Abstract
Objective. To develop, implement, and evaluate a targeted educational module on tuberculosis screening with second-year professional pharmacy students that improves their knowledge, skills, and attitudes regarding tuberculosis screening.
Design. A tuberculosis-screening educational module was developed in collaboration with the Washington State Pharmacy Association and Department of Health and incorporated in a core student pharmacist class. Students completed online didactic training and a live practicum, each lasting 90 minutes.
Assessment. Students were assessed using a pre/postdidactic assessment, live practicum tuberculin skin testing (TST) administration and evaluation assessment, and postprogram written reflection. Student pre/postknowledge assessment scores improved in all areas except in documentation.
Conclusion. The tuberculosis screening educational module significantly improved student knowledge, skills, and attitudes regarding tuberculosis screening.
Keywords: tuberculin test, students, pharmacy, tuberculosis, screening
INTRODUCTION
Tuberculosis (TB) is second only to HIV/AIDS as the greatest killer worldwide as a result of a single infectious agent. It is estimated that one third of the world’s population has latent TB.1 In 2012, there were more than 10 000 reported cases of active TB in the United States, and the Centers for Disease Control estimates that 11 million have latent TB.2,3 For more than 40 years, an important tuberculosis control measurement in the United States has been the identification and treatment of persons with latent Mycobacterium tuberculosis infection. Tuberculin skin testing (TST) is the most commonly used method of latent tuberculosis screening in the United States.4 The World Health Organization’s Stop TB Strategy highlights the importance of engaging “all care providers” to dramatically reduce TB by “public and private actions at national and local levels.”1
Pharmacists are positioned to serve their communities on a local level by providing TST in appropriate patient populations. Pharmacies are located directly in communities and can access a wide spectrum of patients, particularly those at high risk for latent TB. Many pharmacies have “open door” policies that allow patients direct access, often without requiring appointments. Additionally, pharmacies are often open at times that are more convenient for patients (some 24 hours a day and on weekends).
As seen with immunization initiatives, pharmacists are willing and capable of providing public health services.5 Two pharmacists in a grocery store pharmacy setting over 10 months demonstrated ability to assess appropriate patients, administer TST, and interpret TST results.6 Moreover, pharmacists in New Mexico demonstrated pharmacist-administered TST had high follow-up rates.7
King County, where the University of Washington School of Pharmacy resides, reports around 150 cases of tuberculosis annually.8 Changes in King County public health funding and policies created concerns of decreased access to TB screening. To help meet the public health needs of the community, the School of Pharmacy partnered with the Washington State Pharmacy Association and Washington State Department of Health to develop a TB training certificate program for pharmacists and student pharmacists to help increase access to TB screening in King County and the surrounding region.
Training students in tuberculosis-screening as part of the core curriculum at the school was important for several reasons. First, to the authors’ knowledge, this was the first tuberculosis-screening certification developed and administered to pharmacy students. Second, the TB training certificate program strengthened the school’s commitment to the 2013 Center for the Advancement of Pharmaceutical Education (CAPE) Outcomes. In particular, CAPE Outcome 2.3 (Health and Wellness) was addressed by preparing students to design and implement an intervention to improve public health. Outcome 4.3 (Innovation and Entrepreneurship) was reinforced by helping students develop new approaches to improve patient care in a potentially entrepreneurial fashion.9
Third, the TB training certificate program aligned with the school’s mission and strategic action plan. Included in the action plan is the school’s educational philosophy statement that says, “The goal of the PharmD program is to ensure our graduates possess the knowledge, skills, and abilities necessary to render care in an evolving healthcare system . . . Students are also encouraged, through professional and community outreach activities, to develop and incorporate new practices that enhance public health, systems management, and patient-centered care in diverse populations and settings.”10 Thus, training students in a novel intervention to enhance public health coordinates with the educational philosophy of the school.
The tuberculosis screening educational module was designed to train on the placement and assessment of TST. The content was developed in coordination with the Washington State Department of Health TB Services Program and the Washington State Pharmacy Association. It was hypothesized that training and certification in TB screening would increase student pharmacist willingness to provide TST in their future practice.
DESIGN
The Student Pharmacists as Tuberculosis Screeners (SPATS) program was developed to improve students’ knowledge, skills, and attitudes regarding tuberculosis screening. It was developed in concert with the Washington State Pharmacy Association’s pharmacist TB screening program and is similar in design. It differed in that the SPATS program included a web-based didactic component and occurred over two weeks, while the pharmacist TB screening program was live and occurred over a single day. The specific objectives were to: (1) apply therapeutics infectious disease knowledge to tuberculosis screening (knowledge); (2) identify appropriate patients for TST (knowledge); (3) describe TST procedures (knowledge); (4) perform proper administration of a TST (skills); (5) review alternative tuberculosis screening methods (knowledge); (6) accurately evaluate TST results for a variety of patient scenarios (skills); (7) assess a patient for potential false negative TST reaction (skills); and (8) increase comfort and willingness to perform TST in future pharmacy practice (attitude). The study was approved by the institutional review board (IRB) at the University of Washington.
The SPATS program was conducted in spring quarter 2014 as part of the professional pharmacy curriculum at the school. It was implemented in Applied Therapeutics I, a skills-based course taught in tandem with the therapeutics lecture series. Applied Therapeutics I is a 2-credit core pharmacy course offered in the second-year that features a lecture and skills session. The course focuses on application of therapeutics principles, adjustment of therapy to disease-specific and patient-specific characteristics, physical examination and assessment skills, and communication. Just after the SPATS program, students received 180 minutes of didactic training on the epidemiology, pathophysiology, and treatment of tuberculosis as part of their core therapeutics course. The program was strategically placed in Applied Therapeutics I because SPATS coordinated with tuberculosis didactic teaching in the therapeutics lecture series, built upon previous physical assessment training, scaffolded on previous intramuscular and subcutaneous injection technique, and occurred after the community introductory pharmacy practice experience. Applied Therapeutics I is taught by a team of five part-time clinical faculty members. In addition to the Applied Therapeutics I faculty members, two nurses from the Washington State Department of Health and a pharmacist from the Washington State Pharmacy Association were enlisted for the SPATS program. All parties had previously been trained and certified in tuberculosis screening.
SPATS training for 96 second-year professional pharmacy students occurred over two weeks. The training consisted of pre-assessment, tuberculosis and TST didactic (90 minutes), compulsory postdidactic assessment, practicum with live assessment (90 minutes), and written reflection. Because the pre-assessment was not part of the school’s standard teaching methods and protocol, it was voluntary to remain in accordance with IRB recommendations. The postdidactic assessment, which was part of standard teaching methods and protocol, contributed to students’ overall grade and was compulsory.
The 90-minute web-based lecture was made available to students two weeks prior to the practicum with live assessment. The didactic described appropriate patients for TST, proper administration of a TST, alternate tuberculosis screening methods, examples of TST results, and the Center for Disease Control’s Mantoux Tuberculin Skin Test podcast. The postdidactic assessment was administered online and consisted of questions that directly assessed learning objectives 1, 2, 3, and 5. In order to progress to the practicum, students needed to exhibit mastery of the information by correctly answering all questions on the postdidactic assessment. Data presented here includes postdidactic assessment results from students’ first attempt. Students who did not correctly answer all questions on their first attempt met with course instructors for further teaching and were given an additional opportunity to take the postdidactic assessment. Students were required to participate in the didactic training and complete the compulsory postdidactic assessment three days prior to the practicum, leaving sufficient time for instructors to assess whether students exhibited mastery.
The practicum took place in the Bracken Pharmacy Learning Center, a space dedicated to teaching pharmacy skills located on the school’s campus. Several weeks prior to the practicum, students self-selected time slots in groups of 16. Each slot lasted for 90 minutes, and students were only required to attend their assigned time. The first portion of the practicum was 45 minutes long. This portion began with a 10-minute review of TST administration. Students then partnered and practiced TST administration on each other using tuberculin syringes filled with normal saline. Once students felt competent with administration, they completed a TST with an instructor assessing their technique. All students were required to complete the assessment.
The second portion of the practicum was 45 minutes long and was devoted to TST evaluation, including false negative TST reactions. The first five minutes were used to review TST positive and negative reactions based on patient-specific characteristics. Basics in induration measurement were reinforced. Students practiced TST measurements and evaluation using four patient cases with tuberculin testing demonstration arms. Students subsequently completed a case-based assessment that required identification of appropriate patients for TST, accurate measurement of TST results, and correct assessment of their measurement results. In order to receive SPATS certification, students had to exhibit mastery of the practicum portion by correctly answering all questions. Students who did not correctly answer all questions were required to spend extra time reviewing materials with course instructors and given an additional opportunity to take the postdidactic assessment. After completion of the SPATS program, students were required to reflect upon their experiences.
The development phase of the SPATS program was approximately 24 hours, including the creation of the web-based didactic portion. The live practicum and assessment totaled 10 hours, with each 90-minute session having 16 students. Instructor team debriefing took one hour. Postassessment was approximately two hours.
EVALUATION AND ASSESSMENT
The effectiveness of the SPATS program was evaluated by quantitatively assessing student achievement of learning objectives using traditional and nontraditional assessment tools such as an online pre/postdidactic assessment, live TST administration practical assessment, and live TST evaluation assessment; gauging comfort and willingness to perform TST using pre/postdidactic surveying; and qualitatively assessing program with a postprogram reflection exercise.
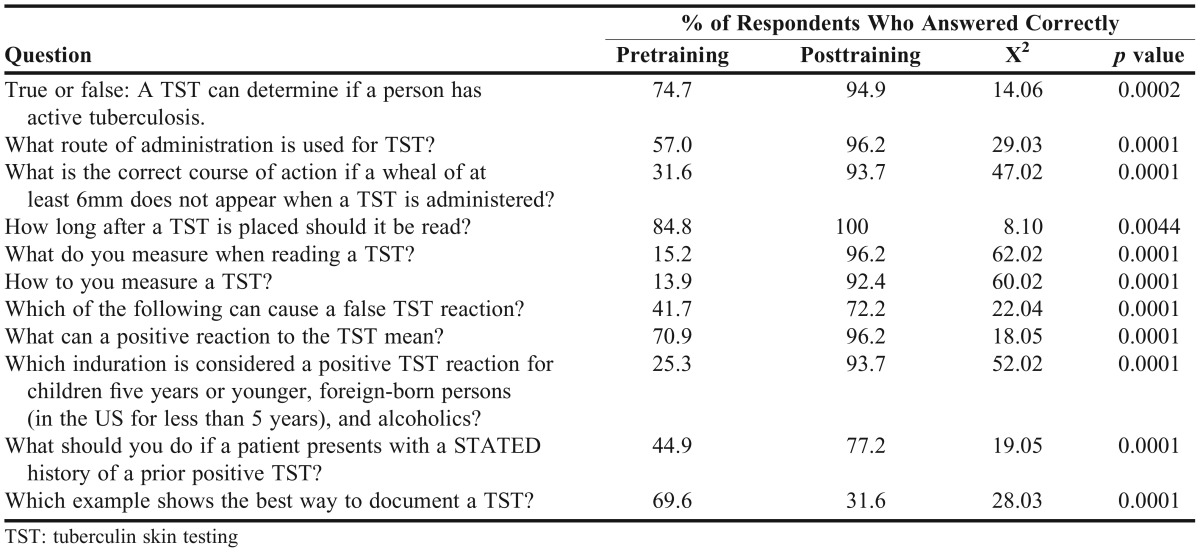
Ninety-six students were enrolled in the course that included the SPATS program. Seventy-nine students completed the pre-assessment and post-assessment (82.3% response rate). Student knowledge about tuberculosis screening was evaluated using paired, pre/post design. Average knowledge quiz scores were compared at baseline and after completion of the SPATS training using a paired t test. Before any SPATS training, the mean pre-assessment score was 48.7 % (SD=1.7%). After the didactic portion, the postassessment mean score was 86.5% (SD = 5.5%). Changes in mean scores were significant (p<0.05). Thirty-eight students needed to meet with course instructors to receive further teaching and successfully retake the assessment. Item analysis comparing the pre/post results was done using a McNemar test (Table 1). Students scored significantly better on the posttest for items 1 through 10 (p<0.05). Students scored significantly worse on the posttest for item 11 (p<0.05). Of the 79 students who completed the pre-assessment, postassessment, and live TST administration and evaluation practical assessment, 70 students successfully completed on their first attempt. Two students needed to repeat TST administration. Seven students needed to repeat the evaluation.
Table 1.
Item Analysis of Knowledge Assessment (n=79)
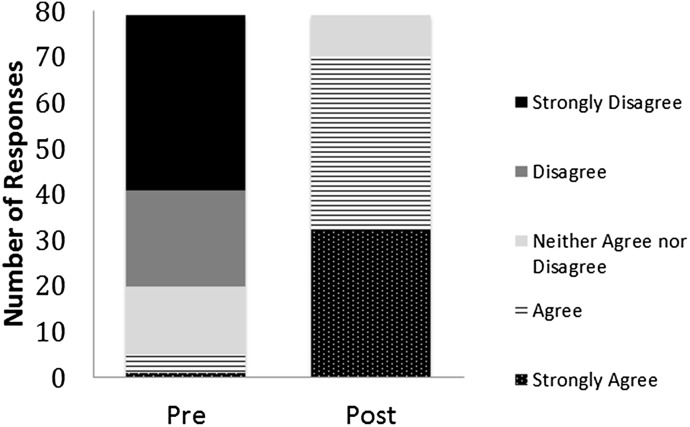
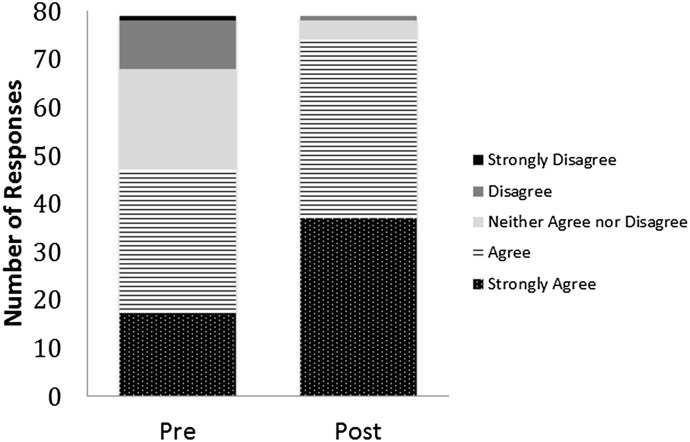
Seventy-nine students completed the comfort and willingness survey before and after the SPATS program (82.3% response rate). Comfort and willingness was gauged using a 2-item questionnaire with a 5-point Likert scale (1=strongly disagree, 2=disagree, 3=neither agree nor disagree, 4=agree, 5=strongly agree). Change in comfort and willingness was assessed using the Wilcoxan signed-rank test based on the paired nature of the data. Comfort in performing TST improved from a mean of 1.9 (1.0) at baseline to 4.3 (0.7) after completion of the SPATS program (p<0.001). Willingness to perform TST improved from a mean of 3.7 (1.00) pre-SPATS training to 4.4 (0.7) posttraining (p<0.001). Distribution of responses for comfort and willingness are presented in Figures 1 and 2, respectively.
Figure 1.
Student Attitude toward Statement - “I am Comfortable Performing Tuberculin Skin Testing”.
Figure 2.
Student Attitude toward Statement “I am Willing to Perform Tuberculin Skin Testing”.
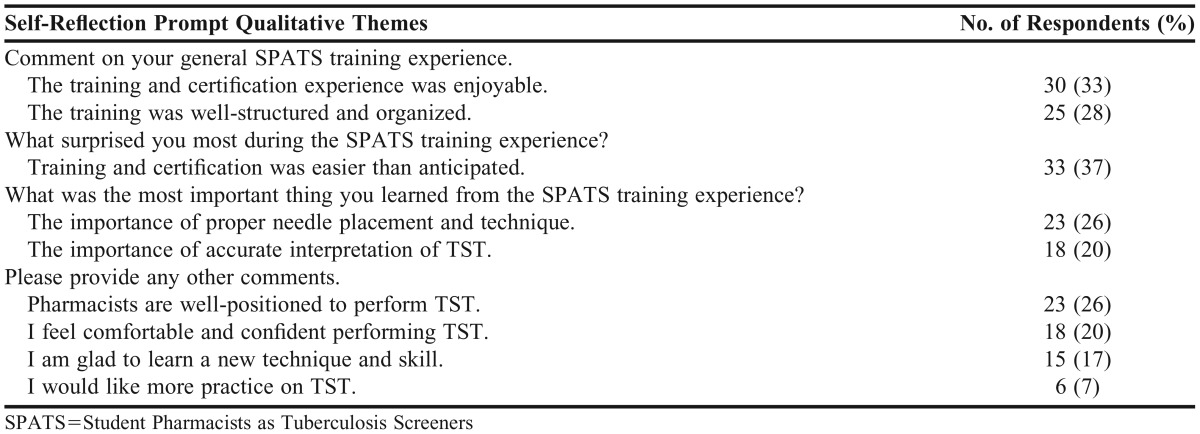
An anonymous reflection survey was used to qualitatively evaluate the SPATS training program. Data was collected for all second-year professional pharmacy students at the conclusion of the SPATS program. Reflection surveys were administered via Canvas Quiz (Instructure, Salt Lake City, UT). Ninety students completed reflection surveys (94% response rate). The reflection consisted of open-ended questions based on the learning outcomes from the SPATS program and input from faculty members. Content validity was tested by sending the reflection to faculty members prior to student use. The open-ended reflection allowed students to express their opinions on TST and their SPATS training. Two faculty members assessed student evaluations using thematic analysis to independently identify emergent themes in response to the reflection prompts. Once identified, themes were adjudicated between the faculty members to achieve agreement and coding for analysis. Key qualitative themes are presented in Table 2.
Table 2.
Self-Reflection Thematic Analysis Results (n=90)
DISCUSSION
The SPATS program was a novel training experience for University of Washington School of Pharmacy students. This study investigated whether SPATS program completion would improve student’s knowledge, skills, and attitudes regarding tuberculosis screening. The design of the study allowed for paired comparisons before and after program completion.
The SPATS program significantly improved student knowledge regarding tuberculosis screening, as made evident by pre/postknowledge assessment scores. Based on item analysis, students significantly improved in application of therapeutics infectious disease knowledge, identification of appropriate patients for TST, description of TST procedures, selection of alternative tuberculosis screening methods, and assessment of potential false negative TST reactions. The only item students did not improve on dealt with appropriate TST documentation.
Qualitative themes that emerged from thematic self-reflection analysis revealed that students enjoyed the SPATS training and certification experience and felt the program was well structured and organized. Many students entered the SPATS training program feeling nervous and apprehensive and were surprised that training and certification were easier than anticipated. Students felt the most important things they learned from the SPATS program were proper intradermal injection technique and accurate TST interpretation. A general theme that emerged in student comments was that pharmacists were well positioned as health care providers to perform TST. Six students noted they would like more practice on TST.
A number of factors made the SPATS training successful. Thoughtful and supportive collaboration with the Washington State Department of Health and the Washington State Pharmacy Association emphasized to students the importance of the SPATS training. The deliberate coordination of the SPATS program with therapeutics lectures on tuberculosis helped pique interest and reinforce learning. Timing the training to scaffold on previous intramuscular and subcutaneous injection training may have helped students feel more prepared and confident when learning intradermal injections. Presenting the didactic portion with web-based technology allowed students to learn and review key materials on demand. Using live classroom time for “just in time” learning and the practicum with assessment helped maximize student engagement and learning. The postdidactic assessment and written reflection allowed students and faculty members to assess SPATS program effectiveness.
There are several areas in which the SPATS program could improve. Several students reported the Center for Disease Control’s Mantoux Tuberculin Skin Test podcast only included audio (and not video). Faculty members tested the podcast on several computers using various web browsers and did not find this to be the case. However, further inquiry into different device and browser requirements for proper podcast viewing should occur. Eight different tuberculin testing demonstration arms were used for TST evaluation during the live practicum. Half of the arms were more realistic than the other half in terms of build, color, and induration. Having all demonstration arms be of superior quality could provide more consistent and realistic training for students. As noted in the written reflection analysis, some students desired more time to practice TST intradermal injections. In future SPATS trainings, additional practice opportunities should be made available to interested students.
SUMMARY
The SPATS program was developed to improve student’s knowledge, skills, and attitudes regarding tuberculosis screening. The SPATS program significantly improved students’ knowledge regarding TST in all areas except documentation. Student skill in tuberculosis screening also improved. There was a significant positive change in students’ survey responses regarding attitude and willingness to perform TST. Students reflected that SPATS training was enjoyable, well-structured and organized, and easier than anticipated. Students also noted that pharmacists are well positioned to perform TST. While there are areas for improvement, the SPATS program was successful in its goals.
ACKNOWLEDGMENTS
The author would like to thank Julie Tomaro and the Washington State Department of Health for their dedication, support, and collaborative spirit. The Washington State Pharmacy Association was instrumental in the development of the SPATS program and their enthusiasm was greatly appreciated. The Applied Therapeutics I faculty members were open and supportive of piloting a new training program. Sellyna Ehlers provided administrative support and ensured needed supplies were available. The authors would also like to acknowledge the pharmacy students involved for their willingness and constructive feedback. The ideas expressed in this manuscript are those of the authors and in no way are intended to represent the position of the Washington State Department of Health, the Washington State Pharmacy Association, or the University of Washington School of Pharmacy.
REFERENCES
- 1.Tuberculosis Fact Sheet. World Health Organization. http://www.who.int/mediacentre/factsheets/fs104/en/index.html. Accessed March 4, 2015.
- 2.TB Trends Fact Sheet. Centers for Disease Control and Prevention. http://www.cdc.gov/tb/publications/factsheets/statistics/TBTrends.htm. Accessed May 30, 2014.
- 3. Latent Tuberculosis Infection: A Guide for Primary Health Care Providers. Centers for Disease Control and Prevention. http://www.cdc.gov/tb/publications/ltbi/intro.htm. Accessed September 15, 2015.
- 4.American Thoracic Society. Targeted tuberculin testing and treatment of latent tuberculosis infections. Am J Respir Crit Care Med. 2000;161:S221–S247. doi: 10.1164/ajrccm.161.supplement_3.ats600. [DOI] [PubMed] [Google Scholar]
- 5.Hogue MD, Grabenstein JD, Foster SL, Rothholz MC. Pharmacist involvement with immunizations: a decade of professional advancement. J Am Pharm Assoc. 2006;46(2):168–179. doi: 10.1331/154434506776180621. [DOI] [PubMed] [Google Scholar]
- 6.Hecox N. Tuberculin skin testing by pharmacists in a grocery store setting. J Am Pharm Assoc. 2008;48(1):86–91. doi: 10.1331/JAPhA.2008.07016. [DOI] [PubMed] [Google Scholar]
- 7.Jakeman B, Gross B, Fortune D, Babb S, Tinker D, Bachyrycz A. Evaluation of a pharmacist-performed tuberculosis testing initiative in New Mexico. J Am Pharm Assoc. 2015;55(3):307–312. doi: 10.1331/JAPhA.2015.14141. [DOI] [PubMed] [Google Scholar]
- 8.Frequently asked questions about tuberculosis. King County Department of Health. http://www.kingcounty.gov/healthservices/health/communicable/TB/faq.aspx. Accessed March 4, 2015.
- 9.Medina MS, Plaza CM, Stowe CD, et al. Center for the Advancement of Pharmacy Education (CAPE) 2013 Educational Outcomes. Am J Pharm Educ. 2013;77(8):Article 162. doi: 10.5688/ajpe778162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mission,vision, and core values. University of Washington School of Pharmacy. http://sop.washington.edu/about/mission-and-vision/. Accessed June 22, 2015.