Norethindrone is the molecule that made Carl Djerassi famous. In 1951, the chemist, who died in January at the age of 91, and his team synthesized the compound, which would become a key ingredient in birth control pills.
Norethindrone was the first progestin, a synthetic version of a natural steroid hormone, progesterone. A few birth control pills contain only a progestin, while the rest combine a progestin and an estrogen analogue. In the more than 60 years since Djerassi’s landmark synthesis, drug makers have experimented with different formulations of oral contraceptives, including introducing new types of progestins and varying levels of estrogen. Their goal has been to maintain the Pill’s effectiveness, while reducing undesirable side effects.
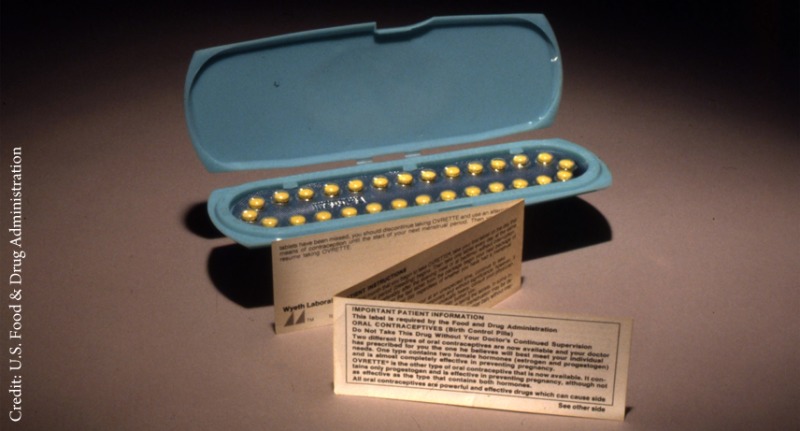
A pack of Orvetta birth control pills from 1970 contained a synthetic version of progesterone, a hormone that blocks ovulation.
Birth control pills work by essentially recapitulating the body’s natural response to pregnancy, says Diana L. Blithe of the National Institute of Child Health & Human Development. After ovulation and throughout pregnancy, the ovaries release a stream of estrogen and progesterone, which travels to receptors in the pituitary. This gland produces gonadotropins, hormones that stimulate ovulation; progesterone and, to a lesser extent, estrogen block the release of those signals, and thus ovulation. If a woman doesn’t become pregnant in that cycle, the ovaries stop releasing progesterone, and levels of the hormone drop precipitously, allowing the pituitary to release gonadotropins to orchestrate the next round of ovulation.
Progestins are the more active ovulation blockers; there are about 10 different progestins found in various birth control pills, each with a unique pharmacological profile. These are used in concert with one of two estrogen analogues ethinyl estradiol and estradiol valerate (which the liver metabolizes into estradiol). The estrogen also helps regulate the uterine lining to prevent breakthrough bleeding.
Scientists’ first attempts to create birth control pills focused on synthesizing progesterone from plant compounds. However, this approach failed to yield an effective oral medication. Progesterone is derived from cholesterol, making it a greasy molecule that doesn’t readily enter the bloodstream because it gets stuck in lipids in the intestines, Blithe says. When chemists synthesize progestins, they add hydrophilic functional groups to allow the molecules to leave the intestines and enter the bloodstream.
Oral availability was only the first pharmacological issue chemists faced. While all progestins inhibit ovulation by interacting with the progesterone receptor, progestins can also bind to receptors for other steroid hormones, such as the androgen and glucocorticoid receptors. These other interactions are responsible for the classic side effects of birth control pills. Androgen-like progestins can promote acne and reduce levels of high-density lipoprotein cholesterol, while glucocorticoid-like progestins can trigger retention of salt and water, leading to bloating.
Early progestins, such as norethindrone, were mainly derived from testosterone, an androgen, says Régine Sitruk-Ware of the Population Council, an international public health organization. These molecules were designed with a single goal: inhibit gonadotropin activity, even if that meant hitting other steroid receptors. The trend in birth control chemistry has been to try to avoid receptor promiscuity by synthesizing molecules more similar to progesterone than early generation progestins, Sitruk-Ware says. Although they successfully limit side effects, these newer progestins may lead to an increased risk of blood clots, though the data are mixed, she says.
Typically, blood clot risk has been associated with the estrogen component of birth control pills. Estrogen receptors in the liver are involved in the production of blood clotting factors. Ethinyl estradiol is much more potent than natural estradiol, and it remains in the body far longer, so it hyperactivates the liver pathway, creating conditions that promote blood clotting.
To decrease the risks of blood clots and other side effects, the dose of estrogen analogues in birth control pills has been gradually dropping over time, says Thomas D. Kimble of CONRAD, a nonprofit organization that conducts reproductive health research. “Formulations containing more than 50 μg of estrogen have not been available in the U.S. since 1988”, he says. For women who already have an increased risk of blood clots, birth control pills without ethinyl estradiol may, for now, be safer than combination pills, Blithe says, though effectiveness is a concern with these options. A possibly better choice, she says, would be to consider long-acting estrogen-free methods, such as intrauterine devices, which do not carry any increased risk of blood clots.
Blithe and others point out that chemists continue to work to reduce the risks associated with oral contraceptives. For example, Sitruk-Ware says there is emerging research on using an estrogen called estetrol that is made in the liver of fetuses. This hormone does not appear to stimulate the production of clotting factors in the liver. Researchers are also developing tissue-specific progestins that focus on receptors in the pituitary, says Donald P. McDonnell of Duke University. Progestins have been associated with a greater risk of certain cancers, such as breast cancer, possibly because they activate receptors in other tissues. A tissue-specific progestin, McDonnell says, may lower those risks.
The hope, Sitruk-Ware says, is that increasing birth control pill options will allow health care providers and their patients to select the best one for each woman’s particular risk factors.
The Pill beyond the Science
The Pill’s influence spreads far beyond chemistry, or even medicine. Three policy experts weigh in on the question: What has been the pill’s greatest impact on society?
Left to right: Claire D. Brindis, Elisha Dunn Georgiou, and Adam Sonfield.
Claire D. Brindis, director of the Philip R. Lee Institute for Health Policy Studies at the University of California, San Francisco:
The Pill was probably one of the most important chemical innovations in our lifetimes, having ramifications for generations of individuals. It doesn’t only affect the girl who is pregnant, but it affects her children. Unplanned pregnancies can trap families in a cycle of poverty. The ability to plan for and consider educational and employment opportunities changes the mindset of someone. Before the birth control pill, many of the decisions about whether to continue in school or pursue a career were not within the reach of the public. The freedom to make those decisions has been truly revolutionary.
Elisha Dunn Georgiou, vice president of programs at Population Action International, a research and advocacy organization focusing on global access to contraception:
The women reading this have two things in common: access to education and the ability to plan if and when they have children. Those are two things that get women to a different place in life, and we’ve arrived there because of the Pill. We’ve contributed to society in a way we would not have otherwise been able to. This is as true of a girl living in Washington, D.C., as a girl living in Zimbabwe. We talk a lot about education being a driver [for women’s success], but the number one reason women leave school, at least in the U.S., is because they get pregnant.
Adam Sonfield, senior public policy associate at the Guttmacher Institute, a nonprofit organization working to advance reproductive rights:
In addition to a wealth of social and economic benefits, the Pill has had substantial health impacts. The birth control pill stands alongside the polio vaccine [in terms of public health benefits]. Unplanned pregnancies and pregnancies close together in time can increase risk for preterm births and low birth weights. Contraception allows women to get healthy before becoming pregnant, to stop taking medications that may be dangerous during pregnancy, to start using folic acid, and to get into prenatal care. There is also evidence that women who planned for their pregnancies are more likely to take healthy steps, such as quitting smoking and drinking.
Erika Gebel Berg is a freelance writer for C&EN, the weekly newsmagazine of the American Chemical Society.
Correction: Updated May 1, 2015 to correct the statement that scientists did not extract progesterone directly from plants.
In collaboration with C&EN.



