Abstract
Background:
Preterm labor, which defines as live-birth delivery before 37 weeks of gestation is a main determinant of neonatal morbidity and mortality around the world.
Objective:
The aim of this study was to determine the prevalence of preterm labor in Iran by a meta-analysis study, to be as a final measure for policy makers in this field.
Materials and Methods:
In this meta-analysis, the databases of Thomson database (Web of Knowledge), PubMed/Medline, Science Direct, Scopus, Google Scholar, Iranmedex, Scientific Information Database (SID), Magiran, and Medlib were searched for articles in English and Persian language published between 1995 and 2014. Among the studies with regard to the inclusion and exclusion criteria, 14 studies (out of 1370 publications) were selected. Data were analyzed by using Stata software version 11. The heterogeneity of reported prevalence among studies was evaluated by the Chi-square based Q test and I2 statistics.
Results:
The results of Chi-square based on Q test and I2 statistics revealed severe heterogeneity (Q=2505.12, p-value < 0.001 and I2= 99.5%) and consequently, the random effect model was used for the meta-analysis. Based on the random effect model, the overall estimated prevalence of preterm in Iran was 9.2% (95% CI: 7.6 – 10.7).
Conclusion:
Present study summarized the results of previous studies and provided a comprehensive view about the preterm delivery in Iran. In order to achieve a more desirable level and its reduction in the coming years, identifying affecting factor and interventional and preventive actions seem necessary.
Key Words: Preterm labor, Prevalence, Meta-analysis, Iran
Introduction
Preterm labor, which defines as live-birth delivery before 37 completed weeks of gestation, is a main determinant of neonatal morbidity and mortality around the world (1, 2). Gestational age less than 28 weeks is defined as extremely preterm, 28 to <32 weeks as very preterm and 32 to <37 weeks as moderate to late preterm. Prematurity is the leading cause of babies' deaths in the first 4 weeks of life and the second leading cause of death after pneumonia in children under 5 years of age (3).
Despite advancing knowledge about risk factors and mechanisms of preterm labor, preterm birth rates are increasing in almost all countries and the development of public health and medical interventions designed to reduce preterm birth (2, 4, 5). Annually about 15 million babies are born prematurely and one million children die from complications of premature birth (3).
Hyaline membrane disease, bronchopulmonary dysplasia, patent ductus arteriosus, necrotizing enterocolitis and intraventricular hemorrhage are short-term complications of preterm birth, and neurological disorders such as cerebral palsy, hydrocephalus, seizures, vision and hearing disorders, and airway disorders are its main long-term complications (6). It should be mentioned that, about three-quarters of the deaths due to preterm birth complications, can be reduced even without neonatal intensive care (3).
Preterm birth is a syndrome with a variety of causes, which classified into: spontaneous preterm birth and provider-initiated preterm birth (7, 8). Previous preterm birth, black race, periodontal disease, and low maternal body-mass index are risk factors of spontaneous preterm births (2, 9, 10). Based on some studies in Iran, low general health status, history of disease during pregnancy, family history of prematurity, previous preterm labor, history of previous neonatal death, periodontal disease, decreased amniotic fluid, multiple pregnancies, infertility, and cervical incompetence were identified as risk factors of preterm labor (11-13).
Considering the importance of preterm birth, the latest statistics in a country can help plan the programs and introduction of guidelines for its reduction and control. On the other hand, due to multiplicity of studies, the need for an accurate and reliable result in this area seems essential.
Meta-analysis by combining results from different studies can increase the sample size, statistical power and precision and provide an overall quantitative result (14, 15). The aim of this study was to determine the prevalence of preterm labor in Iran by a meta-analysis study, to be as a final measure for policy makers in this field.
Materials and methods
This meta-analysis was conducted based on the relevant empirical literature about the prevalence of preterm delivery in Iran. The international databases, including Thomson (Web of Knowledge), PubMed/Medline, Science Direct, Scopus, Google Scholar, Iranmedex, Scientific Information Database (SID), Magiran, and Medlib were systematically searched for articles in English and Persian language published between 1995 and 2014.
The search was performed with all possible combinations of key words; Preterm labor, preterm birth, preterm delivery, and Iran. The search strategy was [“Preterm” OR “Preterm labor” OR “preterm birth” OR “Preterm delivery” AND “Iran”].
All English or Persian electronic letratures that studied the prevalence of preterm labor in each province of Iran were included. Studies in special populations such as employed women, studies in referral centers for high risk pregnancy, and duplicated articles were excluded.
The quality assessment of eligible papers has been followed independently by two researchers using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement (16), and probable disagreement between them resolved through discussion with a third researcher.
Statistical analysis
Data analysis were carried out by the Stata software version 11. Standard error in each study was calculated using the binomial distribution.
The heterogeneity of reported prevalence among studies was evaluated by the Chi-square based Q test and I2 statistics (with significant level of p< 0.1). Based on the rejection of homogeneity hypothesis, the random effect model was used for estimation of pooled prevalence.
Potential publication bias was examined by Begg's test and funnel plot. Also, meta-regression was used for examining the effects of potential factors contributing to the heterogeneity in the prevalence of preterm labor.
Results
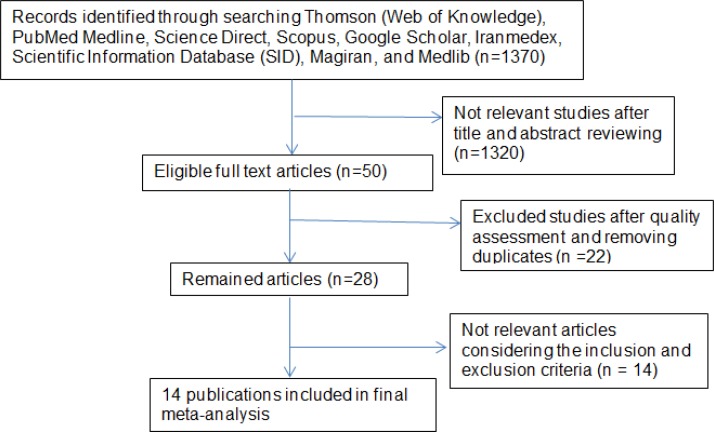
The first step of search in the mentioned databases yielded 1370 publications. In the second step, by reviewing the titles and abstracts, 50 studies were identified that were somewhat related. In the third step, after quality assessment of articles and removing duplicates, 28 studies remained. In the final step, considering the inclusion and exclusion criteria, 14 studies were selected for this meta-analysis (Table I, Figure1). The total sample size in the 14 study was 156461 people. Studies characteristics were entered in the meta-analysis are presented in table I. The highest prevalence of preterm labor was seen in Amini et al study in Tehran that it was equal to 30.4% (17) and the lowest prevalence was 2% in Kermanshah (18). This study was performed from 1995 to 2011. Based on the results of Begg's test, there was no evidence of publication bias (p=0.14).
Table I.
The characteristic of studies were included in the meta-analysis of preterm labor prevalence in Iran
| Reference | Year | Study location | Sample size (n) | Prevalence (%) |
|---|---|---|---|---|
| Afrakhteh M et al. (4) | 1995-1999 | Tehran | 5628 | 7.23 |
| Rajaeefard A et al. (19) | 2009 | Shiraz | 1117 | 8.3 |
| Lotf Alizadeh M et al. (20) | 2002-2003 | Mashhad | 1979 | 16.4 |
| Bayat-Mokhtary M et al. (21) | 2007 | Mashhad | 17129 | 6.1 |
| Ganji T et al. (22) | 2005 | Qom | 1237 | 13.9 |
| Khalaji Nia Z, Sadeghi Moghadam P. (23) | 2007 | Qom | 10913 | 5.6 |
| Marsusi V et al. (24) | 1996 | Tehran | 1969 | 9.43 |
| Sehati Shaghaie F et al. (25) | 2009 | Ardabil | 3575 | 13.4 |
| Sohrabi D, Ghanbari Gorkani M. (26) | 2007 | Zanjan | 4528 | 7.0 |
| Mansourghanaei M. (27) | 1999-2009 | Rasht | 62841 | 5.99 |
| Amini L et al. (17) | 2009 | Tehran | 990 | 30.4 |
| Alijahan R et al. (28) | 2010-2011 | Ardabil | 6705 | 5.1 |
| Pasdar Y et al. (18) | 2010 | Kermanshah | 32450 | 2.0 |
| Nabavizadeh SH et al. (12) | 2010 | Yasuj | 5400 | 2.4 |
Figure 1.
Flow diagram showing the different phases involved in searching for relevant publications
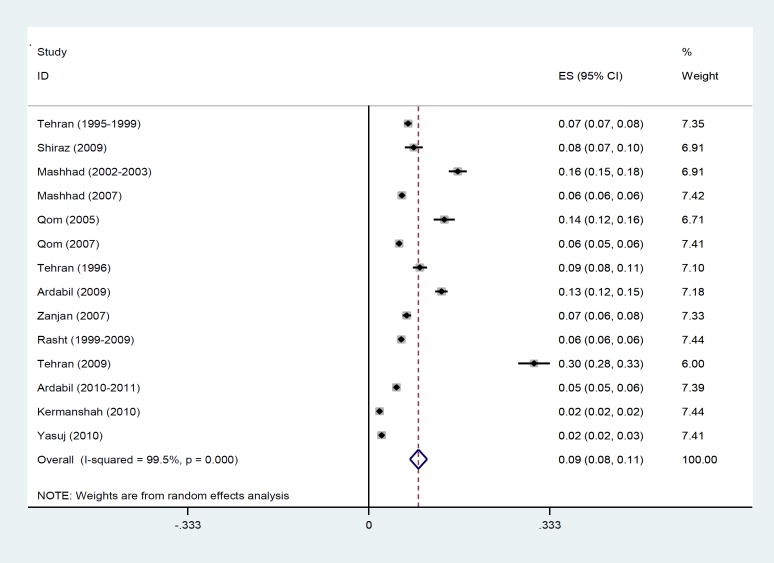
The results of Chi-square test based on Q test and I2 statistics showed severe heterogeneity among the reported prevalence (Q=2505. 12, p-value< 0.001 and I2= 99.5%) and consequently, the random effect model was used for the meta-analysis. The forest plot of eligible articles for estimating preterm labor prevalence in Iran is presented in figure 2. In this plot prevalence, 95% confidence interval (95% CI) and the weight assigned to each study is reported. The size of each square represents the weight of each study and the lines around it is the 95% CI. Based on the random effect model, the overall estimated prevalence of preterm in Iran was 9.2% (95% CI: 7.6 – 10.7).
Figure 2.
Forest plot of preterm labor prevalence in Iran using the random effect model
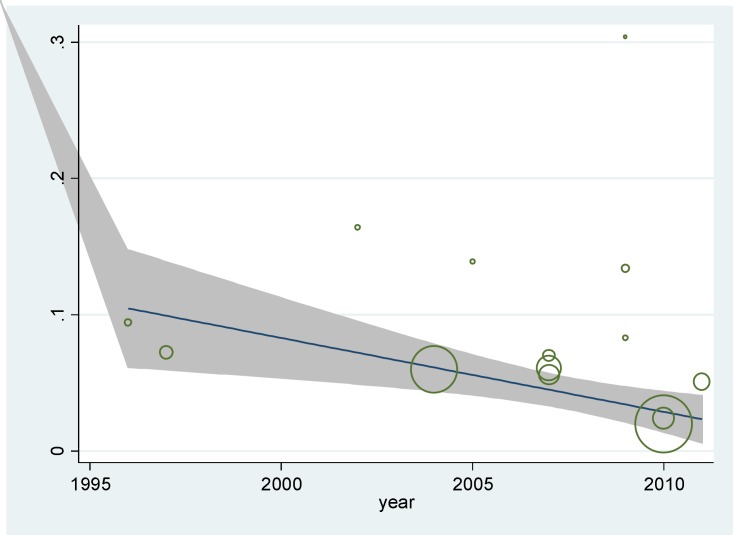
Meta-regression was used to study the effects of suspected factors in heterogeneity, including sample size and year of study (Table II). The results showed that in univariate model, preterm birth was reduced with increasing in sample size, but this was not significant statistically (p=0.19).
Table II.
The effects of suspected factors in heterogeneity
| Variable |
Univariate
|
Multivariate
|
||||
|---|---|---|---|---|---|---|
| Coefficient | SE | p-value * | Coefficient | SE | p-value * | |
| Sample size | -1.20 | 1.09 | 0.19 | -1.45 | 1.11 | 0.22 |
| Year of study | -0.0013 | 0.004 | 0.76 | -0.001 | 0.004 | 0.81 |
Note: Univariate and multivariate models meta regression
p-value < 0.05 considered significant
Also as shown in Figure 3, the prevalence of preterm labor was decreased over time, but this was not statistically significant as well (p=0.76).
Figure 3.
Meta-regression graph of preterm labor prevalence based on the year of study
In the multivariate model, the variables did not have a significant effect on the heterogeneity among studies (p> 0.05).
Discussion
In this study, the overall prevalence of preterm birth based on the results of 14 reviewed studies was estimated 9.2%. Since the meta-analysis use sample size of all studies, it provides a better estimation of the desired indicator (14, 15), therefor this overall indicator can be used in national health planning and policymaking.
Among all of the reviewed studies, the highest prevalence of preterm labor was reported in the study of Mirzaie and Mohammah-Alizadeh among pregnant women referring to the Delivery Ward of Afzalipour Hospital in Kerman (29). Since their study was not a community based on the study and it was not according to the researchers commenting, high prevalence in this study was due to the high rate of referrals from all parts of the province to this hospital for its facilities in having neonatal intensive care unit, therefore it was excluded this study from meta-analysis.
It can be concluded that, hospitals that have a high risk deliveries, the prevalence of preterm birth may be also higher. In contrast, unlike the previous study, which was conducted by Pasdar et al in Kermanshah on all pregnancies during the year, the lowest preterm prevalence was found (18).
Prevalence of preterm birth is different among regions and countries. Worldwide an estimated 11.1% of all live births were born preterm in 2010 (30). Also, based on the World Health Organization 2011 report, the prevalence of preterm delivery in 184 countries was between 5 to 18%, which 60% of these deliveries occurred in Africa and South Asia. In low-income countries, on average, 12% of babies are born prematurely; in contrast, this rate is 9% in high-income countries (3). However, in some high-income countries (such as the United States with 12% and Australia with 10.9%) premature birth is also considerable (7). In this study, the prevalence of preterm delivery was estimated slightly lower than low-income countries, and was similar to the high-income countries. Also, according to the latest reports, ten countries with the highest rates of preterm birth per 100 live births in the world consists of Malawi: 18.1, Comoros: 16.7, Congo: 16.7, Zimbabwe: 16.6, Equatorial Guinea: 16.5, Mozambique: 16.4, Gabon: 16.3, Pakistan: 15.8 and Mauritania: 15.4 (5, 7). The preterm birth rate has been reported 15.7% in Pakistan and 12.8% in Jordan (31, 32).
The results of this study showed that the prevalence of preterm delivery has reduced by increasing the sample size of studies, although were not statistically significant. These findings suggest that studies with low sample size may lead to kind of sampling bias from high-risk pregnancies. Therefor the appropriate sample size and sampling should be considered in these studies.
Based on the result of the present study, the prevalence of preterm birth has decreased over the time with a gentle slope. While based on the results of the Blencowe et al study, preterm delivery in 184 countries from 1990 to 2010, only 3 countries had a decreasing trend, 14 countries had stable rate and all others showed an increasing trend during 20 years (7). Although the reduction in preterm birth during almost 15 years of our study was not statistically significant, but this slight reduction is probably due to the desirable reproductive health or health education programs (33, 34). The main limitation of this study was that it could not classified studies by age-groups, because of the different age distributions of subjects in eligible studies.
Conclusion
Finally, it can be concluded that the present systematic review and meta-analysis summarized the results of previous studies and provided a comprehensive view about the preterm delivery in Iran. Although compared to the developing countries, this prevalence of preterm delivery is acceptable in Iran, but in order to achieve a more desirable level and reduce the rate in the coming years, identifying affecting factors and interventional and preventive actions seem necessary.
Acknowledgments
There were no sources of financial support (personal support).
Conflict of interest
The authors have declared that there is no conflict of interest in this study.
References
- 1.Nguyen N, Savitz DA, Thorp JM. Risk factors for preterm birth in Vietnam. Int J Gynaecol Obstet. 2004;86:70–78. doi: 10.1016/j.ijgo.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 2.Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. The lancet. 2008;371:75–84. doi: 10.1016/S0140-6736(08)60074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Howson C, Kinney M, Lawn J. Born too soon: the global action report on preterm birth 2012. [[cited November 2014]]. Available from: http://www.who.int/maternal_child_adolescent/documents/born_too_soon/en/index.html.
- 4.Afrakhteh M, Ebrahimi S, Valaie N. Prevalence of preterm delivery and its related factors in females referring to Shohada Tajrish Hospital, 1995-99. Pejouhandeh. 2002;7:341–344. [Google Scholar]
- 5.Preterm birth: World Health Organization. 2014. [[cited November 2014]]. Available from: http://www.who.int/mediacentre/factsheets/fs363/en/.
- 6.Moghadami N, Aminikhah B, Davari Tanha F. The effect of maternal body mass index on spontaneous versus induced preterm birth: a prospective study. Tehran univ Med J. 2009;67:221–225. [Google Scholar]
- 7.Blencowe H, Cousens S, Oestergaard MZ, Chou D, Moller AB, Narwal R, et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet. 2012;379:2162–2172. doi: 10.1016/S0140-6736(12)60820-4. [DOI] [PubMed] [Google Scholar]
- 8.Murphy DJ. Epidemiology and environmental factors in preterm labour. Best Pract Res Clin Obstet Gynaecol. 2007;21:773–789. doi: 10.1016/j.bpobgyn.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 9.Lo CC, Hsu JJ, Hsieh CC, Hsieh TT, Hung TH. Risk factors for spontaneous preterm delivery before 34 weeks of gestation among Taiwanese women. Taiwan J Obstet Gynecol. 2007;46:389–394. doi: 10.1016/S1028-4559(08)60008-X. [DOI] [PubMed] [Google Scholar]
- 10.Martius JA, Steck T, Oehler MK, Wulf K-H. Risk factors associated with preterm (< 37+ 0 weeks) and early preterm birth (< 32+ 0 weeks): univariate and multivariate analysis of 106 345 singleton births from the 1994 statewide perinatal survey of Bavaria. Euro J Obstet Gynecol Reprod Biol. 1998;80:183–189. doi: 10.1016/s0301-2115(98)00130-4. [DOI] [PubMed] [Google Scholar]
- 11.Derakhshi B, Esmailnasab N, Ghaderi E, Hemmatpour S. Risk factor of preterm labor in the west of iran: a case-control study. Iran J Public Health. 2014;43:499–506. [PMC free article] [PubMed] [Google Scholar]
- 12.Nabavizadeh SH, Malekzadeh M, Mousavizadeh A, Shirazi HR, Ghaffari P, Karshenas N, et al. Retrospective study of factors related to preterm labor in Yasuj, Iran. Int J Gen Med. 2012;5:1013–1017. doi: 10.2147/IJGM.S33385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khadem N, Rahmani ME, Sanaei A, Afiat M. Association between preterm and low-birth weight with periodontal disease: a case-control study. Iran J Reprod Med. 2012;10:561–566. [PMC free article] [PubMed] [Google Scholar]
- 14.Cohn LD, Becker BJ. How meta-analysis increases statistical power. Psychol Methods. 2003;8:243–253. doi: 10.1037/1082-989X.8.3.243. [DOI] [PubMed] [Google Scholar]
- 15.Noble JH Jr. Meta-analysis: methods, strengths, weaknesses, and political uses. J Lab Clin Med. 2006;147:7–20. doi: 10.1016/j.lab.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 16.Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Preventive Medicine. 2007;45:247–251. doi: 10.1016/j.ypmed.2007.08.012. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies*. [DOI] [PubMed] [Google Scholar]
- 17.Amini L, Mahmoudi Z, Hosseini F, Mahmoudi A. The relationship between the social structure and health and pregnancy outcomes: preterm labor and rupture of water bag. Journal of Sabzevar University of Medical Sciences. 2013;20:109–116. [Google Scholar]
- 18.Pasdar Y, Heidari N, Safari Y, Faramani RS, Izadi N, Jamshidpour M, et al. Prevalence of Some Risk Factors in Pregnant Women. Iran J Obstet Gynecol Infertil. 2012;15:14–23. [Google Scholar]
- 19.Rajaeefard A, Mohammadbeigi A, Mohammadi M, Joulaee H, Alipour H. Evaluation of risk factors in preterm delivery and impact of education in its prevention. Daneshvar Medicine. 2010;17:11–18. [Google Scholar]
- 20.Lotf Alizadeh M, Mohammadzadeh A, Kamandi S, Bagheri S. Prevalence and risk factors of preterm labor in Imam Reza Hospital 2003-2004. Iranian Journal Of Obstetrics, Gyneocology And Infertility. 2005;8:93–100. [Google Scholar]
- 21.Bayat–Mokhtary M, Tabrizian F, Dolatabady E, Khalesian B. Analysis of some maternal risk factors in preterm delivery (in Persian) Journal of Medical Science of Islamic Azad University of Mashhad. 2009;5:140–146. [Google Scholar]
- 22.Ganji T, Einipour Z, Hosseini F. The relationaship of pre-term delivery and stressful life events during pregnancy. IJN. 2009;22:77–86. [Google Scholar]
- 23.Khalaji Nia Z, Sadeghi Moghadam P. Prevalence and maternal risk factors of preterm laboring in Qom, 2007. Qom University of Medical Sciences Journal. 2011;5:30–36. [Google Scholar]
- 24.Marsusi V, Rasekh K. Etiology and prevalence of preterm deliveries in Dr. Shariatie Hospital, 1996-97. Tehran univ med J. 1998;56:31–34. [Google Scholar]
- 25.Sehati Shaghaie F, Ghuchazade M, Asdolaie M, Farzolapur F. Prevalence and Risk Factors of Preterm labor in Health Education Centers of Ardabil Province (2009-2010) Life Science Journal. 2013;10:231–236. [Google Scholar]
- 26.Sohrabi D, Ghanbari Gorkani M. A survey on risk factors and outcomes of women with preterm labor admitted to Valieasr hospital in Zanjan. Journal of Urmia Nursing And Midwifery Faculty. 2011;9:84–89. [Google Scholar]
- 27.Mansourghanaei M. Seasonal Pattern of Preterm Birth. Journal of Guilan University of Medical Sciences. 2011;20:77–83. [Google Scholar]
- 28.Alijahan R, Hazrati S, Mirzarahimi M, Pourfarzi F, Ahmadi Hadi P. Prevalence and risk factors associated with preterm birth in Ardabil, Iran. Iran J Reprod Med. 2014;12:47–56. [PMC free article] [PubMed] [Google Scholar]
- 29.Mirzaie F, Mohammah-Alizadeh S. Contributing factors of preterm delivery in parturient in a University Hospital in Iran. Saudi Med J. 2007;28:400–404. [PubMed] [Google Scholar]
- 30.Blencowe H, Cousens S, Chou D, Oestergaard M, Say L, Moller A-B, et al. Born too soon: the global epidemiology of 15 million preterm births. Reprod Health. 2013;10:S2. doi: 10.1186/1742-4755-10-S1-S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gulamani SS, Premji SS, Kanji Z, Azam SI. A review of postpartum depression, preterm birth, and culture. J Perinat Neonatal Nurs. 2013;27:52–59. doi: 10.1097/JPN.0b013e31827fcf24. [DOI] [PubMed] [Google Scholar]
- 32.Mohammad K, Abu Dalou A, Kassab M, Gamble J, Creedy DK. Prevalence and factors associated with the occurrence of preterm birth in Irbid governorate of Jordan: a retrospective study. Int J Nurs Pract. 2014:11. doi: 10.1111/ijn.12335. doi: 10.1111/ijn.12335. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 33.Vakilian K, Mirzaii K, NajmAbadi Reproductive health in iran: international conference on population and development goals. Oman Med J. 2011;26:143–147. doi: 10.5001/omj.2011.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Khorsandi M, Vakilian K, Torabi Goudarzi M, Abdi M. Childbirth preparation using behavioral-cognitiveskill in childbirth outcomes of primiparous women. JBUMS. 2013;15:76–80. [Google Scholar]