Abstract
Objective
This study examines: 1) whether youth and their caregivers have different preferences for asthma education video topics and 2) if education topic preferences vary by youth and caregiver sociodemographic characteristics.
Methods
Youth (n=83) ages 7–17 years with persistent asthma and their caregivers were recruited at two pediatric practices in North Carolina. Sociodemographic information and youth and caregiver preferences for 9 asthma video education topics were collected during in-person interviews. Bonferroni-corrected chi-square or McNemar tests (α=0.0056) were used to compare youth and caregivers differences in topic preferences and topic preferences by youth and caregiver sociodemographic characteristics, including gender, race, ethnicity, and age.
Results
Youth were primarily male (52%) and from low-income families (74%; caregiver annual income less than $30,000) and many were Hispanic (45%). Youth and parents expressed the most interest in the following two topics: “how to deal with triggers” (90% and 95%, respectively) and “how to keep asthma under control” (87% and 96%, respectively). Caregivers and children were discordant for two topics: “the difference between a rescue and controller medicine” and “how to [help your child] talk to your [his/her] friends about asthma.” No differences were found between youth and caregiver sociodemographic characteristics and video topic preferences.
Conclusions
Youth with persistent asthma and their caregivers differed in their asthma education topic preferences, but preferences did not vary by caregiver or youth sociodemographic characteristics. Studies examining the effectiveness of interventions tailored to differences in educational preferences of youth with asthma and their caregivers are needed.
Keywords: children, respiratory disease, predilections, audiovisual, instruction
Introduction
Asthma is one of the most common chronic health conditions among youth, affecting approximately 10% of children and adolescents in the United States (1). Racial and ethnic minorities have a higher likelihood of having asthma (2) and poorly controlled asthma is more prevalent among school-aged minority youth (3). One of the most important aspects of controlling this respiratory condition is patient self-management (4, 5). Asthma education designed to improve self-management has been shown to improve lung function, increase asthma management self-efficacy, decrease missed school days, decrease activity limitations and reduce emergency room visits (6, 7). Asthma education for caregivers, together with child asthma education, is a valuable part of the management process and an important factor in optimizing asthma control and improving health outcomes for youth with asthma (8).
Asthma education can be delivered using a wide range of methods, including one-on-one education by a health professional, written materials, interactive games, and educational videos (9). One study shows youth prefer asthma videos compared to one-on-one feedback or print media (e.g., magazine or booklet) (10) and a review found that adults prefer multimedia health materials (e.g., video, film, and computer) compared to print (11). Health education videos provide value as an education tool because they are portable, can be viewed multiple times at the individual’s convenience, are widely appealing, can be tailored to individual characteristics, and are effective for use with lower literacy individuals (12–16).
Asthma education is often provided in physicians’ offices, outpatient clinics, hospitals, schools, in homes, or at pharmacies (17, 18). Videos have been shown to be effective for conveying health information, influencing viewers’ awareness, increasing interest and learning, and modifying health behaviors (10, 15, 19–21). Videos are frequently used as supplementary material to clarify asthma information graphically, or encourage patients and caregivers to ask questions in clinic settings (22).
A challenge in developing asthma educational video interventions intended for children with asthma as well as their adult caregivers is that, for optimal effectiveness, such interventions must appeal to both groups. However, we are unaware of any studies that have examined and compared asthma education preferences from the perspective of children with asthma and their caregivers, especially among hard-to-reach groups, such as Hispanics and adolescents. In fact, a recent review found no studies had comprehensively identified parental information needs, and few studies made a distinction between professionally-identified and parent-identified asthma information needs (23), which are often incongruent (24). We are not aware of any studies examining whether parent and child sociodemographic characteristics are associated with preferences for asthma-related education content. This study examines: 1) whether youth and their caregivers have different preferences for asthma education video topics and 2) whether education topic preferences vary by youth and caregiver sociodemographic characteristics.
Methods
Study design and participants
Child-caregiver dyads were recruited from two primary care clinics that were associated with the Expanding Network for Latinos through Community Engagement (ENLaCE) health research consortium in a medium-sized metropolitan county (population ~171 000) in North Carolina (25). Eligible children were ages 7 through 17 years, spoke English or Spanish, could read the assent form, were present at the visit with an adult caregiver (parent or legal guardian) who spoke English or Spanish, used a metered-dose-inhaler (MDI), missed or incorrectly performed at least one step on an inhaler technique assessment, and had mild, moderate, or severe persistent asthma. Persistent asthma was defined as experiencing asthma related daytime symptoms more than twice a week, asthma related nighttime symptoms more than twice a month, or receiving one or more long-term controller therapies for asthma (26, 27). Roughly half (51%) of patients in our sample had moderate/severe persistent asthma (49% had mild persistent asthma) (21).
Participants were enrolled from July 2012 to March 2013 and completed informed consent forms and brief sociodemographic questionnaires administered by a trained, bilingual research assistant prior to their medical visit. The research assistant read the survey questions aloud to children, and caregivers had the option of having the survey read aloud to them or to read it themselves. After the medical visit, the research assistant assessed the child’s metered dose inhaler (MDI) technique. Children were randomized to watch either a 3-minute MDI video (intervention group) designed to illustrate proper inhaler techniques or a nutrition video (control group) in English or Spanish on a laptop computer. The inhaler videos were designed for low health literate and limited English-speaking patients and provided an overview of the device and specific instructions for how to use the device correctly. The nutrition video discussed the importance of balancing protein, carbohydrates and lipids in one’s diet. Randomization was stratified by clinic and the sequence was prepared ahead of time by a statistician using computer-generated random numbers. Immediately after watching the videos, child asthma device technique was assessed a second time.
The child’s inhaler technique was assessed again at a one-month follow up visit where children and caregivers each completed a short interview that assessed their video topic preferences. Follow-up visits typically lasted 20 minutes and were conducted at a location (e.g. home, clinic, and library) that was convenient for the caregiver. Additional details about the larger randomized trial are reported elsewhere (21). This study used survey data collected at baseline (sociodemographic) and follow-up time points (video topic preferences).
We measured the following sociodemographic characteristics: child age (in years), gender, race (white, African American, other), ethnicity (Hispanic vs. not Hispanic) and study assignment status (experimental versus control); caregiver age (in years), gender, race, ethnicity, education level, type of health insurance; annual household income; and literacy level. Literacy level was measured using the Single Item Literacy Screener (SILS) to identify limited reading ability (one component of health literacy) (28). Caregivers were asked “How often do you need to have someone help you when you read instructions, pamphlets, or other written material from your doctor or pharmacy?” Response options include “never,” “rarely,” “sometimes,” “often,” and “always,” but are typically dichotomized as “never/rarely” vs “sometimes/often/always (28).” Outcome data for this study were taken from one question on the follow-up interview (“Would you want to watch a short asthma video about the following topics?”) that assessed caregiver and child asthma education topic interest for nine topics (“yes” or “no”). The nine topics are listed in Table 1. Video education topics were selected based on a qualitative study identifying factors influencing asthma management from the perspective of middle school students and a study identifying child- and caregiver-reported problems/concerns in using asthma medications (10, 29).
TABLE 1.
Study generated question asking about interest in specific asthma education topics
| Would you want to watch a short asthma video about the following topics?
| |
|---|---|
| Youth | Caregiver |
| 1. the difference between a rescue and controller medicine | 1. the difference between a rescue and controller medicine |
| 2. how to remember to take your asthma medicines | 2. how to help your child remember to take his/her asthma medicines |
| 3. tips for managing asthma at school | 3. how to help your child asthma at school |
| 4. tips for managing asthma when exercising or playing | 4. how to help your child manage asthma when exercising or playing |
| 5. how to talk to your friends about asthma | 5. how to help your child talk to his/her friends about asthma |
| 6. how to talk to your teachers and coaches about asthma | 6. how to help your child talk to school personnel about asthma |
| 7. how to talk to your doctor about asthma | 7. how to talk to your child’s doctor about asthma |
| 8. how to deal with asthma triggers | 8. how to deal with asthma triggers |
| 9. how to keep your asthma under control | 9. how to help keep your child’s asthma under control |
Statistical analysis
The sociodemographic characteristics of participants are described with absolute frequencies and percentages. McNemar tests were used to examine whether topic preferences varied between youth and their caregivers. Among youth, chi-square tests were calculated to assess whether asthma education topic preferences varied by child age (ages 7–11 versus ages 12–17), gender, race (White versus other), ethnicity (Hispanic versus not Hispanic) and study assignment status (experimental versus control). Similarly, among caregivers, chi-square tests were conducted to examine whether education topic preferences varied by caregiver age (ages < 40 years versus ≥ 40), gender, ethnicity (Hispanic versus not Hispanic), education (high school or less versus more than high school) and literacy level. In order to account for multiple comparisons, statistical significance was set at a p-value of less than 0.0056 (.05/9 tests) using Bonferroni correction for chi-square and McNemar tests. Analyses were conducted using SAS software, version 9.3 (SAS Institute, Cary, NC).
Results
Sample characteristics
Of the 143 families who were screened, 48 did not meet eligibility criteria, 4 declined to participate, and 91 (64%) were eligible and enrolled in the study. The main reason for ineligibility was not meeting the criteria for persistent asthma. Eight families were lost to follow-up, leaving 83 families (91%) who completed the 1-month follow-up visit. The eight families lost to follow-up were similar demographically to the interviewed families except that they were more likely to have at least a high school education (75% vs 34%, respectively). Sample characteristic information is provided in Table 2.
TABLE 2.
Youth (n=83) and Caregiver (n=83) Sociodemographic Characteristics
| % (N) | |
|---|---|
| Youth age | |
| 7 – 11 years old | 61 (51) |
| 12 – 17 years old | 39 (32) |
| Youth gender | |
| Boy | 52 (43) |
| Girl | 48 (40) |
| Youth race | |
| White | 38 (32) |
| African American | 24 (19) |
| Other | 38 (32) |
| Youth Ethnicity | |
| Hispanic | 45 (37) |
| Caregiver age | |
| 28 – 39 years old | 48 (40) |
| 40 and older | 52 (43) |
| Caregiver education in years | |
| High School or less | 66 (55) |
| More than High School | 34 (28) |
| Insurance type | |
| None | 1 (1) |
| Private | 16 (13) |
| Medicaid | 65 (54) |
| State Children’s Health Insurance Program | 18 (15) |
| Annual household income | |
| Less than $10,000 | 25 (21) |
| $10,000 – $19,999 | 28 (23) |
| $20,000 – $29,999 | 21 (17) |
| $30,000 – $49,999 | 19 (16) |
| $50,000 – $69,999 | 5 (4) |
| $70,000 or more | 2 (2) |
| Caregiver health literacy | |
| need help reading written material | 19 (16) |
| do not need help reading written material | 81 (67) |
Youth video topic preferences
Youth interest in wanting to watch a short asthma video about the various topics ranged from 39% to 90% (shown in Figure 1). Youth were most interested in the topic “how to deal with asthma triggers” (90%), followed by “how to keep asthma under control” (87%) and “tips for managing asthma when exercising or playing” (86%). Youth were least interested in the topic “how to talk to your friends about asthma” (39%).
Figure 1.
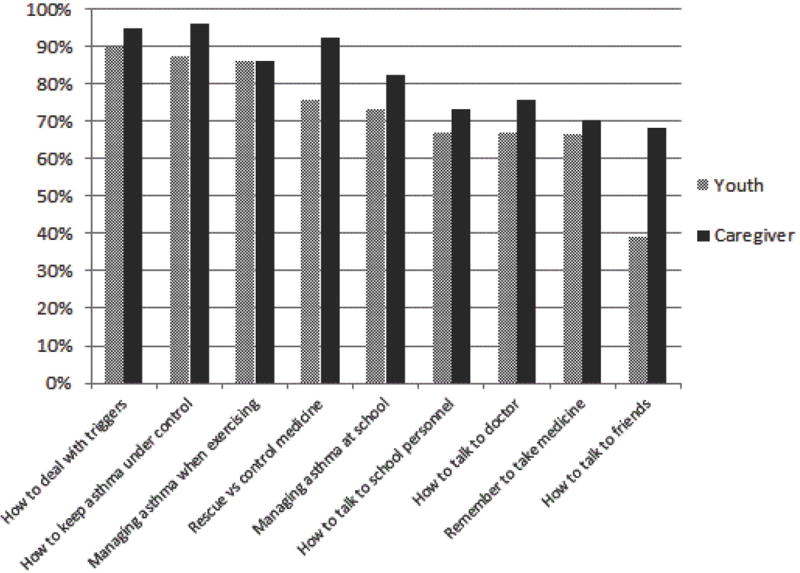
Youth and Caregiver Video Topic Preferences
Caregiver video topic preferences
Caregiver interest in all video topics was above 68% (Figure 1). Caregivers were most interested in the following topics: “how to help keep your child’s asthma under control” (96%), “how to deal with asthma triggers” (95%), and “the difference between a rescue and controller medicine” (92%).
Differences in child and caregiver video topic preferences
Caregivers and children were significantly discordant (where caregivers reported interest in a video topic and youth did not) for two topics: “the difference between a rescue and controller medicine” with 22% of the pairs discordant; McNemar test: χ 2 = 8.04, p = 0.0046) and “how to [help your child] talk to your [his/her] friends about asthma” with 29% of the pairs discordant; McNemar test: χ 2 = 23.0, p < 0.0001) (Figure 2).
Figure 2.
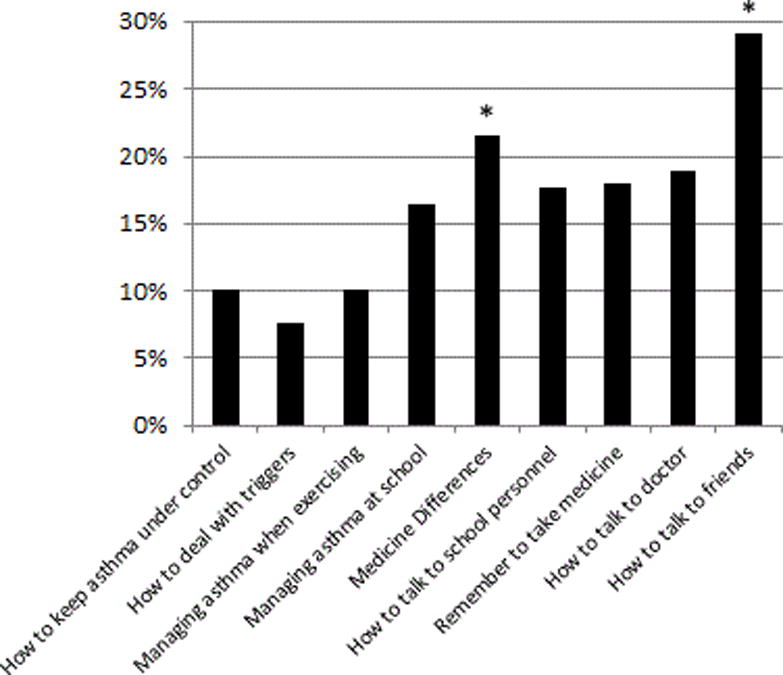
Youth and Caregiver Video Topic Interest Discordance. McNemar analyses comparing parent and child interest in each topic with Bonferroni correction (minimum α=.0056 for significance) indicating discordance where parents expressed an interest in topics and children did not.
Topic preference by study assignment status and sociodemographic characteristics
No significant differences were found related to parent and child topic preference and sociodemographic characteristics (child age, gender, race, ethnicity and study assignment status and caregiver age, gender, race, ethnicity, education level, type of health insurance, annual household income and literacy level) (data not shown).
Discussion
This study is the first to examine whether youth and their caregivers have different preferences for asthma education video topics and whether education topic preferences vary by youth and caregiver sociodemographic characteristics. Results from this study show youth with persistent asthma and their caregivers were strongly interested in receiving asthma management education topics via a brief asthma education video. Youth and caregivers were most interested in learning about how to manage asthma rather than learning how to talk to others about asthma. Both of these preferred topics relate to reducing asthma’s impact on activities of daily living and quality of life, important outcomes for youth and caregivers (30).
Among caregivers’ top three preferred topics was how to tell the difference between a rescue and controller medication. Findings from this study support results from another study showing that when asked about asthma education information that might be useful to them in caring for their child with asthma, caregivers reported information related to medication (58%) and common asthma triggers (62%) (31). Youth rated how to keep asthma under control, how to manage triggers, and managing asthma while exercising as highest among all of the topics. These preferences support research examining young adolescent preferences for an online support intervention finding most youth (82.4%) wanted information about coping with asthma (32).
We found discordance between parent and youth interest (parents expressing interest and youth not expressing interest) for video topics related to talking to friends about asthma and knowing the difference between rescue and controller medicines. The largest discordance, parent interest in helping their child talk to their friends about asthma and youth not expressing interest in the topic, may be related to parents’ expressed desire to prevent their child from feeling isolated or alone in dealing with asthma and to have peer support, while youth desire to fit in and not be different from peers (32). The finding that youth were less likely than caregivers to express interest for education regarding knowing the difference between rescue and controller medicines creates a dilemma for clinicians and developers of asthma educational materials. Given that most experts believe that knowing the difference between rescue and controller medicines is a crucial topic in asthma education, this finding suggests interventions that are tailored to make teaching on this topic appealing and relevant to both youth and caregivers should be developed and tested.
We did not find that asthma topic preferences varied by youth or caregiver sociodemographic characteristics; that is, regardless of child and caregiver age, race, gender, or caregiver education or literacy level, they were interested in the same asthma topics. We are not aware of previous studies that have examined sociodemographic differences in asthma education preferences, but we were surprised that there were no age-related differences. We expected, for example, to find younger children to be more interested in talking to friends about asthma than adolescents because research shows teens with asthma report one of their biggest challenges is to be perceived as normal by their peers (32).
These findings, when taken together with existing research that identify parent/child knowledge gaps (23, 33) and research showing that clinicians and families think differently about asthma and asthma management, (24) highlight the potential for tailored education that addresses the knowledge deficits and education preferences of individual children and their caregivers. The inclusion of youth and caregiver specific interests and preferences will likely strengthen intervention successes. In keeping with current asthma guidelines (EPR 3) (5) that emphasize tailoring asthma self-management education to the needs of each patient and the proposed Healthy People 2020 goal to improve asthma education (34), these findings serve to heighten awareness of both youth and caregiver interests and preferences for asthma education topics. Our findings suggest the need for a larger scale study to further measure the perceived needs and preferences of youth with asthma and their caregivers and to evaluate if educational strategies attuned to the expressed preferences of youth and caregivers promote greater self-efficacy and more effective asthma management.
A strength of this study is that our enrolled sample included a large proportion of racial and ethnic minorities and low-income households - populations at greater risk for poor asthma outcomes. For example, the study sample contained a large proportion of Hispanics, a group not always touched by research efforts and existing healthcare services. Additionally, findings from this study capture a sizable number of caregivers identified with low literacy and research shows these individuals are especially receptive to video-based education (35). Finally, in addition to children, this sample contains adolescents, a group particularly at risk for poor asthma control (3).There are a limited number of educational materials and programs specifically targeting adolescents (36). Inadequate disease specific education is a barrier to adequate asthma management among ethnic minorities (37).
This study is not without limitations. We recruited a convenience sample of parent-child dyads from two pediatric clinics in a moderately populated county in North Carolina. While these clinics were selected because of our successful research track record together, because it was only two clinics and because they were part of the ENLaCE health research consortium, the sample may not be representative and results may not generalize to other pediatric care settings. The small sample size may have limited our ability to detect differences related to child and caregiver sociodemographic characteristics. We recognize that there are topics that were not asked about which would likely be of interest to patients and caregivers, however, the topics included in this study were selected from focus group data designed to identify important themes associated with asthma and asthma management from the patient’s perspective. No baseline measure of knowledge about these topics was administered which prevents our ability to consider the relationship between knowledge and interest. The RCT intervention video was designed specifically to illustrate proper medication techniques, and it is possible that participation in the intervention group may have biased children’s report of interest in the assessed video topics.
Conclusions/Key Findings
A considerable majority of youth with asthma and their caregivers in this sample had an interest in watching videos about practical aspects of asthma, including asthma management and medication use. Youth and caregiver topic interests differed in important ways, but the expressed interests of youth and caregivers was unrelated to sociodemographic factors. Children with asthma and their caregivers should be provided with information that addresses their educational preferences.
Managing asthma can be a challenging task and knowledge of various factors, such as how to deal with triggers and how to keep asthma under control, are essential components of asthma education efforts. It is vital to teach asthma management skills and asthma education to youth with asthma and their caregivers, so that they have the appropriate tools to manage asthma effectively. An important step in tailoring asthma education content is to take the expressed interests of caregivers and youth into account. Future studies should incorporate youth and caregiver preferences in the design and development of asthma education videos.
Acknowledgments
This pilot project was supported by Award Number ULTR000083 from the National Center for Advancing Translational Sciences. Dr. Carpenter’s salary was partially supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant KL2TR000084. We would like to acknowledge the ENLaCE Network for assistance with recruitment and Kristen Morella for her analytical support.
Footnotes
The authors report no conflicts of interest.
References
- 1.Centers for Disease Control and Prevention. Vital signs: asthma prevalence, disease characteristics, and self-management education: United States, 2001–2009. MMWR. Morbidity and mortality weekly report. 2011;60(17):547. [PubMed] [Google Scholar]
- 2.Price JH, Khubchandani J, McKinney M, Braun R. Racial/ethnic disparities in chronic diseases of youths and access to health care in the United States. Biomed Res Int. 2013 doi: 10.1155/2013/787616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Basch CE. Asthma and the achievement gap among urban minority youth. J Sch Health. 2011;81(10):606–13. doi: 10.1111/j.1746-1561.2011.00634.x. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. CDC’s national asthma control program: an investment in america’s health. 2013. [Google Scholar]
- 5.National Heart L, and Blood Institute. National asthma education and prevention program expert panel report 3 (EPR3): guidelines for the diagnosis and management of asthma. Bethesda, MD: US Department of Health and Human Services, National Institutes of Health, National Heart, Lung, and Blood Institute; 2007. [Google Scholar]
- 6.Guevara JP, Wolf FM, Grum CM, Clark NM. Effects of educational interventions for self management of asthma in children and adolescents: systematic review and meta-analysis. BMJ. 2003;326(7402):1308–9. doi: 10.1136/bmj.326.7402.1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahmad E, Grimes DE. The effects of self-management education for school-age children on asthma morbidity: a systematic review. J Sch Nurs. 2011;27(4):282–292. doi: 10.1177/1059840511403003. [DOI] [PubMed] [Google Scholar]
- 8.Kirk S, Beatty S, Callery P, Gellatly J, Milnes L, Pryjmachuk S. The effectiveness of self-care support interventions for children and young people with long-term conditions: a systematic review. Child Care Health Dev. 2013;39(3):305–24. doi: 10.1111/j.1365-2214.2012.01395.x. [DOI] [PubMed] [Google Scholar]
- 9.McDonald V, Gibson P. Asthma self-management education. Chron Respir Dis. 2006;3(1):29–37. doi: 10.1191/1479972306cd090ra. [DOI] [PubMed] [Google Scholar]
- 10.Ayala GX, Miller D, Zagami E, Riddle C, Willis S, King D. Asthma in middle schools: what students have to say about their asthma. J Sch Health. 2006;76(6):208–14. doi: 10.1111/j.1746-1561.2006.00098.x. [DOI] [PubMed] [Google Scholar]
- 11.Wilson EA, Makoul G, Bojarski EA, Bailey SC, Waite KR, Rapp DN, et al. Comparative analysis of print and multimedia health materials: a review of the literature. Patient Educ Couns. 2012;89(1):7–14. doi: 10.1016/j.pec.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 12.Soetens KC, Vandelanotte C, de Vries H, Mummery KW. Using online computer tailoring to promote physical activity: a randomized trial of text, video, and combined intervention delivery modes. J Health Commun. 2014;19(12):1377–92. doi: 10.1080/10810730.2014.894597. [DOI] [PubMed] [Google Scholar]
- 13.Massiah CA, Perren R, Michaels RE. Successfully supersizing marketing instruction: a comparison study of instructional delivery modes for principles of marketing to mega-class sizes. Atlantic Marketing Journal. 2014;3(2):5. [Google Scholar]
- 14.Armstrong AW, Idriss NZ, Kim RH. Effects of video-based, online education on behavioral and knowledge outcomes in sunscreen use: a randomized controlled trial. Patient Educ Couns. 2011;83(2):273–7. doi: 10.1016/j.pec.2010.04.033. [DOI] [PubMed] [Google Scholar]
- 15.Molyneaux H, O’Donnell S, Daniels B. Communicating health information with online videos. Canadian Communication Association Fredericton NewBrunswick. 2011 Jun 1–2; [Google Scholar]
- 16.Cho N, Chambers R. The potential of video in patient education post skin biopsies. University of Ottawa Journal of Medicine. 2014;4(2):32–5. [Google Scholar]
- 17.Sosin A. Asthma camp/education for living. J Asthma. 1991;28(5):357–68. doi: 10.3109/02770909109089463. [DOI] [PubMed] [Google Scholar]
- 18.Coppel JD, Gibson LL, Chodhari R, Wilson R. Methods and benefits of education in pediatric asthma. Clin Pulm Med. 2014;21(6):275–81. [Google Scholar]
- 19.Crow S, Ondrusek A. Video as a format in health information. Med Ref Serv Q. 2002;21(3):21–34. doi: 10.1300/J115v21n03_02. [DOI] [PubMed] [Google Scholar]
- 20.Tuong W, Larsen ER, Armstrong AW. Videos to influence: a systematic review of effectiveness of video-based education in modifying health behaviors. J Behav Med. 2014;37(2):218–33. doi: 10.1007/s10865-012-9480-7. [DOI] [PubMed] [Google Scholar]
- 21.Carpenter DM, Lee C, Blalock SJ, Weaver M, Reuland D, Coyne-Beasley T, et al. Using videos to teach children inhaler technique: a pilot randomized controlled trial. J Asthma. 2015;52(1):81–7. doi: 10.3109/02770903.2014.944983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boulet L-P, Chapman KR, Green LW, FitzGerald JM. Asthma education. CHEST Journal. 1994;106(4_Supplement):184S–96S. doi: 10.1378/chest.106.4_supplement.184s. [DOI] [PubMed] [Google Scholar]
- 23.Archibald MM, Scott SD. The information needs of North American parents of children with asthma: a state-of-the-science review of the literature. J Pediatr Health Care. 2014;28(1):5–13.e2. doi: 10.1016/j.pedhc.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 24.Yoos HL, Kitzman H, Henderson C, McMullen A, Sidora-Arcoleo K, Halterman JS, et al. The impact of the parental illness representation on disease management in childhood asthma. Nurs Res. 2007;56(3):167–74. doi: 10.1097/01.NNR.0000270023.44618.a7. [DOI] [PubMed] [Google Scholar]
- 25.Ingram DD, Franco SJ. NCHS urban-rural classification scheme for counties. Vital and health statistics. Series 2, Data evaluation and methods research. 2012;(154):1–65. [PubMed] [Google Scholar]
- 26.National Heart Lung and Blood Institute. Full report 2007, National Asthma Education and Prevention Program. US Department of Health and Human Services, National Institutes of Health; Expert panel report 3: guidelines for the diagnosis and management of asthma. [Google Scholar]
- 27.Cabana MD, Slish KK, Nan B, Clark NM. Limits of the HEDIS criteria in determining asthma severity for children. Pediatrics. 2004;114(4):1049–55. doi: 10.1542/peds.2003-1162-L. [DOI] [PubMed] [Google Scholar]
- 28.Morris NS, MacLean CD, Chew LD, Littenberg B. The Single Item Literacy Screener: evaluation of a brief instrument to identify limited reading ability. BMC Fam Pract. 2006;7(1):21. doi: 10.1186/1471-2296-7-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sleath B, Ayala GX, Davis S, Williams D, Tudor G, Yeatts K, et al. Child- and caregiver-reported problems and concerns in using asthma medications. J Asthma. 2010;47(6):633–8. doi: 10.3109/02770901003692785. [DOI] [PubMed] [Google Scholar]
- 30.Clark NM, Gong M, Kaciroti N. A model of self-regulation for control of chronic disease. Health Educ Behav. 2014;41(5):499–508. doi: 10.1177/1090198114547701. [DOI] [PubMed] [Google Scholar]
- 31.Deis JN, Spiro DM, Jenkins CA, Buckles TL, Arnold DH. Parental knowledge and use of preventive asthma care measures in two pediatric emergency departments. J Asthma. 2010;47(5):551–6. doi: 10.3109/02770900903560225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stewart M, Letourneau N, Masuda JR, Anderson S, Cicutto L, McGhan S, et al. Support needs and preferences of young adolescents with asthma and allergies: “Just no one really seems to understand”. J Pediatr Nurs. 2012;27(5):479–90. doi: 10.1016/j.pedn.2011.06.011. [DOI] [PubMed] [Google Scholar]
- 33.Elliott JP, Marcotullio N, Skoner DP, Lunney P, Gentile DA. Impact of student pharmacist-delivered asthma education on child and caregiver knowledge. Am J Pharm Educ. 2014;78(10) doi: 10.5688/ajpe7810188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.HealthyPeople.gov. Respiratory Diseases. Available from: http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=36; Accessed November 13, 2015.
- 35.Sobel RM, Paasche-Orlow MK, Waite KR, Rittner SS, Wilson EA, Wolf MS. Asthma 1-2-3: a low literacy multimedia tool to educate African American adults about asthma. J Community Health. 2009;34(4):321–7. doi: 10.1007/s10900-009-9153-9. [DOI] [PubMed] [Google Scholar]
- 36.Srof B, Taboas P, Velsor-Friedrich B. Adolescent asthma education programs for teens: Review and summary. J Pediatr Health Care. 2012;26(6):418–26. doi: 10.1016/j.pedhc.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 37.Rosser FJ, Forno E, Cooper PJ, Celedón JC. Asthma in Hispanics. An 8-Year Update. Am J Respir Crit Care Med. 2014;189(11):1316–27. doi: 10.1164/rccm.201401-0186PP. [DOI] [PMC free article] [PubMed] [Google Scholar]


