Abstract
Concussion is one of the most commonly reported injuries amongst children and youth involved in sport participation. Following a concussion, youth can experience a range of short and long term neurobehavioral symptoms (somatic, cognitive and emotional/behavioral) that can have a significant impact on one’s participation in daily activities and pursuits of interest (e.g., school, sports, work, family/social life, etc.). Despite this, there remains a paucity in clinically driven research aimed specifically at exploring concussion within the youth sport population, and more specifically, multi-modal approaches to measuring recovery. This article provides an overview of a novel and multi-modal approach to measuring recovery amongst youth athletes following concussion. The presented approach involves the use of both pre-injury/baseline testing and post-injury/follow-up testing to assess performance across a wide variety of domains (post-concussion symptoms, cognition, balance, strength, agility/motor skills and resting state heart rate variability). The goal of this research is to gain a more objective and accurate understanding of recovery following concussion in youth athletes (ages 10-18 years). Findings from this research can help to inform the development and use of improved approaches to concussion management and rehabilitation specific to the youth sport community.
Keywords: Medicine, Issue 91, concussion, children, youth, athletes, assessment, management, rehabilitation
Introduction
Concussion can be defined as "a complex pathophysiologic process affecting the brain induced by traumatic biomechanical forces"1, and can result in short and long-term somatic, cognitive and/or emotional/behavioral symptoms2. Functionally, concussion and related symptoms can have a significant impact on one's participation in daily activities and pursuits3. It has been estimated that within the United States, between 1.6 and 3.8 million concussion occur each year as a result of sport participation4. Specific to children and youth involved in sports, concussion is one of the most commonly reported injuries5-7. Despite the impact concussion can have on daily activities and the prevalence of concussion amongst children and youth, there remains a lack of scientific data reporting how the youth brain responds to concussion across a variety of performance domains.
Baseline testing, or the use of pre-injury testing scores as a benchmark for comparison against post-injury testing scores to inform recovery, is a practice of growing popularity within the youth sport community and has been suggested internationally8 to be "helpful to add useful information" (p.3) during the management of concussion. In order to best represent the varied nature of post-concussion symptoms (somatic, cognitive and emotional/behavioral), it is important that the assessment of post-concussion recovery include a variety of outcome measures. Further, current concussion management relies heavily on subjective report of post-concussion symptoms. The validity of this subjective report can be influenced by a variety of factors9 and may lead to both under-reporting of symptoms10,11 and a less accurate and reliable index of recovery. As a result, there is a significant need to explore approaches to measuring post-concussion recovery across performance domains that are both objective and sensitive.
It has been demonstrated that cognition, balance, strength and agility can be impaired in youth following concussion and brain injury12-17. The measures included within this testing protocol were chosen to provide insight into recovery across these domains following concussion and to incorporate the use of validated clinical testing tools that are commonly used across clinical settings focused on concussion management. Further, from a more exploratory perspective, resting state HRV can be seen as an accurate measure of sympathovagal balance18,19 . In a healthy population, sympathovagal balance is defined as the parasympathetic system being dominant at rest, while the sympathetic system is under tonic inhibitory control. It is hypothesized that post-concussion, due to physiological stress, an imbalance between the two systems will exist and resting state may shift to hyperactivity of the sympathetic system and hypoactivity of the parasympathetic system20.
The goal of this study's protocol is to conduct a multi-modal assessment of pre- and post-concussion performance amongst youth athletes (ages 10-18 years) in order to gain a more holistic, objective and accurate understanding of recovery following concussion. This study aims to provide insight into the development and delivery of concussion management and rehabilitation protocols specific to children and youth.
Protocol
The described protocol includes pre-injury/baseline testing and post-injury follow-up assessment and is completed using three stations. This testing can be completed individually or in groups of four subjects at each station at a time. Subjects proceed through each station in the order listed below. Table 1 illustrates the protocol’s testing administration schedule. Ethics approval for this research was obtained from the Holland Bloorview Research Ethics Board at the Holland Bloorview Kids Rehabilitation Hospital. All participants and their legal guardians provide signed informed consent prior to completing the protocol and related data collection.
Pre-injury/Baseline Testing
1. Station 1: Obtaining Pre-injury Demographic Information, Post-concussion Symptom Report and Resting State Heart Rate Variability (HRV) Data
Prior to subject(s) arriving for testing, ensure all equipment is functioning properly and ready for testing and that the assessment rooms are free from unnecessary distractions.
After reviewing parental and subject consent, measure and record the subject’s height and weight. Set up heart rate monitor straps and watches on each subject properly.
Administer the demographic information form and collect post-concussion symptom report using the Child version of the Post-Concussion Symptom Inventory(PCSI-C) while each subject is seated for 5 min.
Have each subject lay supine on the ground on a clean sanitized mat. Turn on the heart rate monitors to record resting state heart rate variability (HRV) data (with R-R interval function set to [On]). Have each subject remain lying in supine quietly without talking for 10 min while recording HR.
After 10 min, click the lap button on the watch to indicate the end of supine lying resting state HRV data collection. Ask the subject to return to a seated position, click the lap button on the watch again to indicate beginning of resting state seated HRV data collection.
Have each subject remain in the seated position for 5 min without talking. After 5 min, stop the watch recording function to end the session and resting state HRV data collection. Ask the subject to take off the heart rate strap and watches.
2. Station 2: Obtaining Cognitive Performance Data
Have each subject sit at an individual cubicle with a personal laptop set up with a mouse. Ensure testing environment is free from distraction.
Administer the Immediate Post-concussion Assessment and Cognitive Testing (ImPACT), a rapid and computerized neuropsychological assessment tool (approximately 25 min to complete).
3. Station 3: Obtaining Static Balance, Grip Strength and Agility/Motor Skills Data
Administer the static balance assessment using the modified Clinical Test of Sensory Integration of Balance (m-CTSIB) on the portable balance system. While standing on the balance system forceplate, the subject completes four ordered conditions that include standing with eyes open for 20 sec; standing with eyes closed for 20 sec; standing with eyes open on indexed foam pad for 20 sec; and standing with eyes closed on indexed foam pad for 20 sec.
Using a Dynamometer, measure and record hand grip strength in kg for both right and left hands. Record the dominant hand for each subject while still completing 3 consecutive trials for each hand starting with the dominant hand. Out of the 3 trials taken, the maximum hand grip on each hand will also be recorded. For each trial the subject is told to squeeze the grip as hard as they can for 3 sec keeping a neutral upper extremity position (standing upright, straight arm parallel beside the body, palm facing the body and wrist neutral).
- In a hallway or gym at least 2.5 m wide and 15 m long administer the agility/motor skills assessment using the ABI-Challenge Assessment (ABI-CA) - Concussion Module. Lay tape on the ground in a straight line marking points for every 1 m. In the following order administer these 6 tests following the guidelines and scoring criteria provided in the concussion module.
- Jumping-jacks (Timed):
- Stand with your arms at your sides and jump into an “X” position with arms and legs, and then instantly jump back into starting position. Count how many can be done in 15 sec.
- Pylon/cone obstacle course run (Timed):
- Run in and out of the pylons to the end (10 m) and back as fast as you can but at a speed that you feel safe. Do not touch the pylons. Run straight through the finish line. (Pylons located at 3, 5, 7, 10 m)
- Backwards tandem walking (Timed):
- On the lined track, walk backwards in a tandem pattern for 5 m. Tandem pattern is touching their heel to their opposite toe on each step.
- Modified shuttle run (Timed):
- Run along the 10 m track, pick up a beanbag at the end of the course, and run back to place the beanbag in a basket at the starting point. They must touch the starting line with their foot each time they return to the basket. Repeat this three times until all the beanbags are in the basket at the starting point.
- Ins and outs (Timed):
- Stand with both feet inside of two parallel lines (in the path) that are 40 cm apart. Move one foot outside of the corresponding line followed by the opposite leg moving outside of the other line. The first foot is then returned to the inside, followed by the second foot. Cycles must be consecutive and should be performed in a rhythmical fashion (equal time between each step), and will be repeated 10x not moving forward or backward.
- Standing long jump: Jump forward from standing with both feet as far as you can and hold the landing for 3 sec. Measure and record the distance from the front of the furthest back foot. Three trials are given to achieve the farthest distance
4. Post-injury/Follow-up Testing
- Obtaining post-concussion data while subject is experiencing post-concussion symptoms
- On the same day a subject suffers an injury, research staff is contacted by subject using either phone or email. Research staff records clinical and functional details regarding the injury.
- Immediately following concussion (24-48 hr post injury), collect: resting state HRV data (repeat steps 1.3, 1.5-1.10); post-concussion symptom data (repeat step 1.4); and balance data (repeat step 3.1). If symptoms are exacerbated during testing, stop data collection and allow subject to rest.
- Continue to collect resting state HRV data (repeat steps 1.3, 1.5-1.10), post-concussion symptom data (repeat step 1.4), and balance data (repeat step 3.1) weekly until post-concussion symptoms have resolved. If symptoms are exacerbated during testing, stop data collection and allow subject to rest.
- Research staff follows up with subject weekly by phone to determine when post-concussion symptoms resolve (using PCSI-C).
5. Obtaining Post-concussion Data While Subject is no Longer Experiencing Post-concussion Symptoms
At 1 week after post-concussion symptoms have resolved, collect: resting state HRV data (repeat steps 1.3, 1.5-1.10); post-concussion symptom data (repeat step 1.4); cognitive performance data (repeat steps 2.1-2.2); balance data (repeat step 3.1); hand grip data (repeat step 3.2); and, agility/motor skills data (repeat step 3.3). If symptoms are exacerbated during testing, stop data collection and allow subject to rest.
At 1 month after post-concussion symptoms have resolved, repeat step 5.1. At 3 months after post-concussion symptoms have resolved, repeat step 5.1. At 6 months after post-concussions symptoms have resolved, repeat step 5.1.
Representative Results
The presented protocol is an ongoing investigation. Table 1 depicts the protocol’s testing administration schedule. Representative results are presented to demonstrate the feasibility of collecting baseline/pre-injury and post-concussion data across a variety of performance domains known to be impacted by concussion in youth. A single case of a concussed youth who has completed all stages of the protocol is presented to demonstrate recovery trajectories across selected outcome measures. Figure 1 provides representative data of baseline/pre-injury to post-concussion cognitive performance, balance and post-concussion symptoms. Further, Figure 2, Figure 3 and Figure 4 demonstrate resting state HRV data along with pilot results indicating preliminary support to use resting state HRV as an indicator of recovery following concussion.
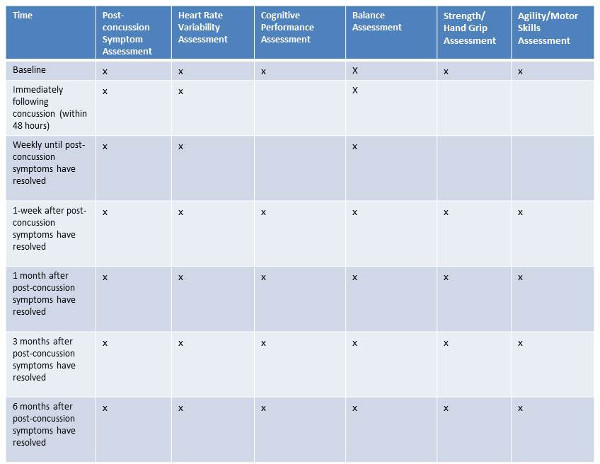 Table 1. Protocol testing administration schedule.
Table 1. Protocol testing administration schedule.
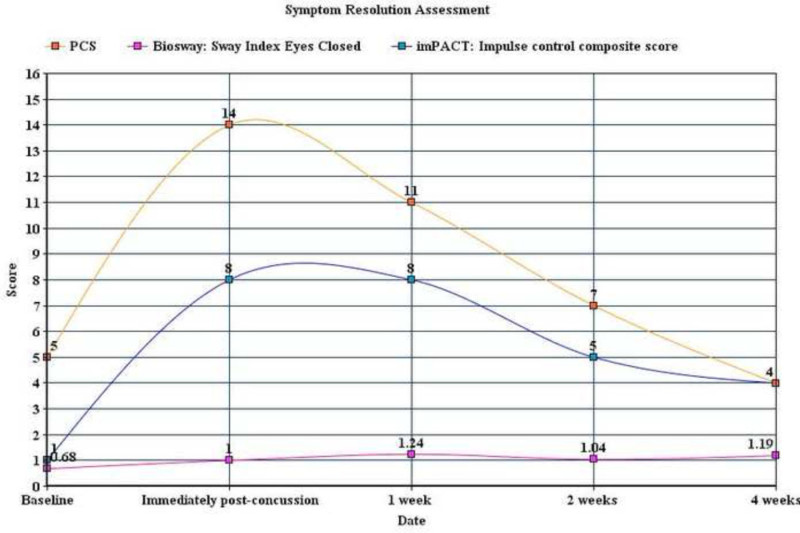 Figure 1. Baseline/pre-injury to post-concussion cognitive performance, balance and post-concussion symptoms. This single case indicates a decrease in cognitive and balance performance (larger score indicates decreased performance) immediately following concussion and an increase in post-concussion symptoms. Although post-concussion symptoms return to baseline levels at 4 weeks post-concussion, cognitive performance and balance deficits remain elevated (although cognitive performance is trending towards baseline levels). Note: Cognitive performance is presented as an impulse control composite score; balance is presented as sway index (standard deviation of sway angle according to center of gravity; the higher the sway index, the more unsteady the subject) during standing with eyes closed; and post-concussion symptoms (PCS) is presented as cumulative value of symptom severity ratings (using a 7-point likert scale; higher value indicates more severe symptoms). Please click here to view a larger version of this figure.
Figure 1. Baseline/pre-injury to post-concussion cognitive performance, balance and post-concussion symptoms. This single case indicates a decrease in cognitive and balance performance (larger score indicates decreased performance) immediately following concussion and an increase in post-concussion symptoms. Although post-concussion symptoms return to baseline levels at 4 weeks post-concussion, cognitive performance and balance deficits remain elevated (although cognitive performance is trending towards baseline levels). Note: Cognitive performance is presented as an impulse control composite score; balance is presented as sway index (standard deviation of sway angle according to center of gravity; the higher the sway index, the more unsteady the subject) during standing with eyes closed; and post-concussion symptoms (PCS) is presented as cumulative value of symptom severity ratings (using a 7-point likert scale; higher value indicates more severe symptoms). Please click here to view a larger version of this figure.
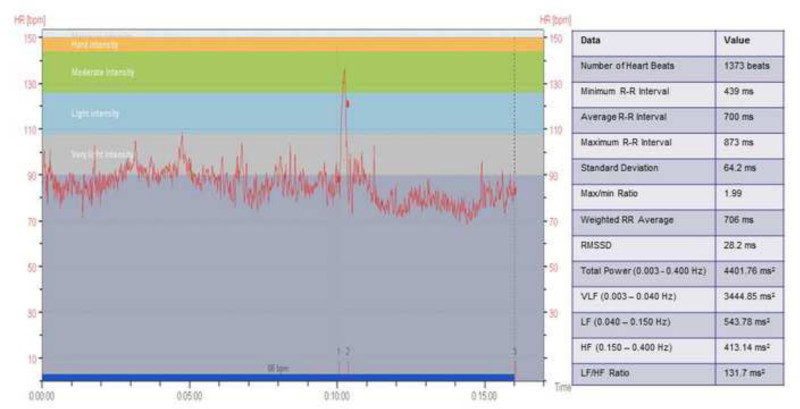 Figure 2. Example resting state heart rate variability (HRV) data. Heart rate (bpm) is shown across time for the entire 15 min HRV trial. Label 1 on the x-axis shows when the subject gets up from laying supine for 10 min. Label 2 shows when the subject begins sitting for the final 5 min of the trial. Label 3 shows when the entire trial is completed. Heart rate intensity is also shown with the corresponding colors. These data are then analyzed with Kubios software to give valuable information regarding HRV. The outcome measures analyzed Total Power (total spectrum power over frequencies between DC and 0.40 Hz), VLF (spectral power of the R-R intervals in the Very Low-Frequency range), LF (spectral power in the Low-Frequency range), HF (spectral power in the High-Frequency range which usually includes the respiratory frequency) are presented. Please click here to view a larger version of this figure.
Figure 2. Example resting state heart rate variability (HRV) data. Heart rate (bpm) is shown across time for the entire 15 min HRV trial. Label 1 on the x-axis shows when the subject gets up from laying supine for 10 min. Label 2 shows when the subject begins sitting for the final 5 min of the trial. Label 3 shows when the entire trial is completed. Heart rate intensity is also shown with the corresponding colors. These data are then analyzed with Kubios software to give valuable information regarding HRV. The outcome measures analyzed Total Power (total spectrum power over frequencies between DC and 0.40 Hz), VLF (spectral power of the R-R intervals in the Very Low-Frequency range), LF (spectral power in the Low-Frequency range), HF (spectral power in the High-Frequency range which usually includes the respiratory frequency) are presented. Please click here to view a larger version of this figure.
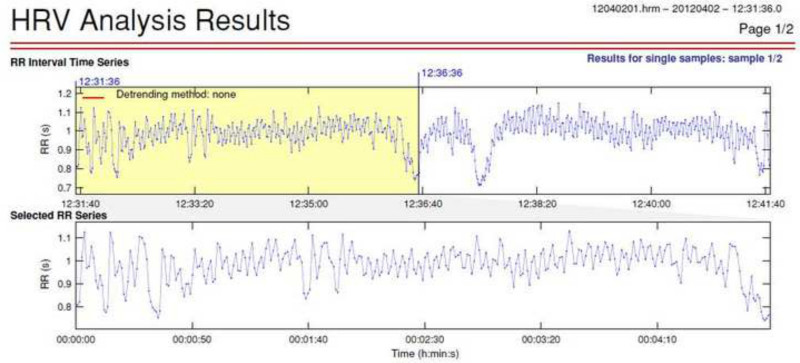 Figure 3. Example resting state HRV data. Total power heart rate variability reflects the total variance in heart rate pattern. Sympathetic activity is the primary contributor to total power frequency domain measures. A pilot study was conducted to obtain baseline and post-concussion measures of HRV frequency domain measures. 5 min selections of HRV were obtained from a longer sample and a low level artifact correction was applied. Please click here to view a larger version of this figure.
Figure 3. Example resting state HRV data. Total power heart rate variability reflects the total variance in heart rate pattern. Sympathetic activity is the primary contributor to total power frequency domain measures. A pilot study was conducted to obtain baseline and post-concussion measures of HRV frequency domain measures. 5 min selections of HRV were obtained from a longer sample and a low level artifact correction was applied. Please click here to view a larger version of this figure.
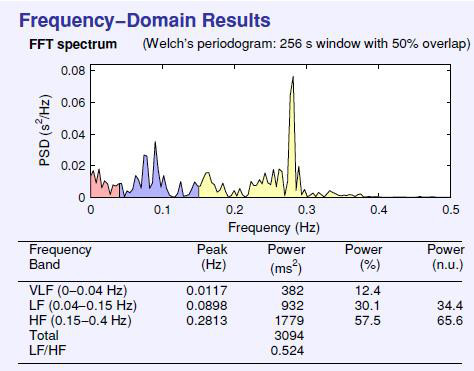 Figure 4. Example frequency domain measures of power for resting state HRV data. Frequency domain measures of power (msec2), using the Fast Fourier Transformation (FFT), were obtained at baseline and each re-test post-concussion. This figure indicates a total power of 3094 msec2.
Figure 4. Example frequency domain measures of power for resting state HRV data. Frequency domain measures of power (msec2), using the Fast Fourier Transformation (FFT), were obtained at baseline and each re-test post-concussion. This figure indicates a total power of 3094 msec2.
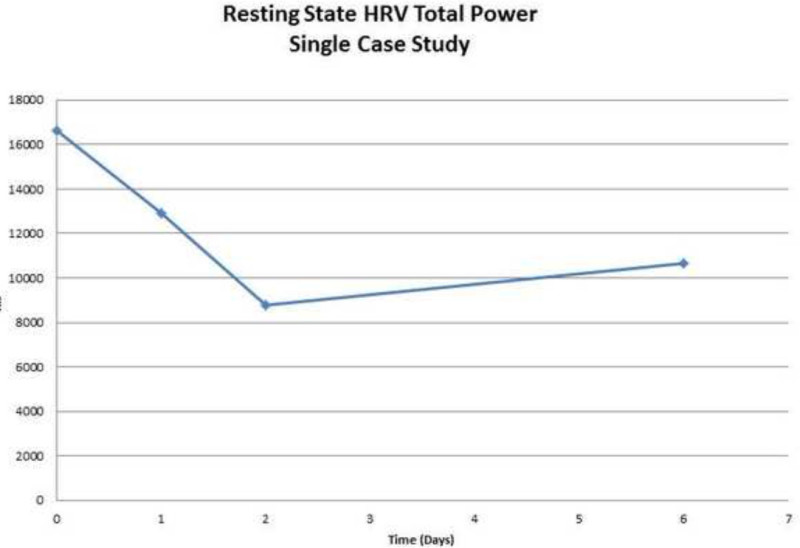 Figure 5. Example total power data across a single pilot participant before (day 0) and after a concussion (days 1-6). Total power (HRV) was graphed versus time. The participants demonstrated reduced total power (HRV) on day 1, day 2 and day 6 post-concussion. This pilot data demonstrates that the protocol for HRV collection, both at baseline and post-concussion, represents a feasible option for clinical examination. Data from this pilot study indicates that total power (HRV) is a tool that warrants further examination as a concussion assessment and management tool. Please click here to view a larger version of this figure.
Figure 5. Example total power data across a single pilot participant before (day 0) and after a concussion (days 1-6). Total power (HRV) was graphed versus time. The participants demonstrated reduced total power (HRV) on day 1, day 2 and day 6 post-concussion. This pilot data demonstrates that the protocol for HRV collection, both at baseline and post-concussion, represents a feasible option for clinical examination. Data from this pilot study indicates that total power (HRV) is a tool that warrants further examination as a concussion assessment and management tool. Please click here to view a larger version of this figure.
Discussion
This protocol presents a multi-modal approach to measuring recovery in youth athletes following a concussion. A critical feature of this protocol is the comparison of post-concussion data across a wide range of performance domains (cognition, balance, strength, agility, resting state heart rate variability, etc.) to pre-injury/baseline. These data serve as a means to indicate recovery amongst individual youth athletes following a concussion. By using common and readily available clinical measures of cognition, balance, strength and agility performance, as well as the experimental use of resting state HRV, this protocol aims to provide much needed insight into which objective measures are most appropriate in order to most effectively manage concussion amongst children and youth. Due to the heterogeneous nature of post-concussion symptoms across individuals following a concussion, the holistic performance data collected can be considered critical in providing a more accurate index of recovery after concussion specific to children and youth. Further, the ability to complete the testing protocol with single subjects or with subjects within successive groups of four, by way of using a station-based approach, promotes feasibility of use of this protocol with its target audience, the youth sport community.
When completing the testing protocol at pre-injury/baseline and post-injury/follow-up testing sessions, it is important that the described test order is adhered to. Demographic information, post-concussion symptom report and resting state HRV data (i.e., Station 1 data) are collected prior to Station 2 and 3 data to ensure results are reflective of the resting state and are not influenced by cognitive and/or physical exertion. Accordingly, cognitive performance data (i.e., Station 2 data) is collected prior to physical measures to ensure that results are not influenced by physical exertion. Static balance, grip strength and agility/motor skills data (i.e., Station 3 data) is collected after all other measures have been collected. Measures in this station progress from less to more physically demanding. Administering them in the prescribed order ensures that fatigue does not negatively impact performance on subsequent tests. This is especially true with regards to the motor skills/agility assessment which is the most physically demanding task and most likely to result in subject fatigue. Additionally, as it has been suggested that exercise may negatively affect performance on neurocognitive testing21. it is important that this measure is completed last. For example, if the motor skills/agility assessment is completed prior to the assessment of resting state HRV, cognition or balance, it is possible that resulting physical fatigue may skew a subject’s performance on these tasks. For this reason, modifications to the test order within the presented protocol are discouraged.
Assessments that are administered during follow-up testing is dependent on a subject’s self-reported post-concussion symptoms. It is important to note that even if a subject’s PCSI is low, it is still possible that one may experience symptom exacerbation (fatigue, dizziness, etc.), due to deconditioning, increased exertion, etc. If a subject does experience symptom exacerbation and is unable to complete follow-up testing, all testing is aborted with no effect on their baseline data. Subjects are advised to rest and not partake in any other exertion-based activities until symptom resolution.
To date, we know very little about how the youth brain and body recover following concussion and the related trajectory and timeframe of this recovery. It is possible for functional changes to occur even after symptom resolution22. Based on this, it is important to follow-up with subjects at 1 month, 3 months and 6 months post-concussion in order to track any changes and identify any areas of concern. A limitation of this protocol can be found when collecting resting state HRV data with children and youth. The heart rate monitors used within this protocol involved fitting subjects with a heart rate sensor and elastic strap that fastens around the subject’s chest, where constant contact between the sensor and the chest is required for data collection. Due to the size of many children and youth within this study, often the elastic strap is too large to fasten tightly and appropriately (e.g., constant contact with subject’s chest and no movement of strap/sensor) to promote effective resting state HRV data collection. To troubleshoot this limitation, it is important to have smaller sized elastic straps readily available for use when working with subjects of a smaller body size.
The described approach to assessing recovery following concussion amongst children and youth considers the need to assess a wide range of skills and abilities across performance domains most influenced by a concussive injury. Further, this protocol uses standardized and objective measures to supplement the subjective report of post-concussion symptoms in order to more accurately indicate post-injury recovery (e.g., return to pre-injury/baseline levels of performance). The data collected will inform which measures are most sensitive to concussion amongst children and youth and in turn, which measures, alone or in combination with one another, can provide the most accurate index of post-concussion recovery.
The goal of this research is to determine methods of data collection that can be used most effectively during the clinical management and rehabilitation of concussion in children and youth in order to promote improved outcomes and the safe participation in meaningful daily activities (e.g., school, sports, family/social life). The concurrent collection of subjective and objective data in the context of a multimodal assessment approach enables a wide range of performance domains to be captured post concussion. Further, the ability to test child and youth subjects on their own or in larger groups, make this technique novel and unique. This study will provide new insight into how the youth brain and body recover after concussion and can inform the development of a standardized approach to the assessment of performance pre-and post-concussion with the youth sport population.
Disclosures
The authors have nothing to disclose.
Acknowledgments
We would like to thank the Canadian Institutes of Health Research (CIHR) who have provided funding for this research. Further, we would like to acknowledge Dr. Tim Taha and Dr. Scott Thomas from the University of Toronto for their assistance with the development of our protocol for the collection of resting state heart rate variability data.
References
- McCrory P, Meeuwisse W, et al. Consensus statement on Concussion in Sport 3rd International Conference on Concussion in Sport held in Zurich, November 2008. Clinical Journal of Sport Medicine: Official Journal of the Canadian Academy of Sport Medicine. 2009;19(3):185–200. doi: 10.1097/JSM.0b013e3181a501db. [DOI] [PubMed] [Google Scholar]
- Kirkwood MW, Yeates KO, Wilson PE. Pediatric sport-related concussion: a review of the clinical management of an oft-neglected population. Pediatrics. 2006;117(4):1359–1371. doi: 10.1542/peds.2005-0994. [DOI] [PubMed] [Google Scholar]
- Khan F, Baguley IJ, Cameron ID. 4: Rehabilitation after traumatic brain injury. The Medical journal of Australia. 2003;178(6):290–295. doi: 10.5694/j.1326-5377.2003.tb05199.x. [DOI] [PubMed] [Google Scholar]
- Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. The Journal of head trauma rehabilitation. 2006;21(5):375–378. doi: 10.1097/00001199-200609000-00001. [DOI] [PubMed] [Google Scholar]
- Browne GJ, Lam LT. Concussive head injury in children and adolescents related to sports and other leisure physical activities. British Journal of Sports Medicine. 2006;40(2):163–168. doi: 10.1136/bjsm.2005.021220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emery CA, Meeuwisse WH. Injury rates, risk factors, and mechanisms of injury in minor hockey. The American journal of sports medicine. 2006;34(12):1960–1969. doi: 10.1177/0363546506290061. [DOI] [PubMed] [Google Scholar]
- Keightley M, Reed N, Green S, Taha T. Age and competition level on injuries in female ice hockey. International journal of sports medicine. 2013;34(8):756–759. doi: 10.1055/s-0032-1327574. [DOI] [PubMed] [Google Scholar]
- McCrory P, Meeuwisse WH, et al. Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. British journal of sports medicine. 2013;47(5):250–258. doi: 10.1136/bjsports-2013-092313. [DOI] [PubMed] [Google Scholar]
- Krol AL, Mrazik M, Naidu D, Brooks BL, Iverson GL. Assessment of symptoms in a concussion management programme: method influences outcome. Brain injury: [BI. 2011;25(13-14):1300–1305. doi: 10.3109/02699052.2011.624571. [DOI] [PubMed] [Google Scholar]
- Williamson IJS, Goodman D. Converging evidence for the under-reporting of concussions in youth ice hockey. British Journal of Sports Medicine. 2006;40(2):128–132. doi: 10.1136/bjsm.2005.021832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassidy JD, Carroll LJ, et al. Incidence, risk factors and prevention of mild traumatic brain injury: results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. Journal of Rehabilitation Medicine: Official Journal of the UEMS European Board of Physical and Rehabilitation Medicine. 2004. pp. 28–60. [DOI] [PubMed]
- Collins MW, Lovell MR, Iverson GL, Cantu RC, Maroon JC, Field M. Cumulative effects of concussion in high school athletes. Neurosurgery. 2002;51(5):1175–1179. doi: 10.1097/00006123-200211000-00011. [DOI] [PubMed] [Google Scholar]
- Lovell MR, Collins MW, Iverson GL, Johnston KM, Bradley JP. Grade 1 or “ding” concussions in high school athletes. The American Journal of Sports Medicine. 2004;32(1):47–54. doi: 10.1177/0363546503260723. [DOI] [PubMed] [Google Scholar]
- Guskiewicz KM. Postural stability assessment following concussion: one piece of the puzzle. Clinical journal of sport medicine: official journal of the Canadian Academy of Sport Medicine. 2001;11(3):182–189. doi: 10.1097/00042752-200107000-00009. [DOI] [PubMed] [Google Scholar]
- Guskiewicz KM. Assessment of postural stability following sport-related concussion. Current Sports Medicine Reports. 2003;2(1):24–30. doi: 10.1249/00149619-200302000-00006. [DOI] [PubMed] [Google Scholar]
- Reed N, Taha T, Tremblay L, Monette G, Keightley M. Concussion and strength performance in youth hockey players. Brain Injury. 2012;26(4-5):766. [Google Scholar]
- Chevignard M, Toure H, Brugel DG, Poirier J, Laurent-Vannier A. A comprehensive model of care for rehabilitation of children with acquired brain injuries. Child: care, health and development. 2010;36(1):31–43. doi: 10.1111/j.1365-2214.2009.00949.x. [DOI] [PubMed] [Google Scholar]
- Goldstein B, Toweill D, Lai S, Sonnenthal K, Kimberly B. Uncoupling of the autonomic and cardiovascular systems in acute brain injury. The American journal of physiology. 1998;275(4 Pt 2):R1287–R1292. doi: 10.1152/ajpregu.1998.275.4.R1287. [DOI] [PubMed] [Google Scholar]
- Korpelainen JT, Huikuri HV, Sotaniemi KA, Myllylä VV. Abnormal heart rate variability reflecting autonomic dysfunction in brainstem infarction. Acta neurologica Scandinavica. 1996;94(5):337–342. doi: 10.1111/j.1600-0404.1996.tb07076.x. [DOI] [PubMed] [Google Scholar]
- Leddy JJ, Kozlowski K, Fung M, Pendergast DR, Willer B. Regulatory and autoregulatory physiological dysfunction as a primary characteristic of post concussion syndrome: implications for treatment. NeuroRehabilitation. 2007;22(3):199–205. [PubMed] [Google Scholar]
- Covassin T, Weiss L, Powell J, Womack C. Effects of a maximal exercise test on neurocognitive function. British journal of sports medicine. 2007;41(6):370–374. doi: 10.1136/bjsm.2006.032334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrory P, Collie A, Anderson V, Davis G. Can we manage sport related concussion in children the same as in adults? British Journal of Sports Medicine. 2004;38(5):516–519. doi: 10.1136/bjsm.2004.014811. [DOI] [PMC free article] [PubMed] [Google Scholar]


