Abstract
Objective. To examine the effectiveness of simulated learning modules (SLMs) encompassing EXcellence in Cultural Experiential Learning and Leadership (EXCELL) core competencies in enhancing pharmacy students’ professional communication skills.
Methods. Students completed three hours of preparatory lectures and eight hours of workshops comprising six SLMs themed around pharmacy practice and pharmacy placements. Each SLM comprised role-plays with actors, facilitation using EXCELL Social Interaction Maps (SIMs), and debriefing. Evaluations of SLMs included quantitative and qualitative survey responses collected before, during and after workshops, and after placements. Facilitators reflected on SLMs as a pedagogic modality.
Results. Student feedback was positive about SLMs as an effective learning tool. The majority indicated areas of new learning and found SLMs enhanced their professional skills and confidence. Facilitator feedback was positive, and suggested SLM optimization strategies.
Conclusion. Student and teaching team recommendations will inform future curriculum development including the optimization of SLMs in pharmacy education.
Keywords: pharmacy, communication, patient simulation, simulation-based education, EXCELL Program
INTRODUCTION
The professional role of pharmacists has developed to incorporate patient counseling,1 and pharmacy education has embraced communication as one of its core values.2 Effective communication is an essential professional standard for pharmacy students.2-4 Good communication skills enable pharmacists to establish effective relationships with patients and health care teams, contributing to the optimization of health outcomes and promotion of interprofessional relationships.2,4-7
While communication skills remain imperative for patient care in pharmacy practice, increasingly communication training is focused on the need for pharmacists to communicate competently with other health professionals.2,8,9 Inadequate communication among health professionals can result in misunderstandings, negatively affect interprofessional relationships, cause suboptimal information transfer, and adversely affect health outcomes.10-12 Interprofessional educational innovations assist in enhancing pharmacists’ communication skills with other disciplines and foster general awareness of the potential of pharmacists’ professional contributions,13,14 thus facilitating pharmacists’ participation in interdisciplinary health care teams.15,16
Pharmacy students’ development of and training in communication skills often uses some mode of simulated learning to assist with acquiring communication competencies and enhancing skills as learners.2,6 Many health disciplines use simulations, including computer simulations, mannequin and actor simulations,17-19 and some pharmacy schools incorporate simulated learning into their curricula.13,15 Examples include virtual patients and online virtual patients,18 virtual practice environments,20 simulated patients with intellectual disabilities,19 and human patient mannequins to teach interdisciplinary team skills.2
A challenge for pharmacy education is to broaden the focus of communication competency development from pharmacy and interdisciplinary professional contexts to the totality of the student learning experience. Importantly, the latter includes student communication with pharmacy preceptors during placements (experiential practicums in community pharmacy) to optimize student learning, readiness for placements and work readiness overall.16,21 Regrettably, the context-specific nature of most published studies renders it challenging to identify the most successful approaches to enhance students’ communications skill development in the classroom or on placement. Many studies advocate a combination of methods involving self-assessment, reflective journaling, oral presentations, scripted exercises, effective precepting, as well as more use of online, virtual, and simulated learning methods. In addition to incorporating these pedagogic approaches with previous cohorts, the present study was also informed by the principal researcher’s experience as “placements convenor,”21 which involved receiving ongoing student (and preceptor) feedback on pharmacy practice and the range of communication and learning challenges both groups encountered during pharmacy placements. Consistent with some reports in the literature,4,22 specific pharmacy practice issues were concerned with ethical and legal obligations, drug issues, and professionalism implications.
An innovative aspect of the present study of simulated learning modules (SLMs) was the incorporation of social interaction maps (SIMs), which represent a modified version of one of the tools used in the “EXcellence in Cultural Experiential Learning and Leadership (EXCELL) Program” model.23,24 Collaboration between applied psychologists led to the development of the EXCELL Program. For almost two decades, the program has been applied in job training preparation for immigrants and in higher education disciplines of business, nursing, pharmacy, and psychology.25 In pharmacy in particular, EXCELL has been integrated in the curricula during first and second years.23 The EXCELL model and the description of its application is readily available in the literature. The program is a schematic, skills-based professional development resource centered around developing participants’ generic social competencies in interacting with others (ie, seeking help, making social contact, participation in a group, refusing a request, expressing disagreement, and giving feedback).23 These generic competencies are fundamental to effective interactions in pharmacy practice and tend to be challenging for students, particularly for those from culturally and linguistically diverse (CALD) backgrounds. An EXCELL SIM outlines the specific verbal and nonverbal behavior demonstrated by interactants in an effective, culturally appropriate communication exchange. Each SIM outlines the four stages of an interaction: Approach, Bridging, Communicating, and Departing (ABCD). In an EXCELL training session, a SIM is developed with group participants for one of the six generic competencies in a specific social scenario. The use of the ABCD model enables the teachers to investigate how “breaking down” the communication process into smaller steps (ie, going back to basics) will be valued by MPharm students. The complete EXCELL training model typically involves preparation of a SIM for a specific communication competency in a specific situation, demonstration of the competency by facilitators using a SIM, practice by participants using SIMs, and feedback and coaching of participants by facilitators. The program was endorsed in a critical review of contemporary research in internationalization of curriculum in the business discipline,26 as well as in earlier critiques.27
The aims of this study were twofold: to examine how pharmacy students and teaching staff perceived the value of six SLMs as a way of enhancing communication skills in practice and on placement and to investigate the inclusion of SIMs as part of simulation training in pharmacy education.
METHODS
The shortage of placement hours in the fourth-year MPharm curriculum at Griffith University on the Gold Coast, Australia necessitated the addition of on-campus activities to provide supplementary learning activities. Simulated learning modules were used in a course comprising placements and communication training, so certain aspects of communication simulation were already present (eg, objective structured clinical examination [OSCE] training and assessment). The student cohort was divided into three groups to undertake SLM lectures and workshops over a 6-week period. Attendance was mandatory. Simulated learning modules comprised two components: three hours of preparatory lectures and two 4-hour workshops, a week apart. Prior to each SLM workshop, preparatory lectures provided an overview of the concept of simulated learning, as well as outlining the “core knowledge” component of each SLM scenario. The rationale underpinning the design was that any knowledge gaps did not detract from the main goal of SLM workshops which was practice and optimization of professional communication. For example, if the scenario included the topic of medication scheduling, the general concept of scheduling was addressed in the lecture so that the SLM workshop could focus solely on the communication issues around scheduling (eg, pharmacist refusing patient’s request for a scheduled medication).
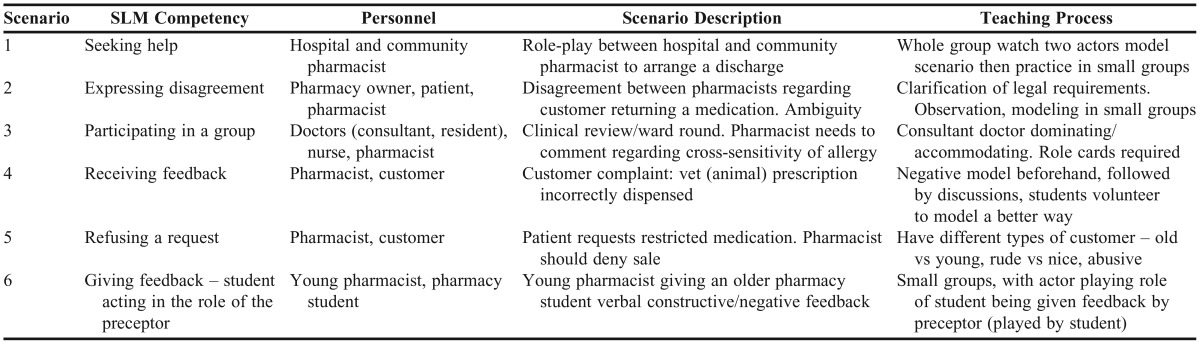
Six SLM scenarios were created by the teaching team who drew on their professional experience as educators and practitioners. Each scenario addressed selected communication competencies from the National Competency Standards Framework for Pharmacists in Australia3 and the EXCELL Program.23,24 Table 1 outlines the six scenarios that comprised the SLMs and the related communication competency. Scenarios included role-plays focusing on interactions between pharmacy colleagues, pharmacists and other health professionals, pharmacists and patients, and preceptors and students. Because community preceptors supervising students on placements can experience challenges providing feedback to students during placement, an additional competency (ie, giving feedback) and corresponding SIM was added to the five generic EXCELL competencies.28
Table 1.
Brief Outline of Pharmacy Simulated Learning Module (SLM) Scenarios (each practiced at varying levels of difficulty)
Actors participated in all SLM workshops, assisting with the demonstration of scenarios in one-on-one role-plays, as well as post-practice debriefing. They were auditioned for and briefed on each scenario and its variations (eg, modifying their communication style from less to more assertive throughout an SLM). The scenarios were scripted for actors to enhance standardization of scenarios, but each included suggestions for variations in order to maximize opportunities for student learning. Members of the teaching team familiar with the principles of the EXCELL Program, and two facilitators (one with a psychology the other with a pharmacy background) provided group facilitation of role-plays during SLMs. Six SIMs, each addressing the core competency of a specific SLM, were presented to students after role-plays and initial debriefing were completed. This process was an adaptation of the usual EXCELL training process where SIMs are created with participants prior to the enactment of a role-play, and the SIM is referred to during the role-play. The variation in this study was used to encourage students to conduct the simulation without the help of any learning aids. The SIM was distributed to students during the debriefing (after the role-play) as a tool to remind them what constituted appropriate verbal and nonverbal behavior at each stage of the interaction. The facilitators explained that the SIM was not meant to be prescriptive in any way, but merely an example of appropriate communication strategies that could be used in the specific scenario. Because of the workshop length (four hours each), light refreshments were included for the teaching team, actors, and students, and regular breaks were taken. Video footage of role-plays (where student approval was granted) was created for future use in the curriculum. Ethics approval was granted by the Griffith University’s Human Research Ethics Committee. Student participation in the research component of the SLMs was voluntary, per the University’s Ethics protocols.
RESULTS
All MPharm students enrolled in the second semester of the first year were required to complete the SLMs. Ninety-four students attended week 1, and 91 attended week 2. There were 32 male and 59 female students (one participant did not state gender). The mean age was 24 years (SD=4.10) and 79.3% of students were Australian citizens/permanent residents, with 63.0% born in Australia, and 20.7% were from overseas. Students were born in 20 different countries: 28.3% from a non-English speaking background (NESB), and 66.0% reported speaking English as the main home language. Students spoke 16 different languages at home.
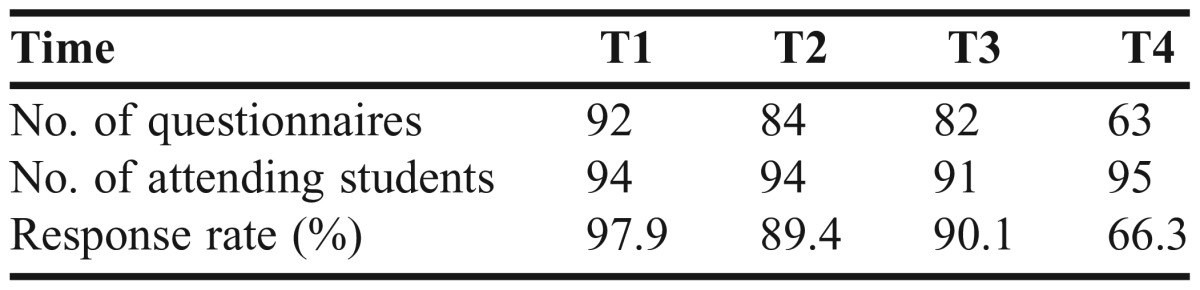
Questionnaires containing qualitative and quantitative measures were administered to students on four occasions (T1-T4, Table 2). Prior to the start of the first SLM workshop (T1), students completed questionnaires containing demographics. At the end of the first SLM workshop (T2), students completed a questionnaire regarding their experience of the SLM workshop. Following completion of the second and final workshop (T3), another questionnaire was administered to collect data about the value of SLMs. Finally, as part of their written placement portfolio at the end of semester, two months after T3, and following the completion of a 3-week pharmacy placement, students completed an additional questionnaire to evaluate the longer-term effect on student’s self-perceived practice skills (T4). The response rate at T4 was notably lower, possibly because T4 surveys were administered several months after SLMs were completed, which could have diminished interest in the survey completion.
Table 2.
Questionnaires Completed for Each Stage of the Research Process (T1-T4)
Quantitative analysis of students’ pre/post SLM responses (5-point Likert scale: 1=strongly disagree to 5=strongly agree) was conducted using descriptive statistics, means comparison (ANOVA), and factor analysis. Qualitative responses were analyzed by coding of the open-ended question responses, facilitated by MAXqda computer software (VERBI GmbH, Berlin, Germany)29 to assist with the management and organization of data coding, sorting, and categorizing. The qualitative data was categorized using open, axial, and selective coding processes.30 To check on reliability, the coding scheme was explained and the questions coded by an independent rater with research training. Both sets of coding were examined independently by a third person with research training and content knowledge. Coding accuracy was confirmed, with consistency well over 90%, indicating an appropriate level of inter-rater reliability.31 On the few occasions where disagreements occurred, a third person examined the relevant transcript section and made a decision in relation to the codes.
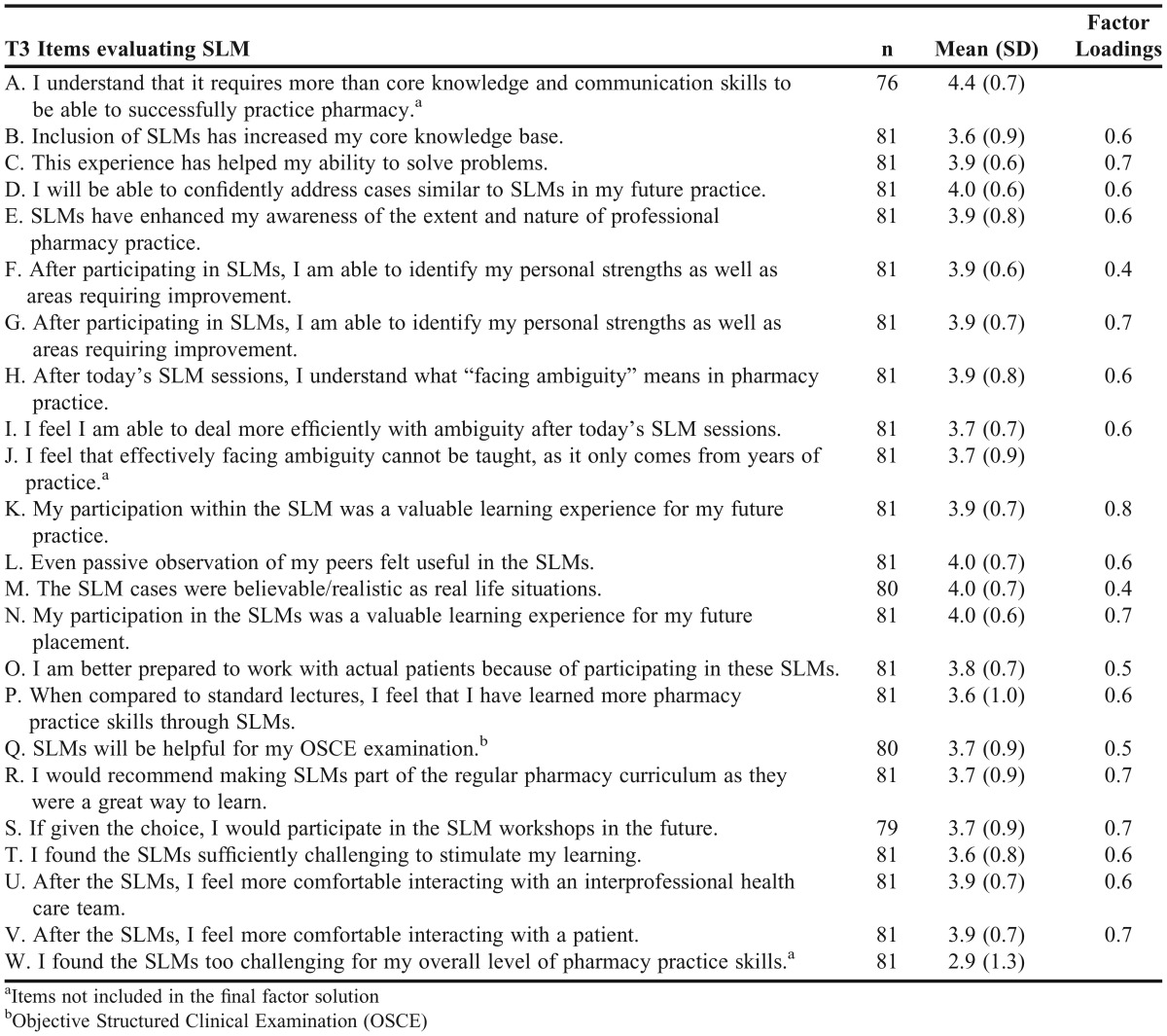
Table 3 shows that the majority of students rated the value of SLMs highly at T3, most items attracting a mean score of around four (on a 5-point scale). Exploratory factor analysis of the 23 items suggested a single factor explaining almost 35% of the shared variance. Statements A and J were conceptually less related to the topic of the value of SLMs, and item W was phrased negatively. As a result, these three items displayed weaker loadings and when removed, the remaining 20 items explained 39% of the shared variance. The resulting scale (scale 20) has a mean score of 3.84, with a normal distribution (Table 3). This scale shows excellent reliability, with a Cronbach alpha of 0.9. The majority of students (61.7%) regarded the SLMs as “sufficiently challenging to stimulate learning” (item T), while only 6.2% of students disagreed. In contrast, item W had a lower mean score of 2.9 and a bimodal distribution. While almost 40% agreed that the SLMs were too challenging, 43.2% disagreed, with 17.3% of responses being neutral. As stated earlier, this item may represent an outlier.
Table 3.
T3 Value of Simulated Learning Modules (SLMs) – Means and Factor Loadings
Demographic differences were evident in responses to the items and scale scores, predominantly for gender, but also for home language and birth country. Males rated the SLM experience more favorably than females, in particular on four items: the value of SLMs for future practice (males M=4.15, females M=3.78, p=0.03) and future placements (males M=4.27, females M=3.93, p=0.02), SLMs being sufficiently challenging to stimulate learning (males M=3.92, females M=3.53, p=0.05), being more comfortable interacting with patients as a result of SLMs (males M=4.19, females M=3.75, p=0.001), as well as on the overall Scale (males M=4.03, females M=3.74 p=0.01). Students recorded as NESB were more likely to rate the SLMs as too challenging (M=3.41), compared with English-speaking students (M=2.67, p=0.2). Overseas NESB students rated SLMs as being “sufficiently challenging to stimulate learning” higher (M=4.10) than did English speaking Australian students (M=3.64, p=0.05). Those born overseas were more likely to rate the SLMs as making them more comfortable interacting with an interprofessional team (M=4.07, SD=0.57) compared with Australian-born students (M=3.75, SD=0.83, p=0.05).
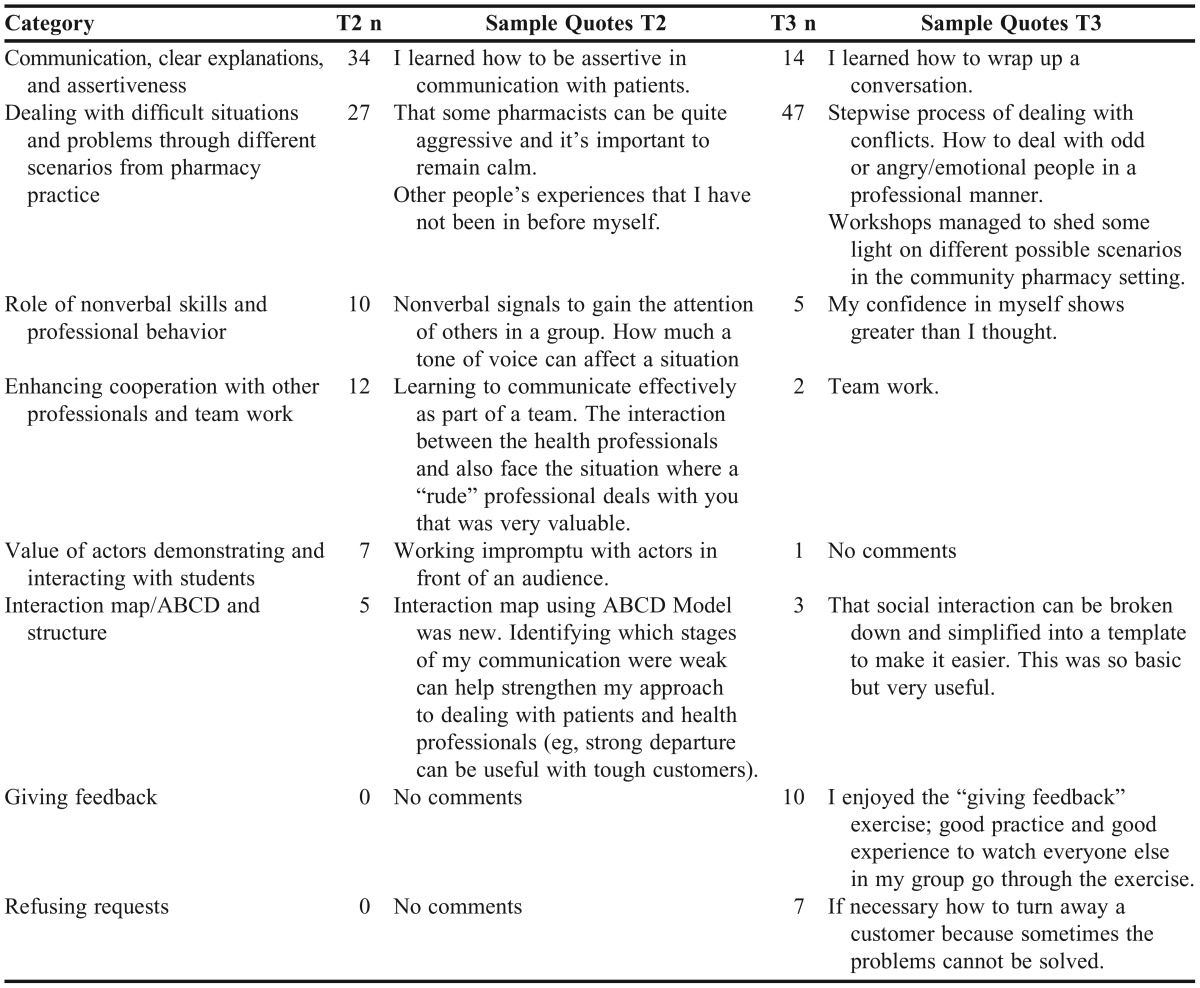
At T2 and T3, students were asked to comment on what they learned that was new from the SLM workshop. Response rates were 88.0% and 92.9%, respectively. As shown in Table 4, students comments at T2 referred to learning communication skills in general, with particular comments about learning to manage difficult situations, learning how to interact with other professionals, developing assertiveness, understanding the important role of nonverbal communication, and considering different pharmacy scenarios. Two respondents reported they did not learn anything new. At T3, students placed the greatest emphasis in their responses on learning how to deal with difficult situations, with a number of positive comments expressed about giving feedback, communicating clearly and assertively, and refusing a request.
Table 4.
Summary of New Learning Reported by Students after Simulated Learning Module (SLM) Workshops (T2 and T3)
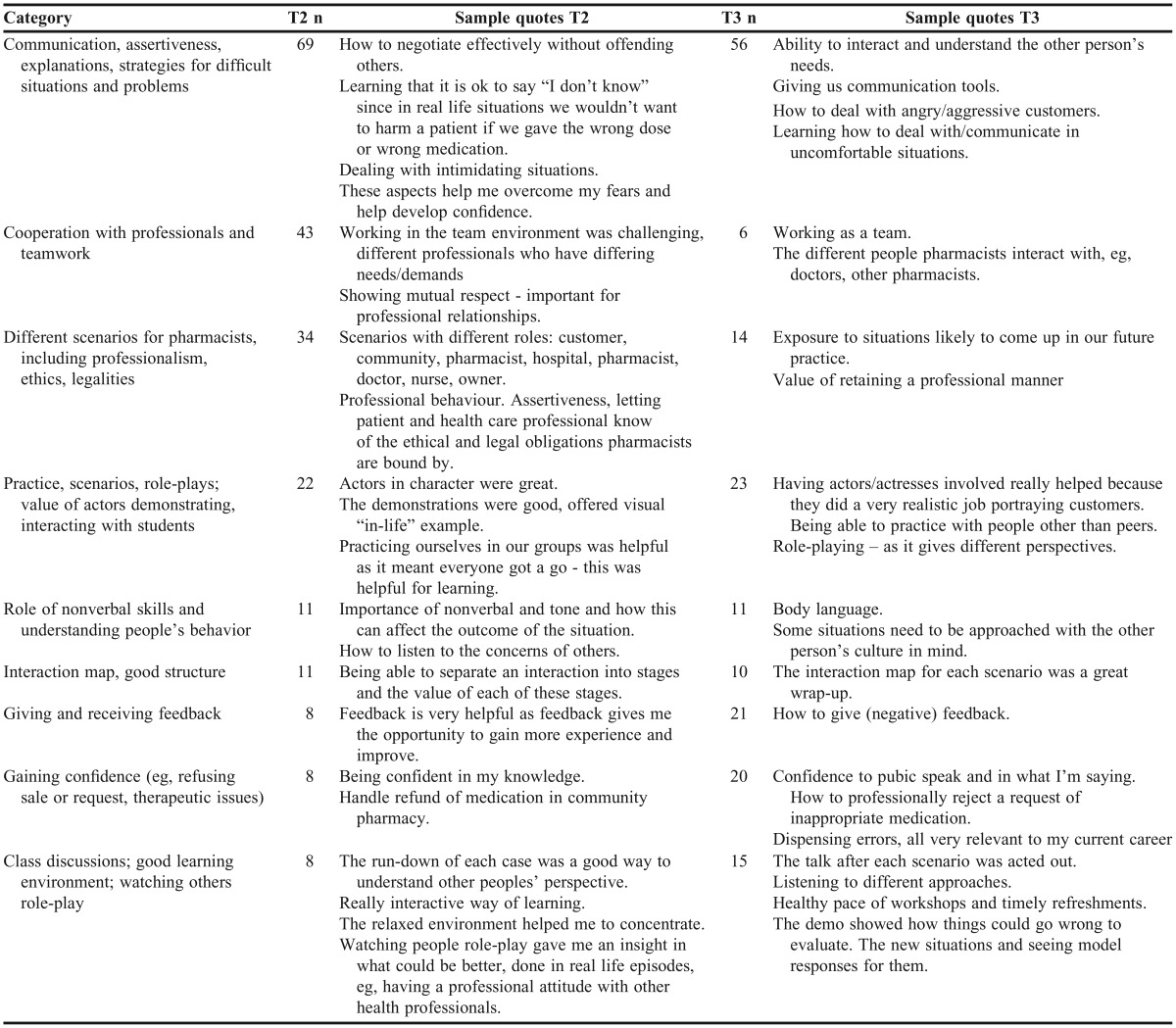
Students were asked what they perceived as the three aspects of SLMs most relevant to their learning. Responses to this question (Table 5) echoed previous responses (Table 4). After the first workshop, 90.2% of those completing questionnaires responded to this question, and after the second workshop, 89.3%. A large number of responses referred to communication and assertiveness, strategies for difficult situations, cooperation with other professionals, and teamwork. Students, as practitioners-in-training, believed the SLM scenarios were relevant to their overall pharmacy practice experience (Table 5). In particular, students appreciated certain aspects of learning: the value of actors in simulating real life, hands-on role-play practice, as well as watching other students role-play, post-practice discussions, and using SIMs. Students’ comments about the actors were positive (70 out of 80 actor-related comments), with students describing actors’ participation as enjoyable, realistic, and encouraging. Students also appreciated the actors’ constructive feedback.
Table 5.
Relevance of Simulated Learning Modules (SLMs) for students’ learning (T2 and T3)
Students were also asked what was not relevant for their learning, and at T2 the response rate was 80.4%, and 56.1% at T3. The majority response was that nothing was irrelevant. Repetition of the variation of the same scenario was perceived as undesirable by some students, while some scenarios were considered more relevant than others. A few students also found working with the actors challenging and uncomfortable, in particular when actors portrayed intimidating, stubborn, or aggressive characters.
DISCUSSION
This project presented an opportunity for pharmacy students to apply their knowledge and skills to a variety of pharmacy practice and experiential placement communication scenarios across the six SLMs. The study achieved its intended aims. Quantitative findings were supported by qualitative data. The majority of students reported benefits from participating in the simulated learning situations. Students found that the SLMs enhanced their learning, demonstrating that the use of structured, straightforward, and basic communication scenarios met their learning needs. While student SLM workshop attendance was mandatory, the participation in research activities was not, and, in addition to the positive comments, students’ high survey response rates also illustrate the level of student enthusiasm and engagement in the SLMs. Previously, reports indicate that students appreciate communication simulation activities in the classroom,32 even when used as an isolated teaching activity.33
The four facilitators reflected on the strengths of SLMs immediately after their completion. They concurred that the modules effectively complemented the existing communication training in the MPharm program by promoting a different type of individual and group work in a safe environment. Students had an opportunity to observe and participate in nuanced, real-life pharmacy practice and placement scenarios and role-play with actors while using practice skills. Certain issues commonly arising during placements could also be addressed before placements, and potential solutions discussed constructively. This was valuable as students had the opportunity to learn “by watching” and “by doing” to suit different learning styles. There was also opportunity for comfortably paced formal and informal interactions, individual and group reflection, and feedback amongst students, facilitators, and actors. Further, a range of professional environments were presented (some interprofessional), and SLMs exposed students to working with actors and role-playing at more professional level. Facilitators observed that that there was a certain “new quality” in student behavior that could be explained by the actors’ presence. Students were simultaneously more relaxed, yet also more alert and spontaneously engaged in role-plays and debriefing in the presence of nonstaff. Through the role-plays (and variations in role-plays), students were exposed to the ambiguity of pharmacy practice and challenges of novel pharmacy experiences, which enabled discussion of related and expanded scenarios.
There were a number of weaknesses in the design, delivery, and execution of SLMs, according to the facilitators. For example, some practice group sizes were big, which perhaps limited students’ opportunity to engage and made time management more challenging. Actors’ abilities sometimes varied, which could have affected the dynamic and quality of the role-plays and subsequent debriefing. Using actors with medical backgrounds, or health professionals themselves would have been more appropriate. These complexities with actors occurred despite auditioning actors prior to workshops, briefing them before each session, and providing the necessary verbal and written information required for each scenario. Some actors also chose to improvise beyond what they were briefed on, and the facilitators had to intervene during the workshop. Facilitators felt that the workshops were too long (four hours each), with, at times, too much repetition. However, more time seemed warranted for each competency, since three SLMs in four hours seemed to be too many. Addressing one competency per week could have been more appropriate, with associated homework, and more face-to-face follow up. At times, some students seemed affected by the emotional intensity of particular scenarios, and this was promptly addressed in the workshops. Another weakness was that the SLM workshops constituted additional work for students, not part of the course, and they effectively undertook 11 additional hours of lectures and workshops in a short semester.
The SLMs developed students’ communication skills in a positive and safe learning environment, with most students awarding the SLMs a score of 4 out of 5. Students had opportunities to learn from group, individual, immediate, and specific feedback and debriefing after each SLM role-play. They reported appreciating the range of scenarios and acquisition of new skills in relation to assertiveness, dealing with difficult situations, nonverbal communication, and interprofessional communication. Interestingly, male students rated SLM activities more favorably than females, in contrast to Fazel and Aghamolaei.34 The student cohort had a diverse population born across 20 different countries, and a higher proportion of those than the general Australian population were born overseas (37%) or spoke a language other than English at home (34%).35
Students characterized with a NESB who were born overseas reported that SLMs stimulated their learning and made them feel more comfortable interacting with an interprofessional team (when compared with the other students). They rated the communication SLMs as more challenging than the English speaking students did, consistent with the findings about the communication challenges of pharmacy students with a NESB.36-38 This suggests that NESB students may be more likely to benefit from communication skills training as part of an SLM, but the level of difficulty can also be more challenging to calibrate for the teaching staff.
Students were positive about the realism actors brought to role-plays and found the actors’ ongoing feedback and encouragement beneficial for learning. Literature also reinforces the use of actors in simulation activities33,39 as they provide more realism, authentic student responses and input, and add sense of veracity and ecological validity. While using actors may be time-consuming and expensive, they are superior to using peers in role-plays.40 It is imperative to ensure reliability and validity of actor performance and training to create a safe and engaging learning environment. The SIMs proved to be a useful pedagogic tool offering a valuable point of discussion after the SLMs. The maps helped students consider a schema for the communication competencies. Literature also supports the use of simulation as a form of communication skills development for pharmacy students,2,9,41 as well as inclusion of the EXCELL in pharmacy education.23,28 Overall, students reported that SLMs enabled them to feel more confident about communication skills in the workplace and assessment activities.
Per student feedback and facilitator reflections, any future SLMs could benefit from: (1) allocating students to diverse learning groups and more strongly encouraging student engagement (perhaps by linking SLMs to assessment); (2) delivering shorter workshops but offering them more frequently, with less repetition of each role-play; (3) providing compulsory audition and ongoing training of actors (ideally with health backgrounds) to create more uniformity and prevent performance/improvisation; (4) addressing different pre-existing levels of students’ English language and communication skills and fine-tuning SLMs accordingly; (5) allowing students on different practice levels to decide if they wanted to be at an advanced or basic level, and writing SLMs accordingly; (6) contextualizing EXCELL as a teaching framework in a developmental way, to be repeated and refined, with each iteration advancing in difficulty/complexity and scaffolded over the year levels (while recognizing that staffing a resource-intensive intervention may be challenging); and (7) discussing with students the advantages and disadvantages of being filmed during role-plays.
This curricular MPharm innovation had certain inherent limitations because of its novel approach. While it was an intention of the study to seek students’ subjective perceptions of the SLMs, students’ self-reports were unvalidated. Future offerings of the program would benefit from the inclusion of objective evaluations such as the use of blind raters (eg, independent teaching staff). Another potential limitation may have been the extent to which students sought to appear competent to their academic facilitators as part of impression management. The inclusion of a control group may strengthen future research of similar SLMs, as would a larger sample size. Similarly, a longitudinal design would be useful in understanding the long-term impact of SLMs. The questionnaires and scales were specifically designed for this study and require appropriate validation. As noted earlier, the capacity to engage and enact the desired behavior in a consistent, appropriate manner at times varied from actor to actor, depending on skill and experience. Selection of actors with experience in health training and simulations, as well as more preparation for the required scenarios would help to ensure greater consistency. Participation in SLM workshops was mandatory but did not contribute to students’ grades. While this was explained to the students and did not seem to impact either their full engagement in the workshops or their positive evaluations, it may have influenced the context in which they perceived the role of SLMs in the curriculum. Finally, the innovation represented a major commitment in terms of staff resources and time involved in planning, execution, and follow up. Although reportedly satisfying for students and staff alike, the long-term sustainability of such a curricular undertaking requires commitment to ensure pedagogic feasibility and quality.
CONCLUSION
Curriculum innovation to include SLMs that incorporate principles of the EXCELL Program is encouraging in terms of positive student and staff feedback. Simulated learning modules tailored to the needs of students as practitioners-in-training are an effective pedagogic strategy. Their strength lies in enabling students to acquire skills they can use in the classroom, in practice, and during professional experiential training. Encouragingly, students indicated many areas of new learning and reported how SLMs enhanced their confidence and professional skills. Facilitator feedback suggested specific approaches to further enhance the quality of simulated learning experiences, informing future curriculum development.
ACKNOWLEDGMENT
This research was financially supported in part by Health Workforce Australia (HWA).
REFERENCES
- 1.Cavaco AM, Romano J. Exploring pharmacists’ communication with customers through screening services. Patient Educ Couns. 2010;80(3):377–383. doi: 10.1016/j.pec.2010.06.028. [DOI] [PubMed] [Google Scholar]
- 2.Wallman A, Vaudan C, Sporrong S. Communications training in pharmacy education, 1995-2010. Am J Pharm Educ. 2013;77(2) doi: 10.5688/ajpe77236. Article 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pharmaceutical Society of Australia (PSA) National Competency Standards Framework for Pharmacists in Australia. Canberra: PSA. 2010 https://www.psa.org.au/download/standards/competency-standards-complete.pdf [Google Scholar]
- 4.Marriott JL, Nation RL, Roller L, Costelloe M, Galbraith K, Stewart P, et al. Pharmacy Education in the Context of Australian Practice. Am J Pharm Educ. 2008;72(6) doi: 10.5688/aj7206131. Article 131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brock D, Abu-Rish E, Chiu CR, Hammer D, Wilson S, Vorvick L, et al. Interprofessional education in team communication: working together to improve patient safety. BMJ Qual Saf. 2013;22(5):414–423. doi: 10.1136/bmjqs-2012-000952. [DOI] [PubMed] [Google Scholar]
- 6.Greenhill N, Anderson C, Avery A, Pilnick A. Analysis of pharmacist-patient communication using the Calgary-Cambridge guide. Patient Educ Couns. 2011;83(3):423–431. doi: 10.1016/j.pec.2011.04.036. [DOI] [PubMed] [Google Scholar]
- 7.Hyvärinen M-L, Tanskanen P, Katajavuori N, Isotalus P. A method for teaching communication in pharmacy in authentic work situations. Commun Educ. 2010;59(2):124–145. [Google Scholar]
- 8.Levett-Jones T, Gilligan C, Lapkin S, Hoffman K. Interprofessional education for the quality use of medicines: designing authentic multimedia learning resources. Nurse Educ Today. 2012;32(8):934–938. doi: 10.1016/j.nedt.2011.10.013. [DOI] [PubMed] [Google Scholar]
- 9.Vyas D, McCulloh R, Dyer C, Gregory G, Higbee D.An interprofessional course using human patient simulation to teach patient safety and teamwork skills Am J Pharm Educ 201276(4)Article 71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cleland JA, Watson MC, Walker L, Denison A, Vanes N, Moffat M. Community pharmacists’ perceptions of barriers to communication with migrants. Int J Pharm Prac. 2012;20(3):148–154. doi: 10.1111/j.2042-7174.2011.00172.x. [DOI] [PubMed] [Google Scholar]
- 11.Hawala-Druy S, Hill MH. Interdisciplinary: cultural competency and culturally congruent education for millennials in health professions. Nurse Educ Today. 2012;32(7):772–778. doi: 10.1016/j.nedt.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 12.Bajramovic J, Tett SE. Problems of pharmacy communication in multicultural Australia. Aust Pharm. 2000;19(7):430–434. [Google Scholar]
- 13.Ragan RE, Virtue DW, Chi SJ.An assessment program using standardized clients to determine student readiness for clinical practice Am J Pharm Educ. 201377(1)Article 14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Masters C. Multidisciplinary, team-based learning: the simulated interdisciplinary to multidisciplinary progressive-level education (SIMPLE©) approach. Clin Simul Nurs. 2012;9(5):e171–e178. [Google Scholar]
- 15.Lupu AM, Stewart AL, O’Neil C. Comparison of active-learning strategies for motivational interviewing skills, knowledge, and confidence in first-year pharmacy students. Am J Pharm Educ. 2012;76(2) doi: 10.5688/ajpe76228. Article 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Emmerton LM, Mampallil L, Kairuz T, McKauge LM, Bush RA. Exploring health literacy competencies in community pharmacy. Health Expect. 2012;15(1):12–22. doi: 10.1111/j.1369-7625.2010.00649.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gates MG, Parr MB, Hughen JE. Enhancing nursing knowledge using high-fidelity simulation. J Nurs Educ. 3011;51(1):9–15. doi: 10.3928/01484834-20111116-01. [DOI] [PubMed] [Google Scholar]
- 18.Watson MO, Jolly BC. The future of Australian medical education: a focus on technology. Med J Aust. 2013;199(5):S26–S28. doi: 10.5694/mja12.10679. [DOI] [PubMed] [Google Scholar]
- 19.O’Boyle-Duggan M, Grech JD, Brandt R. Effectiveness of live simulation of patients with intellectual disabilities. J Nurs Educ. 2012;51(6):334–342. doi: 10.3928/01484834-20120504-01. [DOI] [PubMed] [Google Scholar]
- 20.Hussainy SY, Styles K, Duncan G. A virtual practice environment to develop communication skills in pharmacy students. Am J Pharm Educ. 2012;76(10) doi: 10.5688/ajpe7610202. Article 202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fejzic J, Henderson A, Smith NA, Mey A. Community pharmacy experiential placement: comparison of preceptor and student perspectives in an Australian postgraduate pharmacy programme. Pharm Educ. 2013;13(1):15–21. [Google Scholar]
- 22.Stupans I, March G, Owen SM. Enhancing learning in clinical placements: reflective practice, self-assessment, rubrics and scaffolding. Assess Eval High Educ. 2013;38(5):507–519. [Google Scholar]
- 23.Mak AS, Westwood MJ, Ishiyama FI, Barker MC. Optimising conditions for learning sociocultural competencies for success. Int J Intercult Rel. 1999;23(1):77–90. [Google Scholar]
- 24.Mak AS, Kennedy M. Internationalising the student experience: preparing instructors to embed intercultural skills in the curriculum. Innov High Educ. 2012;37(4):323–334. [Google Scholar]
- 25.Barker M, Mak AS. From classroom to boardroom and ward developing generic intercultural skills in diverse disciplines. J Stud Int Educ. 2013;17(5):573–589. [Google Scholar]
- 26.Caruana V, Ploner J.A critical review of contemporary practice and educational research in internationalization within the business education subject communitiesThe Higher Education Academy2012 [Google Scholar]
- 27.Ward C. Victoria University of Wellington; 2006. International students: interpersonal, institutional and community impacts: update of the 2001 literature review. Ministry of Education; Centre for Applied Cross-cultural Research. [Google Scholar]
- 28.Malangal S, Hills R, McMillan S, Barker M, Blauberg N, Shallcross L. Enhancing intercultural competence among pharmacy students through the EXCELL program. Research and Development in Higher Education: Connections in Higher Education. 2012:35. [Google Scholar]
- 29.Given LM. The SAGE Encyclopedia of Qualitative Research Methods. Thousand Oaks, CA: SAGE Publications, Inc; 2008. [Google Scholar]
- 30.Corbin J, Strauss A. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. 3rd Ed. Thousand Oaks, CA: SAGE Publications, Inc.; 2008. [Google Scholar]
- 31.Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. 2nd Ed. Thousand Oaks, CA: SAGE Publications, Inc.; 1994. [Google Scholar]
- 32.Branch C. Pharmacy students’ learning and satisfaction with high-fidelity simulation to teach drug-induced dyspepsia. Am J Pharm Educ. 2013;77(2) doi: 10.5688/ajpe77230. Article 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fernandez R, Parker D, Kalus JS, Miller D, Compton S. Using a human patient simulation mannequin to teach interdisciplinary team skills to pharmacy students. Am J Pharm Educ. 2007;71(3) doi: 10.5688/aj710351. Article 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fazel I, Aghamolaei T. Attitudes toward learning communication skills among medical students of a university in Iran. Acta Med Iran. 2011;49(9):625–629. [PubMed] [Google Scholar]
- 35.Year Book Australia. Canberra: Australia; 2008. Australian Bureau of Statistics. [Google Scholar]
- 36.McKauge L, Emmerton L, Bond J, et al. The Student Experience, HERDSA Annual Conference. Darwin: Australia; 2009. An initiative to improve the professional communication skills of first-year pharmacy students. [Google Scholar]
- 37.Jones J, Krass I, Holder GM, Robinson RA. Selecting pharmacy students with appropriate communication skills. Am J Pharm Educ. 2000;64(1):68–73. [Google Scholar]
- 38.Watermeyer J. “She will hear me”: how a flexible interpreting style enables patients to manage the inclusion of interpreters in mediated pharmacy interactions. Health Commun. 2011;26(1):71–81. doi: 10.1080/10410236.2011.527623. [DOI] [PubMed] [Google Scholar]
- 39.Lin K, Travlos DV, Wadelin JW, Vlasses PH. Simulation and introductory pharmacy practice experiences. Am J Pharm Educ. 2011;75(10) doi: 10.5688/ajpe7510209. Article 209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Churchouse C, Rudd C. Edith Cowan University; Perth, Australia: 2008. Bridging the theory to practice gap using performance based simulation. Sustainability in Higher Education: Directions for Change. EDU-COM 2008 International Conference. [Google Scholar]
- 41.Jabbur-Lopes MO, Mesquita AR, Silva LMA, Neto ADA, Lyra DP. Virtual patients in pharmacy education. Am J Pharm Educ. 2012;76(5) doi: 10.5688/ajpe76592. Article 92. [DOI] [PMC free article] [PubMed] [Google Scholar]