, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980-2000. N Engl J Med. 2007;356(23):2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 4.Ho PM, Bryson CL, Rumsfeld JS. Medication adherence its importance in cardiovascular outcomes. Circulation. 2009;119(23):3028–3035. doi: 10.1161/CIRCULATIONAHA.108.768986. [DOI] [PubMed] [Google Scholar]
- 5.Naderi SH, Bestwick JP, Wald DS. Adherence to drugs that prevent cardiovascular disease: meta-analysis on 376,162 patients. Am J Med. 2012;125(9):882–887.e1. doi: 10.1016/j.amjmed.2011.12.013. [DOI] [PubMed] [Google Scholar]
- 6.Chowdhury R, Khan H, Heydon E, et al. Adherence to cardiovascular therapy: a meta-analysis of prevalence and clinical consequences. Eur Heart J. 2013;34(38):2940–2948. doi: 10.1093/eurheartj/eht295. [DOI] [PubMed] [Google Scholar]
- 7.Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43(6):521–530. doi: 10.1097/01.mlr.0000163641.86870.af. [DOI] [PubMed] [Google Scholar]
- 8.Ho PM, Magid DJ, Shetterly SM, et al. Medication nonadherence is associated with a broad range of adverse outcomes in patients with coronary artery disease. Am Heart J. 2008;155(4):772–779. doi: 10.1016/j.ahj.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 9.Kelly JM. Sublingual nitroglycerin: improving patient compliance with a demonstration dose. J Am Board Fam Pract Am Board Fam Pract. 1988;1(4):251–254. [PubMed] [Google Scholar]
- 10.Nicoleau CM. Evaluation of a comprehensive cardiac rehabilitation program. 1985 [Google Scholar]
- 11.Zhao Y. [Accessed June 11, 2014];Effects of a discharge planning intervention for elderly patients with coronary heart disease in Tianjin, China: A randomized controlled trial. 2004 http://search.proquest.com.proxy.mul.missouri.edu/pqdt/docview/305041963/abstract/CE2FD56D4F7B49F2PQ/1?accountid=14576.
- 12.Costa e Silva R, Pellanda L, Portal V, Maciel P, Furquim A, Schaan B. Transdisciplinary approach to the follow-up of patients after myocardial infarction. Clin Sao Paulo Braz. 2008;63(4):489–496. doi: 10.1590/S1807-59322008000400013. doi:S1807-59322008000400013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lourenco L, Rodrigues RCM, Gallani CB, Spana TM. Effectiveness of the combination of planning strategies in adhering to the drug therapy and health related quality of life among coronary heart disease outpatients. Montreal, Canada: 2011. [Google Scholar]
- 14.Miller P, Wikoff R, Garrett MJ, McMahon M, Smith T. Regimen compliance two years after myocardial infarction. Nurs Res. 1990;39(6):333–336. [PubMed] [Google Scholar]
- 15.Ara S. A literature review of cardiovascular disease management programs in managed care populations. J Manag Care Pharm JMCP. 2004;10(4):326–344. doi: 10.18553/jmcp.2004.10.4.326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cutrona SL, Choudhry NK, Fischer MA, et al. Targeting cardiovascular medication adherence interventions. J Am Pharm Assoc JAPhA. 2012;52(3):381–397. doi: 10.1331/JAPhA.2012.10211. [DOI] [PubMed] [Google Scholar]
- 17.Maddox TM, Ho PM. Medication adherence and the patient with coronary artery disease: challenges for the practitioner. Curr Opin Cardiol. 2009;24(5):468–472. doi: 10.1097/HCO.0b013e32832ed62d. [DOI] [PubMed] [Google Scholar]
- 18.Schadewaldt V, Schultz T. Nurse-led clinics as an effective service for cardiac patients: results from a systematic review. Int J Evid Based Healthc. 2011;9(3):199–214. doi: 10.1111/j.1744-1609.2011.00217.x. [DOI] [PubMed] [Google Scholar]
- 19.Cooper H, Hedges LV, Valentine JC, editors. The Handbook of Research Synthesis and Meta-Analysis. 2nd. Russell Sage Foundation; 2009. [Google Scholar]
- 20.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reed JG, Baxter PM. The Handbook of Research Synthesis and Meta-Analysis. 2nd. Russell Sage Foundation; 2009. Using reference databases; pp. 73–101. [Google Scholar]
- 22.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Comprehensive Meta-Analysis. Englewood, NJ: Biostat; 2005. [Google Scholar]
- 23.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to Meta-Analysis. 1st. Wiley; 2009. [Google Scholar]
- 24.Calvert SB, Kramer JM, Anstrom KJ, Kaltenbach LA, Stafford JA, Allen LaPointe NM. Patient-focused intervention to improve long-term adherence to evidence-based medications: A randomized trial. Am Heart J. 2012;163(4):657–665. doi: 10.1016/j.ahj.2012.01.019. [DOI] [PubMed] [Google Scholar]
- 25.Campbell N, Ritchie L, Thain J, Deans H, Rawles J, Squair J. Secondary prevention in coronary heart disease: a randomised trial of nurse led clinics in primary care. Heart. 1998;80(5):447–452. doi: 10.1136/hrt.80.5.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Choudhry NK, Avorn J, Glynn RJ, et al. Full coverage for preventive medications after myocardial infarction. N Engl J Med. 2011;365(22):2088–2097. doi: 10.1056/NEJMsa1107913. [DOI] [PubMed] [Google Scholar]
- 27.Edworthy SM, Baptie B, Galvin D, et al. Effects of an enhanced secondary prevention program for patients with heart disease: a prospective randomized trial. Can J Cardiol. 2007;23(13):1066–1072. doi: 10.1016/s0828-282x(07)70875-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Faulkner MA, Wadibia EC, Lucas BD, Hilleman DE. Impact of pharmacy counseling on compliance and effectiveness of combination lipid-lowering therapy in patients undergoing coronary artery revascularization: A randomized, controlled trial. Pharmacotherapy. 2000;20:410–416. doi: 10.1592/phco.20.5.410.35048. [DOI] [PubMed] [Google Scholar]
- 29.Gould KA. A randomized controlled trial of a discharge nursing intervention to promote self-regulation of care for early discharge interventional cardiology patients. Dimens Crit Care Nurs. 2011;30(2):117–125. doi: 10.1097/DCC.0b013e3182052324. [DOI] [PubMed] [Google Scholar]
- 30.Guthrie RM. The effects of postal and telephone reminders on compliance with pravastatin therapy in a national registry: Results of the first myocardial infarction risk reduction program. Clin Ther. 2001;23(6):970–980. doi: 10.1016/s0149-2918(01)80084-9. [DOI] [PubMed] [Google Scholar]
- 31.Jiang X, Sit JW, Wong TK. A nurse-led cardiac rehabilitation programme improves health behaviours and cardiac physiological risk parameters: Evidence from Chengdu, China. J Clin Nurs. 2007;16(10):1886–1897. doi: 10.1111/j.1365-2702.2007.01838.x. [DOI] [PubMed] [Google Scholar]
- 32.Kotowycz MA, Cosman TL, Tartaglia C, Afzal R, Natarajan MK, et al. Safety and feasibility of early hospital discharge in ST-segment elevation myocardial infarction-A prospective and randomized trial in low-risk primary percutaneous coronary intervention patients (the Safe-Depart Trial) Am Heart J. 2010;159(1):117. doi: 10.1016/j.ahj.2009.10.024. [DOI] [PubMed] [Google Scholar]
- 33.Kripalani S, Schmotzer B, Jacobson TA. Improving medication adherence through graphically enhanced interventions in coronary heart disease (IMAGE-CHD): A randomized controlled trial. J Gen Intern Med. 2012:1–9. doi: 10.1007/s11606-012-2136-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lehr BK. A comparative study of self-management and cognitive-behavioral therapies in the treatment of cardiac rehabilitation patients. 1987 [Google Scholar]
- 35.Muñiz J, Gómez-Doblas JJ, Santiago-Pérez MI, et al. The effect of post-discharge educational intervention on patients in achieving objectives in modifiable risk factors six months after discharge following an episode of acute coronary syndrome, (CAM-2 Project): A randomized controlled trial. Health Qual Life Outcomes. 2010;8 doi: 10.1186/1477-7525-8-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Polack J, Jorgenson D, Robertson P. Evaluation of different methods of providing medication-related education to patients following myocardial infarction. Can Pharm J. 2008;141(4):241–247. [Google Scholar]
- 37.Shemesh E, Koren-Michowitz M, Yehuda R, et al. Symptoms of posttraumatic stress disorder in patients who have had a myocardial infarction. J Consult Liaison Psychiatry. 2006;47(3):231–239. doi: 10.1176/appi.psy.47.3.231. [DOI] [PubMed] [Google Scholar]
- 38.Sherrard H, Struthers C, Kearns SA, Wells G, Mesana T. Using technology to create a medication safety net for cardiac surgery patients: A nurse-led randomized control trial. Can J Cardiovasc Nurs. 2009;19(3):9–15. [PubMed] [Google Scholar]
- 39.Smith DH, Kramer JM, Perrin N, et al. A randomized trial of direct-to-patient communication to enhance adherence to beta-blocker therapy following myocardial infarction. Arch Intern Med. 2008;168(5):477–483. doi: 10.1001/archinternmed.2007.132. [DOI] [PubMed] [Google Scholar]
- 40.Yilmaz MB, Pinar M, Naharci I, et al. Being well-informed about statin is associated with continuous adherence and reaching targets. Cardiovasc Drugs Ther. 2005;19(6):437–440. doi: 10.1007/s10557-005-5202-5. [DOI] [PubMed] [Google Scholar]
- 41.Zuckerman IH, Weiss SR, McNally D, Layne B, Mullins CD, Wang J. Impact of an educational intervention for secondary prevention of myocardial infarction on Medicaid drug use and cost. Am J Manag Care. 2004;10(7 Part 2):493–500. [PubMed] [Google Scholar]
- 42.Miller P, Wikoff R, McMahon M, Garrett MJ, Ringel K. Influence of a nursing intervention on regimen adherence and societal adjustments postmyocardial infarction. Nurs Res. 1988;37(5):297–302. [PubMed] [Google Scholar]
- 43.Miller P, Wikoff R, McMahon M, et al. Personal adjustments and regimen compliance 1 year after myocardial infarction. Heart Lung. 1989;18(4):339–346. [PubMed] [Google Scholar]
- 44.Choudhry NK, Brennan T, Toscano M, et al. Rationale and design of the Post-MI FREEE trial: a randomized evaluation of first-dollar drug coverage for post-myocardial infarction secondary preventive therapies. Am Heart J. 2008;156(1):31–36. doi: 10.1016/j.ahj.2008.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gould KA. A randomized controlled trial of a discharge nursing intervention to promote self-regulation of care for early discharge interventional cardiology patients. 2009:250. doi: 10.1097/DCC.0b013e3182052324. Ph.D. [DOI] [PubMed] [Google Scholar]
- 46.Conn VS, Enriquez M, Ruppar TM, Chan KC. Cultural relevance in medication adherence interventions with underrepresented adults: systematic review and meta-analysis of outcomes. doi: 10.1016/j.ypmed.2014.10.021. under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Conn V. Packaging interventions to increase medication adherence: systematic review and meta-analysis. doi: 10.1185/03007995.2014.978939. under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Burnier M, Schneider MP, Chioléro A, Stubi CL, Brunner HR. Electronic compliance monitoring in resistant hypertension: the basis for rational therapeutic decisions. J Hypertens. 2001;19(2):335–341. doi: 10.1097/00004872-200102000-00022. [DOI] [PubMed] [Google Scholar]
- 49.Lowy A, Munk VC, Ong SH, et al. Effects on blood pressure and cardiovascular risk of variations in patients' adherence to prescribed antihypertensive drugs: role of duration of drug action. Int J Clin Pract. 2011;65(1):41–53. doi: 10.1111/j.1742-1241.2010.02569.x. [DOI] [PubMed] [Google Scholar]
- 50.Westbrook JI, Duffield C, Li L, Creswick NJ. How much time do nurses have for patients? A longitudinal study quantifying hospital nurses' patterns of task time distribution and interactions with health professionals. BMC Health Serv Res. 2011;11:319. doi: 10.1186/1472-6963-11-319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jones M, Johnston D. Understanding phenomena in the real world: the case for real time data collection in health services research. J Health Serv Res Policy. 2011;16(3):172–176. doi: 10.1258/jhsrp.2010.010016. [DOI] [PubMed] [Google Scholar]
- 52.Krantz MJ, Havranek EP, Haynes DK, Smith I, Bucher-Bartelson B, Long CS. Inpatient initiation of beta-blockade plus nurse management in vulnerable heart failure patients: a randomized study. J Card Fail. 2008;14(4):303–309. doi: 10.1016/j.cardfail.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 53.Kirscht JP, Kirscht JL, Rosenstock IM. A test of interventions to increase adherence to hypertensive medical regimens. Health Educ Q. 1981;8(3):261–272. doi: 10.1177/109019818100800303. [DOI] [PubMed] [Google Scholar]
- 54.Piette JD, Weinberger M, McPhee SJ, Mah CA, Kraemer FB, Crapo LM. Do automated calls with nurse follow-up improve self-care and glycemic control among vulnerable patients with diabetes? Am J Med. 2000;108(1):20–27. doi: 10.1016/s0002-9343(99)00298-3. [DOI] [PubMed] [Google Scholar]
- 55.Logan AG, Milne BJ, Achber C, Campbell WP, Haynes RB. Work-site treatment of hypertension by specially trained nurses. A controlled trial. Lancet. 1979;2(8153):1175–1178. doi: 10.1016/s0140-6736(79)92397-3. [DOI] [PubMed] [Google Scholar]
- 56.Rudd P, Miller NH, Kaufman J, et al. Nurse management for hypertension. A systems approach. Am J Hypertens. 2004;17(10):921–927. doi: 10.1016/j.amjhyper.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 57.Chi MD, Vansomphone SS, Liu ILA, et al. Adherence to statins and LDL-cholesterol goal attainment. Am J Manag Care. 2014;20(4):e105–e112. [PubMed] [Google Scholar]
- 58.Nag SS, Daniel GW, Bullano MF, et al. LDL-C goal attainment among patients newly diagnosed with coronary heart disease or diabetes in a commercial HMO. J Manag Care Pharm JMCP. 2007;13(8):652–663. doi: 10.18553/jmcp.2007.13.8.652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. [Accessed June 6, 2014];Coronary Heart Disease and Stroke Deaths --- United States. 2006 http://www.cdc.gov/mmwr/preview/mmwrhtml/su6001a13.htm. [PubMed]
- 60.Gerber BS, Cho YI, Arozullah AM, Lee SYD. Racial differences in medication adherence: A cross-sectional study of Medicare enrollees. Am J Geriatr Pharmacother. 2010;8(2):136–145. doi: 10.1016/j.amjopharm.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rolnick SJ, Pawloski PA, Hedblom BD, Asche SE, Bruzek RJ. Patient characteristics associated with medication adherence. Clin Med Res. 2013;11(2):54–65. doi: 10.3121/cmr.2013.1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Valentine JC. Judging the quality of primary research. In: Cooper HM, Hedges LV, Valentine JC, editors. The Handbook of Research Synthesis and Meta-Analysis. 2nd. Russell Sage Foundation; 2009. pp. 122–146. [Google Scholar]
- 63.Conn VS, Rantz MJ. Research methods: managing primary study quality in meta-analyses. Res Nurs Health. 2003;26(4):322–333. doi: 10.1002/nur.10092. [DOI] [PubMed] [Google Scholar]
- 64.Dunbar-Jacob J, Sereika SM, Houze M, Luyster FS, Callan JA. Accuracy of Measures of Medication Adherence in a Cholesterol-Lowering Regimen. West J Nurs Res. 2012;34(5):578–597. doi: 10.1177/0193945912439251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hansen RA, Kim MM, Song L, Tu W, Wu J, Murray MD. Comparison of methods to assess medication adherence and classify nonadherence. Ann Pharmacother. 2009;43(3):413–422. doi: 10.1345/aph.1L496. [DOI] [PubMed] [Google Scholar]
- 66.Zeller A, Ramseier E, Teagtmeyer A, Battegay E. Patients' Self-Reported Adherence to Cardiovascular Medication Using Electronic Monitors as Comparators. Hypertens Res. 2008;31(11):2037–2043. doi: 10.1291/hypres.31.2037. [DOI] [PubMed] [Google Scholar]


