Abstract
Magnetically-responsive nano/micro-engineered biomaterials that enable a tightly controlled, on-demand drug delivery have been developed as new types of smart soft devices for biomedical applications. Although a number of magnetically-responsive drug delivery systems have demonstrated efficacies through either in vitro proof of concept studies or in vivo preclinical applications, their use in clinical settings is still limited by their insufficient biocompatibility or biodegradability. Additionally, many of the existing platforms rely on sophisticated techniques for their fabrications. We recently demonstrated the fabrication of biodegradable, gelatin-based thermo-responsive microgel by physically entrapping poly(N-isopropylacrylamide-co-acrylamide) chains as a minor component within a three-dimensional gelatin network. In this study, we present a facile method to fabricate a biodegradable drug release platform that enables a magneto-thermally triggered drug release. This was achieved by incorporating superparamagnetic iron oxide nanoparticles and thermo-responsive polymers within gelatin-based colloidal microgels, in conjunction with an alternating magnetic field application system.
Keywords: Bioengineering, Issue 108, Microgel, gelatin, thermo-responsive polymer, alternating magnetic field, superparamagnetic nanoparticles, magnetothermal stimulus, drug delivery
Introduction
Stimuli-responsive drug delivery systems that enable a tightly controlled drug delivery in response to either endogenous or exogenous stimuli (e.g., temperature or pH) have been extensively investigated as new types of smart soft devices for drug delivery. Microscale hydrogels have been widely employed as a drug delivery platform in that they confer controllable and sustainable drug release profiles as well as tunable chemical and mechanical properties1-3. In particular, the colloidal microgels exhibit many advantages as a vehicle for drug delivery due to their rapid responsiveness to external stimuli and suitable injectability to local tissue in a minimally invasive manner4. The poly(N-isopropylacrylamide) (pNIPAM) or its copolymers have been widely adopted in synthesizing thermo-responsive microgels by grafting pNIPAM with biodegradable/ biocompatible polymers including gelatin, chitosan, alginate acid, or hyaluronic acid5,6, in which a phase transition characteristic of pNIPAM at its lower critical solution temperature (LCST) can be used as a trigger of drug release7. We recently demonstrated a fabrication of biodegradable, gelatin-based thermo-responsive microgel by incorporating poly(N-isopropylacrylamide-co-acrylamide) [p(NIPAM-co-AAm)] chains as a minor component within three-dimensional gelatin networks8. The gelatin/p(NIPAM-co-AAm) microgel exhibited a tunable deswelling to temperature increase, which positively correlated to the release of bovine serum albumin (BSA).
During the last several years, there have been increasing efforts to develop a magnetically responsive drug delivery platform that can trigger the release of drug in an on-demand fashion9,10. The basic principle for the synthesis of magnetically responsive drug delivery platform utilizes the characteristic of superparamagnetic nanoparticles (MNPs) to generate heat when they receive a high frequency alternating magnetic field (AMF), which triggers a temperature-sensitive drug release. This holds promise for future clinical applications in that this system can target deep into the tissue, enables a non-invasive and remotely controlled drug release and can be combined with hyperthermia treatment and magnetic resonance imaging system10-12. Such platforms include: (1) MNPs/pNIPAM hybrid microgel particles 13-15 and (2) macroscopic hydrogel scaffolds incorporating immobilized MNPs16-18. The pNIPAM-based microgel platforms demonstrated a finely-tunable volume phase transition responsiveness to magneto-thermal stimuli. However, they still rely on complex and sophisticated techniques in the fabrication and the use of pNIPAM polymers with a high content can be potentially cytotoxic to cells19, which may limit their in vivo applications. The macroscopic scaffolds exhibit a relatively slow response to external stimuli and require an invasive surgical transplantation compared to colloidal microgels.
The water-in-oil emulsification has been the standard method to produce submillimeter or micrometer-sized gel particles20. At the water-oil interface of the emulsion, microgel particle forms a spherical shape due to the minimization of surface energy of the water droplet under mechanical shear force. This method allows the production of a large amount of aqueous spherical gel droplets in a simple fabrication procedure and has been successfully adopted for fabricating gelatin-based microgels for drug delivery applications21-23.
Here, we present a facile method to synthesize a magnetothermally responsive gelatin-based microgels for drug delivery application by employing the water-in-oil emulsification method. This was achieved by physically incorporating iron oxide MNPs and p(NIPAM-co-AAm) chains as a minor component within a spherical microscale gelatin network that is covalently crosslinked by a naturally-derived crosslinker genipin, in conjunction with a high frequency alternating magnetic field (AMF) application system.
Protocol
Note: The overall process of fabricating magnetic field-responsive gelatin microgels is illustrated in Figure 1A.
1. Preparing Solutions and Suspensions
Prepare a crosslinker genipin (1% w/v) solution by dissolving 20 mg of genipin in 2 ml of phosphate buffered saline (1x PBS; pH 7.4). Vortex the solution and place in a 50 oC water bath for 2 hr to completely dissolve the solution.
Prepare a surfactant solution by dissolving 20 mg of poly(ethylene glycol)-poly(propylene glycol)-poly(ethylene glycol) (Mw = 2,900 Da; referred to as L64) in 200 ml of PBS to be at the concentration of 100 ppm.
Prepare a 15% (w/v) gelatin solution by dissolving 64.5 mg of gelatin in 0.43 ml of PBS. Vortex the solution and place it on water bath at 37 oC until it reaches a sol phase, where the solution becomes fluidic. Then, vortex the gelatin solution 2 - 3 times to ensure the homogeneity of the sample.
- Preparation of p(NIPAM-co-AAm)/MNPs solution with a model drug (BSA):
- Disperse 10.75 mg of hydrophilic MNPs in 0.43 ml of PBS and then dissolve 12.9 mg of p(NIPAM-co-AAm) in the MNP suspension to make the concentration at 3% (w/v). The increased concentration of p(NIPAM-co-AAm) can be used to achieve an increased deswelling behavior of microgels.
- Use Texas-Red conjugated bovine serum albumin (TR-BSA; Mw ~66 kDa) as a model drug. Dissolve 0.5 mg of TR-BSA in the mixture of p(NIPAM-co-AAm)/MNPs.
Prepare mixtures of gelatin/p(NIPAM-co-AAm)/MNPs/BSA solution (0.86 ml) by adding mixture of p(NIPAM-co-AAm)/MNPs (0.43 ml) into the gelatin solution (0.43 ml) and then thoroughly vortex them to make a homogeneous mixture. Thus, the concentrations of polymers and MNP become half of the initial concentrations in the final mixture.
2. Emulsification
Pour 15 ml of silicone oil [polydimethylsiloxane (viscosity 350 cSt)] into a clean and sterile beaker.
Immediately add the pre-prepared aqueous mixtures of gelatin/p(NIPAM-co-AAm)/MNPs/BSA solution (0.86 ml) into the silicone oil and emulsify the aqueous mixture in the oil phase by stirring with a magnetic stirring bar at 900 rpm at 30 oC for 30 min.
3. Gelation and Transfer of Micro-droplets to an Aqueous Solution
Transfer the emulsion (~16 ml) from beaker into a 50 ml tube.
Cool down the tube for 10 min at 4 °C for gelation of the micro-droplets in the oil.
Fill the tube with the prepared L64 solution (at 4 oC) up to 50 ml and vigorously shake the tube. It may be possible that a portion of L64 surfactants would be within the microgels.
Centrifuge the tube for 20 min at 2,300 x g at 4 oC.
Regularly check for the presence of the pellet of gel particles on the side of the tube. If the particles are not seen, centrifuge for another 20 min at the same speed and temperature. Proceed to carefully remove supernatant without disturbing the pellet formed on the inner wall of the tube.
Repeat steps (3.3) through (3.5) once more. Each time, transfer the sample to a new tube to avoid the inclusion of any oil droplets in the microgel suspension. After this step, ensure that surfactants or oil droplets are not present in the sample suspension. However, the repeated separation steps may lead to loss of initial materials.
4. Covalent Crosslinking of the Microgels
Add 2 ml of genipin solution (prepared in section 1) to the pellet of gel particles and mix them well by vortexing the solution.
Quickly transfer the tube of the suspension in water bath at 23 oC to initiate a covalent crosslinking reaction during a desired crosslinking time (e.g., 5 - 120 min).
After crosslinking, immediately remove any excessive crosslinkers by discarding the genipin solution, resuspending the microgels in PBS, and centrifuging the tube for 20 min at 2,300 x g (4 oC). If needed, cautiously break apart formed pellet with a pipette tip. This washing step can be repeated up to 3 times if the genipin is still remaining in the solution.
Discard the supernatant and resuspend the microgels in PBS at a desired density (e.g., 5 × 106 microgels/ml) by counting the number with a hemocytometer.
For microscopic observations, load the microgel suspension in the space between a slide glass and a cover slip and seal the boundary of the cover slip with epoxy resin.
5. Application of Alternating Magnetic Field for Triggering Drug Release
Place the tube with desired concentration of microgels in aqueous media into the chamber of magnetic coils. If necessary, insert a fiber optic temperature probe into the tube to monitor temperature change of the media during the application of AMF.
Apply high frequency (>100 kHz) AMF at a defined field strength (>5 kA/m) and for a specified duration. Following the application of AMF, centrifuge the sample tube for 20 min at 2,273 x g (4 oC) and collect the supernatant to quantify the amount of TR-BSA released from microgel to the surrounding media using spectrophotometry. The excitation and emission wavelengths for Texas Red are 584 nm and 612 nm, respectively.
Representative Results
When the protocol is performed correctly, the fabricated microgels should exhibit a well-characterized spherical morphology and colloidal dispersibility with diameters in the range between 5 μm to 20 μm (Figure 1B and C). Either fluorescent MNPs or fluorescent BSA can be used to confirm whether MNPs or drugs (BSA in this study) are properly encapsulated within the microgel (Figure 1D). The fabricated microgels can be stable and stored at 4 oC for up to 4 weeks in the absence of any enzymatically degrading agents including collagenase. The incorporation of p(NIPAM-co-AAm) in the gelatin microgel enables it to exhibit a temperature dependent volume change (Figure 2A), in which the increase of temperature of the media from 22 oC to 42 oC resulted in the deswelling of gelatin microgels incorporating p(NIPAM-co-AAm) by ~40% in volume, in contrast to only ~10% volume change for gelatin microgel without p(NIPAM-co-AAm) (Figure 2B). The extent of deswelling of the gelatin/p(NIPAM-co-AAm) microgels can be tuned as functions of the crosslinking degree of the gelatin matrix and the concentration of p(NIPAM-co-AAm)8.
If MNPs are properly incorporated in the gelatin/p(NIPAM-co-AAm) microgel, the microgel should experience a temperature increase within the gel upon the application of an appropriate AMF, which may induce an increase of the solution temperature as well. In this study, the application of a short exposure of AMF (10 min) at a magnetic field strength of 20 kA/m resulted in gradual increases in temperature by 10 oC (from 20 oC to 30 oC) in the media (Figure 2C). It is expected that the actual temperature increase within the microgel would be much higher than the one observed in the media, since the matrix of the microgel may hinder heat dissipation to the surrounding area. The extent of TR-BSA release from gelatin/p(NIPAM-co-AAm)/MNPs was measured to be ~35%, while the TR-BSA release from gelatin/MNPs microgel without incorporating p(NIPAM-co-AAm) was significantly low at ~10% (Figure 2D). Thus, our results indicate that the release of BSA in response to AMF application was induced by the deswelling of gelatin/p(NIPAM-co-AAm)/MNPs microgel, associated with the shrinkage of p(NIPAM-co-AAm) polymer chains within the microgel (Figure 3). Since the extent of microgel deswelling is proportional to the both extent of temperature increase and concentration of p(NIPAM-co-AAm)8, a strategy to increase either amount of MNPs24 or p(NIPAM-co-AAm)8 in step 1 in the protocol section may result in increased release of BSA at a given field strength and frequency of AMF application.
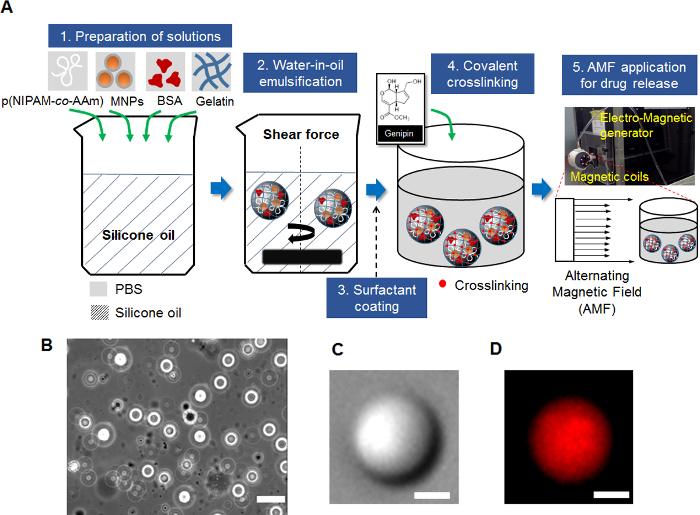 Figure 1. Preparation of Gelatin Hybrid Microgels.(A) Schematic overview of the fabrication of magnetically responsive microgels. (B) Phase contrast microscopic image of a colloidal suspension of magneto-responsive microgels incorporating superparamagnetic nanoparticles (MNPs) and thermo-responsive p(NIPAM-co-AAm) chains. Scale bar = 50 μm. (C) Differential interference contrast (DIC) image of a single microgel. Scale bar = 5 μm. (D) Fluorescence microscopic image of the single microgel encapsulating TR-BSA. The fluorescence signals in the image are from TR-BSA. Scale bar = 5 μm. Please click here to view a larger version of this figure.
Figure 1. Preparation of Gelatin Hybrid Microgels.(A) Schematic overview of the fabrication of magnetically responsive microgels. (B) Phase contrast microscopic image of a colloidal suspension of magneto-responsive microgels incorporating superparamagnetic nanoparticles (MNPs) and thermo-responsive p(NIPAM-co-AAm) chains. Scale bar = 50 μm. (C) Differential interference contrast (DIC) image of a single microgel. Scale bar = 5 μm. (D) Fluorescence microscopic image of the single microgel encapsulating TR-BSA. The fluorescence signals in the image are from TR-BSA. Scale bar = 5 μm. Please click here to view a larger version of this figure.
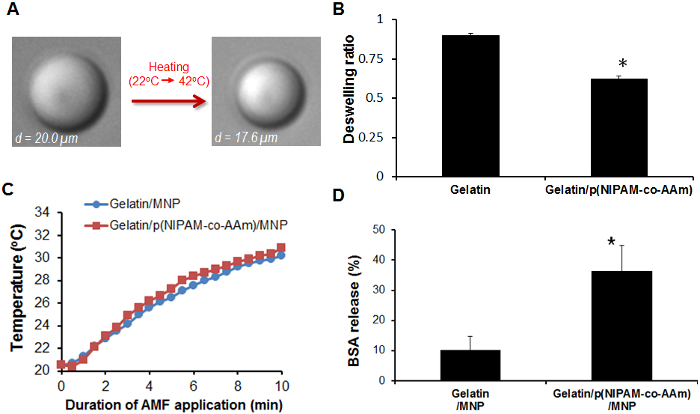 Figure 2. Thermo-responsive Deswelling Behavior and BSA Release from Gelatin Hybrid Microgels. (A) Representative DIC images showing the deswelling of gelatin/p(NIPAM-co-AAm) microgel induced by temperature increase from 22 oC to 42 oC. This figure has been modified from reference [8]. (B) Comparison of the deswelling ratio (final volume / initial volume) of the pure gelatin microgels and the gelatin microgels embedding p(NIPAM-co-AAm) chains in response to temperature increase from 22 oC to 42 oC. This figure has been modified from reference [8]. (C) Changes in ambient temperature in the media during the AMF application (at field strength of 20kA/m and at frequency of 2.1 MHz). (D) The release of TR-BSA (%) in response to AMF (20 kA/m at 2.1 MHz) application for 10 min. The extent of TR-BSA release from microgels was quantified by measuring the ratio of fluorescence intensity of TR-BSA, in the media of microgels solution after AMF stimulus, to total fluorescence intensity of TR-BSA within microgles before AMF stimulus at 22 oC, using a spectrophotometer *: p <0.05 between groups. Please click here to view a larger version of this figure.
Figure 2. Thermo-responsive Deswelling Behavior and BSA Release from Gelatin Hybrid Microgels. (A) Representative DIC images showing the deswelling of gelatin/p(NIPAM-co-AAm) microgel induced by temperature increase from 22 oC to 42 oC. This figure has been modified from reference [8]. (B) Comparison of the deswelling ratio (final volume / initial volume) of the pure gelatin microgels and the gelatin microgels embedding p(NIPAM-co-AAm) chains in response to temperature increase from 22 oC to 42 oC. This figure has been modified from reference [8]. (C) Changes in ambient temperature in the media during the AMF application (at field strength of 20kA/m and at frequency of 2.1 MHz). (D) The release of TR-BSA (%) in response to AMF (20 kA/m at 2.1 MHz) application for 10 min. The extent of TR-BSA release from microgels was quantified by measuring the ratio of fluorescence intensity of TR-BSA, in the media of microgels solution after AMF stimulus, to total fluorescence intensity of TR-BSA within microgles before AMF stimulus at 22 oC, using a spectrophotometer *: p <0.05 between groups. Please click here to view a larger version of this figure.
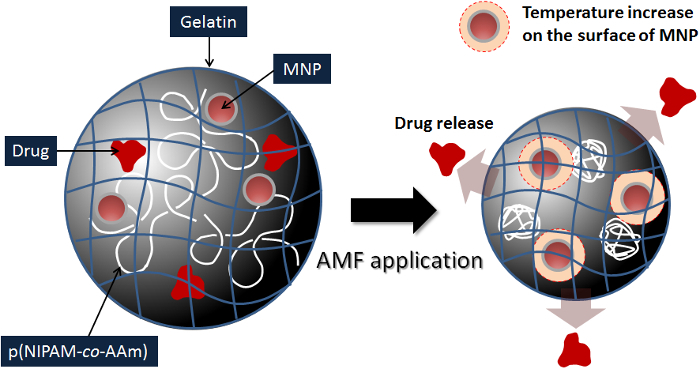 Figure 3. A Schematic Illustration of the Potential Mechanism by Which Gelatin/p (NIPAM-co-AAm)/MNPs Microgel Releases Drugs in Response to AMF Application.
Please click here to view a larger version of this figure.
Figure 3. A Schematic Illustration of the Potential Mechanism by Which Gelatin/p (NIPAM-co-AAm)/MNPs Microgel Releases Drugs in Response to AMF Application.
Please click here to view a larger version of this figure.
Discussion
The technology described here demonstrates a proof of concept on the use of nanoparticle-microgel hybrids for magneto-thermally triggered drug release. This was achieved by physically entrapping MNPs and p(NIPAM-co-AAm) chains within a microscale three-dimensional gelatin network crosslinked by genipin. The magnetic field-responsive platform was sufficient to generate heat within the microgel in response to a remotely applied AMF, which in turn triggered the release of a model drug, BSA.
A strategy to embed both MNPs and p(NIPAM-co-AAm) appears to be critical for achieving a desired drug release from the gelatin microgel, since the extent of BSA release from gelatin/MNPs microgel in the absence of p(NIPAM-co-AAm) was significantly lower than the one from microgel incorporating p(NIPAM-co-AAm), even though the extent of temperature increase to AMF application were similar in both types of microgels (Figure 2C and 2D). We demonstrated that the deswelling behavior of gelatin/p(NIPAM-co-AAm) microgel is induced by the shrinkage of p(NIPAM-co-AAm) polymer chains in response to an increase in temperature; moreover, the deswelling behavior positively correlates with the extent of drug release from the microgel8. Taken together, this supports that the shrinkage of p(NIPAM-co-AAm) due to MNPs heating may be the main driving force for the BSA release from gelatin/p(NIPAM-co-AAm)/MNPs microgels.
We previously reported that the application of a high frequency AMF to MNPs could trigger increase in temperature on the surface of MNPs in a manner that is proportional to the magnitude of AMF strength and concentrations of MNPs25. It has been shown that AMF strength of 5 - 30 kA/m is sufficient to induce an appropriate heating on the surface of MNPs9,25,26. Thus, the extent of drug release from gelatin/p(NIPAM-co-AAm)/MNPs microgel can be tuned by appropriately changing parameters, which include the amount of p(NIPAM-co-AAm), crosslinking time, the amount of MNPs, and AMF parameters (field intensity, frequency, and duration of exposure).
In our protocol for fabricating magneto-thermally responsive microgels, the most critical step is the covalent crosslinking of gelatin gel particles in genipin solution. Careful control of the crosslinking time and temperature, as well as maintaining homogeneity of the microgel suspension in the genipin solution, is required to achieve desired gel elasticity, which may influence the microgel responsivity. After crosslinking, the removal of unreacted genipin molecules is also an important step.
The gelatin has been shown to be biocompatible with low immunogenicity and enzymatically degradable8,27. The chemical crosslinker, genipin, has been considered to be non-toxic28. Thus, our gelatin-based drug delivery platform exhibiting characteristics of magnetic responsivity and suitable biodegradability may offer a useful tool for tissue engineering application as an on-demand drug carrier.
However it should be also noted that the current protocol has limitations. First, the microgels made by water-in-oil emulsification method generally exhibit a polydispersity, which may result in heterogeneity in encapsulation of drugs and MNPs among particles. Microfluidics can be a good alternative to overcome this limitation29. Second, the current drug delivery system still has a limitation that it must be used at a body temperature of 37 ˚C due to a small degree of deswelling characteristic at the temperature, associated with a relatively low value of LCST (~ 34 ˚C) for poly(NIPAM-co-AAm) polymer used in this study. The use of thermoresponsive polymer that can exhibit a higher LCST may overcome this issue30.
Disclosures
The authors have nothing to disclose.
Acknowledgments
This study was supported by Farris Family Innovation Award and NIH 1R01NR015674-01 to MK. The authors thank Josep Nayfach (Qteris, Inc) for providing an electro-magnetic generator system as well as his technical consultation. The authors also thank Huan Yan (LCI & Chemical Physics Interdisciplinary Program, Kent State University) for her technical assistants.
References
- Langer R. Biomaterials in drug delivery and tissue engineering: one laboratory's experience. Acc. Chem. Res. 2000;33:94–101. doi: 10.1021/ar9800993. [DOI] [PubMed] [Google Scholar]
- Rivest CM, Morrison D, Ni B, Rubib J, Yadav V, Mahdavi A, Karp J, Khademhosseini A. Microscale hydrogels for medicine and biology: synthesis, characteristics and applications. J Mech Mater Struct. 2007;2:1103–1119. [Google Scholar]
- Kawaguchi H. Thermoresponsive microhydrogels: preparation, properties and applications. Polym. Int. 2014;63:925–932. [Google Scholar]
- Vinogradov SV. Colloidal microgels in drug delivery applications. Curr. Pharm. Des. 2006;12:4703–4712. doi: 10.2174/138161206779026254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liechty WB, Kryscio DR, Slaughter BV, Peppas NA. Polymers for drug delivery systems. Annu Rev Chem Biomol Eng. 2010;1:149–173. doi: 10.1146/annurev-chembioeng-073009-100847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumari A, Yadav SK, Yadav SC. Biodegradable polymeric nanoparticles based drug delivery systems. Colloids Surf. B Biointerfaces. 2010;75:1–18. doi: 10.1016/j.colsurfb.2009.09.001. [DOI] [PubMed] [Google Scholar]
- Shibayama M, Tanaka T. Volume Phase-Transition and Related Phenomena of Polymer Gels. Adv Polym Sci. 1993;109:1–62. [Google Scholar]
- Sung B, Kim C, Kim MH. Biodegradable colloidal microgels with tunable thermosensitive volume phase transitions for controllable drug delivery. J Colloid Interface Sci. 2015;450:26–33. doi: 10.1016/j.jcis.2015.02.068. [DOI] [PubMed] [Google Scholar]
- Kumar CS, Mohammad F. Magnetic nanomaterials for hyperthermia-based therapy and controlled drug delivery. Adv. Drug Deliv. Rev. 2011;63:789–808. doi: 10.1016/j.addr.2011.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mura S, Nicolas J, Couvreur P. Stimuli-responsive nanocarriers for drug delivery. Nat. Mater. 2013;12:991–1003. doi: 10.1038/nmat3776. [DOI] [PubMed] [Google Scholar]
- Kong SD, et al. Magnetic field activated lipid-polymer hybrid nanoparticles for stimuli-responsive drug release. Acta biomaterialia. 2013;9:5447–5452. doi: 10.1016/j.actbio.2012.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayashi K, et al. Magnetically responsive smart nanoparticles for cancer treatment with a combination of magnetic hyperthermia and remote-control drug release. Theranostics. 2014;8:834–844. doi: 10.7150/thno.9199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki D, Kawaguchi H. Stimuli-sensitive core/shell template particles for immobilizing inorganic nanoparticles in the core. Colloid Polym Sci. 2006;284:1443–1451. [Google Scholar]
- Bhattacharya S, Eckert F, Boyko V, Pich A. Temperature-, pH-, and magnetic-field-sensitive hybrid microgels. Small. 2007;3:650–657. doi: 10.1002/smll.200600590. [DOI] [PubMed] [Google Scholar]
- Wong JE, Gaharwar AK, Muller-Schulte D, Bahadur D, Richtering W. Dual-stimuli responsive PNiPAM microgel achieved via layer-by-layer assembly: Magnetic and thermoresponsive. J Colloid Interf Sci. 2008;324:47–54. doi: 10.1016/j.jcis.2008.05.024. [DOI] [PubMed] [Google Scholar]
- Zhao X, et al. Active scaffolds for on-demand drug and cell delivery. Proc. Natl. Acad. Sci. U.S.A. 2011;108:67–72. doi: 10.1073/pnas.1007862108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu F, et al. Release of magnetic nanoparticles from cell-encapsulating biodegradable nanobiomaterials. ACS nano. 2012;6:6640–6649. doi: 10.1021/nn300902w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li YH, et al. Magnetic Hydrogels and Their Potential Biomedical Applications. Adv Funct Mater. 2013;23:660–672. [Google Scholar]
- Cooperstein MA, Canavan HE. Assessment of cytotoxicity of (N-isopropyl acrylamide) and poly(N-isopropyl acrylamide)-coated surfaces. Biointerphases. 2013;8:19. doi: 10.1186/1559-4106-8-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jorgensen L, Moeller EH, van de Weert M, Nielsen HM, Frokjaer S. Preparing and evaluating delivery systems for proteins. Eur J Pharm Sci. 2006;29:174–182. doi: 10.1016/j.ejps.2006.05.008. [DOI] [PubMed] [Google Scholar]
- Holland TA, Tabata Y, Mikos AG. In vitro release of transforming growth factor-beta 1 from gelatin microparticles encapsulated in biodegradable, injectable oligo(poly(ethylene glycol) fumarate) hydrogels. J Control Release. 2003;91:299–313. doi: 10.1016/s0168-3659(03)00258-x. [DOI] [PubMed] [Google Scholar]
- Liang HC, Chang WH, Lin KJ, Sung HW. Genipin-crosslinked gelatin microspheres as a drug carrier for intramuscular administration: in vitro and in vivo studies. J Biomed Mater Res. Part A. 2003;65:271–282. doi: 10.1002/jbm.a.10476. [DOI] [PubMed] [Google Scholar]
- Solorio L, Zwolinski C, Lund AW, Farrell MJ, Stegemann JP. Gelatin microspheres crosslinked with genipin for local delivery of growth factors. J Tissue Eng Regen Med. 2010;4:514–523. doi: 10.1002/term.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Regmi R, et al. Hyperthermia controlled rapid drug release from thermosensitive magnetic microgels. J Mater Chem. 2010;20:6158–6163. [Google Scholar]
- Kim MH, et al. Magnetic nanoparticle targeted hyperthermia of cutaneous Staphylococcus aureus infection. Ann Biomed Eng. 2013;41:598–609. doi: 10.1007/s10439-012-0698-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivkov R, et al. Application of high amplitude alternating magnetic fields for heat induction of nanoparticles localized in cancer. Clin Cancer Res. 2005;11:7093s–7103s. doi: 10.1158/1078-0432.CCR-1004-0016. [DOI] [PubMed] [Google Scholar]
- Huang S, Fu X. Naturally derived materials-based cell and drug delivery systems in skin regeneration. J Control Release. 2010;142:149–159. doi: 10.1016/j.jconrel.2009.10.018. [DOI] [PubMed] [Google Scholar]
- Malafaya PB, Silva GA, Reis RL. Natural-origin polymers as carriers and scaffolds for biomolecules and cell delivery in tissue engineering applications. Adv. Drug Deliv. Rev. 2007;59:207–233. doi: 10.1016/j.addr.2007.03.012. [DOI] [PubMed] [Google Scholar]
- Shah R, Kim J, Agresti J, Weitz D, Chu L. Fabrication of monodisperse thermosensitive microgels and gel capsules in microfluidic devices. Soft Matter. 2008;4:2303–2309. [Google Scholar]
- Hoare T, et al. Magnetically triggered nanocomposite membranes: a versatile platform for triggered drug release. Nano letters. 2011;11:1395–1400. doi: 10.1021/nl200494t. [DOI] [PMC free article] [PubMed] [Google Scholar]


