Abstract
A 10-year-old golden retriever dog was presented for chronic right forelimb lameness associated with a painful swelling at the lateral aspect of the proximal ulna. Proximal ulnar ostectomy and stabilization resulted in a good clinical outcome. The proposed diagnosis is chronic desmitis and enthesiophytosis of the radio-ulnar interosseous ligament.
Résumé
Desmite chronique et enthésiophytose du ligament interosseux radio-ulnaire chez un chien. Un Golden retriever de 10 ans a été présenté pour boiterie chronique du membre thoracique droite associée à un gonflement douloureux à l’aspect latéral de l’ulna proximal. Une ostéotomie ulnaire proximale avec stabilisation ont permit un bon résultat clinique. Le diagnostic proposé est une desmite chronique et enthésiophytose du ligament interosseux radio-ulnaire.
(Traduit par Isabelle Vallières)
Case description
A 10-year-old spayed female golden retriever dog was presented with a 2-month history of right forelimb lameness without known trauma. The referring veterinarian prescribed the non-steroidal anti-inflammatory drug (NSAID) meloxicam (Metacam; Boehringer-Ingelheim, Burlington, Ontario), 0.1 mg/kg body weight (BW), PO, q24h, for 1 wk; this was associated with significant improvement of the lameness. After moderately intense activity, the dog exhibited severe lameness. Upon presentation to the Veterinary University Hospital Center of the Faculty of Veterinary Medicine of the University of Montreal, the dog exhibited lameness which was moderate at the walk and severe at the trot. All lameness evaluations were subjective. No significant findings were noted upon general physical examination other than the alteration in gait.
Orthopedic examination findings included moderate right antebrachial muscle atrophy when subjectively comparing it to the contralateral limb and a firm swelling (3 cm × 1 cm × 1 cm) at the cranio-lateral aspect of the proximal portion of the ulna, extending onto the cranial aspect of the radius. Marked pain was elicited upon palpation of this region even under sedation. Pronation and supination were particularly painful. The rest of the orthopedic examination was unremarkable. Radiographs of the affected antebrachium were acquired. Increased opacity in the radius and ulna corresponded to the firm swelling noted on the physical examination. There was an ulnar osseous proliferation extending towards the radius (Figure 1). Contralateral antebrachial radiographs were taken and were considered normal. Computed tomography (CT) was performed to further characterize this lesion. The study confirmed a pointed, triangular proliferation of the ulna oriented toward the radius with a reactive proliferation of the radius surrounding the ulnar projection (Figure 2). The lesions appeared to be chronic and inactive. The borders were regular, well-defined, and surrounded by sclerotic bone suggesting a chronic inflammation of the interosseous ligament with a secondary osseous proliferation of the radius and ulna. A neoplastic process seemed unlikely considering the organization of the lesion, but could not be excluded without a biopsy.
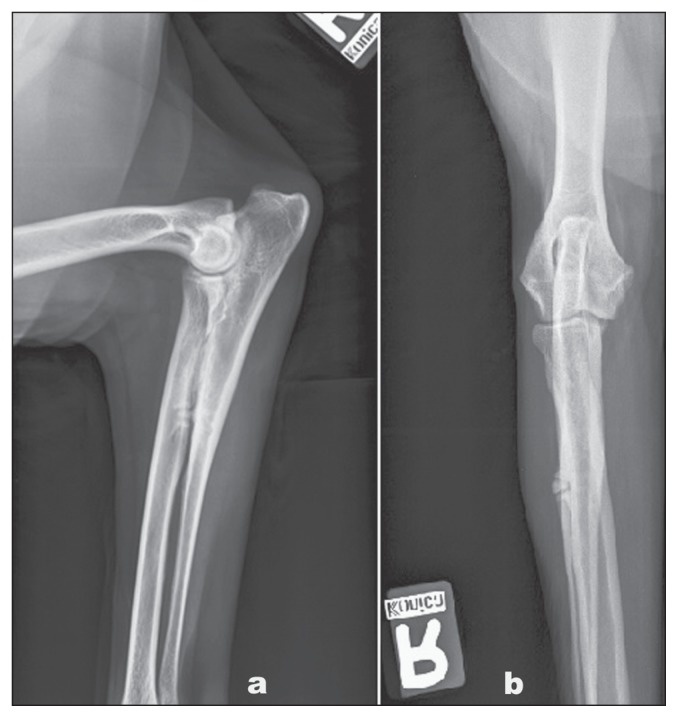
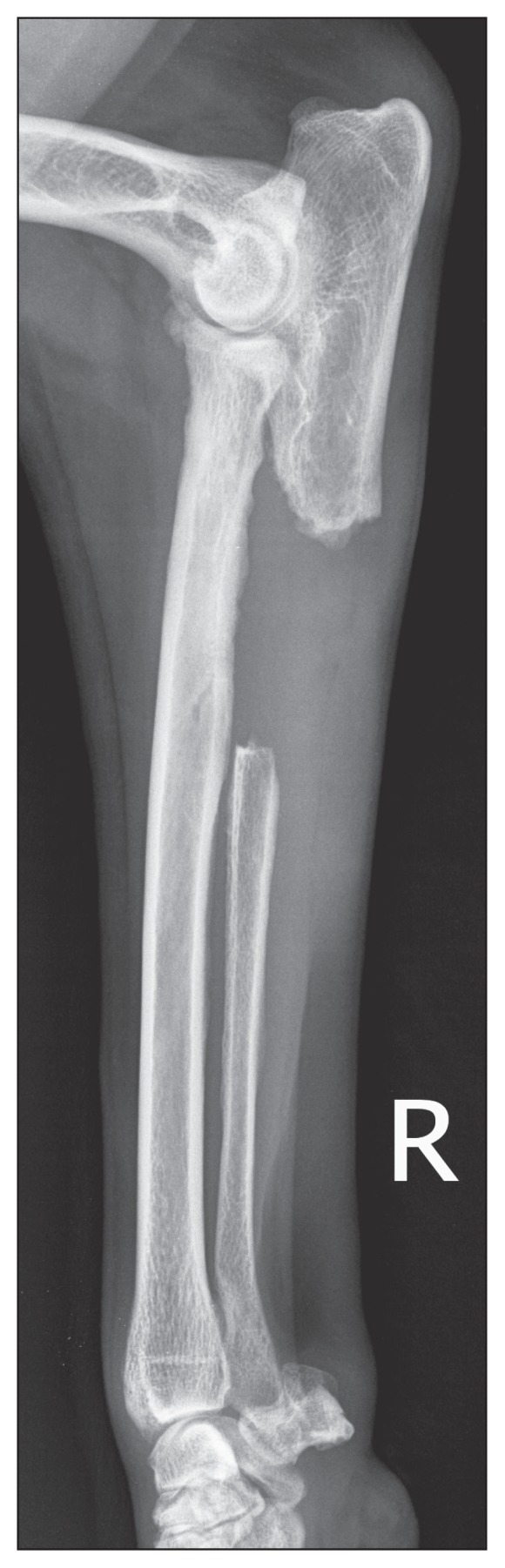
Figure 1.
Lateral (a) and cranio-caudal (b) radiographs of the right antebrachial region of a 10-year-old neutered female golden retriever dog presented with a 2-month history of right forelimb lameness. There was an increase in bone opacity of the radius and ulna density corresponding to the firm swelling that was present, with a suspicion of ulnar proliferation extending towards the radius.
Figure 2.
Computed tomography reconstructed images of the right antebrachial region to further characterize the lesion. The study confirmed a pointed/triangular proliferation of the ulna towards the radius with a reactive proliferation of the radius surrounding the ulnar projection.
Because medical treatment consisting of an analgesic (Tramadol; Gentes et Bolduc, St. Hyacinthe, Quebec) 3 mg/kg BW, PO, q12h, an NSAID (meloxicam), 0.1 mg/kg BW, PO, q24h, and rehabilitation had already been pursued and proven ineffective, surgical treatment was considered. To the authors’ knowledge, there has been no description in the literature of any surgical treatment for a bony proliferative lesion located at the insertion of the interosseous ligament between the radius and the ulna. Two surgical options were presented and explained to the owners: i) curettage of the proliferative lesion to decrease contact between the radius and ulna, or ii) ulnar ostectomy. The owners opted for ulnar ostectomy.
A lateral approach to the ulna was performed as previously described (1). This approach allowed us to identify the irregular proliferation from the ulna that extended towards the radius. A single well-defined bone spur was not identified. Rather, a 3 cm × 1 cm × 1 cm proliferation originating from the cranio-medial aspect of the ulna, in close contact with the cranio-lateral aspect of the radius was observed. A larger ulnar ostectomy than planned before surgery was done because the precise dimensions of the proliferation could not be outlined with the imaging modalities used (Figure 3a intra-operative; 3b ex-vivo). A 1 cm segment of the proximal interosseous ligament was preserved in an attempt to stabilize the proximal portion of the ulna (Figures 4a, 4b). The dog recovered uneventfully from surgery.
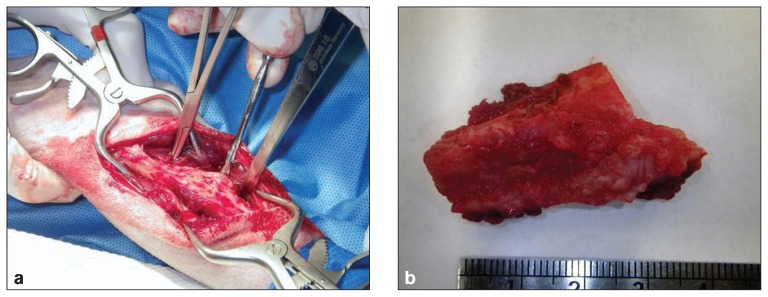
Figure 3.
a — Intra-operative image of the cranio-lateral approach to the ulna. This approach allows identification of an irregular proliferation from the ulna to the radius. b — Ex-vivo image of the ulnar ostectomy; note the irregular proliferation.
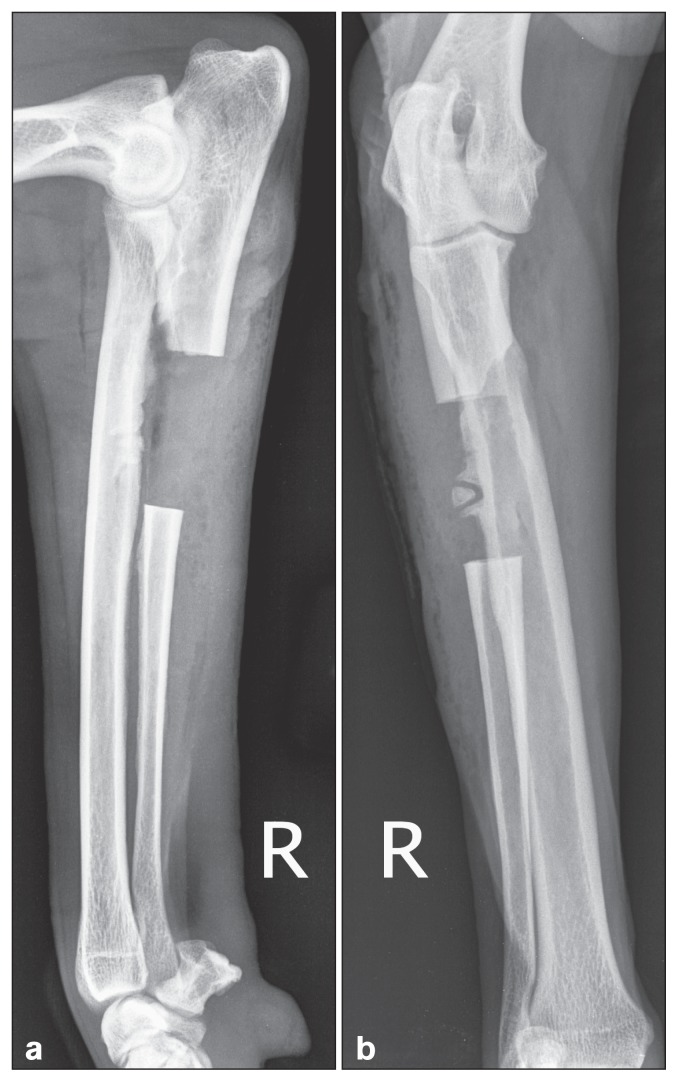
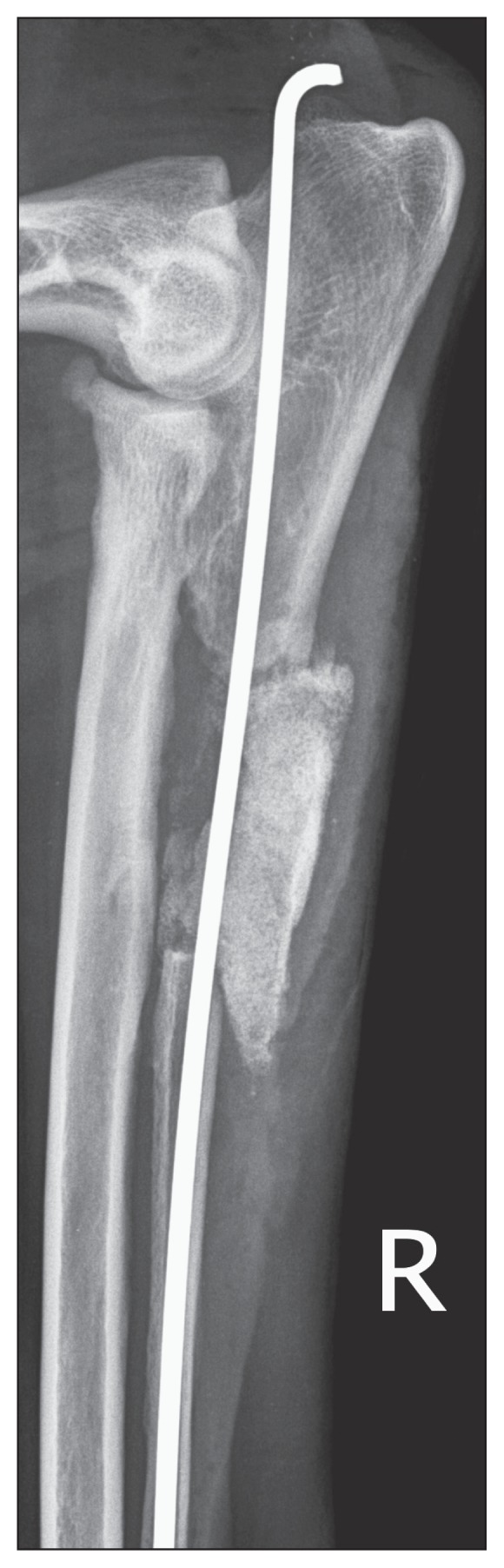
Figure 4.
a — Lateral post-operative radiograph of the right antebrachium following ulnar ostectomy. b — Cranio-caudal postoperative radiograph of the right antebrachium following ulnar ostectomy.
A 3.5 cm × 2.5 cm × 1 cm segment of ulna including portions of the interosseous ligament was submitted for histopathological analysis. Sections of the interosseous ligament consisted of bundles of mature collagen fibers, areas of fibrocartilage, and a few blood vessels and nerves surrounded by loose connective tissue. The fibrocartilage appeared multifocally degenerate and some lacunae were empty. Trabeculae of woven bone had proliferated from the cortex of the ulna and elevated the periosteum (Figure 5). There was no evidence of neoplasia. Based on the clinical and radiographic evaluations, CT, and histopathology results, a diagnosis of chronic desmitis and enthesiophytosis of the radio-ulnar interosseous ligament was proposed.
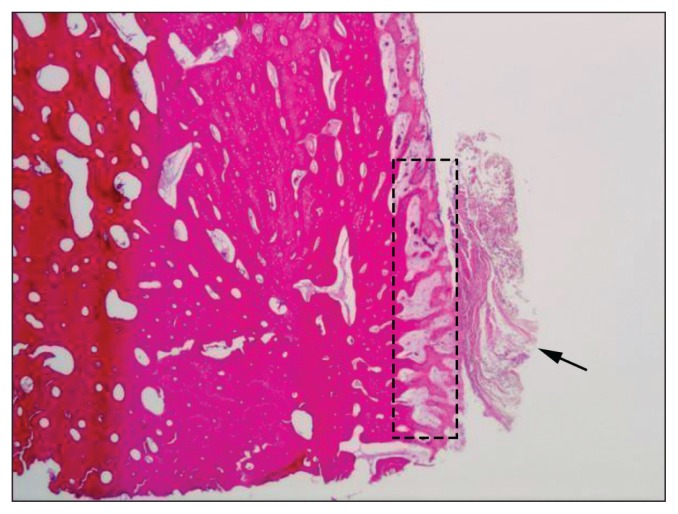
Figure 5.
Photomicrograph taken from the submitted ulna and portions of the interosseous ligament (arrow). Trabeculae of woven bone (rectangle) have proliferated from the cortex of the ulna and elevated the periosteum by 1 to 3 mm. There is no evidence of a neoplastic process.
The dog was discharged 4 d after the surgery and recovered well following surgical treatment. Lameness improved significantly until 10 wk after surgery when the lameness acutely reoccurred. Moderate lameness was observed at the walk and the trot. Furthermore, the proximal part of the ulna was palpably unstable upon elbow flexion and caudal subluxation of the distal aspect of the proximal portion of the ulna was palpated. We suspected an acute tear of the remnant of the proximal interosseous ligament. We observed caudal displacement of the distal portion of the proximal ulna on follow-up radiographs when compared to immediate post-operative radiographs (Figure 6). Surgical stabilization of the proximal ulna was performed using an intramedullar pin in combination with a bioglass graft (Consil Orthopedic; Nutramax Laboratories, Englewood, Maryland, USA; Figure 7). Despite instructions to the owners to confine the dog during the postoperative course, the dog was not kept confined. Two weeks after the second procedure, the implant migrated proximally by 2 cm (Figure 8) and had to be removed. External coaptation using a modified Robert-Jones bandage reinforced with a molded lateral splint (Delta-Lite Cast; BSN Medical, Laval, Quebec) supported the ostectomy site for an additional 4 wk while the critical defect consolidated. Physical, orthopedic, and radiological evaluations were performed at week 20. Palpation revealed a stable, non-painful distal aspect of the proximal portion of the ulna. As noted on the lateral radiograph (Figure 9), the proximal ulnar segment did not seem to have migrated further caudally; bioglass resorption or migration was not noted. Proximal and distal gap consolidation were incomplete.
Figure 6.
Lateral radiograph of the right antebrachium of suspected acute tear interosseous ligament at 10 wk after the ulnar ostectomy. Caudal subluxation of the distal aspect of the proximal portion of the ulna can be observed. Moderate osteoarthritis (osteophytes on the cranial aspect of the radial head) is noted and could be secondary to destabilization of the proximal ulna.
Figure 7.
Post-operative medio-lateral radiograph after surgical stabilization of the proximal ulna using an intramedullary pin in combination with a bioglass graft.
Figure 8.

Lateral radiograph of the right antebrachium at 12 wk. The intramedullary pin had significantly migrated proximally and was exhibiting plastic deformation (bending).
Figure 9.

Lateral radiograph of the right antebrachium at 20 wk.
At the 11-month follow-up visit, there was no lameness at walk and only mild lameness present at the trot. The dog had regained subjectively painless full motion of its right forelimb; pronation and supination were not painful. The functional recovery, however, was not objectively documented.
Discussion
The anatomy of the radius and ulna joint and the interosseous ligament vascular supply are well-described (2). A syndesmotic joint unites the radius and ulna. The ulna is considered to be a fixed segment. The radius revolves around the ulna. The space between the radius and the ulna is closed by a fibrous sheet called the interosseous membrane, which has multiple vascular openings. A strong interosseous ligament is located at the junction of the proximal and middle third of the lateral aspect of the radius and ulna. This ligament is used to reinforce the interosseous membrane. The major blood supply to the interosseous ligament is derived from the common interosseous artery arising from the median artery at the proximal quarter of the forearm and giving rise to the interosseous palmar artery and an interosseous dorsal artery, respectively (3). The interosseous palmar artery is the largest and is located at the palmar side of the interosseous membrane dividing into a palmar ramus and an interosseous ramus. The ulnar artery is another branch which joins the collateral ulnar artery arising from the brachial artery.
Diseases associated with chronic thoracic limb lameness include degenerative and developmental diseases of the shoulder, elbow, and carpal joints, traumatic ligamentous damages, medullary inflammation, fractures, primary or secondary osseous neoplastic lesions, other non-osseous neoplastic processes, and lameness of neurologic origin such as cervical disk disease and peripheral nerve tumors. Infectious or immune-mediated diseases must also be considered. This case report introduces a new differential diagnosis for chronic thoracic limb lameness associated with bony proliferation. As reported by Benjamin et al (4), enthesiophytes or bony spurs are bony outgrowths that extend from skeletal structures into the soft tissues of tendons or ligaments at their attachments. In contrast, osteophytes form around the articular surfaces of synovial joints (5) in patients afflicted with osteoarthritis. Rogers et al (5) suggested that, in humans, enthesiophyte and osteophyte formation represent a skeletal response to stress. They proposed that enthesiophytes represent an adaptation to ligament injury as osteophytes are an adaptation to joint injury in order to modify the loading on synovial joints whose stability or function has been compromised. Benjamin et al (6) suggested that endochondral ossification could play a role in enthesiophyte formation. There seems to be an extension of normal enthesis growth and their longitudinal orientation along the axis of the ligament reflects the orientation of the rows of fibrocartilage cells. We suggest that chronic desmitis and enthesiophytosis best describe the process in our patient. Histopathological results tend to support our proposition.
The diagnosis of interosseous ligament disease is one of exclusion. Pain has to be localized to the area of the interosseous ligament, and elicited with pronation/supination. All other potential sources of lameness have to be excluded after investigation when judged appropriate. Medical management consisting of rest/exercise restriction combined with NSAIDs with or without the use of analgesics seems to be mostly effective. Patients which do not respond to medical management become surgical candidates.
In our patient, surgical treatment was recommended following unsatisfactory results using medical management. Radiographs and CT were used to further describe the painful lesion and to plan surgical management. An MRI with angiography could have been useful to investigate an eventual ischemic lesion and would have helped to further delineate the extent of the lesion, thus allowing more precise surgical treatment. The objective of the operative technique was to eliminate direct contact between the radius and ulna in the region of interest, while maintaining a healthy proximal part of the interosseous ligament with the goal of allowing stabilization of the proximal part of the ulna (7). A limited segmental ulnar ostectomy was performed in this patient. The length of the ostectomy was larger than previously planned which left us with a limited length of radio-ulnar ligament and a destabilized proximal ulna. Local curettage and debridement could also have been used; however, the possibility of post-operative reformation of this lesion was unknown. During the postoperative care, the dog exhibited lameness associated with instability of the distal aspect of the proximal ulna subsequent to a suspected tear of the ligament. In retrospect, a better approach would have been to immediately stabilize the ulna with an implant and a bioglass/bone graft because of the creation of a critical-sized defect. Removing the interosseous ligament at the same time as the ostectomy with concurrent stabilization could also be recommended as it potentially eliminates the source of pain and could prevent local synostosis. If an ulnar ostectomy is performed, we recommend immediate stabilization to prevent the caudal subluxation of the proximal ulna, which, as observed in this patient, could result in the rapid development of osteoarthritis of the elbow joint. As noted on the lateral radiograph (Figure 6), there was rapid development of osteophytes on the cranial aspect of the radial head.
The differential diagnosis of chronic thoracic limb lameness associated with a firm swelling localized at the site of insertion of the interosseous ligament must now include chronic desmitis and enthesiophytosis of the radio–ulnar interosseous ligament. CVJ
Footnotes
Use of this article is limited to a single copy for personal study. Anyone interested in obtaining reprints should contact the CVMA office (hbroughton@cvma-acmv.org) for additional copies or permission to use this material elsewhere.
References
- 1.Piermattei DL, Gilson SD, Schwarz PD. Treatment of humeroulnar sub-luxation with a dynamic proximal ulnar osteotomy. A review of 13 cases. Vet Surg. 1989;18:114–122. doi: 10.1111/j.1532-950x.1989.tb01053.x. [DOI] [PubMed] [Google Scholar]
- 2.Evans HE, Lahunta A. Angiology. In: Evans HE, Lahunta A, editors. Miller’s Anatomy of the Dog. 4th ed. St. Louis, Missouri: Saunders; 2012. pp. 641–642. [Google Scholar]
- 3.Barone R. Angiologie. In: Barone R, editor. Anatomie comparée des mammifères domestiques. Paris, France: Vigot; 1996. pp. 250–251. [Google Scholar]
- 4.Benjamin M, Toumi H, Ralphs JR, Bydder G, Best TM, Milz S. Where tendons and ligaments meet bone: Attachment sites (“entheses”) in relation to exercise and/or mechanical load. J Anat. 2006;208:471–490. doi: 10.1111/j.1469-7580.2006.00540.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rogers J, Shepstone L, Dieppe P. Bone formers: Osteophyte and enthesophyte formation are positively associated. Ann Rheum Dis. 1997;56:85–90. doi: 10.1136/ard.56.2.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Benjamin M, Rufai A, Ralphs JR. The mechanism of formation of bony spurs (enthesophytes) in the Achilles tendon. Arth Rheum. 2000;43:576–583. doi: 10.1002/1529-0131(200003)43:3<576::AID-ANR14>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 7.Might K, Hanzlik KA, Case JB, et al. In vitro comparison of proximal ulnar osteotomy and distal ulnar osteotomy with release of the interosseous ligament in a canine model. Vet Surg. 2011;40:321–326. doi: 10.1111/j.1532-950X.2011.00805.x. [DOI] [PubMed] [Google Scholar]