Abstract
Background
Recent anatomic studies suggest the superficial musculoaponeurotic system (SMAS) layer attenuates in the midface. This led the author to switch from a bilamellar high SMAS dissection to a “total composite flap” technique, preserving skin and SMAS/platysma as one layer in a critical “deep-plane transition zone” (DTZ) lateral to the zygomaticus major muscle. This allows traction on the SMAS to translate to the malar fat pad via a “cantilever bridge” effect, which is lost when skin is undermined in the DTZ.
Objectives
This paper attempts to answer the question of whether the composite flap or bilamellar technique better lifts the midface, comparing groups where the DTZ was undermined: (1) only at a sub-SMAS level; or (2) at both subcutaneous and sub-SMAS levels.
Methods
Thirty-five patients underwent bilamellar facelifts with skin and SMAS separated in the DTZ. Midfacial elevation was measured using size-matched preoperative and 18-month (average) postoperative photographs for the 70 hemi-midfaces. The same analysis was done for 35 patients undergoing total composite flap facelift, maintaining skin and SMAS as one layer in the DTZ. The two groups were compared.
Results
In the bilamellar group, the mean percentage of midfacial elevation at 18 months postoperative was 5.5% (range, 0.0%-17.8%). In the composite flap group, the percentage was 11.7% (range, 0.1%-32.3%). The difference was statistically significant.
Conclusions
Maintaining skin-SMAS attachments in the DTZ improves midface elevation during SMAS facelifting, exploiting a “cantilever bridge” effect of the skin transferring traction on the SMAS to the malar fat pad.
Level of Evidence: 4
 Therapeutic
Therapeutic
The aesthetics of the midfacial region are critical in defining beauty and youth, and hence also in facial rejuvenation surgery. Many surgeons have advocated employing superficial musculoaponeurotic system (SMAS)-release techniques to elevate the midface in a way that is harmonious with the way they lift the jowls and other deep-tissue structures affected by aging.1-3 These techniques employ sub-SMAS release of the zygomatic and upper and lower key masseteric ligaments to free up and elevate the mobile anterior soft tissues of the mid (and lower) face. This ability to access the anterior face to lift jowls, neck, and midface as one integrated unit sets the SMAS-release approach apart from both SMAS-plication techniques and subperiosteal midface lifting techniques.
A SMAS-release facelift can use either a bilamellar (skin and SMAS dissected separately as two flaps) or deep-plane (skin-SMAS composite flap) dissection. Within the deep-plane category exist two types of dissection of the superomedial portion of the flap. The standard deep-plane technique, as originally developed by Skoog in 1974, undermines midfacial tissues at a deep subcutaneous level, superficial to orbicularis oculi.4 The composite flap technique originated by Hamra includes orbicularis oculi in the flap, so that this muscle supports malar fat elevation.3 Also, in the neck, Skoog undermines SMAS-platysma, while Hamra converts to a subcutaneous neck dissection. As described below, the author's “total composite flap” technique combines the deeper dissection plane of both of these, using a sub-SMAS, suborbicularis oculi composite flap in the midface, and a subplatysmal composite flap dissection in the neck. The composite flap of the face is the portion relevant to the case analysis of this paper, but its continuation into the neck is described herein as well.
The composite flap lift gives a more natural appearance and avoids both the skin irregularities and potential bleeding complications associated with extensive subcutaneous dissection. The bilamellar technique allows the use of different vectors in lifting the skin vs the SMAS. However, examination of facial anatomy intraoperatively shows that SMAS and skin most likely age along the same vector. Tight connective tissue and vascular attachments make facelift skin flap elevation both traumatic and bloody. In contrast, the sub-SMAS plane's areolar and avascular prezygomatic, premasseteric (upper, middle, and lower), and buccal spaces between the retaining ligaments open readily with blunt dissection. Thus, it is within these facial spaces (beautifully described by Mendelson)5 that gravity acts to cause aging, rather than the subcutaneous plane. This suggests that while an “anatomic” reversal of aging requires extensive sub-SMAS release, the appropriate vectors of pull can be applied without separating the skin from the SMAS flap. And although skin tailoring, particularly in the post auricular area, may require more extensive skin undermining (where there is no SMAS layer anyway), there is no reason to undermine skin more extensively in the face itself than is necessary to access the deep plane at the appropriate level.
In fact, modern anatomic knowledge of the SMAS (outlined below) suggests a specific reason not to do so. The SMAS layer attenuates and essentially disappears medially to the zygomaticus major muscle.6,7 This makes a composite flap dissection laterally to this point mandatory in order to translate SMAS traction into the midface. The region of this mandatory composite flap dissection that is relevant to midface elevation is herein termed the deep-plane transition zone (DTZ) (Figure 1). The anatomic basis for it is described below.
Figure 1.
Deep-plane transition zone (DTZ). The borders of the trapezoidal-shaped DTZ are: laterally, an oblique line starting 4.5 cm anterior to the tragus and ending 2.5 cm antero-inferior to the ear lobule, even with the oral commissure; superiorly, the midpoint of the zygomatic arch; medially, the zygomaticus major muscle with an anterior bend over the prezygomatic space; and inferiorly, the transverse line even with the oral commissure. As shown in Figure 5, the deep-plane dissection continues inferior to this line, across the jawline and into the neck, but the area above it is the portion relevant to midface elevation.
A point of terminology should be made here. The author's dissection in the midface is a composite flap dissection since it includes orbicularis oculi muscle in the flap. Some authors have noted the distinction between the deep-plane and composite flap dissections in the midface, with the latter including orbicularis oculi muscle and the former leaving it deep to the flap.8,9 However, the area of sub-SMAS transition in the DTZ lateral to the orbicularis oculi is identical in both traditional deep-plane and composite flap dissections, thus the term “deep-plane transition zone.”
Midface SMAS Anatomy and the Cantilever Bridge Effect
Multiple studies over the past few years have refined our knowledge of the SMAS, with the most recent ones showing that the SMAS layer attenuates anatomically and functionally as it courses into the midface.6,7 A 2008 study of 100 cadaver facial halves and intraoperative observations during 150 deep-plane facelifts by Gassner et al concluded that “(s)uperolateral to the modiolus, a soft tissue gap separates the zygomaticus major muscle and the SMAS … . no ligamentous or fascial attachments that could transmit tension connect the SMAS with the middle or upper third of the melolabial fold … (and) when the massetericocutaneous and platysmoauricular ligaments are adequately freed up, lateral tension on the SMAS is transmitted only to the buccinator muscle, modiolus, and orbicularis oris muscle.”6 Figure 2 illustrates the attenuation pattern of the SMAS layer.
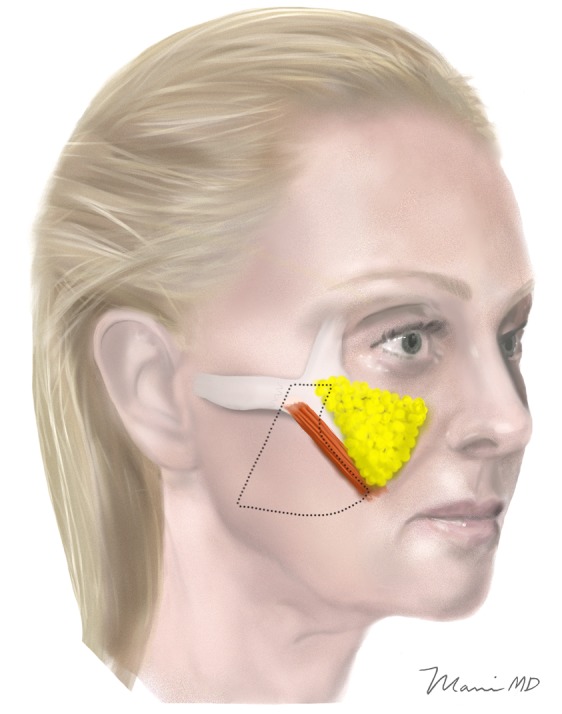
Figure 2.
SMAS layer attenuation. The thinning of the SMAS as it courses towards the zygomaticus major muscle is shown.
Combined with the author's own intraoperative experience, the Gassner anatomic study led to a change in technique to preserve a composite flap in the DTZ. Aside from anatomy, the physics of SMAS tension have been studied since the change was made, and these studies support this decision as well. The strength of the upper lateral SMAS has been verified to easily carry a composite flap in both preauricular and mastoid areas of fixation.10 However, a study published in Aesthetic Surgery Journal in July 2014 suggests that the elastic modulus and ultimate strength of the inferomedial SMAS is distinctly less than that of the upper lateral SMAS, with stronger and weaker zones defined (Figure 3).7 This further underscores the need to preserve a composite flap to reinforce this weaker area of SMAS, and translate superolateral SMAS pull into the midface. Figure 4 shows that the composite flap in the DTZ overlaps the weaker medial SMAS in the midface.
Figure 3.
SMAS strength zones. The elastic modulus and ultimate strength of the upper lateral SMAS is distinctly greater than that of the more medial and inferior SMAS, divided into two zones, I (stronger) and II (weaker). Adapted from Hu et al.7
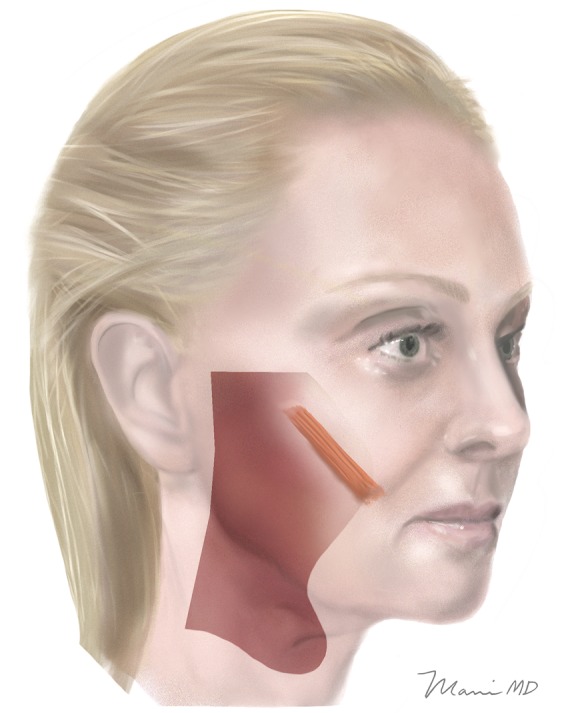
Figure 4.
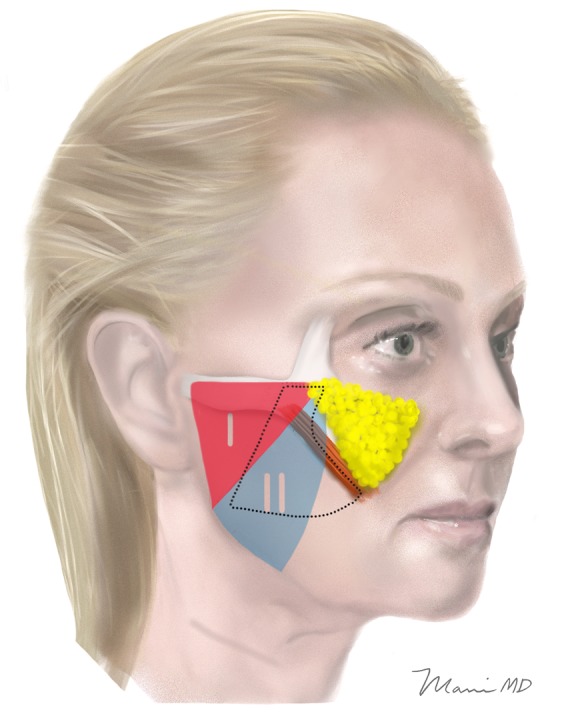
SMAS strength zones with DTZ overlaid. The DTZ overlaps the weaker medial SMAS in the midface. This ensures that the flap in this area is structurally and functionally adequate to transmit tension into the midface.
So the design of the DTZ reflects intraoperative and cadaveric studies relative to SMAS anatomy and strength. The borders of the trapezoidal-shaped DTZ (Figure 1) are: laterally, an oblique line starting 4.5 cm anterior to the tragus and ending 2.5 cm antero-inferior to the ear lobule, even with the oral commissure; superiorly, the midpoint of the zygomatic arch; medially, the zygomaticus major muscle with an anterior bend over the prezygomatic space; and inferiorly, the transverse line even with the oral commissure. (The deep-plane dissection continues inferior to this line, across the jawline and into the neck, but the area above it is the portion relevant to midface elevation.) The author's composite flap (including suborbicularis oculi) midface dissection begins more anteriorly in its uppermost section than the high-SMAS techniques previously described, which initiate the dissection more laterally with a right angle just anterior to the helical root.1-3,11 The purpose of the author's more anterior entry into the SMAS is to move the point of flap fixation closer to the midface while still maintaining SMAS attachments to skin in the DTZ (Figure 5). This orientation also incidentally places the dissection anterior to the course of the temporal branch of the facial nerve.
Figure 5.
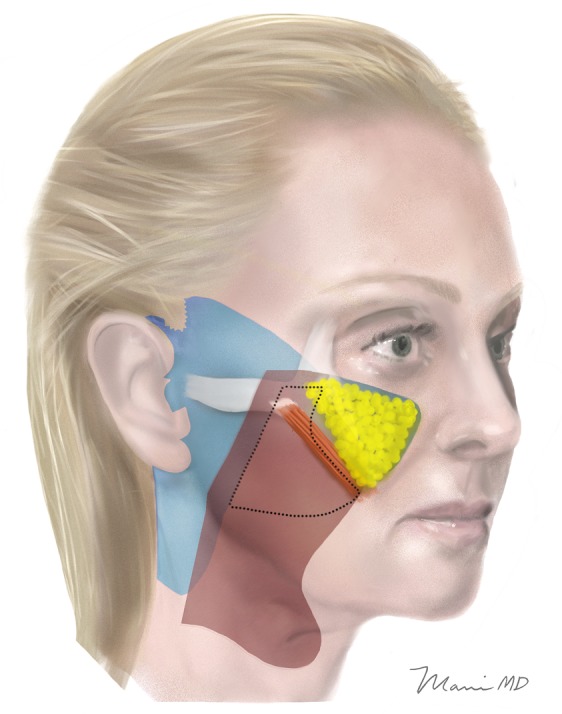
Areas of undermining for the author's technique. Limits of skin (in blue) and SMAS (in red) undermining for the author's technique, with the DTZ entirely within the red area of composite-flap undermining. The area of undermining medial to the zygomaticus major muscle is subcutaneous by definition, since there is no SMAS layer in this zone. (The premasseteric dissection joins an extended subplatysmal dissection into the neck. Platysma, but not skin, is undermined towards the midline of the neck, preserving cervical facial nerve branches. This continuation of the facial composite flap into the neck generates a very smooth, youthful jaw and neckline, while elevating ptotic submandibular glands and avoiding irregularities characteristic of subcutaneous neck dissection.)
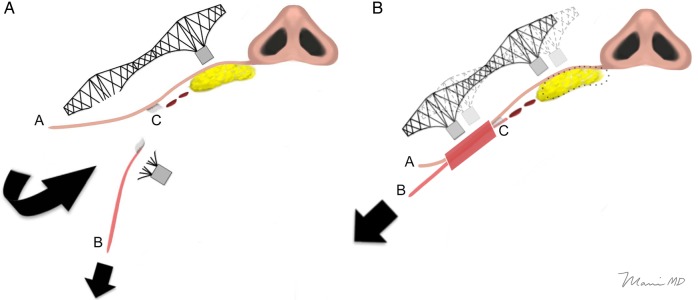
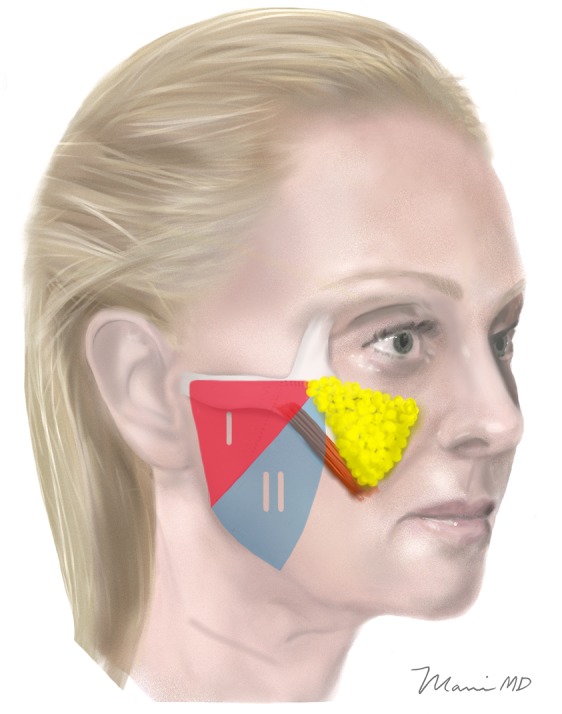
One way to conceptualize the role of the DTZ in translating SMAS elevation into the midface is that the skin is used as a “cantilever bridge.” The diagram (Figure 6A) of an axial section at the level of the nasal base illustrates what happens in a truly “bilamellar” facelift, where the skin and SMAS are separated in the DTZ. This dissection transects the first support of the “cantilever bridge” that transmits lateral SMAS tension into the malar fat pad. The image shows the skin being separated from the SMAS, and this separation extends (as it does in the traditional bilamellar SMAS lifting techniques) medially, beyond the zygomaticus muscles. Traction applied to the SMAS simply separates it farther from the malar fat pad because all durable attachments between it and the SMAS have been severed by the subcutaneous dissection. (The main vector of pull tends to be more vertical; however, the lateral vector is shown for purposes of this illustration.)
Figure 6.
(A) This diagram of an axial section at the level of the nasal base illustrates what happens in a dissection where the skin and SMAS are separated in the DTZ. This dissection transects the first support of the “cantilever bridge” that transmits lateral SMAS tension into the malar fat pad. The image shows the skin (“A”) being separated from the SMAS (“B”), and this separation extends (as it does in the traditional bilamellar SMAS lifting techniques) medially, to beyond the location of the zygomaticus muscles. Traction applied to the SMAS separates it farther from the malar fat pad because all durable attachments, including retaining ligaments (“C”), between it and the SMAS have been severed by the subcutaneous dissection. Although the main vector of pull tends to be more vertical, the lateral vector is shown for purposes of this illustration. (B) In contrast, the second diagram of an axial section where the skin (“A”) and SMAS (“B”) have been left attached to one another in the DTZ (red-shaded area) illustrates the “cantilever bridge effect” of the skin elevating the malar fat pad up as the SMAS is elevated. Traction on the SMAS transmits via the skin to the malar fat pad, which shifts superolaterally (its former location being shown by the dotted outline). Retaining ligaments (“C”) are left intact at the subcutaneous level. Although not specifically shown in this diagram, retaining ligaments are separated at the sub-SMAS level in both composite flap and bilamellar techniques.
In contrast, the second diagram (Figure 6B) of an axial section where the skin and SMAS have been left attached to one another in the DTZ (red-shaded area) illustrates the “cantilever bridge effect” of the skin elevating the malar fat pad up as the SMAS is elevated. Traction on the SMAS transmits via the skin to the malar fat pad, which shifts superolaterally (its former location being shown by the dotted outline).
METHODS
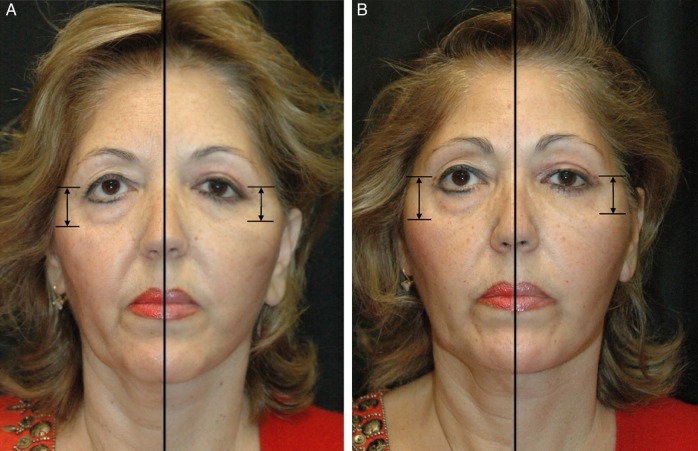
In order to test the hypothesis that maintenance of the SMAS-cutaneous supporting ligaments in the DTZ improves midface elevation during sub-SMAS facelifting, 70 patients' results (a total of 140 hemifaces) were analyzed. The author's chosen technique changed from a bilamellar to a total composite-flap dissection in March of 2010. Thus the group done after that change was compared to the group done before. A series of 35 total composite flap facelifts with 12 to 24 months' follow-up photographs available (70 hemifaces, performed over 28 months between March 2010 and June 2012) were compared to a matched group of 35 bilamellar facelifts (70 hemifaces) done during the 30 months between September 2007 and February 2010. Excluded from both groups were any patients who underwent fat transfer to the cheek or eyelid areas, or skin pinch during lower blepharoplasty (the author uses exclusively a no-touch, fat-repositioning technique during lower blepharoplasty with skin pinch added very occasionally). Midfacial elevation was measured by determining the percentage decrease in the distance from the midpupil to the lid/cheek junction on exact size-matched preoperative and postoperative frontal photographs taken under identical conditions. The midpupil was used rather than the lower lid margin since involuntary orbicularis oculi contraction can cause subtle variations in lower lid position in photographs. This measuring technique was chosen by the author as the best method of assessing a difference which had been observed clinically following conversion to the deep-plane technique, and is similar to a technique recommended by Hamra as the most objective means available of assessing facelift results.9 Figure 7 depicts the technique, with a half-and-half frontal view photograph of the same hemiface preoperatively and postoperatively. The digital measuring tool of Adobe Photoshop (Adobe, Inc., San Jose, CA) was used to quantify this percentage.
Figure 7.
Half-and-half photograph showing a mirror image of the right (A) and left (B) hemiface of a 54-year-old woman before and 12 months after total composite flap facelift, and reference marks used for measurements. The midpupil to lid/cheek junction was measured. This measuring technique is similar to that recommended by Hamra as the most objective means available of assessing midface elevation.
The author is in private practice and this study was not approved by an Institutional Review Board. The study reviews a series of cases before and after a change in technique was established. The author's technique was changed not for the purpose of this study, but rather, as noted above, in response to intraoperative findings and emerging anatomic studies related to midface SMAS structure and function. Informed consent was acquired in all cases.
Surgical Technique
In the author's technique of total composite flap facelift, the SMAS-skin flap is elevated along a vector which has been tentatively identified and marked preoperatively with the patient in the upright position, and confirmed or slightly altered based on the effect observed on the operating table. The vector in the face tends to be more vertical than lateral. The vector for neck correction is usually slightly more lateral than the face vector.
Full release of retaining ligaments between the prezygomatic and three (upper, middle, and lower) premasseteric spaces is necessary to elevate the mobile anterior face. This is a concept the author presented at the 2008 American Society for Aesthetic Plastic Surgery annual meeting, and which has been argued by Marten, Mendelson, and others.1-3,5,11-13 This pattern of release is shown in Figure 5 with areas of skin (in blue) and SMAS (in red) undermining for the author's technique, with the DTZ entirely within the red area of composite-flap dissection. The lower, middle, then upper premasseteric spaces are opened, followed by the prezygomatic space which, as noted above, is entered from a SMAS incision more anteriorly than the conventional high-SMAS technique. Once the origin of the zygomaticus major muscle is identified, dissection proceeds deep to orbicularis oculi muscle, superficially to the zygomaticus major muscle, and medially into the area of the malar fat pad, since this plane is free of facial nerve branches (and, as shown in Figure 5, is deep to malar fat but not sub-SMAS since the SMAS layer does not exist here). Retaining ligaments between the prezygomatic and premasseteric spaces are carefully separated.
An intraoperative photograph of the author's completed composite flap midface dissection is shown in Figure 8. In the photograph the zygomaticus major muscle can be seen, with the zygomatic facial nerve branch to orbicularis oculi coursing above it and marginal mandibular, zygomatic, and buccal branches (also shown) carefully identified and preserved during release of the retaining ligaments.
Figure 8.
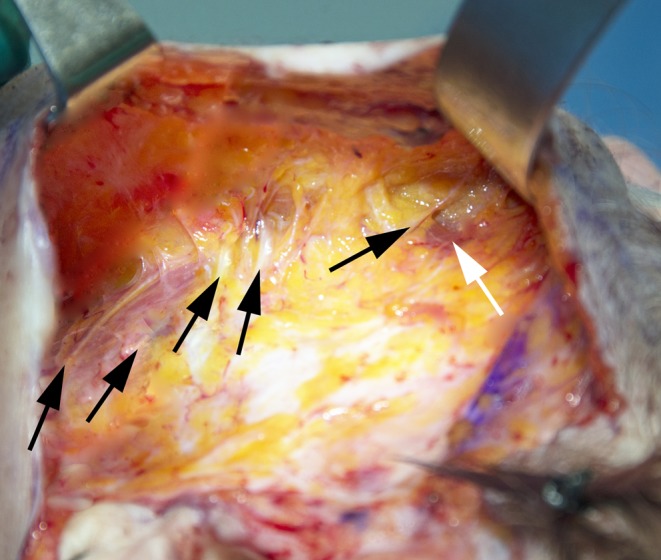
Total composite flap facelift dissection as demonstrated on a 52-year-old woman. Upper and lower key masseteric ligaments, as well as zygomatic ligaments, have been fully released. At upper right are the prezygomatic space and the origin of the zygomaticus major muscle (white arrow). Orbicularis oculi fibers have been elevated with the composite flap, and are visible being retracted above zygomaticus major. Facial nerve branches are visible and are marked by black arrows. Left to right, these branches are: marginal mandibular branch, lower buccal trunk, upper buccal trunk, zygomatic branch, and zygomatic branch to orbicularis oculi (coursing over the zygomaticus major muscle).
Dissection over the gonial angle carries an increased risk of injury to the marginal mandibular branch of the facial nerve. This is because: (1) the platysma often adheres to the inferior parotid capsule where the vertical SMAS incision line extends over the angle; and (2) this nerve branch becomes superficial as it crosses the facial artery to innervate the lip depressors. Precautions are taken to avoid marginal branch injury both preoperatively and intraoperatively. First, during preoperative marking, the patient is asked to clench the jaw and the pulse of the facial artery is palpated just anterior to the flexed masseter muscle. This point is marked and dissection is kept posteriorly to it. Second, as described by Barton,11 the subplatysmal dissection proceeds from the established sub-SMAS plane in the cheek downward and slightly anterior to the tail of the parotid, keeping the proximal marginal branch deep. After the plane is established in this manner, the vertical SMAS incision is carried over the gonial angle. The marginal mandibular branch is often identified during this dissection with careful vertical scissor spreading.
As noted above, the author's total composite flap technique joins the premasseteric dissection with extended subplatysmal dissection into the neck (Figure 6) rather than the subcutaneous elevation of previously-described modern composite flap techniques.3,11 Cervical facial nerve branches are identified and preserved. The rationale for this modification is presented in the Discussion section below.
Composite flap fixation is accomplished with interrupted horizontal mattress-style sutures of 2.0 and 3.0 Ethibond (Ethicon US, LLC, Somerville, NJ). The superior portion of the SMAS is secured to the zygomatic arch periosteum anteriorly to the course of the frontal branch of the facial nerve, and to the deep temporal fascia posteriorly to it (or to the zygomatic arch in cases where it doesn't reach). The neck portion of the SMAS/platysma is secured to the mastoid periosteum. Some of the SMAS of the composite flap will overlay the earlobe, and this portion (and only this portion) is released to allow insetting of the skin. Sutures are placed one centimeter or less apart from SMAS of the flap into fixed SMAS posteriorly to complete the flap fixation. A video demonstrating the surgical technique can be viewed at www.aestheticsurgeryjournal.com.
RESULTS
Measurements showed that maintaining skin-SMAS attachments in the DTZ resulted in significantly greater midface elevation. Average follow-up time in both groups was 18 months (range, 12-24 months). In the group operated on prior to maintenance of those attachments in the DTZ, the mean percentage of midfacial elevation at an average 18 months postoperative was 5.5% (range, 0.0%-17.8%). Examples of before and after photographs from this group are shown in Figure 9 and Supplemental Figures S1 and S2. In the subsequent group, the mean percentage of midfacial elevation at an average 18 months postoperative was 11.7% (range, 0.1%-32.3%). Examples from this group are shown in Figure 10 and Supplemental Figures S3-S6 (postoperative photographs later than 24 months are shown in some cases to illustrate longevity of initial results). Using the unpaired t test, the difference between the two groups was statistically significant, with a P-value of less than 0.05. Complications were minimal, with one unilateral hematoma in a male patient in the earlier group (1.4% incidence), and one temporary frontal branch palsy (1.4%) in the earlier group which resolved within 3 months. One patient (1.4%) in the later group underwent revision for recurrent laxity, which was done at 18 months postoperative.
Figure 9.
Example of a bilamellar facelift (early group). This 56-year-old woman complained of general facial aging and said that people thought she looked angry even when she was not. On examination she had moderate midfacial deep tissue ptosis, deepening nasolabial folds, and jowling, as well as platysmal laxity. (A, C) Preoperative and (B, D) 24 month postoperative photographs of a facelift with skin and SMAS raised as separate flaps in the DTZ and midline corset platysmaplasty. She also underwent endoscopic browlift and upper blepharoplasty. The elevation of midfacial highlights in this case was negligible.
Figure 10.
Example of a total composite flap facelift (later group). This 54-year-old woman (same patient featured in Figure 7) complained of looking tired and droopy. Examination showed severe ptosis of mid- and lower deep facial tissues, platysmal laxity, and upper and lower lid blepharochalasis. (A, C) Preoperative and (B, D) 14 month postoperative photographs of a facelift with skin and SMAS left attached in the DTZ. She also underwent midline corset platysmaplasty with digastric shaving and partial inferior platysmal transection, upper blepharoplasty, and transconjunctival lower blepharoplasty with fat repositioning. Elevation of midfacial highlights was significant in this case (16% on right and 10% on left). The incision is not visible and the jawline is restored, without excessive thinning of the tissues which can occur with lateral neck skin undermining.
The average age in the earlier group was 55 years (range, 42-75 years). In the later group, the average age was 53 years (range, 43-69 years). The earlier group consisted of 29 females and 6 males, and the later group had 30 females and 5 males.
DISCUSSION
The results of this study suggest that there is an advantage to maintaining a composite flap dissection in the zone lateral and parallel to the lateral border of the zygomaticus major, medial to which the SMAS begins to attenuate both structurally and functionally according to recent studies.6,7 However, other conceptions of SMAS midface anatomy − that the SMAS invests the zygomaticus major muscles, or that it extends to, and invests, the nasolabial fold − can be considered also. When this is done, it turns out that a composite flap still may work best.
Some cadaver dissections have drawn different conclusions from Gassner et al regarding the anatomy of the SMAS in the midface. One of them suggests that it invests the zygomaticus major and minor muscles.14 This echoes the belief of many surgeons with a large experience in this anatomic area such as Owsley.15 However, if SMAS does indeed invest these muscles, sub-SMAS dissection must switch to the subcutaneous plane in the area lateral to them, since the muscles themselves cannot be elevated without distorting their action and endangering facial nerve branches deep to them. And therefore, in this case as well, skin and SMAS must be left attached to one another in the more lateral DTZ to transfer any lateral SMAS tension into the midface.
What about the possibility that the SMAS continues medially, as a separate layer superficial to the zygomaticus muscles, and invests the nasolabial fold itself, as some surgeons have maintained?16,17 In this scenario, traction on the SMAS – if dissected separately from the skin all the way to the nasolabial fold − will only accentuate the nasolabial fold. In their 2010 article Sundine and Connell argue against this commonly-held view, based on their experience in over 1000 SMAS facelifts in the past decade which show excellent nasolabial fold effacement gained through intraoperative SMAS traction.17 However, their technique – appropriately – does not undermine skin as a separate layer in the anterior cheek: “(t)he anterior cheek, which has connections from the SMAS to the skin, is not undermined because this would lose a major support of the SMAS to the incisions in the temporal area and would not result in the pleasing concavity that occurs when the attachments from the anterior SMAS to the skin are left intact.”17 Of course, as discussed above, based on the findings of recent anatomic studies, the SMAS does not exist as a durable layer in the anterior cheek, and it is the SMAS-skin attachments in the slightly more lateral DTZ which allow this “pleasing concavity.” In other words, if indeed there is no SMAS layer in the anterior cheek, as Gassner's study suggests, then by definition there can be no SMAS-skin attachments in the anterior cheek. Those attachments exist in the more lateral cheek and should be exploited there in just the way Sundine and Connell describe more anteriorly (Figures 2 and 5).
So, while recent studies suggest that the SMAS layer attenuates in the midface, all of the three major possibilities of SMAS midface anatomy support maintaining a composite flap in the DTZ. Additionally, given the functional studies showing the inferomedial SMAS to be significantly weaker, its anatomy in the midface as a separate layer of surgical significance becomes irrelevant.
One other alternative to midface elevation is a dissection done via a transcutaneous lower blepharoplasty incision. This incision does preserve orbicularis oculi innervation and function, including the blink reflex which comes from a buccal branch medially.18 However, some surgeons (the author included) avoid transcutaneous approaches to lower blepharoplasty, and moreso, midface lifting via lower blepharoplasty, given the fact that they: (1) necessarily violate two lamellae of the lower lid, leading to an increased risk of scleral show; and (2) require a slightly longer skin incision than doing a minor “skin pinch” (only when necessary). Midface lifting through a subciliary incision elevates the cheek along an unnatural vertical vector which does not reverse the actual inferomedial vector of aging, as well as causing some orbicularis oculi denervation with a “frozen” look, and (as with skin-muscle lower blepharoplasty) a greater risk of scleral show.
Aside from the necessity of maintaining skin and SMAS attachments in the DTZ, the sub-SMAS release of zygomatic- and masseteric-cutaneous ligaments is a key principle presented here which has been argued in the past, as noted in the Introduction above.1-3,5,11-13 There are other facelift approaches which attempt to address midface elevation without this sub-SMAS release. In SMAS plication, MACS lift, or SMAS-ectomy procedures, release of the zygomatic and masseteric-cutaneous retaining ligaments is done if subcutaneous facelift dissection extends anteriorly enough. However, this occurs at a more superficial level while the SMAS is manipulated without release of the ligaments. Therefore elevation of the mobile anterior face is either dependent upon sutures into fatty tissue or, if placed into SMAS fibers, counteracted by the downward pull of these fixed ligaments, and less likely to be effective or durable. Releasing these retaining ligaments at the deeper level allows the volume of the anterior facial tissues to be lifted in a way that reverses the aging process more anatomically.
In a subcutaneous lateral-to-medial midface dissection, the skin might still be considered a “cantilever” to carry the malar fat pad upward, with “quilting” type sutures used to anchor the skin flap superiolaterally. However, in this situation: (1) the quilting suture it would cause a dimple; and (2) its effect would be lost when the dimple relaxed. Indeed, others have found that the longevity of this type of “deep-subcutaneous” malar fat elevation technique was limited, most likely due to the distance between the malar fat pad and the fixation point of the skin (essentially, at the skin incision point above the tragus).9 Since the lower, sub-SMAS portion of his procedure remained elevated in the long term, jawline contour was maintained, but the subcutaneously-dissected malar fat elevation failed.
An alternative to elevation of midface tissues is volume addition in the form of fillers or the more potentially permanent autologous fat transfer. These types of volume addition can be used to improve anterior cheek highlights; however, they are less predictable than surgical elevation and not only do not correct, but can exacerbate the depth of aging nasolabial folds.
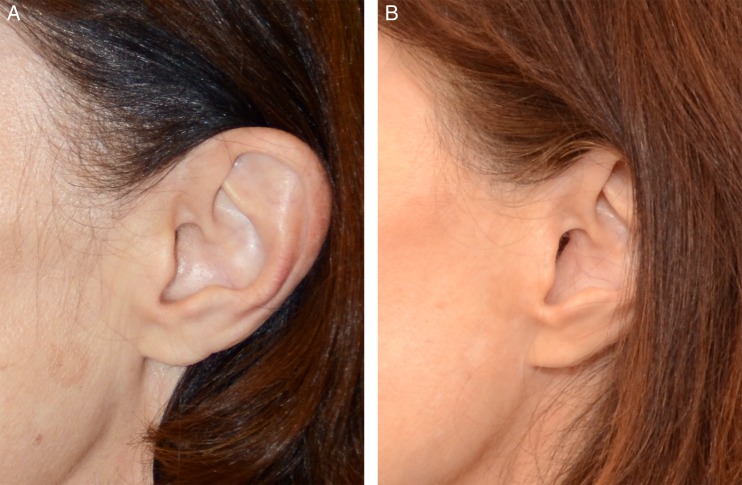
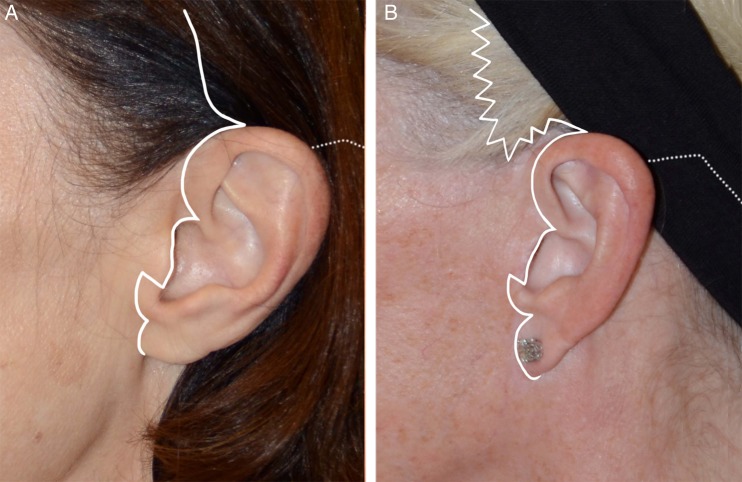
A dissection technique where the DTZ is maintained lateral to the midface avoids these potential pitfalls of transcutaneous lower lid incision for cheek dissection while maintaining a uniform, appropriately-vectored composite flap to lift neck, jawline, and midface harmoniously. The author's technique uses a point of fixation for the upper SMAS cuff that is proximal enough to the malar fat to elevate it effectively and durably. Another advantage of composite-flap elevation is that tension on the skin incisions is more reliably eliminated. Examples of incision design and healed skin incisions are shown in Figures 11-13. The postauricular incision design is not shown but the incision runs up the postauricular sulcus and just within the posterior hairline, acutely beveled so that hair grows through the hairless edge of the flap as it heals.
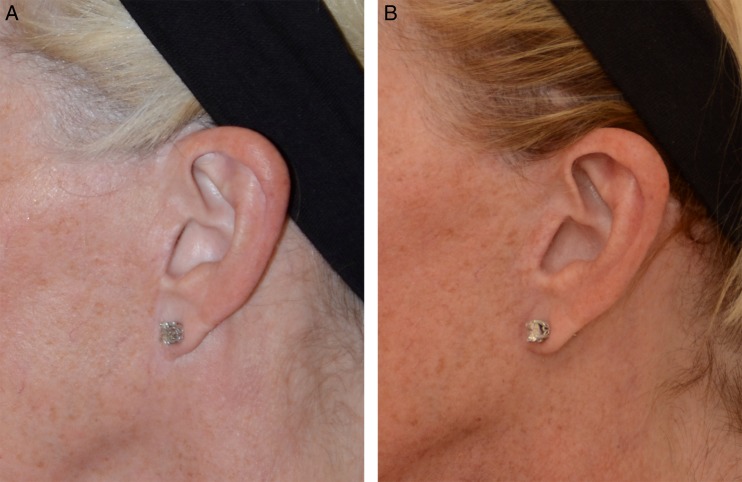
Figure 12.
(A) Preoperative photograph of this 57-year-old woman's ear (same patient in Figure 11A). (B) Fifteen-month postoperative photograph after primary total composite flap facelift, showing preservation of the tragal contours and the intertragal incisure below the tragus. The incision is essentially invisible even on close inspection.
Figure 11.
(A) Incision diagram for primary total composite flap facelift demonstrated on a 57-year-old woman. The incision begins in the temporal hair and angles posteriorly just above the helical root. It then curves downward and makes a sharp posterior angle just above the tragus, then continues just behind the crest of the tragus, turning acutely supero-anterior at the base of the tragus and then following the contour of the intertragal incisure to the upper ear lobe, with a notch just superior to the lobe and then around it. (The postauricular incision runs up the postauricular sulcus and just within the posterior hairline, acutely beveled so that hair grows through the hairless edge of the flap as it heals.) (B) Preauricular incision design for secondary total composite facelift demonstrated on a 60-year-old woman. To avoid raising the sideburn, the incision begins behind the anterior 1/3 of the sideburn with w-plasties which course under the sideburn as depicted. The remainder of the incision is the same as in Figure 11A.
Figure 13.
(A) Preoperative photograph of this 60-year-old woman's ear (same patient in Figure 11B). The scar from a previous facelift (done by another surgeon) is visible and shows a truncated tragus as well as a vertical line over the intertragal incisure. The ear lobe is also attached at the scar. (B) Thirteen-month postoperative photograph after secondary total composite flap facelift. The sideburn has not been raised, and the tragal contours have been re-established. The intertragal incisure has been restored. The ear lobe now hangs normally.
Less relevant to the midface effect, but still worthy of discussion, is the author's composite flap (“Skoog-type”) neck dissection. A criticism of this technique has been that the neck skin often ages faster than platysma, so it should be undermined separately.3 However, several points support using a composite flap in the neck: (1) even in cases of accelerated neck aging, the neck skin remains attached to platysma muscle, and extensive subplatysmal undermining and advancement carries a significant amount – often 3 to 5 cm – of skin to be removed; (2) although cervical facial nerve branches will be encountered and should be preserved, the subplatysmal plane in the neck opens up even more readily than that in the face with no specific ligaments to be released (both of which may explain why the neck sometimes ages faster than the face); (3) as in the face – and even moreso – irregularities resulting from separate skin dissection are avoided; (4) elevation of a face-neck composite flap as one unit means that the neck portion supports the face portion rather than exerting downward traction on it; (5) ptotic submandibular glands, which are subplatysmal, are elevated and supported; and (6) restoration of platysma to its original position over the mandibular border creates a smoother, fuller jawline (Figure 10D and Supplemental Figure S5D).
This study has its limitations as well as potential unique benefits. Although the results showed statistically significant improvement in midface elevation with the composite-flap dissection, the sample size is limited. Also, while better for simplicity of study design, measurement of one dimension of midface elevation on a two-dimensional photograph is only one of many ways of judging an operation whose results are three-dimensional and sculptural.
The main way in which this study aims to enhance the knowledge base of facial rejuvenation surgery is by applying the latest knowledge of SMAS structure and function to surgical technique. This could be the continuing benefit of this and other similar future studies. The unique aspect of the author's technique is the composite flap (including suborbicularis oculi) midface dissection which begins more anteriorly in its uppermost section than high-SMAS techniques previously described, combined with composite skin-platysma (Skoog-type) dissection in the neck comprising a “total composite flap” face and necklift.
CONCLUSION
In SMAS-release facelifting, subcutaneous dissection beyond the DTZ destroys the “cantilever bridge” skin connection between SMAS laterally and malar fat medially. This type of bilamellar dissection may not be helpful anyway, since tight connective tissue attachments between skin and underlying SMAS indicate that gravity does not pull the skin in a separate direction from the SMAS. The extension of midface sub-SMAS dissection beyond the vertical line of ligamentous attachments just lateral to the mimetic muscles (described most clearly by Mendelson4) defines the “SMAS release” lift; and as noted above, this is a critical step towards a smooth and uniform correction of mid- and lower-face deep tissue ptosis. But the anatomy and physical strength of the SMAS as it courses into the midface has to be considered very carefully when deciding how far to undermine skin. Only if the DTZ is preserved can that extended release achieve optimal midface elevation.
Supplementary Material
This article contains supplementary material located online at www.aestheticsurgeryjournal.com.
Disclosures
The author declared no potential conflicts of interest with respect to the research, authorship, and publication of this sarticle.
Funding
The author received no financial support for the research, authorship, and publication of this article.
Supplementary Material
REFERENCES
- 1.Connell BF, Semlacher RA. Contemporary deep layer facial rejuvenation. Plast Reconstr Surg. 1997;1006:1513-1523. [DOI] [PubMed] [Google Scholar]
- 2.Marten TJ. High SMAS facelift: combined single flap lifting of the jawline, cheek, and midface. Clin Plast Surg. 2008;354:569-603. [DOI] [PubMed] [Google Scholar]
- 3.Hamra ST. Composite rhytidectomy. Plast Reconstr Surg. 1992;901:1-13. [DOI] [PubMed] [Google Scholar]
- 4.Skoog T. Plastic Surgery: New Methods and Refinements. Philadelphia: Saunders, 1974:1306-1342. [Google Scholar]
- 5.Mendelson B. Facelift anatomy, SMAS retaining ligaments and facial spaces. In: Aston SJ, Steinbrech DS, Walden JL, eds. Aesthetic Plastic Surgery. London, UK: Saunders Elsevier; 2009:53-72. [Google Scholar]
- 6.Gassner HG, Rafii A, Young A, Murakami C, Moe KS, Larrabee WF Jr.. Surgical anatomy of the face: implications for modern face-lift techniques. Arch Facial Plast Surg. 2008;101:9-19. [DOI] [PubMed] [Google Scholar]
- 7.Hu X, Wang Z, Wang Q, Zhang C, Hu G, Qin H. Are There Differences Between the Upper and Lower Parts of the Superficial Musculoaponeurotic System? A Preliminary Biomechanical Study. Aesthet Surg J. 2014;345:661-667. [DOI] [PubMed] [Google Scholar]
- 8.Mendelson BC. Discussion of: Hamra ST. A study of the long-term effect of malar fat repositioning in face lift surgery: short-term success but long-term failure. Plast Reconstr Surg. 2002;1103:952-955. [DOI] [PubMed] [Google Scholar]
- 9.Hamra ST. A study of the long-term effect of malar fat repositioning in face lift surgery: short-term success but long-term failure. Plast Reconstr Surg. 2002;1103:940-951. [DOI] [PubMed] [Google Scholar]
- 10.Trussler AP, Hatef D, Broussard GB, Brown S, Barton FE. The viscoelastic properties of the SMAS and its clinical translation: firm support for the high-SMAS rhytidectomy. Plast Reconstr Surg. 2011;1283:757-764. [DOI] [PubMed] [Google Scholar]
- 11.Barton FE., Jr. The “high SMAS” face lift technique. Aesthet Surg J. 2002;225:481-486. [DOI] [PubMed] [Google Scholar]
- 12.Mendelson BC. Surgery of the superficial musculoaponeurotic system: principles of release, vectors, and fixation. Plast Reconstr Surg. 2001;1076:1545-1552. [PubMed] [Google Scholar]
- 13.Mani ME. Midface Lifting: How and Why. Presented at the American Society for Aesthetic Plastic Surgery Annual Meeting, San Diego, CA, May 2008. [Google Scholar]
- 14.Macchi V, Tiengo C, Porzionato A et al. Histotopographic study of the fibroadipose connective cheek system. Cells Tissues Organs. 2010;1911:47-56. [DOI] [PubMed] [Google Scholar]
- 15.Owsley JQ. Lifting the malar fat pad for correction of prominent nasolabial folds. Plast Reconstr Surg. 1993;913:463-474. [PubMed] [Google Scholar]
- 16.Mitz V, Peyronie M. The superficial musculo-aponeurotic system (SMAS) in the parotid and cheek area. Plast Reconstr Surg. 1976;581:80-88. [DOI] [PubMed] [Google Scholar]
- 17.Sundine MJ, Connell BF. Analysis of the effects of subcutaneous musculoaponeurotic system facial support on the nasolabial crease. Can J Plast Surg. 2010;181:11-14. [PMC free article] [PubMed] [Google Scholar]
- 18.McCord CD, Walrath JD, Nahai F. Concepts in eyelid biomechanics with clinical implications. Aesthet Surg J. 2013;332:209-221. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.