Abstract
Alzheimer disease (AD) primarily affects older adults. This neurodegenerative disorder is the most common cause of dementia and is a leading source of their morbidity and mortality. Patient care costs in the United States are about 200 billion dollars and will more than double by 2040. This case report describes the remarkable improvement in a patient with advanced AD in hospice who received 5 computed tomography scans of the brain, about 40 mGy each, over a period of 3 months. The mechanism appears to be radiation-induced upregulation of the patient’s adaptive protection systems against AD, which partially restored cognition, memory, speech, movement, and appetite.
Keywords: Alzheimer disease, CT scan, adaptive protection systems, ionizing radiation
Introduction
Alzheimer disease (AD) is a neurodegenerative disorder of uncertain cause and pathogenesis which primarily affects older adults. It accounts for more than 50% of the cases of dementia and is one of the leading sources of morbidity and mortality in the aging population. The most essential and often earliest clinical manifestation of AD is selective memory impairment. While treatments are available that can ameliorate some symptoms of the illness, there is no cure or disease-modifying therapy currently available, and the disease inevitably progresses in all patients. The incidence and prevalence of AD increase exponentially with age, essentially doubling in prevalence every 5 years after the age of 65 years.1 There are rare inherited forms of AD (less than 1% of all cases) that present before 65 years of age.2
In the United States, in 2012, an estimated 5.2 million people older than 65 years had AD. This figure is projected to rise to 13.8 million by 2050. In a Medicare survey of 22 896 adults aged 65 and older, 15 diseases accounted for 70% of all deaths. Dementia was second to heart failure as a cause of mortality, accounting for 19% of deaths.3 While individuals do not die of AD per se, advanced AD increases vulnerability for other disorders, commonly infections, which ultimately lead to their death.4 Costs attributable to the care of these people range between 157 and 215 billion dollars and are expected to more than double by 2040.5
In patients with the typical form of the illness, deficits in other cognitive domains may appear with or after the development of memory impairment. Executive dysfunction and visuospatial impairment are often present relatively early, while deficits in language and behavioral symptoms often manifest later. These deficits develop and progress insidiously.1 Dyspraxia, or difficulty performing learned motor tasks, usually occurs later in the disease. It leads to progressive difficulty first with complex, multistep motor activities; then dressing; using utensils to eat; and other self-care tasks. This is a big contributor to dependency in mid to late stages of AD. Other signs and symptoms are decreased sense of smell, sleep disturbances, seizures,6 and motor signs. There can be a variety of atypical presentations and mixed dementias, that is, AD coexisting with other processes, including vascular dementia and Parkinson disease.
Alzheimer disease progresses inexorably. An older age of onset of AD (>80 years) may be associated with a slower rate of decline compared to younger patients. The survival after diagnosis ranges from 3 to 20 years, with an average life expectancy of 8 to 10 years. The mainstay of management is still symptomatic: treatment of behavioral disturbances, environmental manipulations to support function, and counseling with respect to safety issues.7 Patients generally succumb to terminal-stage complications, such as dehydration, malnutrition, and infection. Patients with advanced AD are admitted to hospice for palliative care as their end-of-life approaches.5
The changes in the brain of patients with AD are associated with diffuse and neuritic plaques, marked by amyloid β (Aβ) deposition and tangles, which are comprised of the accumulation of hyperphosphorylated tau protein. The study of AD is being transformed by the availability of new biomarker technologies to measure such changes. Large clinical trials are evaluating anti-amyloid and other therapies, utilizing imaging or cerebrospinal fluid biomarkers. While the pathogenesis of AD remains unclear, all forms of AD appear associated with overproduction and/or decreased clearance of Aβ peptides.4 Autopsy data suggest that symptomatic AD will not occur in every patient with amyloid in the brain.1
The study of AD has focused on 3 interrelated hypotheses4:
Amyloid plaques are a unique genetic and lifestyle disease due to increased production of Aβ 42 in younger, genetically high-risk individuals and reduced metabolism and removal among older individuals.
Vascular disease is an independent determinant of vascular dementia but also of increased amyloid deposition and neurodegeneration.
Dementia is primarily due to aging and neurodegeneration, independent of amyloid and vascular disease.
Structural brain imaging with computed tomography (CT) and magnetic resonance imaging (MRI) is indicated in the evaluation of patients with suspected AD. It can suggest potential alternative or additional diagnoses. Findings in AD include both generalized and focal atrophy as well as white matter lesions. The most characteristic focal finding in AD is reduced hippocampal volume or medial temporal lobe atrophy. Because hippocampal volumes decline in normal aging, age-specific criteria are needed. Functional brain imaging with fluorodeoxyglucose positron emission tomography (FDG-PET), functional MRI, perfusion MRI, or single-photon emission computed tomography (SPECT) reveals distinct regions of low metabolism (PET) and hypoperfusion in AD. Both FDG-PET and SPECT are the only functional neuroimaging methods that are currently reasonably widely available for clinical use. FDG-PET may be most useful in distinguishing AD from other diseases. A 2013 consensus opinion concluded that amyloid imaging is not appropriate in patients who meet the core clinical criteria for probable AD and have a typical age of onset, and such a scan should not be used to determine dementia severity.1,4,8
The process of AD begins well before clinical symptoms arise, and this period may be the optimal time to intervene if disease-modifying therapies can be identified. Laboratory and imaging biomarkers are increasingly used in research settings to better define prodromal and preclinical forms of AD and identify candidates for early-intervention clinical trials.
Case Report: Partial Recovery of a Patient From Advanced AD After CT Scans to the Brain
The patient is 81 years of age. She began to exhibit symptoms of dementia about 10 years ago, when her illness was diagnosed as the onset of AD. Her disease had progressed gradually to the final stages of advanced AD. The patient had been in hospice care for several months, since April 8, 2015. Hospice care is allowed only if life expectancy is less than 6 months. A neuropsychologist examined her on May 21 and found her to be completely nonresponsive. The patient would frequently refuse her medications and was almost totally noncommunicative. She would only rarely utter a single word and that word would not be appropriate. She was almost immobile; she had not attempted to rise from her wheelchair in months.
Her spouse was aware that low doses of ionizing radiation generally stimulate a patient’s protection systems against diseases and age-related deterioration.9 He requested her physician to prescribe a standard CT scan to determine any anatomical changes that have occurred and to stimulate neuroprotective systems. Two scans were carried out on July 23, 2015. Two days later, her caregiver, who was unaware of this radiation treatment, reported a noticeable improvement. The caregiver was quoted as saying “She is doing so well that it is amazing. I have never seen someone improve this much. She wanted to get up and walk. She was talking some, with more sense, and she was feeding herself again.”
On August 6, another CT scan was provided. On August 11, the following recording on the spouse’s cell phone was made by the daughter of the patient’s best friend in the memory care unit. “I just wanted to just tell you how beautiful the last couple of days have been when I visited and (she) was so interactive. Oh my goodness! I don’t know what the last few days have been, but, and even today, she was like super relaxed. I don’t know if it was the non-full moon or what. Anyway, I just wanted to say how nice it was to see your wife doing so good.”
On August 12, the patient’s spouse received the following e-mail from the patient’s caregiver:
Hi …, I have noticed that … has been much more talkative lately. She really wasn’t talking much at all. She will read words in books, ask questions, ask who people are. She seems to be much more aware of her surroundings. At times she tries to push herself up from her wheelchair thinking that there is something she needs to be doing. She is eating by herself and eating all of her food. Her mood is very good. She is not as tired as she had been during the times I am there.
Another CT scan was administered on August 20, and patient’s condition continued to improve. During the week of September 14, the following behaviors were observed:
A sign of old memory return was seen when she called her daughter’s old roommate by name and then said “roommate.”
An improvement in motor function was seen when, in an exercise group, the patient lifted her leg and did several head turns in phase with the group.
The patient often talked in 3- to 5-word sentences as well as shorter responses, such as “yes, no, maybe, and so on” Whatever her verbal response, it almost always seemed appropriate.
The patient’s improvement following these CT scans was being noticed by all of her rotating caregivers, by her 2 personal caregivers, by all family members, and by visiting friends. Slow but steady improvement continued for about another 3½ weeks.
An additional CT scan was given on October 1. Almost immediately, a significant setback was observed with an estimated loss of about 80% of the gain. This was very discouraging initially, but a slow recovery of cognitive ability began again. A neuropsychologist examined the patient on October 28 and indicated that she was able to give some simple verbal responses, which reflected some minimal improvement from the May 21 examination by the same doctor.
The patient’s slow progress continued until November 20, when she was judged to be no longer eligible for the hospice care that had begun on April 8. It was to last only 6 months. Withdrawal of hospice care was another indicator of the cognitive and physical improvement. She is judged improved enough to be readmitted to a stimulating, dementia day care program that she had been discharged from 18 months ago.
To understand the reason for the patient’s setback after the last CT scan, the patient’s spouse asked the hospital to provide the X-ray doses that had been given during the 4 visits. The doses, CTDIvol, are measured in a plastic patient model and used as a reference for patient dose. They are the doses, in mGy, that were output by the scanner. The values reported are:
| Date (2015): | July 23 | August 06 | August 20 | October 01 |
| Dose (CTDIvol): | 82.34 (39.49 + 42.85) | 38.74 | 46.94 | 38.54 |
Note that 2 CT scans were given on July 23 in order to obtain a satisfactory image of the brain. So the patient actually received a total of 5 scans. Each scan delivered a dose of about 40 mGy. The images were not assessed after each CT scan to measure any change in the amount of amyloid plaque present.
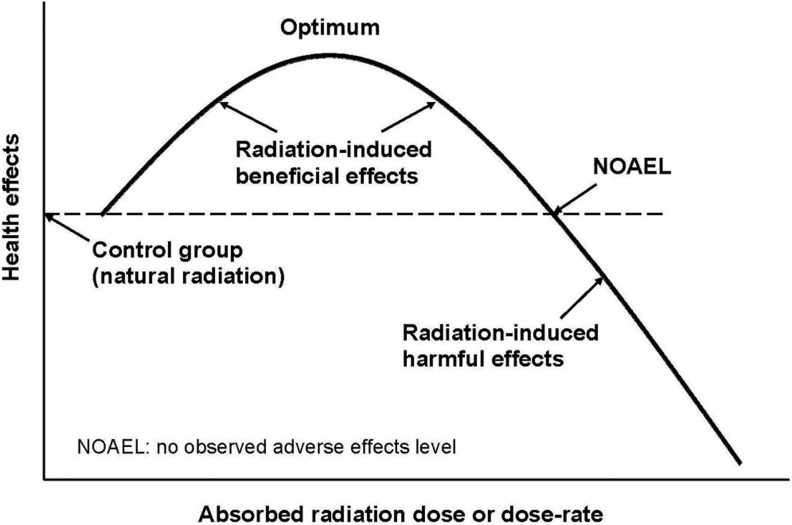
Referring to Figure 1, the observed positive responses of the patient suggest that the cumulative dose of the first 4 radiation exposures, a total of 168 mGy, was in the range of increasing radiation-induced beneficial health effects. The fifth exposure brought the cumulative dose beyond the optimum level and caused a significant decrease in the cognitive and mobility benefit.
Figure 1.
Dose–response model for ionizing radiation.
However, as of January 30, 2016, the patient has recovered beyond her late August condition, and she continues to improve.
Beneficial Effects of Ionizing Radiation
Beneficial effects of ionizing radiation were identified by medical scientists and practitioners very soon after the discoveries of X-rays and radioactivity about 120 years ago. They initially employed radiation to diagnose fractures and other medical conditions but quickly discovered that large exposures were harmful. However, low exposures produced remarkably positive effects. Murphy and Morton observed in 1915 that a low radiation dose, to the entire bodies of mice, increased the activities of their protective processes against the overproduction of lymphocytes, significantly preventing or impairing tumor growth.10 Many important applications of radiation, other than curing cancer were identified in the early 1900s. Many thousands of patients were treated with low radiation with no apparent increases in the incidence of cancer or genetic effects, long after these radiation treatments. The applications include healing of wounds and the cure of a wide variety of infections, such as gas gangrene, carbuncles and boils, sinus infections, inner ear infections, pneumonia, and treatments of arthritis and a multitude of other inflammatory conditions.11,12,13 A very recent article describes the treatment and cure of bronchial asthma.14 An assessment of animal model studies on the capacity of long-term, whole-body γ rays to affect life span concluded that low dose rates enhance longevity; the median life span of a population is usually increased by 10% to 30% but not the maximum life span potential.15 The mechanism for beneficial health effects of radiation is upregulation of an organism’s adaptive protection systems by multiple or chronic low-dose exposures.16,17
How much harm does a low radiation dose cause? The spontaneous rate of DNA damage is enormous.18 The average number of endogenous DNA alterations per average cell (note 1), per day, is about a million. About 10−1 are double-strand breaks (DSBs). The main cause of this damage is metabolic reactive oxygen species. Surprisingly, the rate of DNA damage caused by a low level of ionizing radiation is relatively negligible. A background radiation level of 1 mGy (note 2) per year induces about 10−2 DNA alterations per cell, per day. About 10−4 DNA alterations per cell, per day are DSBs. The endogenous DNA damage rate is about 100 million times the rate from background radiation. The DSB rate is about 1000 times the DSB rate from 1 mGy per year.19
The protection systems prevent, repair, remove, and replace cell and tissue damage, regardless of whether the damage was caused by endogenous metabolic processes or by toxic damage by all of the exogenous causes, including radiation. These systems, which include the immune system, act to restore and maintain all biological functions necessary for survival in good health. All organisms adapt to their environments, so when a small increase in the ambient radiation level occurs, the protection systems adjust to this additional stress by becoming upregulated, that is, by increasing their levels of activity.
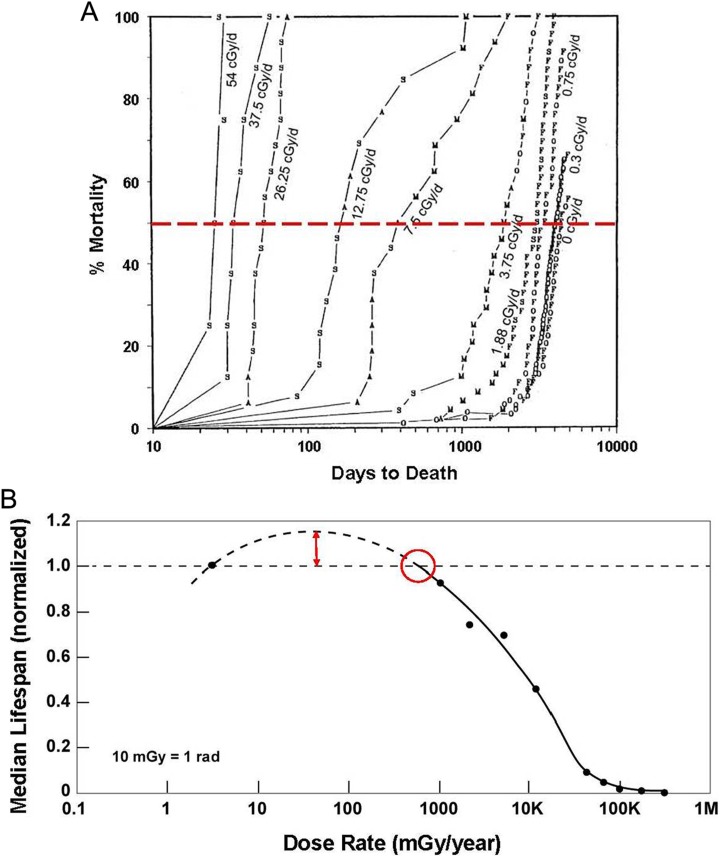
The observed results are net beneficial health effects, including increased life span,15,20,10,21 as shown in Figure 2A and B. On the other hand, a very high, acute exposure causes tissue damage by cell killing as in radiation therapy of tumors. A high dose rate over a long period of time is harmful because it inhibits the protection systems and may damage them. Figure 1 illustrates the dose–response behavior of this phenomenon. There is a threshold dose or dose rate above which a beneficial health effect is observed.23 This observed health effect transitions from beneficial to harmful above the no observed adverse effects level (NOAEL). The dose locations of the threshold, NOAEL, and the amount of benefit or harm for a particular radiation-induced health effect at a given dose depend on the patient’s genetic characteristics, age, and medical condition. This applies not only to ionizing radiations but also to any physical or chemical stressor.
Figure 2.
A, Mortality curves for groups of dogs in different Co60 radiation levels.22 Note that the intersection of the red dashed line (at 50% mortality) with each mortality curve defines the median life span of the group of dogs in the indicated radiation level. B, Median life span versus radiation level.12 Note that the no observed adverse effects level (NOAEL) for γ-radiation-induced life span reduction in dogs is about 700 mGy/year (70 cGy/year).
For a patient’s static defences to act, stresses need to exceed threshold levels to disturb cell and/or tissue functions. The metabolic or dynamic defences include (1) fast-acting ones that start immediately after an injury occurs (DNA repair alone involves more than 150 genes) and (2) delayed defences that arise by upregulation of defense mechanisms leading to adapt the system to repetitive stress for a prolonged period of time. Such adaptive protection may follow also repeated short-term stresses and serve the integrity of the system even for life. Adaptive protections are stimulated maximally by an acute exposure to about 150 mGy.
Low-dose-induced adaptive protections may operate not only against damage from renewed irradiation but also against damage from toxic impacts from nonradiation sources.16,17 Adaptive protections may include reduced damage causation, increased damage repair, and damage removal, for instance, by immune responses against cancer cells, bringing a lifelong benefit. One may speculate that also damage accumulation of β amyloid through glial cells may be prevented, interrupted, or eliminated following exposure to such low doses at which adaptive protections operate at their best.
Proposed Treatments of Patients Having AD With Ionizing Radiation
Bistolfi states that vascular–cerebral amyloidosis is the hallmark of AD.24 Localized tracheobronchial amyloidosis (TBA) has been successfully treated with beams of radiation, 20 Gy in 10 fractions of 200 cGy in 2 weeks. As 20 Gy in 2 weeks is followed by inflammatory reactions, this high dosage cannot be suggested in the hypothetical treatment of AD. An innovative alternative might be a weekly long-term low dose, say 50 to 100 cGy, fractionated radiotherapy (RT), matching the very slow response of amyloid to radiation. Before applying it to patients with AD, the proposed schedule should be tried in patients with TBA to compare the new results of long-term fractionated RT with the results of 20 Gy/2 w. Should long-term fractionated RT prove effective, its application to patients with AD might become an effective and safe treatment.24
Doss discusses the concerns that have been expressed recently regarding the observed increased DNA damage from activities such as thinking and exercise.25 Such concerns have arisen from an incomplete accounting of the full effects of the increased oxidative damage. When the effects of the induced adaptive protective responses, such as increased antioxidants and DNA repair enzymes, are taken into consideration, there would be less endogenous DNA damage during the subsequent period of enhanced defenses, resulting in improved health from the thinking and exercise activities. A low dose of radiation, which causes oxidative stress and increased DNA damage, upregulates adaptive protection systems that decrease diseases. There are ongoing debates regarding the carcinogenicity of low radiation, with 2 recent advisory committee reports coming to opposite conclusions. Data published since then have overwhelmingly ruled out its carcinogenicity, paving the way to consider its use for disease reduction. Stimulation of adaptive protection with low doses of radiation is a promising approach to control neurodegenerative diseases, for which there are no methods of prevention or cure. A compelling ethics case should be written to pave the way for a clinical study using low doses of radiation to treat AD and other neurodegenerative diseases.25
A study in Australia on the use of ultrasound energy removed Aβ and restored memory in an AD mouse model.26 Since mechanical stress is a method of upregulating adaptive protective systems, it is not surprising that this approach succeeded. The authors used repeated scanning ultrasound (SUS) treatments of the mouse brain, without the need for any additional therapeutic agent such as anti-Aβ antibody. Spinning disk confocal microscopy and high-resolution 3D reconstruction revealed extensive internalization of Aβ into the lysosomes of activated microglia in mouse brains, with no concomitant increase observed in the number of microglia. Plaque burden was reduced compared to the sham-treated mice. Cleared plaques were observed in 75% of SUS-treated mice. These mice also displayed improved performance on 3 memory tasks. These findings suggest that repeated SUS could be considered as a potential treatment for AD in humans.26 The significant physical differences between the skull of a human and a mouse would present a major challenge.
On July 17, 2013, an application for a patent was published, titled Radiation therapy for treating Alzheimer’s disease.27 It makes 14 claims for treating human patients by a method, which is based on studies carried out using mice. The method comprises administering a relatively large amount of ionizing radiation to the brain of the patient employing a variety of different radiation sources. The total dose ranges from 300 to 1800 cGy, administered in dose fractions of 50 to 300 cGy per day. The method is claimed to treat AD by reducing the number or size of amyloid plaques in the brain of the patient.27
Discussion
Was it the low doses of ionizing radiation from the CT scans to the brain that produced the beneficial health effects (decrease in AD symptoms) observed in this patient? Improvements in symptoms of patient with AD have occurred without any treatment but rarely. Generally, patients with advanced AD progress inexorably to death. It is very unusual to observe such a strong reversal. Some might argue that this is only an anecdotal case; however, it is a fact that a very significant improvement happened within 2 days after the first 2 radiation exposures totalling 82 mGy. And further improvements were observed soon after the third and fourth radiation exposures. As of January 30, 2016, the patient has recovered from her very disappointing setback, following the October 1 exposure, and her condition continues to improve.
Assuming that AD develops because a person’s protective system becomes less effective with age and fails to prevent, repair, remove, and replace all of the endogenously occurring cell and tissue damage, it is reasonable to expect that stimulation of these systems by applying a small amount of stress would prevent, stop, or reverse some of this damage. This stress could be administered, either continuously or in a series of dose fractions, to induce these systems to adapt to higher levels of activity. A booster treatment could be given annually or when signs of increased AD reappear.
Since the process of AD begins well before clinical symptoms arise, it would be wise to start prophylactic treatment as soon as the onset of AD is identified to increase its latency.
Bistolfi points out that ten 200-cGy radiation treatments for removing plaque are far too intense for treating AD. He suggests the alternative of a weekly long-term low dose, 50 to 100 cGy.24 The human evidence of our case report suggests the optimum cumulative dose is about 160 to 180 mGy. The dose ranges in the patent application,27 300 to 1800 cGy, are far above the optimum radiation dose identified in our case report.
Conclusion
Alzheimer disease is the most common cause of dementia and is one of the leading sources of morbidity and mortality in the aging population. There are no treatments to cure or delay it. The costs to care for the patients with AD in the United States are very high and are expected to double by 2040.
This case report provides human evidence that low doses of ionizing radiation to the brain, as provided in several normal CT scans, can produce significant improvements in the condition of a patient with advanced AD.
This evidence suggests a need for clinical studies to develop an optimal treatment, based on the stimulation of the adaptive protection systems with low doses of ionizing radiation or other stressors. Upregulation of these protective systems in aged people would reverse, stop, or delay cell and tissue damage and would prevent or cure AD.
Notes
An average cell weighs about 10− 9 g. Therefore, a person weighing 70 kg has about 70 trillion cells.
The gray (Gy) is the SI unit for absorbed ionizing radiation dose, energy in joules per kilogram of mass. A dose of 1 Gy = 1 J/kg; 1 mGy = 0.001 Gy, and 1 cGy = 0.01 Gy = 1 rad.
Footnotes
Authors' Note: The subject matter of this publication is included in pending patent applications.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Wolk DA, Dickerson BC. Clinical features and diagnosis of Alzheimer disease. UpToDate. 2015. Web site http://www.uptodate.com/. Accessed February 2, 2016.
- 2. Sherva R, Kowall NW. Genetics of Alzheimer disease. UpToDate. 2015. Web site http://www.uptodate.com/. Accessed February 2, 2016.
- 3. Keene CD, Montine TJ, Kuller LH. Epidemiology, pathology, and pathogenesis of Alzheimer disease. UpToDate. 2015. Web site http://www.uptodate.com/. Accessed February 2, 2016.
- 4. Relkin N. Neuroimaging studies in the evaluation of dementia. UptoDate. 2015. Web site http://www.uptodate.com/. Accessed February 2, 2016.
- 5. Mitchell SL. Palliative care of patients with advanced dementia. UpToDate. 2015. Web site http://www.uptodate.com/. Accessed February 2, 2016.
- 6. Boggs JG. Seizures and epilepsy in the elderly patient: Etiology, clinical presentation, and diagnosis. UpToDate. 2015. Web site http://www.uptodate.com/. Accessed February 2, 2016.
- 7. Press D, Alexander M. Treatment of dementia. UpToDate. 2015. Web site http://www.uptodate.com/. Accessed February 2, 2016.
- 8. Johnson KA, Minoshima S, Bohnen NI, et al. Appropriate use criteria for amyloid PET: a report of the Amyloid Imaging Task Force, the Society of Nuclear Medicine and Molecular Imaging, and the Alzheimer’s Association. J Nucl Med. 2013;54(3):476–490. [DOI] [PubMed] [Google Scholar]
- 9. Cuttler JM, Pollycove M. Can cancer be treated with low doses of radiation? J Am Phys Surg. 2003;8(4):108–111. Web site http://www.jpands.org/vol8no4/cuttler.pdf. Accessed March 16, 2016. [Google Scholar]
- 10. Murphy JB, Morton JJ. The effect of roentgen rays on the rate of growth of spontaneous tumors in mice. J Exper Med. 1915;22(6):800–803. Web site http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2125377/pdf/800.pdf. Accessed March 16, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cuttler JM. Commentary on Fukushima and beneficial effects of low radiation. Dose Response. 2013;11(4):432–443. Web site http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3834738/. Accessed March 16, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cuttler JM. Remedy for radiation fear—discard the politicized science. Dose Response. 2014;12(2):170–184. Web site http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4036393/. Accessed March 16, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Calabrese EJ, Dhawan G, Kapoor R. Use of X-rays to treat shoulder tendonitis/bursitis: a historical assessment. Arch Toxicol. 2014;88(8):1503–1517. [DOI] [PubMed] [Google Scholar]
- 14. Calabrese EJ, Dhawan G, Kapoor R. The use of X-rays in the treatment of bronchial asthma: a historical assessment. Radiat Res. 2015;184(2):180–192. [DOI] [PubMed] [Google Scholar]
- 15. Calabrese EJ, Baldwin LA. The effects of gamma rays on longevity. Biogerontology. 2000;1(4):309–319. [DOI] [PubMed] [Google Scholar]
- 16. Feinendegen LE, Brooks AL, Morgan WF. Biological consequences and health risks of low-level exposure to ionizing radiation: commentary on the workshop. Health Phys. 2011;100(3):247–259. [DOI] [PubMed] [Google Scholar]
- 17. Feinendegen LE, Pollycove M, Neumann RD, ed. Hormesis by low dose radiation effects: low-dose cancer risk modeling must recognize up-regulation of protection In: Baum RP. Therapeutic Nuclear Medicine. Berlin, Germany: Springer; 2012:789–805. ISBN 973-3-540-36718-5. [Google Scholar]
- 18. Billen D. Spontaneous DNA damage and its significance for the “negligible dose” controversy in radiation protection. Radiat Res. 1990;124(2):242–245. Web site http://radiationeffects.org/wp-content/uploads/2014/08/Billen-1990_SpontaneousDNAdamage-RadProt.pdf. [PubMed] [Google Scholar]
- 19. Pollycove M, Feinendegen LE. Radiation-induced versus endogenous DNA damage: possible effect of inducible protective responses in mitigating endogenous damage. Hum Exp Toxicol. 2003;22(6):290–306. [DOI] [PubMed] [Google Scholar]
- 20. Cameron JR. Longevity is the most appropriate measure of health effects of radiation. Radiology. 2003;229(1):14–15. Web site http://pubs.rsna.org/doi/full/10.1148/radiol.2291030291. Accessed March 16, 2016. [DOI] [PubMed] [Google Scholar]
- 21. Cuttler JM, Feinendegen LE. Commentary on inhaled 239PuO2 in dogs—a prophylaxis against lung cancer? Dose Response. 2015;13(1):1–8. Web site http://dos.sagepub.com/content/13/1/dose-response.15-003.Cuttler.full. Accessed March 16, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Fliedner TM, Graessle DH, Meineke V, Feinendegen LE. Hemopoietic response to low dose-rates of ionizing radiation shows stem cell tolerance and adaptation. Dose Response. 2012;10(4):644–663. Web site http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3526333/. Accessed March 16, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mitchel RE, Burchart P, Wyatt H. A lower dose threshold for the in vivo protective adaptive response to radiation. Tumorigenesis in chronically exposed normal and Trp53 heterozygous C57BL/6 mice. Radiat Res. 2008;170(6):765–775. [DOI] [PubMed] [Google Scholar]
- 24. Bistolfi F. Localized amyloidosis and Alzheimer’s disease: the rationale for weekly long-term low dose amyloid-based fractionated radiotherapy. Neuroradiol J. 2008;21(5):683–692. [DOI] [PubMed] [Google Scholar]
- 25. Doss M. Low dose radiation adaptive protection to control neurodegenerative diseases. Dose Response. 2014;12(2):277–287. Web site http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4036399/. Accessed March 16, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Leinenga G, Götz J. Scanning ultrasound removes amyloid-β and restores memory in an Alzheimer’s disease mouse model. Sci Transl Med. 2015;7(278):1–11. [DOI] [PubMed] [Google Scholar]
- 27. Martinez A, Marples B, Wilson G, Fontanesi J. Radiation therapy for treating Alzheimer’s disease (Patent Publication EP2613849 A1, Application No. EP20110824177). 2013. Web site http://www.google.com/patents/EP2613849A1?cl=en.