Abstract
INTRODUCTION
Extraosseous osteosarcomas are rare, accounting for approximately 4% of all osteosarcomas. A literature review yields very few cases of osteosarcoma primarily arising from the hepatic parenchyma.
CASE REPORT
This report describes a case of a man in his 50s with a history of hepatitis C and cirrhosis who presented with 5 days of progressive right upper quadrant pain. Magnetic resonance imaging of the abdomen and pelvis demonstrated a 4.4 cm × 4.8 cm × 4.8 cm right hepatic lobe mass with a large area of necrosis and peripheral enhancement. The subsequent liver biopsy showed few cores of tumor composed of fibroblastic malignant cells producing lace-like osteoid matrix. Osteosarcomatous foci in other parts of the body were excluded by performing extensive physical examination, radiologic imaging, and biopsy. Hence, a primary osteosarcoma was diagnosed. The patient underwent portal vein embolization in preparation for a surgical resection of the right liver lobe. He was admitted six weeks after the embolization for dyspnea and abdominal distension and expired due to abdominal hematoma and pulmonary embolism.
CONCLUSION
Based on the rarity, lack of consensus in treatment, and dismal prognosis, extraosseous osteosarcoma should be considered a separate entity from osseous osteosarcoma. More data and research are needed in this rare and understudied malignancy.
Keywords: osteosarcoma, extraosseous, hepatic
Introduction
Osteosarcoma is the most common bone malignancy, usually arising from skeletal lesions.1,2 Extraosseous osteosarcoma is a rare, primary mesenchymal soft tissue tumor capable of producing osteoid, bone, or chondroid matrix,1,3,4 accounting for approximately 4% of all osteosarcomas.2,4 A literature review yields very few cases of osteosarcoma primarily arising from the hepatic parenchyma.5–15 The data on risk factors, epidemiology, pathogenesis, and treatment of this rare tumor are limited.5–21 We report a case of primary hepatic osteosarcoma in a man in his 50s with a past medical history of hepatitis C and cirrhosis who expired 4 months after diagnosis. The Maimonides Medical Center IRB/Research Committee has stated that no IRB approval is needed for publication of this report.
Case Report
A man in his 50s with a history of hepatitis C virus and liver cirrhosis presented with 5 days of progressive right upper quadrant pain. A computed tomography scan (CT scan) of the abdomen and pelvis showed a large liver mass (Fig. 1). The patient was treated for possible liver abscess with antibiotics. The patient did not improve with antibiotics. A magnetic resonance imaging (MRI) was done due to persistence of symptoms, which demonstrated a 4.4 cm × 4.8 cm × 4.8 cm right hepatic lobe mass with a large area of necrosis with peripheral enhancement (Fig. 2). Subsequently, a liver biopsy was performed that demonstrated a hepatic osteosarcoma. The core biopsy yielded fibroblastic malignant cells producing lace-like osteoid matrix (Fig. 3). Rare osteoclast-like giant cells and mitotic figures were also seen (Fig. 4). Liver parenchyma and carcinomatous element were absent. Extensive sampling of the liver did not show any evidence of carcinomatous or sarcomatous transformation, ruling out choriocarcinoma. Core biopsies of both benign and malignant liver tissues did not show any embryonic or fetal pattern differentiation, thereby excluding hepatoblastoma and hepatocellular carcinoma. On immunohistochemistry, the tumor cells were negative for HepPar1 and AE1/3 and reactive for vimentin. A whole-body positron emission tomography–computed tomography (PET/CT) scan also demonstrated malignant-level uptake in the 1.8 cm × 0.9 cm soft tissue nodule just anterior to the patellar surface of the left distal femur, later confirmed by MRI. Excisional biopsy of the deep left knee mass, which revealed pigmented villonodular synovitis (PVNS) and histological feature, did not resemble the tumor in the liver. The diagnosis of primary osteosarcoma was made for which the patient underwent portal vein embolization in preparation for a surgical resection of the right liver lobe. He was admitted six weeks after the embolization for dyspnea and abdominal distension and expired two weeks later.
Figure 1.

CT showing 4.8 cm × 4.2 cm × 5.9 cm peripheral low-attenuation lesion with small peripheral septations within the right hepatic lobe.
Figure 2.
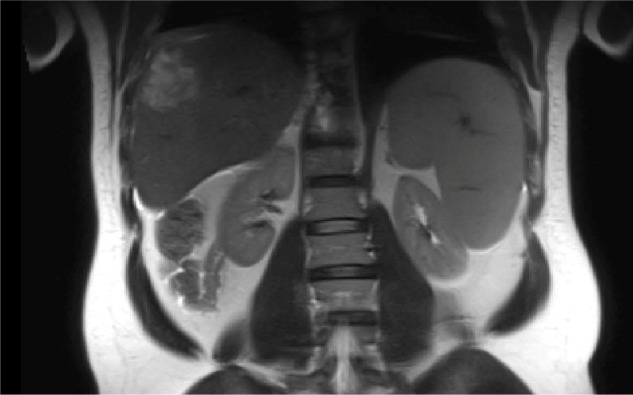
MRI demonstrating a mildly heterogeneous T2 hyperintense lesion in the right hepatic lobe, measuring approximately 4.4 cm × 4.8 cm × 4.9 cm.
Figure 3.
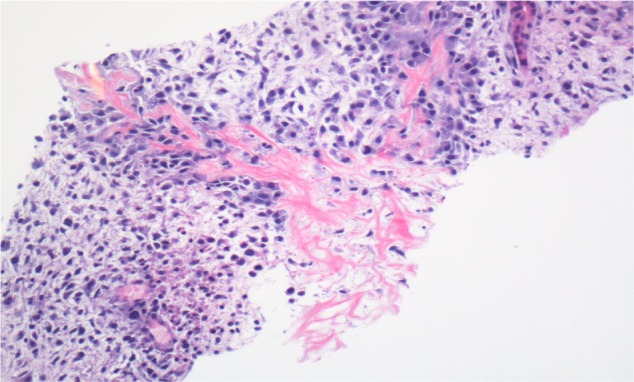
Neoplastic cells with osteoid deposition (hematoxylin and eosin [H&E] × 100).
Figure 4.
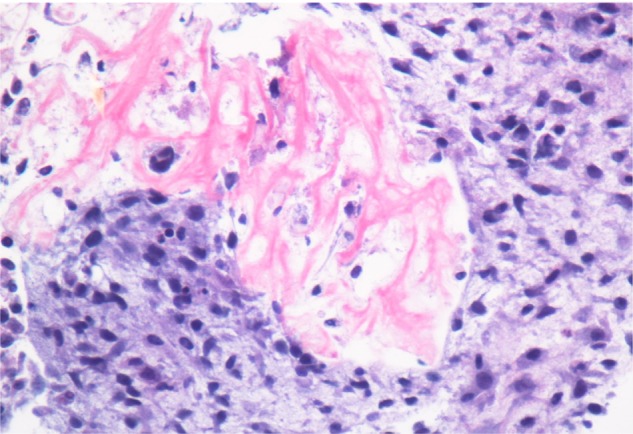
Pleomorphic tumor cells and osteoid deposition (H&E × 400).
Discussion
Osteosarcomas usually arise from skeletal lesions and are charac terized by the production of osteoids by malignant cells.1–4 Extraskeletal osteosarcoma (ESOS) accounts for less than 2% of all soft tissue sarcomas, and the most common anatomic sites are soft tissues of the limbs and the limb girdle.1,3,4,21 Primary osteosarcomas of parenchymal organs are very rare, but cases arising with the thyroid, kidney, gallbladder, breast, mesentery, uterus, brain, lung, bladder, heart, and colon have been reported.22–32
Primary osteosarcoma of the liver is an exceedingly rare hepatic tumor. A literature search yielded 11 case reports of primary hepatic osteosarcoma.5–15 Four of the preceding patients had underlying liver cirrhosis.5–8 Exclusion of an alternative liver neoplasm and osteosarcomatous foci in other parts of the body is the key to diagnose a primary osteosarcoma.5–15 Thus, our patient underwent core biopsies of both benign and malignant liver parenchymas as well as an excisional biopsy of the left knee in order to rule out metastatic disease. The biopsy results were negative for other primary and metastatic liver tumors. The knee biopsy showed PVNS, which is a benign proliferative histiocytic disorder of the synovium. There are very few cases of patients with malignant pigmented villonodular synovitis (MPVNS) reported in the literature.33,34 Our patient’s knee biopsy did not show any cancerous cell, which resembled MPVNS or tumor in the liver.
The pathogenesis of primary liver osteosarcoma is unclear. In general, several etiological factors have been implicated in the pathogenesis of cancer, which include age, lifestyle, radiation, chemotherapy, ischemic stress, trauma, genetic predisposition, and infections such as hepatitis. Previous exposure to radiation has been described as a risk factor for the develop ment of ESOS.4,20 Our patient did not have a history of exposure to radiation. Sumiyoshi and Niho suggested the possible tumorigenesis of the proliferating mesenchymal tissues in the cirrhotic liver.6 Since our patient is the fifth case report of primary hepatic osteosarcoma who had underlying liver cirrhosis, it is of great interest to study the further role of cirrhosis in the pathogenesis of this rare tumor.
ESOS tends to occur in late adulthood, and most patients are in the fifth to seventh decades at the time of diagnosis compared with the osteosarcoma of bone, which occurs in the younger age group.1–4 It has poor prognosis. Lee et al reported that five-year survival of ESOS was 37% in a review of 40 patients, whereas it was 16% in a brief review of ESOS between 1975 and 2009 in Norway as reported by Kjetil Berner et al.3,20 The majority of primary hepatic osteosarcoma patients were older than 50 years and died shortly after diagnosis, despite surgical resection.5–14 There was a single report of a 19-year-old patient who was tumor free for 3 years after surgical resection and adjuvant chemotherapy.15
Conclusion
Because extraosseous osteosarcoma is so rare, has no proven therapy, and has a dire prognosis, it should be conside red a separate entity from osseous osteosarcoma, despite similar histopathology. To date, it appears that surgical resection with adjuvant chemoradiation is the best treatment choice,16–21 although due to the rarity of the disease, no evidence-based treatment protocols exist.
Acknowledgments
The authors thank Jeffrey Lipton, MD (Department of Pathology), Mark Flyer, MD (Department of Radiology), Division of Hematology and Oncology, and Department of Internal Medicine, Maimonides Medical Center, Brooklyn, NY.
Footnotes
ACADEMIC EDITOR: Athavale Nandkishor, Associate Editor
PEER REVIEW: Three peer reviewers contributed to the peer review report. Reviewers’ reports totaled 863 words, excluding any confidential comments to the academic editor.
FUNDING: Authors disclose no external funding sources.
COMPETING INTERESTS: Authors disclose no potential conflicts of interest.
Paper subject to independent expert blind peer review. All editorial decisions madeby independent academic editor. Upon submission manuscript was subject to anti-plagiarism scanning. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of competing interests and funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties. This journal is a member of the Committee on Publication Ethics (COPE).
Author Contributions
TGLT, MS and ABC designed the case report, acquired and interpreted the data and wrote first draft of this case report. All authors contributed to intellectual context and approved the final manuscript.
REFERENCES
- 1.Klein MJ, Siegal GP. Osteosarcoma: anatomic and histologic variants. Am J Clin Pathol. 2006;125(4):555–81. doi: 10.1309/UC6K-QHLD-9LV2-KENN. [DOI] [PubMed] [Google Scholar]
- 2.Stiller CA, Bielack SS, Jundt G, Steliarova-Foucher E. Bone tumours in European children and adolescents, 1978–1997 Report from the automated childhood cancer information system project. Eur J Cancer. 2006;42(13):2124–35. doi: 10.1016/j.ejca.2006.05.015. [DOI] [PubMed] [Google Scholar]
- 3.Lee JS, Fetsch JF, Wasdhal DA, Lee BP, Pritchard DJ, Nascimento AG. A review of 40 patients with extraskeletal osteosarcoma. Cancer. 1995;76(11):2253–9. doi: 10.1002/1097-0142(19951201)76:11<2253::aid-cncr2820761112>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 4.Bane BL, Evans HL, Ro JY, et al. Extraskeletal osteosarcoma. A clinicopathologic review of 26 cases. Cancer. 1990;65(12):2762–70. doi: 10.1002/1097-0142(19900615)65:12<2762::aid-cncr2820651226>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 5.Maynard JH, Fone DJ. Hemochromatosis with osteogenic sarcoma in the liver. Med J Aust. 1969;2:1260–3. doi: 10.5694/j.1326-5377.1969.tb103375.x. [DOI] [PubMed] [Google Scholar]
- 6.Sumiyoshi A, Niho Y. Primary osteogenic sarcoma of the liver-report of an autopsy case. Acta Pathol Jpn. 1971;21(2):305–12. doi: 10.1111/j.1440-1827.1971.tb00126.x. [DOI] [PubMed] [Google Scholar]
- 7.Kitayama Y, Sugimura H, Arai T, Nagamatsu K, Kino I. Primary osteosarcoma arising from cirrhotic liver. Pathol Int. 1995;45(4):320–5. doi: 10.1111/j.1440-1827.1995.tb03464.x. [DOI] [PubMed] [Google Scholar]
- 8.Liony C, Lemarchand P, Manchon ND, et al. A case of primary osteosarcoma of the liver. Gastroenterol Clin Biol. 1990;14(12):1003–6. [PubMed] [Google Scholar]
- 9.Govender D, Rughubar KN. Primary hepatic osteosarcoma: case report and literature review. Pathology. 1998;30(3):323–5. doi: 10.1080/00313029800169556. [DOI] [PubMed] [Google Scholar]
- 10.von Hochstetter AR, Hättenschwiler J, Vogt M. Primary osteosarcoma of the liver. Cancer. 1987;60(9):2312–7. doi: 10.1002/1097-0142(19871101)60:9<2312::aid-cncr2820600933>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 11.Boldt C, Pabst U, Nitsche R, et al. Primary osteosarcoma of the liver. Case report and literature review. Pathology. 1999;20(6):359–64. doi: 10.1007/s002920050372. [DOI] [PubMed] [Google Scholar]
- 12.Craig JR, Peters RL, Edmondson HA. Atlas of Tumor Pathology: Tumors of the Liver and Intrahepatic Bile Ducts. Second Series, Fascicle 26. Washington, DC: Armed Forces Institute of Pathology; 1989. pp. 223–55. [Google Scholar]
- 13.Krishnamurthy NV, Casillas VJ, Bejarano P, et al. Primary osteosarcoma of liver. Eur J Radiol Extra. 2004;50(1):31–6. [Google Scholar]
- 14.Park SH, Choi SB, Kim WB, et al. Huge primary osteosarcoma of the liver presenting an aggressive recurrent pattern following surgical resection. J Dig Dis. 2009;10(3):231–5. doi: 10.1111/j.1751-2980.2009.00391.x. [DOI] [PubMed] [Google Scholar]
- 15.Nawabi A, Rath S, Nissen N, et al. Primary hepatic osteosarcoma. J Gastrointest Surg. 2009;13(8):1550–3. doi: 10.1007/s11605-009-0852-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miller BJ. CORR Insights(®):should high-grade extraosseous osteosarcoma be treated with multimodality therapy like other soft tissue sarcomas? Clin Orthop Relat Res. 2015;473(11):3612–4. doi: 10.1007/s11999-015-4519-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Federman N, Bernthal N, Eilber FC, Tap WD. The multidisciplinary management of osteosarcoma. Curr Treat Options Oncol. 2009;10(1–2):82–93. doi: 10.1007/s11864-009-0087-3. [DOI] [PubMed] [Google Scholar]
- 18.Fan Z, Patel S, Lewis VO, Guadagnolo BA, Lin PP. Should high-grade extraosseous osteosarcoma be treated with multimodality therapy like other soft tissue sarcomas? Clin Orthop Relat Res. 2015;473(11):3604–11. doi: 10.1007/s11999-015-4463-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ahmad SA, Patel SR, Ballo MT, et al. Extraosseous osteosarcoma: response to treatment and long-term outcome. J Clin Oncol. 2002;20(2):521–7. doi: 10.1200/JCO.2002.20.2.521. [DOI] [PubMed] [Google Scholar]
- 20.Berner K, Bjerkehagen B, Bruland ØS, Berner A. Extraskeletal osteosarcoma in Norway, between 1975 and 2009, and a brief review of the literature. Anticancer Res. 2015;35(4):2129–40. [PubMed] [Google Scholar]
- 21.Lee S, Lee MR, Lee SJ, et al. Extraosseous osteosarcoma: single institutional experience in Korea. Asia Pac J Clin Oncol. 2010;6(2):126–9. doi: 10.1111/j.1743-7563.2010.01278.x. [DOI] [PubMed] [Google Scholar]
- 22.Trowell JE, Arkell DG. Osteosarcoma of thyroid gland. J Pathol. 1976;119:123–7. doi: 10.1002/path.1711190208. [DOI] [PubMed] [Google Scholar]
- 23.Axelrod R, Naidech HJ, Myers J, Steinberg A. Primary osteosarcoma of the kidney. Cancer. 1978;41(2):724–7. doi: 10.1002/1097-0142(197802)41:2<724::aid-cncr2820410244>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 24.Olgyai G, Horváth V, Kocsis J, et al. Extraskeletal osteosarcoma in the gallbladder. Magy Seb. 2003;56(2):57–60. [PubMed] [Google Scholar]
- 25.Momoi H, Wada Y, Sarumaru S, et al. Primary osteosarcoma of the breast. Breast Cancer. 2004;11(4):396–400. doi: 10.1007/BF02968048. [DOI] [PubMed] [Google Scholar]
- 26.Choudur HN, Munk PL, Nielson TO, Ryan AG. Primary mesenteric extraskeletal osteosarcoma in the pelvic cavity. Skeletal Radiol. 2005;34(10):649–52. doi: 10.1007/s00256-005-0909-8. [DOI] [PubMed] [Google Scholar]
- 27.Caputo MG, Reuter KL, Reale F. Primary osteosarcoma of the uterus. Br J Radiol. 1990;63(751):578–80. doi: 10.1259/0007-1285-63-751-578. [DOI] [PubMed] [Google Scholar]
- 28.Ohara N, Hayashi K, Shinohara C, et al. Primary osteosarcoma of the cerebrum with immunohistochemical and ultrastructural studies: report of a case. Acta Neuropathol. 1994;88(4):384–8. doi: 10.1007/BF00310384. [DOI] [PubMed] [Google Scholar]
- 29.Karfis EA, Karaiskos T, Cheva A, et al. Primary extraosseous osteosarcoma of the lung. Acta Oncol. 2010;49(1):114–6. doi: 10.3109/02841860902953864. [DOI] [PubMed] [Google Scholar]
- 30.Okada E, Hasegawa Y, Takahashi K, Goto K. Primary osteosarcoma of the urinary bladder. Int Urol Nephrol. 1997;29(4):437–40. doi: 10.1007/BF02551110. [DOI] [PubMed] [Google Scholar]
- 31.Takeuchi I, Kawaguchi T, Kimura Y, et al. Primary cardiac osteosarcoma in a young man with severe congestive heart failure. Intern Med. 2007;46(10):649–51. doi: 10.2169/internalmedicine.46.6267. [DOI] [PubMed] [Google Scholar]
- 32.Shimazu K, Funata N, Yamamoto Y, Mori T. Primary osteosarcoma arising in the colon: report of a case. Dis Colon Rectum. 2001;44(9):1367–70. doi: 10.1007/BF02234799. [DOI] [PubMed] [Google Scholar]
- 33.Imakiire N, Fujino T, Morii T, et al. Malignant pigmented villonodular synovitis in the knee – report of a case with rapid clinical progression. Open Orthop J. 2011;5:13–6. doi: 10.2174/1874325001105010013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wael N, Ayman N, Hesham E, et al. Treatment of diffuse pigmented villonodular synovitis of the knee with combined surgical and radiosynovectomy. HSS J. 2009;5(1):19–23. doi: 10.1007/s11420-008-9104-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


