Abstract
Addiction is a chronic brain disease with consequences that remain problematic years after discontinuation of use. Despite this, treatment models focus on acute interventions and are carved out from the main health care system. The Patient Protection and Affordable Care Act (2010) brings the opportunity to change the way substance use disorder (SUD) is treated in the United States. The treatment of SUD must adapt to a chronic care model offered in an integrated care system that screens for at-risk patients and includes services needed to prevent relapses. The partnering of the health care system with substance abuse treatment programs could dramatically expand the benefits of prevention and treatment of SUD. Expanding roles of health information technology and nonphysician workforces, such as social workers, are essential to the success of a chronic care model.
Keywords: Substance use disorder, Affordable Care Act, chronic care model, health information technology, social workforce, screening brief intervention and referral to treatment
INTRODUCTION
Substance use disorder (SUD) is among the most serious and costly public health issues in the United States and globally. The estimated costs to the American economy were $223.5 billion in 2006 for excessive alcohol drinking (Bouchery, Harwood, Sacks, Simon, & Brewer, 2011) and $193 billion in 2007 for illicit drug abuse and related problems (U.S. Department of Justice & National Drug Intelligence Center, 2011). The urgency of the problem is epitomized by the sharp rise in the misuse and abuse of opioid analgesics in the United States over the past decade with the associated dramatic increases in death from overdoses (Centers for Disease Controls and Prevention [CDC], 2011; Paulozzi, 2011). This rising problem added an estimated economic cost of $53.4 billion in 2006 (Hansen, Oster, Edelsberg, Woody, & Sullivan, 2011). The epidemic of opioid abuse is particularly poignant in that it relates to the abuse of a medication prescribed by the health care system, highlighting the need for implementing screening and appropriate interventions or referrals for patients with a SUD in primary care settings.
Treatment for SUD has been separated from mainstream health care, partly due to the longstanding “carve-out” of the behavioral health–managed care system. The isolation of behavioral health care from mainstream medical care has impeded the delivery of integrated care and services needed by those with a SUD. Carving out the delivery and financing of behavioral managed care may have helped contain costs and improve the care for the more serious cases of abuse and addiction (Ma & McGuire, 1998), but the disadvantage is that the majority of individuals with mild and moderate substance use problems have missed the opportunity for early detection, timely intervention, and referral at an early stage of substance abuse (Tai, Wu, & Clark, 2012). This problem is amplified by the large proportion of patients with a SUD with comorbid mental health and other medical conditions (Stein, 1999).
On the other hand, the benefits of integrated systems are shown by a randomized clinical trial (RCT) in which individuals with comorbid SUD and physical conditions had significantly higher utilization of inpatient care and emergency room visits when assigned to an independent care group compared to those assigned to an integrated care group (Parthasarathy, Mertens, Moore, & Weisner, 2003). Integration of care is not only more practical for the substance abuser but also serves to educate health care providers and counselors about their unique therapeutic tools and expertise facilitating adoption of medication and behavioral therapies that may have otherwise been dismissed (Carter, 1990; Williams et al., 1999).
Treatments for SUD in the United States have often been viewed as inadequate or ineffective due to the high rates of relapse (McLellan, Lewis, O'Brien, & Kleber, 2000). Acute episodic treatment models, which are the norm for SUD by themselves, are insufficient to prevent subsequent relapses (McKay, 2005; McLellan, McKay, Forman, Cacciola, & Kemp, 2005). Not only does the high rate of relapse demoralize patients and those who care for them, it also negatively affects public opinion by misleading policy makers into thinking that SUD treatment does not work (McLellan, 2002).
Addiction is recognized as a chronic brain disease in that the changes of the brain associated with repeated drug exposures persist for a long time after drug discontinuation (Volkow & Li, 2005). Thus, SUD treatment should not focus solely on temporary abstinence, or acute management of withdrawal symptoms but include long-term strategies for reducing relapse and improving the quality of patients’ medical and social lives. However, the tools and infrastructure to support the management of SUD as a chronic disease have been lacking in our health care system. For example, the continuous monitoring and intervening tools needed for the proper care of patients with a SUD are not supported by current payment systems, and there are no collaborative provider teams that can implement them (Anderson & Knickman, 2001; Dennis & Scott, 2012; McLellan, 2010; Rosenthal, Fernandopulle, Song, & Landon, 2004).
Thus, implementing strategies to prevent medical and social consequences from SUD is required. As introduced above, the necessary transformations in the care of SUD include (a) changing from a reactive model that intervenes when the person is already sick, to a proactive one that emphasizes preventive services such as implementation of screening and brief intervention (SBI) in primary care settings and (b) changing from an episodic acute model into a chronic care model (CCM) attuned to the chronic and relapsing characteristics of SUD. These changes of proactively seeking and screening patients with a SUD (who are often reluctant to seek help) and their long-term engagement in treatment will be able to substantially increase the number of effectively treated SUD patients. These proposed changes fit well within the Affordable Care Act (ACA) of 2010 (CCH Inc., 2010) and the Parity Act of 2008 (U.S. Department of the Treasury, U.S. Department of Labor, & U.S. Department of Health and Human Services, 2010) because this legislation requires that the SUD treatment coverage is “no more restrictive” than all other medical and surgical procedures.
HOW THE ACA CAN IMPROVE PREVENTIVE CARE FOR SUD
An estimated 22.1 million Americans age 12 or older were classified with dependence or abuse of alcohol and/or illicit drugs during 2010 (Substance Abuse and Mental Health Services Administration [SAMHSA], 2011). However, only 4.1 million of these individuals received some type of treatment, mostly in either self-help groups or rehabilitation centers, and very few received such care in the medical care systems (SAMHSA, 2011). Thus, the majority of individuals with risky drinking and/or drug use behaviors remain untreated or undertreated (see Figure 1, adopted from Dr. Thomas McLellan's presentation seen in Maslack, 2010).
FIGURE 1.
The triangle represents the U.S. population. The terms to the right of the figure refer to subpopulations by drug consumption level and the degree of substance use severity.
In addition, misuse and abuse of prescription drugs has become an alarming public health crisis in the United States that has evolved over the past 20 years. The increase in the diversion and abuse of opioid analgesics has been associated with the sharp rise of unintended overdose deaths in the United States over the past 10 to 15 years (CDC, 2011). Individuals with a SUD are also more likely to have mental disorders and physical health problems, including chronic pain that may require prescriptions of potentially addictive medications. Substance abusers without regular medical and substance abuse care are 10% to 27% more likely to be hospitalized than those with regular medical and/or substance abuse care (Laine et al., 2001). Screening and early intervention offered in the context of regular care, therefore, holds great potential for halting the progression of substance use problems into addiction and for curtailing the deleterious effects of drug abuse on pulmonary, cardiovascular, infectious, and mental diseases.
The primary health care setting is particularly well suited to screen for alcohol and drug use (Green, Cifuentes, Glasgow, & Stange, 2008; Lundberg, 1997; O'Connor & Samet, 2002). The high prevalence of alcohol and drug use problems detected in primary care settings (Pilowsky & Wu, 2012; Saitz, 2005) has made primary care settings key venues for early detection and prevention of alcohol and drug problems. For instance, a survey conducted in 2003 to 2005 in the New England area found that 15% of adolescents presenting at routine medical visits screened positive for alcohol or drug use (Knight et al., 2007). Research data also support the practice of SBI for harmful alcohol drinking in emergency departments and primary care settings (Bertholet, Daeppen, Wietlisbach, Fleming, & Burnand, 2005). Although universal SBI for harmful alcohol drinking in primary care setting has been recommended (Grade B) by U.S. Preventive Services Task Force since 2004 (U.S. Preventive Services Task Force, 2004; Whitlock, Polen, Green, Orleans, & Klein, 2004), many primary care practices have been slow to adopt it (Bradley et al., 2006).
Evidence to support the feasibility and efficacy of implementing Screening, Brief Intervention and Referral to Treatment (SBIRT) for illicit drugs and prescription medications in medical settings is not yet as extensive as that for licit substances (Saitz et al., 2010), but it is rapidly accumulating (Pilowsky & Wu, 2012). Bernstein et al. (2005) showed in a randomized controlled trial that a single brief motivational interview in a hospital medical visit helped cocaine and heroin addicts achieve abstinence. A large SAMHSA-sponsored demonstration program in six states also showed that implementing SBIRT in various general medical settings including emergency departments, rural health centers, and primary care clinics helped reduce patients’ drug use, increased the likelihood of entering specialty treatment, and improved their quality of life and reduced Medicaid costs (Estee, Wickizer, He, Shah, & Mancuso, 2010; Krupski et al., 2010; Madras et al., 2009). A state-funded (State of Florida) implementation project showed that SBI at seniors’ homes or centers decreased elderly patients’ odds of alcohol abuse, prescription drug misuse, and of depression (Schonfeld et al., 2010). Currently, multiple RCTs (ClinicalTrials.gov Identifier: NCT01683227, NCT01131520, NCT01003834, NCT00876941, NCT01113190, NCT01124591, NCT01207791, NCT00877331, NCT00913770) funded by the National Institute on Drug Abuse (NIDA) are evaluating the efficacy and effectiveness of various SBIRT strategies in identifying and intervening drug problems in emergency departments and primary care and improving health outcomes.
Evidence is mounting to support the inclusion of SBI as a reommended preventive service for SUD (Pilowsky & Wu, 2012). The ACA requires that preventive services be covered by health plans without cost sharing (Gray & Sullivan, 2011). As of January 1, 2014, substance abuse services will be considered “essential health benefits” to be included in the standard health benefit packages provided by health insurance companies. The mounting evidence and the legislative support by the ACA indicate that SBI for drug use will become available in primary care in the near future.
HOW THE ACA CAN IMPROVE THE LONG-TERM OUTCOMES OF SUD TREATMENT
The ACA eliminates lifetime caps and restricts the annual caps currently imposed by many of the insurance plans. This will allow for patients to receive continuing care for their SUD with affordable out-of-pocket spending. To successfully transform SUD care into a chronic care model to improve long-term outcomes, the treatment community must (a) embrace coordinated chronic care models, (b) adopt modern health information technologies, and (c) cultivate a multidisciplinary workforce.
Coordinated SUD Treatment in a Chronic Care Model (CCM)
Patients screened positive or diagnosed with substance abuse or dependence in first-line care settings should immediately begin a planned and coordinated chronic care treatment program with evidence-based treatment strategies. A CCM does not merely stand for extending time in treatment or follow-up. It is a multiprong patient care with the following key components: (a) self-management support, (b) decision support, (c) delivery system design, (d) clinical information systems, (e) health care organization, and (f) community resources (Bodenheimer, Wagner, & Grumbach, 2002a; Coleman, Austin, Brach, & Wagner, 2009). The CCM has been successfully adopted in treating common chronic diseases such as diabetes (Elissen et al., 2012; Kuo et al., 2011; Sunaert et al., 2010), hypertension (Gallagher, de Lusignan, Harris, & Cates, 2010), depression (Woltmann et al., 2012), and asthma (Mangione-Smith et al., 2005) in the United States and worldwide with improved care and health outcomes (Bodenheimer, Wagner, & Grumbach, 2002b; Coleman et al., 2009). Since the CCM was introduced more than a decade ago, clinical experiences and studies of CCM with many chronic diseases have demonstrated significant improvement of health outcomes associated with at least four key elements (Wagner, 1998). These key elements are (a) improving providers’ knowledge and skills in following treatment guidelines; (b) educating, engaging, and supporting patients to improve their self-efficacy and adherence to treatment plans; (c) emphasizing multidisciplinary team service at the organizational level to improve monitoring/reviewing and follow-up of patients; and (d) leveraging health information technology systems such as patient and/or disease specific registry and electronic health records (EHRs) to support the first three elements (Coleman et al., 2009; Renders et al., 2001). In summary, technology and people are the two major determinants of the success of a CCM (Dorr et al., 2006). Therefore, the establishment of strong health information exchange/sharing tools and a multidisciplinary and effective team-based service are crucial points when designing a CCM for SUD.
Adoption of Modern Health Information Technologies (HITs)
Chronic care management can be significantly hampered without effective health information exchange (Marchibroda, 2008). The widespread implementation of modern HITs, including EHRs, is now an essential tool to enable health information exchange and sharing among providers. The Health Information Technology for Economic and Clinical Health Act (HITECH Act), a critical component of the American Recovery and Reinvestment Act of 2009 (ARRA; United States 111th Congress, 2009), provides substantial financial incentives for health care providers to adopt certified EHRs for meaningful use (Blumenthal, 2010; Blumenthal & Tavenner, 2010). Inclusion of mental health and substance abuse treatment providers in HITECH incentive programs is an essential health policy victory that will allow for the integration of SUD care within primary care settings. Not only can EHRs help patients with a SUD move across different treatment providers with shared health information, but also consistently provide “treatment guidelines” to SUD care and primary care providers by embedding clinical decision support (CDS) algorithms into the EHRs. Implementation of EHRs can strongly support chronic care management and coordination. For instance, information included in EHRs can be an important alert to primary care and SUD care providers so that clinical decisions can be made in a timely fashion, resulting in a timely referral or reintervention to prevent relapse.
In addition, the explosion of mobile technologies in recent years is also expected to exert an important impact on the integrated chronic care (Topol, 2011). It encourages and facilitates patients and providers to adopt Tele-health. It is predicted that in the near future, patients can use their smart phones to transmit personal medical information such as images, locations, and hazardous environmental exposure data to a remote clinic for medical consultation and monitoring. In the context of SUD care, a patient's location may be important information for identifying and assessing potential relapses. In another example, consumers can download the MedlinePlus application free of charge on their smart phones and access health and drug information provided by the U.S. National Library of Medicine (NLM). This is an inexpensive and fast way to improve patients’ self-education and self-support critical to improving self-efficacy. In conclusion, advanced HITs are the essential tools for the integration of cost-effective and high-quality SUD care into a comprehensive health care system.
Social Workers as Care Managers for SUD in the CCM
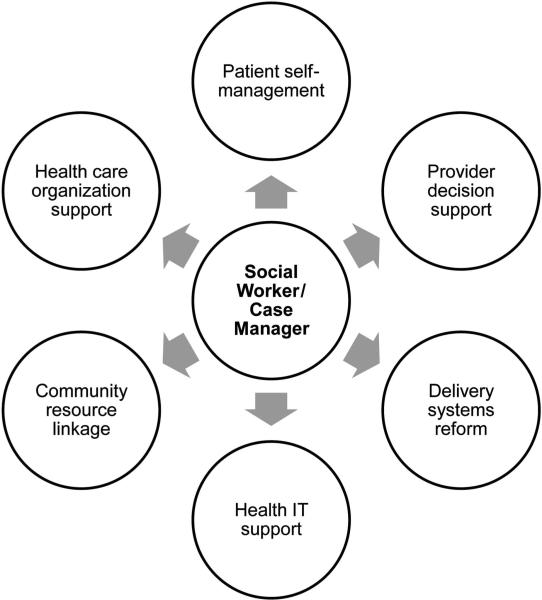
Advanced HITs are an effective tools to facilitate information sharing and communication but strong organizational support is also critical to achieving the aims of CCM (Protti, 2009). One major challenge in managing patients with chronic conditions is to engage patients in their treatment, increase their adherence to the treatment plan, and monitor their self-management (McLellan et al., 2000). For instance, individuals with SUD often face substantial psychosocial and cultural disadvantages such as a lack of social and/or family support and stable employment and face significant stigma (Serban, 1984). These negative factors can trigger relapse and are barriers to treatment adherence. In addition, there are also barriers in the service delivery system including poor communication and coordination between care providers and insufficient personnel. To overcome these barriers, it is critical to enhancing the roles of the nonphysician health care workforce, including nurses, health educators, behavioral health counselors, and social workers (Coleman et al., 2009). Social workers, for example, are well positioned to be “care managers” or “case managers” to help improve patients’ adherence to treatment and retention in treatment programs (see Figure 2). This figure illustrates how social workers can play a central coordinating role as care managers in helping individuals with SUDs and family members in a multiplicity of ways. For instance, a social worker in a OB/GYN hospital service facilitates and coordinates ongoing addiction treatment at a methadone maintenance clinic for a pregnant woman addicted to heroin; a social worker in a community mental health clinic determines that one of the factors contributing to clinical depression of a young woman is the stress associated with her husband's alcohol problem and refers her to Al-Anon, a mutual support program for family members; and a social worker in various medical settings may facilitate and educate patients who express interest in stopping smoking and provide counseling services that can help with smoking cessation. Social workers are well trained to (a) advocate for vulnerable populations such as patients with SUDs, (b) assist SUD patients and their families in seeking social support, (c) use their motivational interviewing skills to screen and assess risky substance use, (d) motivate SUD patients to modify unhealthy behaviors and be engaged in self-management support, (e) communicate with clinicians in making individualized clinical decisions based on assessment results, and (f) finally, as care mangers, to help ensure that health information contained in the EHRs flow smoothly and accurately within and across care organizations.
FIGURE 2.
The critical coordinating role of a social worker in an integrated care model for patients with substance use disorder. IT = information technology.
Over the last decade, social workers have played pivotal roles in group, family or individual counseling, medical/case management, and research/care coordination in clinical trials done through the Clinical Trial Network (CTN) funded by NIDA (Wells & Daley, 2012). In a continuing care model for addiction care developed by Chestnut Health Systems, “linkage managers,” who were well trained and experienced professionals in public health or social work fields, played a key role in the long-term-care management of SUD called “Recovery Management Checkups” (RMC) (Dennis, Foss, & Scott, 2007; Dennis & Scott, 2012). “Linkage Managers” helped participants identify early relapse symptoms and be engaged in reinterventions. Participants in the RMC group, compared with the control group, had 19% more reinterventions during a 4-year period, and experienced a much longer period of time in abstinence (1,026 vs. 93 days) and less time (89 vs. 126 months) having substance use problems. Of note, the long-term abstinence (4–7 years) was associated with more social support in housing, living conditions, employment, and mental health services (Dennis & Scott, 2012).
CONCLUSIONS
Addiction is a chronic disease for which multiple episodes of treatment, remission, relapse, and retreatment frequently occur before achieving stable recovery. The recent health care reform legislation provides many opportunities to transform an episodic and reactive treatment model into a proactive chronic treatment care model. A comprehensive CCM for SUD should start from routine SBI in primary care settings to detect early-risk behaviors in patients. The care for persons diagnosed with SUD should follow a CCM with effective coordination and collaboration between primary care and behavioral health care services to ensure continuity of care. Aggressively leveraging modern HITs and expanding roles of nonphysician workforces, such as social workers, are critical to the success of chronic care management of SUD. With a new transformed care model, prevention and early treatment for SUDs will become an essential part of a more effective continuing care system, which under full implementation of the ACA will lead to vastly improved public health in the United States.
ACKNOWLEDGMENT
Betty Tai and Nora D. Volkow are federal employees of the National Institute on Drug Abuse, the National Institutes of Health. There is no conflict of interests. The opinions expressed in this manuscript are those of the authors and do not represent the official position of the U.S. government.
Contributor Information
Betty Tai, Center for the Clinical Trials Network, National Institute on Drug Abuse, National Institutes of Health, Bethesda, Maryland, USA.
Nora D. Volkow, National Institute on Drug Abuse, National Institutes of Health, Bethesda, Maryland, USA
REFERENCES
- Anderson G, Knickman JR. Changing the chronic care system to meet people's needs. Health Affairs. 2001;20(6):146–160. doi: 10.1377/hlthaff.20.6.146. [DOI] [PubMed] [Google Scholar]
- Bernstein J, Bernstein E, Tassiopoulos K, Heeren T, Levenson S, Hingson R. Brief motivational intervention at a clinic visit reduces cocaine and heroin use. Drug and Alcohol Dependence. 2005;77(1):49–59. doi: 10.1016/j.drugalcdep.2004.07.006. [DOI] [PubMed] [Google Scholar]
- Bertholet N, Daeppen JB, Wietlisbach V, Fleming M, Burnand B. Reduction of alcohol consumption by brief alcohol intervention in primary care: Systematic review and meta-analysis. Archives of Internal Medicine. 2005;165(9):986–995. doi: 10.1001/archinte.165.9.986. [DOI] [PubMed] [Google Scholar]
- Blumenthal D. Launching HITECH. New England Journal of Medicine. 2010;362(5):382–385. doi: 10.1056/NEJMp0912825. [DOI] [PubMed] [Google Scholar]
- Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. New England Journal of Medicine. 2010;363(6):501–504. doi: 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. Journal of the American Medical Association. 2002a;288(14):1775–1779. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: The chronic care model, Part 2. Journal of the American Medical Association. 2002b;288(15):1909–1914. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- Bouchery EE, Harwood HJ, Sacks JJ, Simon CJ, Brewer RD. Economic costs of excessive alcohol consumption in the U.S., 2006. American Journal of Preventive Medicine. 2011;41(5):516–524. doi: 10.1016/j.amepre.2011.06.045. [DOI] [PubMed] [Google Scholar]
- Bradley KA, Williams EC, Achtmeyer CE, Volpp B, Collins BJ, Kivlahan DR. Implementation of evidence-based alcohol screening in the Veterans Health Administration. American Journal of Managed Care. 2006;12(10):597–606. [PubMed] [Google Scholar]
- Carter BL. Pharmacotherapy and the primary care physician. Primary Care: Clinics in Office Practice. 1990;17(3):469–477. [PubMed] [Google Scholar]
- CCH Incorporated . Patient Protection and Affordable Care Act; Health Care and Education Reconciliation Act of 2010: Text of P.L. 111-148, as signed by the President on March 23, 2010; text of P.L. 111-152, as signed by the President on March 30, 2010: JCT technical explanation of P.L. 111-148 and P.L. 111-152. Author; Chicago, IL: 2010. [Google Scholar]
- Centers for Disease Control and Prevention [CDC] Vital signs: Overdoses of prescription opioid pain relievers—United States, 1999–2008. Morbidity and Mortality Weekly Report. 2011;60(43):1487–1492. [PubMed] [Google Scholar]
- Coleman K, Austin BT, Brach C, Wagner EH. Evidence on the chronic care model in the new millennium. Health Affairs. 2009;28(1):75–85. doi: 10.1377/hlthaff.28.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis ML, Foss MA, Scott CK. An eight-year perspective on the relationship between the duration of abstinence and other aspects of recovery. Evaluation Review. 2007;31(6):585–612. doi: 10.1177/0193841X07307771. [DOI] [PubMed] [Google Scholar]
- Dennis ML, Scott CK. Four-year outcomes from the early re-intervention (ERI) experiment using recovery management checkups (RMCs). Drug and Alcohol Dependence. 2012;121(1/2):10–17. doi: 10.1016/j.drugalcdep.2011.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorr DA, Wilcox A, Burns L, Brunker CP, Narus SP, Clayton PD. Implementing a multidisease chronic care model in primary care using people and technology. Disease Management. 2006;9(1):1–15. doi: 10.1089/dis.2006.9.1. [DOI] [PubMed] [Google Scholar]
- Elissen AM, Steuten LM, Lemmens LC, Drewes HW, Lemmens KM, Meeuwissen JA, Vrijhoef HJ. Meta-analysis of the effectiveness of chronic care management for diabetes: Investigating heterogeneity in outcomes. Journal of Evaluation in Clinical Practice. 2012 doi: 10.1111/j.1365-2753.2012.01817.x. doi:10.1111/j.1365-2753.2012.01817.x. [DOI] [PubMed] [Google Scholar]
- Estee S, Wickizer T, He L, Shah MF, Mancuso D. Evaluation of the Washington state screening, brief intervention, and referral to treatment project: Cost outcomes for Medicaid patients screened in hospital emergency departments. Medical Care. 2010;48(1):18–24. doi: 10.1097/MLR.0b013e3181bd498f. [DOI] [PubMed] [Google Scholar]
- Gallagher H, de Lusignan S, Harris K, Cates C. Quality-improvement strategies for the management of hypertension in chronic kidney disease in primary care: A systematic review. British Journal of General Practice: The Journal of the Royal College of General Practitioners. 2010;60(575):e258–265. doi: 10.3399/bjgp10X502164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray BJ, Sullivan KC. Provisions in the Patient Protection and Affordable Care Act (PPACA) Nova Science Publisher's; New York, NY: 2011. [Google Scholar]
- Green LA, Cifuentes M, Glasgow RE, Stange KC. Redesigning primary care practice to incorporate health behavior change: Prescription for health round-2 results. American Journal of Preventive Medicine. 2008;35(5 Suppl):S347–S349. doi: 10.1016/j.amepre.2008.08.013. [DOI] [PubMed] [Google Scholar]
- Hansen RN, Oster G, Edelsberg J, Woody GE, Sullivan SD. Economic costs of nonmedical use of prescription opioids. Clinical Journal of Pain. 2011;27(3):194–202. doi: 10.1097/AJP.0b013e3181ff04ca. [DOI] [PubMed] [Google Scholar]
- Knight JR, Harris SK, Sherritt L, Van Hook S, Lawrence N, Brooks T, Kulig J. Prevalence of positive substance abuse screen results among adolescent primary care patients. Archives of Pediatrics and Adolescent Medicine. 2007;161(11):1035–1041. doi: 10.1001/archpedi.161.11.1035. [DOI] [PubMed] [Google Scholar]
- Krupski A, Sears JM, Joesch JM, Estee S, He L, Dunn C, Ries R. Impact of brief interventions and brief treatment on admissions to chemical dependency treatment. Drug and Alcohol Dependence. 2010;110(1/2):126–136. doi: 10.1016/j.drugalcdep.2010.02.018. [DOI] [PubMed] [Google Scholar]
- Kuo S, Bryce CL, Zgibor JC, Wolf DL, Roberts MS, Smith KJ. Cost-effectiveness of implementing the chronic care model for diabetes care in a military population. Journal of Diabetes Science and Technology. 2011;5(3):501–513. doi: 10.1177/193229681100500305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laine C, Hauck WW, Gourevitch MN, Rothman J, Cohen A, Turner BJ. Regular outpatient medical and drug abuse care and subsequent hospitalization of persons who use illicit drugs. Journal of the American Medical Association. 2001;285(18):2355–2362. doi: 10.1001/jama.285.18.2355. [DOI] [PubMed] [Google Scholar]
- Lundberg GD. New winds blowing for American drug policies. Journal of the American Medical Association. 1997;278(11):946–947. [PubMed] [Google Scholar]
- Ma CA, McGuire TG. Costs and incentives in a behavioral health carve-out. Health Affairs. 1998;17(2):53–69. doi: 10.1377/hlthaff.17.2.53. [DOI] [PubMed] [Google Scholar]
- Madras BK, Compton WM, Avula D, Stegbauer T, Stein JB, Clark HW. Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: Comparison at intake and 6 months later. Drug and Alcohol Dependence. 2009;99(1/3):280–295. doi: 10.1016/j.drugalcdep.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangione-Smith R, Schonlau M, Chan KS, Keesey J, Rosen M, Louis TA, Keeler E. Measuring the effectiveness of a collaborative for quality improvement in pediatric asthma care: Does implementing the chronic care model improve processes and outcomes of care? Ambulatory Pediatrics: The Official Journal of the Ambulatory Pediatric Association. 2005;5(2):75–82. doi: 10.1367/A04-106R.1. [DOI] [PubMed] [Google Scholar]
- Marchibroda JM. The impact of health information technology on collaborative chronic care management. Journal of Managed Care Pharmacy. 2008;14(2 Suppl):S3–S11. [PubMed] [Google Scholar]
- Maslack B. Will primary care doctors help implement primary services in addiction prevention and treatment? The New York Society of Addiction Medicine. 2010 Feb 22; Retrieved from http://nysam-asam.com/news-member-news-classifieds/2010/2/22/will-primary-care-doctors-help-implement-primary-services-in.html.
- McKay JR. Is there a case for extended interventions for alcohol and drug use disorders? Addiction. 2005;100(11):1594–1610. doi: 10.1111/j.1360-0443.2005.01208.x. [DOI] [PubMed] [Google Scholar]
- McLellan AT. Have we evaluated addiction treatment correctly? Implications from a chronic care perspective. Addiction. 2002;97(3):249–252. doi: 10.1046/j.1360-0443.2002.00127.x. [DOI] [PubMed] [Google Scholar]
- McLellan AT. Treatment given high priority in new White House drug control policy. Interview by Bridget Kuehn. Journal of the American Medical Association. 2010;303(9):821–822. doi: 10.1001/jama.2010.210. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Lewis DC, O'Brien CP, Kleber HD. Drug dependence, a chronic medical illness: Implications for treatment, insurance, and outcomes evaluation. Journal of the American Medical Association. 2000;284(13):1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- McLellan AT, McKay JR, Forman R, Cacciola J, Kemp J. Reconsidering the evaluation of addiction treatment: From retrospective follow-up to concurrent recovery monitoring. Addiction. 2005;100(4):447–458. doi: 10.1111/j.1360-0443.2005.01012.x. [DOI] [PubMed] [Google Scholar]
- O'Connor PG, Samet JH. Substance abuse: The expanding role of general internal medicine. Journal of General Internal Medicine. 2002;17(5):398–399. doi: 10.1046/j.1525-1497.2002.20212.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parthasarathy S, Mertens J, Moore C, Weisner C. Utilization and cost impact of integrating substance abuse treatment and primary care. Medical Care. 2003;41(3):357–367. doi: 10.1097/01.MLR.0000053018.20700.56. [DOI] [PubMed] [Google Scholar]
- Paulozzi LJ. Drug-induced deaths—United States, 2003–2007. MMWR. Surveillance Summaries. 2011;60(Suppl):60–61. [PubMed] [Google Scholar]
- Pilowsky DJ, Wu LT. Screening for alcohol and drug use disorders among adults in primary care: A review. Substance Abuse and Rehabilitation. 2012;3(1):25–34. doi: 10.2147/SAR.S30057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Protti D. Integrated care needs integrated information management and technology. Healthcare Quarterly. 2009;13(Spec No):24–29. doi: 10.12927/hcq.2009.21093. [DOI] [PubMed] [Google Scholar]
- Renders CM, Valk GD, Griffin S, Wagner EH, Eijk JT, Assendelft WJ. Interventions to improve the management of diabetes mellitus in primary care, outpatient and community settings. Cochrane Database of Systematic Reviews. 2001;(4) doi: 10.1002/14651858.CD001481. Art No. CD001481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal MB, Fernandopulle R, Song HR, Landon B. Paying for quality: Providers' incentives for quality improvement. Health Affairs. 2004;23(2):127–141. doi: 10.1377/hlthaff.23.2.127. [DOI] [PubMed] [Google Scholar]
- Saitz R. Clinical practice. Unhealthy alcohol use. New England Journal of Medicine. 2005;352(6):596–607. doi: 10.1056/NEJMcp042262. [DOI] [PubMed] [Google Scholar]
- Saitz R, Alford DP, Bernstein J, Cheng DM, Samet J, Palfai T. Screening and brief intervention for unhealthy drug use in primary care settings: Randomized clinical trials are needed. Journal of Addiction Medicine. 2010;4(3):123–130. doi: 10.1097/ADM.0b013e3181db6b67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schonfeld L, King-Kallimanis BL, Duchene DM, Etheridge RL, Herrera JR, Barry KL, Lynn N. Screening and brief intervention for substance misuse among older adults: The Florida BRITE project. American Journal of Public Health. 2010;100(1):108–114. doi: 10.2105/AJPH.2008.149534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serban G. Social stress and drug abuse. In: Serban G, editor. The social and medical aspects of drug abuse. Springer Netherlands; New York, NY: 1984. pp. 125–133. [Google Scholar]
- Stein MD. Medical consequences of substance abuse. Psychiatric Clinics of North America. 1999;22(2):351–370. doi: 10.1016/s0193-953x(05)70081-2. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Results from the 2010 National Survey on Drug Use and Health: Summary of National Findings. Author; Rockville, MD: 2011. NSDUH Series H-41, HHS Publication No. SMA 11-4658. [Google Scholar]
- Sunaert P, Bastiaens H, Nobels F, Feyen L, Verbeke G, Vermeire E, De Sutter A. Effectiveness of the introduction of a chronic care model-based program for type 2 diabetes in Belgium. BMC Health Services Research. 2010;10:207. doi: 10.1186/1472-6963-10-207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tai B, Wu L, Clark H. Electronic health records: Essential tools in integrating substance abuse treatment with primary care [Commentary]. Substance Abuse and Rehabilitation. 2012;3:8. doi: 10.2147/SAR.S22575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topol E. Mobile-izing healthcare. Wireless technologies will continue to revolutionize the industry. Modern Healthcare. 2011;52(Suppl) [PubMed] [Google Scholar]
- United States 111th Congress . Stimulus: American Recovery and Reinvestment Act of 2009 Public Law 111-5 Official Text. Government Institutes/Bernan Press; Lanham, MD: 2009. [Google Scholar]
- U.S. Preventive Services Task Force Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: Recommendation statement. Annals of Internal Medicine. 2004;140(7):554–556. doi: 10.7326/0003-4819-140-7-200404060-00016. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Justice & National Drug Intelligence Center National drug threat assessment, 2011. 2011 Retrieved from https://www.ncjrs.gov/App/Publications/abstract.aspx?ID=258072.
- U.S. Department of the Treasury, U.S. Department of Labor, & U.S. Department of Health and Human Services Interim final rules under the Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act of 2008. Interim final rules with request for comments. Federal Register. 2010;75(21):5409–5451. [PubMed] [Google Scholar]
- Volkow N, Li TK. The neuroscience of addiction. Nature Neuroscience. 2005;8(11):1429–1430. doi: 10.1038/nn1105-1429. [DOI] [PubMed] [Google Scholar]
- Wagner EH. Chronic disease management: What will it take to improve care for chronic illness? Effective Clinical Practice. 1998;1(1):2–4. [PubMed] [Google Scholar]
- Wells EA, Daley DC. NIDA's clinical trials network: A source of social work practice-relevant knowledge.. Paper presented at the Annual Meeting of the Society for Social Work and Research; Washington DC.. Jan 11–15, 2012. [Google Scholar]
- Whitlock EP, Polen MR, Green CA, Orleans T, Klein J. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: A summary of the evidence for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2004;140(7):557–568. doi: 10.7326/0003-4819-140-7-200404060-00017. [DOI] [PubMed] [Google Scholar]
- Williams JW, Jr., Rost K, Dietrich AJ, Ciotti MC, Zyzanski SJ, Cornell J. Primary care physicians' approach to depressive disorders. Effects of physician specialty and practice structure. Archives of Family Medicine. 1999;8(1):58–67. doi: 10.1001/archfami.8.1.58. [DOI] [PubMed] [Google Scholar]
- Woltmann E, Grogan-Kaylor A, Perron B, Georges H, Kilbourne AM, Bauer MS. Comparative effectiveness of collaborative chronic care models for mental health conditions across primary, specialty, and behavioral health care settings: Systematic review and meta-analysis. American Journal of Psychiatry. 2012;169(8):790–804. doi: 10.1176/appi.ajp.2012.11111616. [DOI] [PubMed] [Google Scholar]