Abstract
Individuals with autism spectrum disorder (ASD) experience higher rates of psychopathology than their typically developing peers or peers with other intellectual or developmental disabilities. Little is known about the developmental course of psychiatric symptoms such as internalizing and externalizing behaviors in this population. Individual characteristics and aspects of the family environment may explain variability in outcomes for adults with ASD. The present study extends our current understanding of psychopathology among individuals with ASD by examining group-based trajectories of internalizing and externalizing symptoms in adulthood. Overall, the results showed that symptoms became less severe over time. Distinct patterns of change in psychopathology were observed and associated with differential profiles of psychotropic medication use, comorbid mental health diagnoses, and residential placement. The likelihood of following each developmental trajectory was estimated based on characteristics of the adults with ASD (gender, adaptive behavior, and autistic symptoms) and maternal expressed emotion (criticism and warmth). Maternal criticism and warmth were identified as key risk and protective factors, respectively, with important implications for future research and intervention for individuals with ASD.
Autism spectrum disorders (ASDs) are neurodevelopmental disorders involving core impairments in social functioning and communication (Dawson, 2008; Landa, Holman, & Garrett-Mayer, 2007), occurring in approximately 1 in 68 children in the United States (Centers for Disease Control, 2014). Individuals with ASD experience heightened levels of psychopathology compared to their typically developing peers and peers with other intellectual and developmental disabilities (Bradley, Summers, Wood, & Bryson, 2004; Brereton, Tonge, & Einfeld, 2006; Hastings & Mount, 2001; McClintock, Hall, & Oliver, 2003). In adulthood, individuals with ASD present with high and persistent problem behaviors and psychiatric symptoms (Hutton, Goode, Murphy, Couteur, & Rutter, 2008; Mouridsen, Rich, Isager, & Nedergaard, 2008) as well as elevated rates of psychiatric disorders, particularly anxiety and depression (Billstedt, Gillberg, & Gillberg, 2005; Farley et al., 2009; Larsen & Mouridsen, 1997; Mouridsen et al., 2008).
Given the high prevalence of psychopathology among adults with ASD, it is necessary to chart the course of psychiatric symptoms starting earlier in adolescence and adulthood. The present analyses draw on a multicohort longitudinal study of adolescents and adults with ASD (a) to present variations in the developmental course of psychopathology among individuals with ASD from early to late adulthood, as measured by maternal report of internalizing and externalizing symptoms and (b) to identify individual and environmental risk factors for internalizing and externalizing symptoms in this population.
Developmental Course of Internalizing and Externalizing Symptoms
Internalizing and externalizing symptoms are key indicators of psychopathology that can be assessed through parent report across the lifespan. Presence of these symptoms in childhood and adolescence increases the risk of psychiatric diagnoses in adulthood (Cicchetti & Toth, 1991). Internalizing symptoms include anxiety, sadness, social withdrawal, and fearfulness while externalizing symptoms include overactivity, poor impulse control, noncompliance, and aggression (Achenbach & Edelbrock, 1981; Werry & Quay, 1971). These dimensions were initially based on clinical classification systems but were later validated empirically as distinct dimensions of behavior (Ciccchetti & Toth, 1991). Although there is a moderate degree of concordance between these dimensions (Kraatz Keiley, Bates, Dodge, & Pettit, 2000), internalizing and externalizing symptoms are each associated with unique risk factors and psychiatric disorders (Ormel et al., 2005; Williams et al., 2009).
Levels of internalizing and externalizing behaviors have been shown to decline into adulthood in the general population (Achenbach & Rescorla, 2003; Hofstra, van der Ende, & Verhulst, 2000). A similar pattern is observed for individuals with ASD and other developmental disorders (Murphy et al., 2005; Shattuck et al., 2007; Totsika, Felce, Kerr, & Hastings, 2010). Despite declines, however, behavioral and emotional problems remain high in adulthood for individuals with ASD (Gray et al., 2012). Moreover, a pattern of amelioration in behavioral and emotional symptoms is not uniform across individuals in this population (Anderson, Maye, & Lord, 2011). Individuals with ASD show a greater range of trajectories in behavioral and emotional symptoms than their typically developing peers. Into adulthood, Gray et al. (2012) documented a general pattern of decline in behavioral and emotional problems over time among individuals with ASD, yet some experienced no change (22.5%) or even increases (15.7%) in problems. Heterogeneity in change in internalizing and externalizing symptoms has been observed among individuals with other intellectual and developmental disabilities as well (Forster, Gray, Taffe, Einfeld, & Tonge, 2011; Hauser-Cram & Woodman, 2015). Taken together, these findings highlight the need to explore variations in the developmental course of internalizing and externalizing symptoms among adults with ASD. There may be subgroups of adults with ASD who experience little improvement or worsening of symptoms over time.
Predictors of Internalizing and Externalizing Symptoms
The likelihood of following various trajectories may relate to individual and environmental characteristics. Similar to typically developing individuals, gender may play a role. In the general population, women's greater self-regulation and sensitivity to interpersonal concerns increases their vulnerability to internalizing problems, while greater aggression and socialization practices relating to self-assertion may place men at higher risk for externalizing problems (Leadbeater, Kuperminc, Blatt, & Hertzog, 1999; Zahn-Waxler, Shirtcliff, & Marceau, 2008). The findings regarding potential gender differences in individuals with ASD are mixed (Gray et al., 2012; Solomon, Miller, Taylor, Hinshaw, & Carter, 2012; Worley & Matson, 2011). Additional research is needed to clarify the contribution of gender to psychopathology in this population, particularly during adulthood.
Beyond gender, risk for psychopathology may differ by level of functioning. Specific to individuals with ASD, functioning can be represented by adaptive behavior or the severity of impairment in symptoms of autism. Adaptive behavior refers to an overarching set of skills that an individual demonstrates in day to day life, including daily living skills such as self-care and preparing meals. These skills are related to general intelligence but provide a more nuanced representation of an individual's strengths and limitations (Paskiewicz, 2009). The severity of impairments in the core symptoms of ASD represents an additional index of level of functioning. The core symptoms of ASD include impairments in social interaction, communication, and restricted repetitive and stereotyped patterns of behavior, interests, and activities (American Psychiatric Association, 2000). Though correlated, measures of adaptive behavior and autistic symptoms represent distinct aspects of an individual's functioning in everyday life.
The findings regarding the impact of level of functioning on internalizing and externalizing symptoms are mixed. Several studies have reported greater symptoms among individuals with lower levels of adaptive behavior (McCarthy & Boyd, 2001; Totsika, Toogood, Hastings, & Lewis, 2008) and more severe autism symptoms (Anderson et al., 2011). In contrast, other studies report elevated behavioral and emotional symptoms among individuals with fewer deficits in functioning (Forster et al., 2011; Taffe, Tonge, Gray, & Einfeld, 2008). Given the limited literature on the link between level of functioning and symptoms of psychopathology in individuals with ASD, it is unclear whether adults with higher or lower functional skills are at risk for developing symptoms of psychopathology.
Beyond individual characteristics, there is evidence that aspects of the family environment can influence behavioral and emotional development among individuals with ASD, from early toddlerhood through adulthood (Baker, Neece, Fenning, Crnic, & Blacher, 2010; Baker, Seltzer, & Greenberg, 2011; Greenberg, Seltzer, Hong, & Orsmond, 2006; Smith, Greenberg, Seltzer, & Hong, 2008). Expressed emotion (EE) represents one critical aspect of the family environment that has been linked to outcomes for individuals with ASD. EE measures key aspects of interpersonal relationships in everyday family life through parent narrative, such as criticism, hostility, warmth, positive comments, and emotional overinvolvement (Wearden, Tarrier, Barrowclough, Zastowny, & Rahill, 2000). The criticism dimension of EE captures the degree to which a caregiver exhibits disapproval toward a child. Criticism measured through parent narrative has been shown to relate to behavioral observations of antagonism, negativity, disgust, harshness, and lower responsiveness (McCarty, Lau, Valeri, & Weisz, 2004). Within families of children with ASD, higher levels of maternal criticism predicted greater externalizing behaviors, above and beyond type of disability and age as well as maternal anxiety and distress (Hastings, Daley, Burns, & Beck, 2006). Maternal criticism was also found to predict greater behavior problems among adolescents and adults with ASD (Baker et al., 2010).
Exclusive focus on negative aspects of family relationships masks our understanding of the impact of positive family processes on development. Maternal affect and the quality of parent–child interactions have long been demonstrated to predict child adaptation and functioning (Borkowski, Ramey, & Bristol-Powers, 2001; Overbeek, Stattin, Vermulst, Ha, & Engels, 2007). Within families of adolescents and adults with ASD, Smith et al. (2008) found aspects of the mother–child relationship, including closer relationship quality and higher levels of warmth and praise, to relate to lower levels of autistic symptoms and behavior problems.
Long-Term Impacts of Internalizing and Externalizing Symptoms
Heightened levels of internalizing and externalizing symptoms relate to compromised social and academic competence and adult psychiatric disorders for individuals with ASD (Chadwick, Walker, Bernard, & Taylor, 2000; de Bildt, Sytema, Kraijer, Sparrow, & Minderaa, 2005; Kim, Szatmari, Bryson, Streiner, & Wilson, 2000). Internalizing and externalizing problems are associated with lower quality of life outcomes in this population, including more limited social integration, leisure activities, health and security, and self-determination (Gerber, Baud, Giroud, & Carminati, 2008). Internalizing issues have also been linked to later mood and social relationship problems, such as greater self-reported feelings of loneliness, more depressive symptoms, and greater difficulties with friendships among individuals with ASD (Anderson et al., 2011).
The Present Study
The present study aimed to address current gaps in the literature on the development of psychopathology among individuals with ASD. The first aim was to present group-based trajectories of internalizing and externalizing symptoms using maternal report, because these symptoms are key indicators of psychopathology (Cicchetti & Toth, 1991). Prior research suggests heterogeneity in change in psychopathology among individuals with ASD (Anderson et al., 2011; Gray et al., 2012); therefore, we expect the developmental course of symptoms to differ by group. In line with findings from previous studies using similar group-based methods with individuals with intellectual and developmental disabilities (Anderson et al., 2011; Hauser-Cram & Woodman, 2015), we expect the analyses will reveal a small group of individuals with chronically high, or possibly increasing, levels of psychopathology over time. We expect an additional small group will display chronically low levels of psychopathology over time, with the remaining majority of individuals showing patterns of moderate symptoms over time. The findings are expected to highlight a high-risk group of adults with ASD in need of intervention and treatment.
The relationship between internalizing and externalizing trajectories within individuals was also examined in order to improve our understanding of the co-occurrence of these symptoms over time. Given the heterogeneity in change in internalizing and externalizing symptoms observed in previous research (Forster et al., 2011; Hauser-Cram & Woodman, 2015), we expect some individuals will show different patterns of change on these dimensions. In other words, some individuals may display high rates of internalizing symptoms but moderate to low rates of externalizing symptoms, and vice versa. Longitudinal data on the interplay of internalizing and externalizing symptoms is mixed, with some studies finding internalizing symptoms to exacerbate externalizing symptoms while others find the reverse direction of causation (Masten et al., 2005).
The second aim was to address the extent to which characteristics of the individuals with ASD (gender, autism symptoms, and adaptive behavior) and characteristics of their family environment (maternal criticism and maternal warmth), measured at or before the start of the trajectories, predicted the developmental course of internalizing and externalizing symptoms. Above and beyond characteristics of adults with ASD, individuals whose mother displays higher levels of criticism and lower levels of warmth are expected to have higher levels of psychopathology, based on previous research (Baker et al., 2010; Hastings et al., 2006; Smith et al., 2008). The extent to which trajectory groups correspond with independent indicators of psychopathology (mental health diagnoses or medication use) was presented. We expect individuals with higher levels of internalizing and externalizing symptoms to also show other indicators of psychopathology, including more parent-report mental health diagnosis and greater use of psychotropic medications (Esbensen, Greenberg, Seltzer, & Aman, 2009; Tsakanikos, Costello, Holt, Sturmey, & Bouras, 2007).
Method
Participants
Participants were drawn from an ongoing, longitudinal study of 406 individuals with ASD and their families, the Adolescents and Adults with Autism Study (Seltzer et al., 2003). Analyses in the present study used data from 7 data collection time points: Time 1 (T1, 1998–2000), Time 2 (T2, 2000–2001), Time 3 (T3, 2002–2003), Time 4 (T4, 2004–2005), Time 7 (T7, 2007–2008), Time 8 (T8, 2009–2010), and Time 9 (T9, 2011–2012). Families were recruited in Massachusetts (N = 204) and Wisconsin (N = 202) through agencies, schools, diagnostic clinics, and media announcements. Identical recruitment procedures were used in both states. Families met three criteria at the start of the study: the family included a child with an ASD diagnosis given by an independent medical, psychological, or educational professional; the child with ASD was 10 years of age or older; and the child's scores on the research-administered Autism Diagnostic Interview—Revised (ADI-R; Lord, Rutter, & Le Couteur, 1994) were consistent with an ASD diagnosis.
Of the 406 participants, 384 (94.6%) met criteria for autistic disorder on the ADI-R: qualitative impairments in communication and language, and qualitative impairments in reciprocal social interaction, repetitive, restrictive, and stereotyped behaviors with an onset of symptoms prior to 36 months. The remaining 22 participants (5.4%) demonstrated a pattern of impairments on the ADI-R that was consistent with a diagnosis of Asperger disorder or pervasive developmental disorder—not otherwise specified. Terminology surrounding autism spectrum disorders has changed over time. We use the term autism spectrum disorders or ASD as an umbrella term for the diagnoses represented in this sample to match language used in recruitment efforts and language used in existing research in the field. It is not certain all participants would meet criteria for ASD according to the DSM-5.
The present sample consists of 259 families for which data on the outcome variables were available (T7, T8, and T9). Slightly more than half of the families were from Wisconsin (53%). The majority of participants with ASD were male (75%). Seventy percent had a comorbid diagnosis of intellectual disability, consistent with the estimated prevalence of intellectual disability among individuals with ASD more broadly (Fombonne, 2003; Gillberg & Coleman, 1992). Participants ranged from 10 to 48 years of age (M 21.23, SD = 9.04) at T1 (see Table 1). More than half of participants (66%) lived in the family home at the start of the study. Most parents were married (79%) at that time. Fifty-eight percent of mothers had an associate's degree or higher. Maternal age ranged from 32 to 81 years (M = 50.77, SD = 10.05). More than half of mothers (67%) were employed. Compared to the full sample of 406 families, the mothers in this sample were more likely to have an associate's degree or higher, t (258) = 2.14, p = .03. No sample differences were significant for adult gender, age, and residential status or parental marital status, education, employment, age, or state at T1. The majority of the sample (73%) participated in T7, T8, and T9. Adults with ASD who dropped out of the study after T7 (n = 69) did not differ from those who remained in the study (n = 190) on levels of internalizing or externalizing symptoms at T7.
Table 1.
Summary of data collection
| T1 | T2 | T3 | T4 | T7 | T8 | T9 | |
|---|---|---|---|---|---|---|---|
| Outcome (T7–T9) | |||||||
| Psychopathology (ABC-L) | X | X | X | ||||
| Adult characteristics (T7–T9) | |||||||
| Medication use | X | X | X | ||||
| Mental health diagnoses | X | X | X | ||||
| Adult and family characteristics (T1–T7) | |||||||
| Demographics (maternal education, child gender) | X | ||||||
| Autism symptoms (ADI-R) | X | X | X | X | X | ||
| Adaptive behavior (W-ADL) | X | X | X | ||||
| Maternal criticism and warmth (FMSS) | X | X | X | X | |||
| Participant age | |||||||
| M | 21.23 | 22.87 | 24.37 | 25.98 | 29.50 | 31.06 | 32.24 |
| SD | 9.04 | 9.10 | 9.10 | 9.06 | 8.76 | 8.87 | 8.00 |
| Minimum | 10 | 11 | 12 | 14 | 18 | 19 | 21 |
| Maximum | 48 | 50 | 51 | 53 | 57 | 58 | 60 |
Note: T1, Time 1, 1998–2000; T2, Time 2, 2000–2001; T3, Time 3, 2002–2003; T4, Time 4, 2004–2005; T7, Time 7, 2007–2008; T8, Time 8, 2009–2010; T9, Time 9, 2011–2012; ABC-L, Adult Behavior Checklist; ADI-R, Autism Diagnostic Interview—Revised; W-ADL, Waisman Activities of Daily Living; FMSS, Five Minute Speech Sample.
Measures
The present study used measures across seven data collection time points (see Table 1 for a summary). Internalizing and externalizing symptoms were measured at T7, T8, and T9. Adult and family characteristics measured at or before the start of the trajectories (T1–T7) were aggregated across waves and examined as predictors of trajectories of internalizing and externalizing symptoms (gender, adaptive behavior, and autism symptoms; maternal education, maternal criticism, and warmth). Additional characteristics of the adults with ASD measured during the course of the trajectories (T7–T9) were aggregated across waves and examined as independent indicators of psychopathology in separate analyses (medication use and mental health diagnoses).
Outcome variables (T7–T9)
Internalizing and externalizing symptoms
Mothers completed the Adult Behavior Checklist (ABC-L; Achenbach & Rescorla, 2003) as a measure of internalizing and externalizing symptoms at T7, T8, and T9. Mothers were asked to indicate if a variety of behaviors for their son or daughter within the past 6 months were 0 = not true, 1 = somewhat/sometimes true, or 2 = very/often true. Internalizing symptoms represented scores across three syndrome scales: anxious/depressed (e.g., “complains of loneliness”), somatic complaints (e.g., “feels tired without good reason”), and withdrawn (e.g., “would rather be alone than with others”). Externalizing symptoms represented scores across three syndrome scales: aggressive behavior (e.g., “physically attacks people”), intrusive (e.g., “teases a lot”), and rule-breaking behavior (e.g., “lying and cheating”). Raw scores for internalizing and externalizing symptoms and their accompanying subscales were used as outcome variables. Use of raw scores is recommended for statistical analyses in order to take into account the full range of variation in the scales (Achenbach & Rescorla, 2003). Standardized scores (t scores) were used to report the number of adults in the sample with clinically significant internalizing and externalizing symptoms (t > 63) as well as symptoms on individual scales (t > 69).
The ABC-L has demonstrated good validity and reliability (Achenbach & Rescorla, 2003). The ABC-L is an upward extension of the Child Behavior Checklist, which has been used extensively in research on internalizing and externalizing symptoms in children and adolescents. There is strong evidence for the validity of the Child Behavior Checklist in individuals with ASD (Pandolfi, Magyar, & Dill, 2009, 2012). Among adults with intellectual disability, the ABC-L demonstrated internal consistency, interrater reliability, and concurrent and convergent validity (Tenneij & Hoot, 2007). The Cronbach a values in the present study ranged from 0.68 to 0.94 across scales.
Adult characteristics (T7–T9)
Co-residence
Mothers were asked to indicate whether or not their son or daughter was living in the family home at T7, T8, and T9. The participant was considered co-resident if he or she lived at home at any point during this time point.
Medication use
Mothers were asked to report the name of each prescription medication taken by their son or daughter at T7, T8, and T9. The medications were coded and classified into their respective drug categories based on standard drug classifications in the Physician's Desk Reference (PDR) Drug Guide for Mental Health Professionals (Comer, 2002). Medications were grouped as psychotropic and nonpsychotropic (see Esbensen et al., 2009). Psychotropic medications included antipsychotics, antidepressants, anxiolytics and sedative-hypnotics, central nervous system stimulants, and antimanic medications. Anticonvulsants and hypotensive medications were included in this category for individuals with no comorbid diagnosis of seizure disorder or hypertension, respectively. Nonpsychotropic medications included antilipemics, antibiotics, antiemetics, and medications for thyroid, diabetes, respiration, hormones, ocular, gastrointestinal, and other miscellaneous purposes. Anticonvulsants and hypotensive medications were counted as nonpsychotropic medications for individuals with a comorbid diagnosis of seizure disorder or hypertension, respectively. Over-the-counter medications such as analgesics, laxatives, vitamins, antifungal medication, antacids, and topicals were not counted as medications. The number of reported psychotropic and nonpsychotropic medications was averaged across waves (T7–T9).
Mental health diagnoses
Mothers were asked if they had ever been told by a health care professional (i.e., psychiatrist, physician, or psychologist) that their son or daughter had any of the following diagnoses: anxiety, depression, attention-deficit disorder (ADD), attention-deficit/hyperactivity disorder (ADHD), obsessive compulsive disorder, schizophrenia, or bipolar disorder. Adults with ASD were coded as having (1) or not having (0) each of these diagnoses based on reports across T7, T8, and T9. It should be noted that DSM-IV prevents a diagnosis of ADD/ADHD in the context of ASD. Nevertheless, many mothers in the present study reported that their son or daughter received a co-occurring diagnosis of ADD/ADHD. Research on clinical populations supports the frequent co-occurrence of ADD/ADHD traits in individuals with ASD (Davis & Kollins, 2012) and the revised DSM-5 permits comorbid ADD/ADHD and ASD diagnoses (van der Meer et al., 2012).
Adult and family characteristics (T1–T7)
Demographics
Maternal education was recorded at T1 on an ordinal scale with 1 = high school graduate or less, 2 = some college, 3 = associates or bachelor's degree, and 4 = postbachelor's degree or graduate degree. The gender of the adult with ASD was recorded at T1 as 0 = female and 1 = male.
Autism symptoms
The ADI-R (Lord et al., 1994) was used to measure autism symptoms. The ADI-R was conducted as a standardized interview with the mother at T1, T2, T3, T4, and T7. Items on this measure are based on criteria for an autism diagnosis outlined by the DSM-IV (American Psychiatric Association, 2000) and the International Classification of Diseases (World Health Organization, 1992). Items across three primary symptom domains (repetitive behaviors and restrictive interests, impairments in reciprocal social interaction, and impairments in communication) were coded as 0 = no abnormality present, 1 = possible abnormality, and 2 = definite abnormality. Some items also contained a possible score of 3 = extreme abnormality; however, scores of 2 and 3 were combined as recommended by Lord et al. (1994). The total score for current severity of symptoms was averaged across waves (T1–T7). The interviewers who administered the ADI-R participated in an approved training program. Interrater reliability was high for individual items between two interviewers and two supervising PhD clinical psychologists experienced in the diagnosis of ASD and the ADI-R. The ADI-R has demonstrated good testretest reliability, diagnostic validity, convergent validity, and specificity and sensitivity in past research (Hill et al., 2001; Lord et al., 1997). Cronbach a in the present sample ranged from 0.78 to 0.86 across waves.
Adaptive behavior
Adaptive behavior of the adolescent or adult with ASD was assessed using the Waisman Activities of Daily Living Scale (Maenner et al., 2013) at T1, T4, and T7. Mothers were asked to rate the independence of their son or daughter in 17 activities of daily living (e.g., prepare simple foods and grooming) on a 3-point scale (0 = does not do at all, 1 = could do but does not/does with help, and 2 = independent). Total scores were averaged across waves (T1–T7). The Waisman Activities of Daily Living has demonstrated strong internal consistency and criterion and construct validity for individuals with intellectual disabilities (Maenner et al., 2012). Cronbach a in the present sample ranged from 0.92 to 0.94 across waves.
Criticism and warmth
The Five-Minute Speech Sample (FMSS) was used to code the level of criticism and warmth at T2, T3, T4, and T7, following the standardized procedures outlined in the coding manual developed by Magaña et al. (1986). The mother was asked to speak about her son or daughter with ASD for 5 min without interruption. The speech sample was recorded, transcribed, and coded for levels of criticism and warmth.
Maternal criticism was rated as 0 = low, 3 = borderline, or 5 = high. Mothers were rated as high on criticism if they (a) make a negative opening remark, (b) describe their relationship with their son or daughter in negative terms, or (c) make one or more criticisms about their son or daughter during the speech sample. A count of borderline or high ratings on criticism across waves (T2, T3, T4, and T7) was used to represent maternal criticism; therefore, scores ranged from 0 (never rated high on criticism) to 4 (always rated high on criticism).
Maternal warmth was rated on a 6-point scale from 0 = no warmth to 5 = high warmth. Warmth ratings were based on tone of voice; spontaneity of expression of sympathy, concern, and empathy; and expression of interest in the child. A count of moderately high (4) or high (5) ratings on warmth across waves (T2, T3, T4, and T7) was used to represent a maternal warmth; therefore, scores ranged from 0 (never rated as moderately high/high on warmth) to 4 (always rated moderately high/high on warmth).
All ratings were performed by an independent researcher with extensive experience in coding the FMSS. A second experienced researcher independently coded a subsample of transcripts (N = 30) with moderate agreement (83.3%, κ = 0.67). There is good correspondence between the FMSS and the full Camberwell Family Interview (Magaña et al., 1986). This measure has been used previously in studies of expressed emotion in families raising children with developmental disabilities (Beck, Daley, Hastings, & Stevenson, 2004). Additional information on use of the FMSS in the present sample can be found in Esbensen et al. (2009). Mothers’ self-report characteristics of the broader autism phenotype, as measured at T7 using the Broad Autism Phenotype Questionnaire (Hurley, Losh, Parlier, Reznick, & Piven, 2007), were unrelated to ratings of warmth (r = .03, p = .63) and criticism (r = .02, p = .78).
Analytic plan
The distributions of the outcome variables were checked for normality. Scores on anxious/depressed, somatic complaints, aggressive behavior, and rule-breaking behavior were positively skewed. The results did not differ for raw and transformed values on these variables; therefore, results using the raw values were reported to facilitate interpretation. Missing data on predictor variables (9%) were imputed using the Markov Chain Monte Carlo procedure in SPSS version 19. Estimates were pooled across five imputed data sets. Pooling results across multiple imputed data sets is recommended because excluding cases with missing data biases estimates and reduces statistical power (Widaman, 2006).
A semiparametric group-based method (Jones, Nagin, & Roeder, 2001; Nagin, 1999, 2005) was used to identify distinct trajectories of symptoms among adults with ASD. This method was designed to identify clusters of individuals with similar developmental pathways. Internalizing and externalizing symptoms were examined as a function of age of the adult with ASD (years) using the PROC TRAJ procedure in SAS (described in Jones et al., 2001). Trajectories therefore represent developmental trends rather than changes within individuals across three waves.
To address the first research aim, an unconditional model was fit to identify the number and shape of trajectory groups for each symptom scale. The Bayesian information criterion (BIC) was used to identify the best fitting model, as recommended by Nagin (2005). As an additional estimate of model fit, the posterior probabilities of group membership were evaluated (see Nagin, 2005). An average posterior probability of 0.70 or higher for individuals assigned to a given group is considered evidence of acceptable model fit (Nagin, 2005). When graphing the unconditional models, trajectories were truncated to the age range represented by members of each group to most accurately represent the data and avoid extrapolation. As part of the first research aim of this study, the joint probability of membership in internalizing and externalizing trajectory groups was estimated. Building off univariate models for each outcome, the dual model estimates the joint probability of membership in any given combination of groups across outcomes (Nagin & Tremblay, 2001). Additional information on estimation of joint trajectories using PROC TRAJ can be found in Jones and Nagin (2007).
To address the second research aim, multinomial logistic regression was used to test the extent to which characteristics of the adults with ASD and their mothers predicted trajectory group membership. The likelihood of membership in each trajectory group was compared to the likelihood of membership in the trajectory group with the lowest level of symptoms over time (i.e., Group 1). In the present analyses, trajectory group membership based on psychopathology across waves T7, T8, and T9 was predicted by adult and family characteristics measured from T1 to T7 (controlling for the adult's age). Profiles of adults with ASD in each internalizing and externalizing trajectory group were constructed based on medication use and mental health diagnoses (T7–T9), with cases weighted by their probability of membership in each group so that more prototypical cases contributed more to that group's profile. In addition, the unweighted descriptive statistics for the full sample were reported.
Results
Descriptive statistics and comparisons by gender
Three indices were used to describe scores on the ABC-L: raw scores; T scores, which are standardized by age and gender; and the percentage of individuals with scores in the clinical range. The descriptive statistics across syndrome scales are presented in Table 2, with comparisons by gender. Women showed lower anxious/depressed T scores, which indicates that the women with ASD in this sample showed lower levels of symptoms of anxiety and depression relative to the norms for their female peers, as compared to men with ASD in this sample relative to the norms for their male peers. Women had higher T scores for rule-breaking behavior and intrusive as well as overall externalizing behaviors, indicating that women with ASD in this sample had higher symptoms on these scales relative to the norms for their female peers than did men with ASD relative to the norms for their male peers.
Table 2.
Descriptive statistics and clinical cutoffs for syndrome scales averaged across Times 7, 8, and 9
| Men (N = 194) |
Women (N = 65) |
Independent Samples t Test |
||||||
|---|---|---|---|---|---|---|---|---|
| Raw Score |
T Score |
Raw Score |
T Score |
Raw Score |
T Score |
|||
| M (SD) | M (SD) | Clinical Rangea | M (SD) | M (SD) | Clinical Rangea | t (df = 257) | t (df = 251) | |
| Internalizing symptoms | 13.66 (8.01) | 59.16 (8.19) | 49% (25.3%) | 14.10 (7.66) | 58.46 (7.56) | 12% (18.5%) | –0.20 | –2.21 |
| Anxious/depressed | 5.84 (4.80) | 58.34 (7.53) | 23% (11.9%) | 5.71 (4.56) | 56.01 (6.72) | 4% (6.2%) | –0.20 | –2.34* |
| Somatic complaints | 2.25 (2.20) | 55.71 (6.06) | 14% (7.2%) | 2.88 (2.48) | 56.07 (5.86) | 10% (15.4%) | –0.14† | 1.50 |
| Withdrawn | 5.57 (3.30) | 62.91 (8.42) | 64% (33.0%) | 5.51 (2.96) | 64.69 (7.77) | 29% (44.6%) | –0.14 | 1.57 |
| Externalizing symptoms | 14.24 (9.75) | 56.43 (7.83) | 28% (14.4%) | 16.42 (9.43) | 59.65 (8.12) | 17% (26.2%) | 1.93 | 0.41** |
| Aggressive behavior | 6.87 (5.61) | 57.51 (7.23) | 14% (7.2%) | 8.39 (5.79) | 58.73 (6.79) | 5% (7.7%) | 1.82† | 0.41 |
| Intrusive | 2.58 (2.02) | 54.78 (4.59) | 9% (4.6%) | 3.11 (1.91) | 57.47 (5.22) | 4% (6.2%) | 1.87† | 1.20*** |
| Rule breaking behavior | 4.78 (3.54) | 58.24 (5.66) | 11% (5.7%) | 4.93 (3.26) | 60.35 (6.42) | 12% (18.5%) | 1.84 | 1.24* |
Percentage of participants in the clinical range across Time 7, 8, or 9.
p < .10.
p < .05.
p < .01.
p < .001.
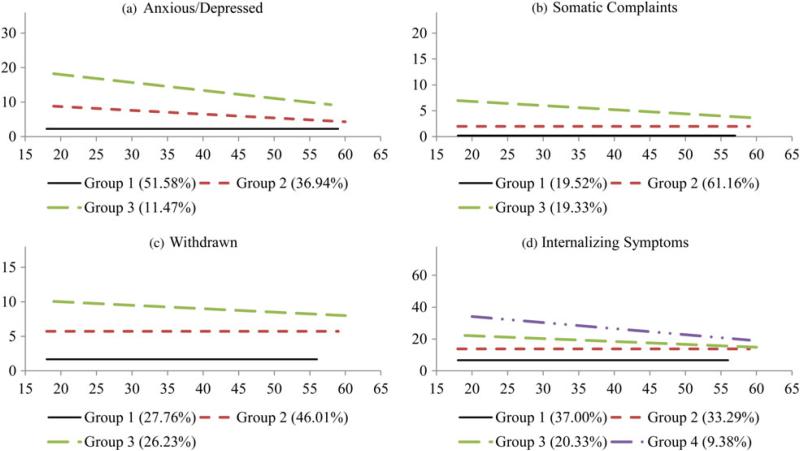
Trajectories of internalizing symptoms
The first aim of the study was to describe trajectories of internalizing and externalizing symptoms for groups of adults with ASD. A three group model fit best (based on BIC scores) for anxious/depressed (Figure 1a), somatic complaints (Figure 1b), and withdrawn (Figure 1c) syndrome scales. For each scale, Group 1 reflected participants with low and stable symptoms over time. This group was dominant for anxious/depressed symptoms. Group 2 displayed moderate symptom levels that either declined (anxious/depressed) or remained stable (somatic complaints and withdrawn) across development. This pattern was dominant for somatic complaints and withdrawn symptoms. For each outcome, Group 3 was identified as the most problematic group, with the highest level of symptoms. Across syndrome scales, however, levels were found to decline for this elevated group. For internalizing symptoms overall, a four-group model fit best (Figure 1d). The largest group showed low but stable symptoms over time (Group 1), followed by another group with stable symptoms at slightly higher levels (Group 2). A third group had moderately elevated symptoms that declined slightly over time (Group 3). The final group had the highest levels in adolescence that declined over time (Group 4).
Figure 1.
(Color online) Trajectories of internalizing symptoms: (a) anxious/depressed, (b) somatic complaints, (c) withdrawn, and (d) internalizing symptoms.
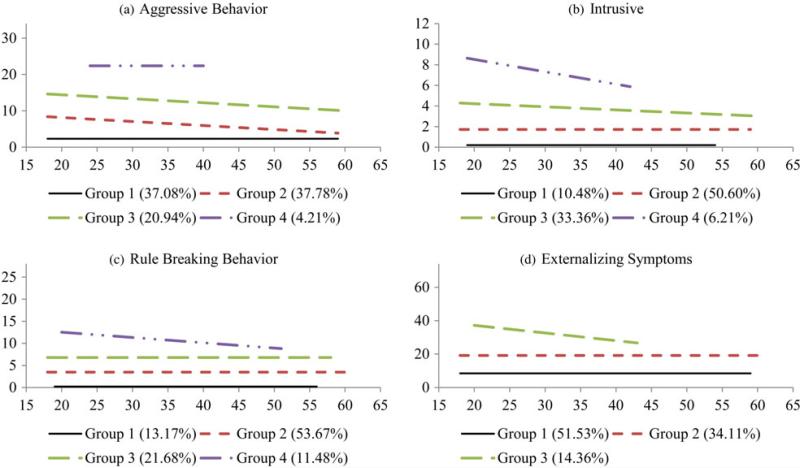
Trajectories of externalizing symptoms
A four-group model fit best (based on BIC scores) for aggressive behavior (Figure 2a), intrusive (Figure 2b), and rule-breaking behavior (Figure 2c) syndrome scales. Similar to syndrome scales for internalizing symptoms, severity increased with group number. Group 1 for each outcome showed low and stable symptoms over time. Group 2 displayed slightly higher levels that either declined (aggressive behavior) or remained stable (intrusive and rule-breaking behavior) across development. This pattern was the dominant pattern across syndrome scales. Group 3 showed even higher symptom levels that declined for aggressive behavior and intrusive but remained stable for rule-breaking behavior. The final group (Group 4) consisted of participants with the highest level of symptoms over time. For aggressive behavior, this high group maintained a stable level of symptoms, while the highest group for intrusive and rule-breaking behavior declined. For externalizing symptoms overall (Figure 2d), a three-group model fit best. Slightly more than half experienced low and stable symptoms over time (Group 1), while over one third showed moderate levels of symptoms that remained constant across development (Group 2). The final group showed elevated symptoms during adolescence that slowly decreased through middle adulthood (Group 4).
Figure 2.
(Color online) Trajectories of externalizing symptoms: (a) aggressive, (b) intrusive, (c) rule-breaking behavior, and (d) externalizing symptoms.
Model fit
Adults with ASD were assigned to each group with 87% confidence for internalizing symptom scales and 88% confidence for externalizing symptom scales, exceeding the criterion for adequate model fit of 70% (Nagin, 2005). The average age of participants in each group did not significantly differ by trajectory group for any outcome. In other words, age of the adults with ASD did not relate to the probability of membership in a particular trajectory group. Patterns of participation across T7, T8, and T9 likewise did not significantly differ by trajectory group. It was therefore not the case that individuals who dropped out of the study after T7 or T8 were more likely to be in a particular trajectory group.
Joint trajectories of internalizing and externalizing symptoms
Table 3 shows the probability of jointly following each of the internalizing and externalizing trajectories. On the diagonal, we see three patterns of correspondence between levels of internalizing and externalizing problems: low on both outcomes, moderate and stable on both outcomes, and high but declining on both outcomes. More than half (66.4%) demonstrated a pattern of correspondence. The remaining third (33.6%) of the sample showed a divergent pattern. Nine percent of participants displayed consistently low externalizing symptoms but moderate and stable levels of internalizing symptoms. An additional 7% showed consistently low externalizing symptoms coupled with high and declining internalizing symptoms. Very few participants showed a pattern of high and declining externalizing symptoms with moderate and stable levels of internalizing symptoms.
Table 3.
Joint probability of internalizing trajectory group and externalizing trajectory group
| Externalizing Trajectory Group | Internalizing Trajectory Group |
||
|---|---|---|---|
| Group 1 | Group 2 | Groups 3 & 4 | |
| Group 1 | 28.8% | 8.6% | 6.6% |
| Group 2 | 7.8% | 23.2% | 8.3% |
| Group 3 | <0.1% | 1.5% | 14.4% |
Predictors of trajectory group membership
The second aim of the study was to examine characteristics of the adults with ASD and their families as predictors of trajectory group membership. The likelihood of membership in each trajectory group was compared to the likelihood of membership in the trajectory group with the lowest level of symptoms over time (Group 1). The findings from the multivariate, multinomial logistic regression models are described below.
Internalizing symptoms
Compared to a pattern of low and steady anxious/depressed symptoms (Group 1), the likelihood of membership in Group 2 was increased by a history of higher adaptive behavior (Table 4). The odds of membership in Group 2 are increased by 5%, with each additional unit increase in adaptive behavior. The likelihood of membership in Group 3 was increased by a history of higher adaptive behavior and lower maternal warmth. The odds of membership in Group 3 are increased by 9% with each additional unit increase in adaptive behavior. With each time point a mother was rated as high in warmth, the odds of her child with ASD belonging in Group 3 for anxious/depressed symptoms were reduced by 33%. For somatic complaints, the likelihood of membership in Group 3 was increased by a history of lower maternal warmth. With each count of high maternal warmth, the odds of adults with ASD belonging in Group 3 for somatic complaints decreased by 32%.
Table 4.
Multinomial logistic regression predicting trajectory membership for internalizing scales
| Anxious/Depressed |
Somatic Complaints |
Withdrawn |
Internalizing Symptoms |
||
|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | ||
| Group 1 | Reference group | Reference group | Reference group | Reference group | |
| Group 2 | Maternal education | 1.06 (0.81, 1.39) | 0.82 (0.61, 1.10) | 0.96 (0.73, 1.26) | 1.03 (0.79, 1.35) |
| Maternal criticism | 1.55 (1.16, 2.08)** | 0.77 (0.56, 1.05)† | 1.13 (0.84, 1.52) | 1.08 (0.82, 1.44) | |
| Maternal warmth | 0.93 (0.72, 1.19) | 0.91 (0.69, 1.19) | 0.84 (0.66, 1.08) | 0.76 (0.60, 0.97)* | |
| Age | 0.97 (0.93, 1.01) | 1.01 (0.97, 1.06) | 0.98 (0.95, 1.02) | 0.97 (0.94, 1.01)† | |
| Gender (male) | 0.83 (0.42, 1.65) | 0.48 (0.21, 1.12)† | 0.70 (0.34, 1.46) | 1.18 (0.59, 2.37) | |
| Autism symptoms | 1.02 (0.91, 1.13) | 1.05 (0.94, 1.17) | 1.09 (0.96, 1.23) | 1.03 (0.91, 1.15) | |
| Adaptive behavior | 0.96 (0.91, 1.01)† | 1.01 (0.95, 1.06) | 0.99 (0.94, 1.05) | 1.00 (0.95, 1.05) | |
| Group 3 | Maternal education | 1.69 (1.06, 2.69) | 0.75 (0.51, 1.09) | 0.93 (0.66, 1.30) | 1.16 (0.84, 1.62) |
| Maternal criticism | 2.26 (1.35, 3.79) | 0.80 (0.54, 1.18) | 1.73 (1.22, 2.45)** | 1.16 (0.83, 1.62) | |
| Maternal warmth | 0.81 (0.53, 1.25)* | 0.66 (0.47, 0.94)* | 0.78 (0.58, 1.05)† | 0.76 (0.56, 1.04)† | |
| Age | 0.97 (0.91, 1.03) | 0.99 (0.93, 1.04) | 0.97 (0.93, 1.02) | 0.94 (0.90, 0.99)* | |
| Gender (male) | 0.42 (0.16, 1.10) | 0.51 (0.18, 1.40) | 0.85 (0.35, 2.08) | 0.95 (0.42, 2.15) | |
| Autism symptoms | 1.04 (0.88, 1.22) | 1.00 (0.87, 1.15) | 1.15 (1.00, 1.31)* | 1.02 (0.90, 1.15) | |
| Adaptive behavior | 0.96 (0.89, 1.04)* | 0.98 (0.91, 1.05) | 1.03 (0.97, 1.10) | 1.06 (1.00, 1.13)† | |
| Group 4 | Maternal education | — | — | — | 1.10 (0.72, 1.69) |
| Maternal criticism | — | — | — | 1.64 (1.04, 2.58)* | |
| Maternal warmth | — | — | — | 0.66 (0.44, 0.99)* | |
| Age | — | — | — | 0.99 (0.94, 1.05) | |
| Gender (male) | — | — | — | 1.22 (0.41, 3.58) | |
| Autism symptoms | — | — | — | 0.98 (0.83, 1.15) | |
| Adaptive behavior | — | — | — | 1.07 (0.99, 1.16)† |
p < .10.
p < .05.
p < .01.
For withdrawn symptoms, adults with ASD were more likely to follow Group 3 than Group 1 if they had a history of higher maternal criticism. Each additional count of high maternal criticism was associated with an 84% increase in the odds of membership in Group 3. For internalizing symptoms overall, a history of higher criticism and lower warmth increased the likelihood of membership in Group 3. Each additional count of high maternal warmth decreased the odds of membership in Group 3 by 23%. For every count of high criticism, the odds of membership in Group 3 for overall internalizing symptoms increased by 66%.
Externalizing symptoms
For aggressive behavior, the likelihood of membership in trajectory Groups 2 and 3 was increased by a history of lower maternal warmth (Table 5). With each additional count of high maternal warmth, the odds of membership in Group 2 decreased by 22% and the odds of membership in Group 3 decreased by 26%. A historyof higher maternal criticism increased the likelihood of membership in Groups 3 and 4. Each additional count of high criticism was associated with a 73% increase in the odds of membership in Group 3 and a 97% increase in the odds of membership in Group 4. A history of higher criticism increased the likelihood of membership in Groups 3 and 4 for intrusive symptoms. The odds of membership in Group 3 were increased by 55% with each additional count of high criticism. The odds of membership in Group 4 were almost tripled by each count of high criticism.
Table 5.
Multinomial logistic regression predicting trajectory membership for externalizing scales
| Aggressive Behavior |
Intrusive |
Rule Breaking Behavior |
Externalizing Symptoms |
||
|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | ||
| Group 1 | Reference group | Reference group | Reference group | Reference group | |
| Group 2 | Maternal education | 0.94 (0.72, 1.23) | 0.82 (0.55, 1.22) | 0.91 (0.63, 1.31) | 1.06 (0.81, 1.39) |
| Maternal criticism | 1.10 (0.83, 1.46) | 1.21 (0.79, 1.86) | 1.52 (1.01, 2.28)* | 1.55 (1.16, 2.08)** | |
| Maternal warmth | 0.79 (0.62, 0.99)* | 0.93 (0.65, 1.32) | 1.05 (0.76, 1.45) | 0.93 (0.72, 1.19) | |
| Age | 1.00 (0.97, 1.04) | 1.00 (0.94, 1.05) | 1.00 (0.95, 1.05) | 0.97 (0.93, 1.01) | |
| Gender (male) | 0.64 (0.31, 1.32) | 1.34 (0.48, 3.78) | 0.84 (0.32, 2.21) | 0.83 (0.42, 1.65) | |
| Autism symptoms | 1.09 (0.97, 1.22) | 0.98 (0.84, 1.14) | 1.10 (0.96, 1.26) | 1.02 (0.91, 1.13) | |
| Adaptive behavior | 1.00 (0.95, 1.05) | 0.98 (0.90, 1.06) | 1.01 (0.94, 1.09) | 0.96 (0.91, 1.01)† | |
| Group 3 | Maternal education | 0.96 (0.68, 1.36) | 1.03 (0.66, 1.58) | 1.20 (0.77, 1.87) | 1.69 (1.06, 2.69)* |
| Maternal criticism | 1.74 (1.23, 2.47)** | 1.55 (0.97, 2.46)† | 1.91 (1.20, 3.05)** | 2.26 (1.35, 3.79)** | |
| Maternal warmth | 0.74 (0.55, 1.01)* | 0.75 (0.51, 1.10) | 0.87 (0.59, 1.29) | 0.81 (0.53, 1.25) | |
| Age | 1.01 (0.96, 1.05) | 1.00 (0.94, 1.06) | 0.97 (0.92, 1.03) | 0.97 (0.91, 1.03) | |
| Gender (male) | 0.51 (0.21, 1.20) | 0.83 (0.28, 2.45) | 0.87 (0.28, 2.66) | 0.42 (0.16, 1.10)† | |
| Autism symptoms | 1.06 (0.93, 1.21) | 0.95 (0.81, 1.12) | 1.18 (1.00, 1.40)* | 1.04 (0.88, 1.22) | |
| Adaptive behavior | 0.99 (0.93, 1.05) | 0.94 (0.86, 1.02) | 1.00 (0.92, 1.09) | 0.96 (0.89, 1.04) | |
| Group 4 | Maternal education | 1.29 (0.64, 2.59) | 1.32 (0.62, 2.79) | 1.37 (0.80, 2.34) | — |
| Maternal criticism | 1.84 (0.93, 3.63)† | 3.22 (1.44, 7.16)** | 2.77 (1.51, 5.08)** | — | |
| Maternal warmth | 0.57 (0.28, 1.17) | 0.66 (0.31, 1.42) | 0.89 (0.51, 1.57) | — | |
| Age | 0.97 (0.87, 1.07) | 0.96 (0.85, 1.08) | 0.98 (0.91, 1.05) | — | |
| Gender (male) | 0.35 (0.08, 1.53) | 0.74 (0.15, 3.81) | 0.71 (0.20, 2.56) | — | |
| Autism symptoms | 1.07 (0.82, 1.38) | 1.01 (0.76, 1.34) | 1.23 (1.00, 1.53)* | — | |
| Adaptive behavior | 0.92 (0.81, 1.05) | 1.05 (0.92, 1.20) | 1.03 (0.93, 1.13) | — |
p < .10.
p < .05.
p < .01.
A history of higher maternal criticism increased the likelihood that adults with ASD would follow the trajectories of Groups 2, 3, and 4 for rule-breaking behavior. With each count of high criticism, the odds of trajectory membership were increased by 52% for Group 2, 102% for Group 3, and 191% for Group 4. Maternal criticism also differentiated trajectories of overall externalizing symptoms. With each additional count of high criticism, the odds of membership in Group 2 were increased by 64% and Group 3 were increased by 141%. In addition, higher levels of maternal education increased the likelihood of membership in Group 3.
Trajectory group profiles
As seen in Table 6, adults with low and stable trajectories of internalizing symptoms reported the lowest use of psychotropic medications. Use of psychotropic medications was higher among adults with elevated trajectories of internalizing symptoms. Adults who demonstrated the highest levels of internalizing symptoms over time (Group 4) also reported the highest use of psychotropic medications on average. The number of mental health diagnoses was also higher among adults with elevated trajectories of internalizing symptoms. Adults in Group 4 were estimated to have 2.4 mental health diagnoses on average, as compared to less than 1 diagnosis on average for adults in Group 1. The proportion of adults with a mental health diagnosis was highest for Group 4, across all diagnosis types. Estimates of anxiety and depression diagnoses were high. The number of adults living in the family home was lowest for the group with the highest levels of internalizing symptoms (Group 4).
Table 6.
Profiles of internalizing trajectory groups weighted by probability of group membership
| Internalizing Symptoms |
|||||
|---|---|---|---|---|---|
| Group 1 |
Group 2 |
Group 3 |
Group 4 |
Unweighted Total |
|
| Characteristic T7–T9 | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) |
| Medication use | |||||
| No. of nonpsychotropic | 1.14 (1.25) | 1.17 (1.34) | 1.10 (1.41) | 1.10 (1.30) | 1.14 (1.49) |
| No. of psychotropic | 1.22 (1.19) | 1.31 (1.18) | 1.27 (1.21) | 1.91 (1.34) | 1.33 (1.26) |
| No. of mental health diagnoses | 0.85 (1.14) | 1.13 (1.14) | 1.32 (1.09) | 2.36 (1.23) | 1.18 (1.21) |
| Anxiety | 0.26 (0.44) | 0.40 (0.49) | 0.53 (0.50) | 0.80 (0.41) | 0.41 (0.49) |
| Depression | 0.06 (0.25) | 0.11 (0.31) | 0.13 (0.34) | 0.63 (0.49) | 0.14 (0.35) |
| ADD/ADHD | 0.20 (0.41) | 0.20 (0.40) | 0.23 (0.43) | 0.25 (0.44) | 0.21 (0.41) |
| OCD | 0.27 (0.45) | 0.34 (0.48) | 0.36 (0.49) | 0.49 (0.51) | 0.33 (0.47) |
| Schizophrenia | 0.00 (0.00) | 0.01 (0.09) | 0.02 (0.16) | 0.09 (0.29) | 0.02 (0.13) |
| Bipolar disorder | 0.06 (0.03) | 0.09 (0.03) | 0.08 (0.04) | 0.20 (0.09) | 0.09 (0.28) |
| Coresidence | 0.35 (0.48) | 0.47 (0.50) | 0.43 (0.50) | 0.28 (0.46) | 0.40 (0.49) |
Note: T7–T9, Time 7–Time 9; ADD/ADHD, Attention-deficit disorder/attention-deficit/hyperactivity disorder; OCD, obsessive compulsive disorder; coresidence, in parental home.
As seen in Table 7, adults with low and stable trajectories of externalizing symptoms reported the lowest use of psychotropic medications. Adults with moderate and stable levels of externalizing symptoms reported the highest number of medications. The number of mental health diagnoses was higher among adults with elevated trajectories of externalizing symptoms. Group 3 had the highest representation of each mental health disorder, with the exception of bipolar disorder. The number of adults living in the family home was lowest for the group with the highest levels of externalizing symptoms (Group 3).
Table 7.
Profiles of externalizing trajectory groups weighted by probability of group membership
| Externalizing Symptoms |
||||
|---|---|---|---|---|
| Group 1 |
Group 2 |
Group 3 |
Unweighted Total |
|
| Characteristic T7–T9 | M (SD) | M (SD) | M (SD) | M (SD) |
| Medication use | ||||
| No. of nonpsychotropic | 1.07 (1.32) | 1.16 (1.31) | 1.42 (1.52) | 1.14 (1.49) |
| No. of psychotropic | 1.14 (1.17) | 1.62 (1.20) | 1.40 (1.39) | 1.33 (1.26) |
| No. of mental health diagnoses | 0.91 (1.08) | 1.43 (1.29) | 1.78 (1.24) | 1.18 (1.21) |
| Anxiety | 0.33 (0.47) | 0.48 (0.50) | 0.63 (0.49) | 0.41 (0.49) |
| Depression | 0.11 (0.32) | 0.19 (0.40) | 0.16 (0.37) | 0.14 (0.35) |
| ADD/ADHD | 0.17 (0.38) | 0.24 (0.43) | 0.32 (0.48) | 0.21 (0.41) |
| OCD | 0.28 (0.45) | 0.38 (0.49) | 0.47 (0.51) | 0.33 (0.47) |
| Schizophrenia | 0.00 (0.06) | 0.03 (0.17) | 0.04 (0.19) | 0.02 (0.13) |
| Bipolar disorder | 0.05 (0.21) | 0.12 (0.33) | 0.20 (0.41) | 0.09 (0.28) |
| Coresidence | 0.40 (0.49) | 0.41 (0.50) | 0.35 (0.48) | 0.40 (0.49) |
Note: T7–T9, Time 7–Time 9; ADD/ADHD, Attention-deficit disorder/attention-deficit/hyperactivity disorder; OCD, obsessive compulsive disorder; coresidence, in parental home.
Discussion
This study extends our current understanding of the development of psychopathology among individuals with ASD by examining trajectories of internalizing and externalizing symptoms into adulthood, a period of development in which there has been little longitudinal research to date. As expected, groups of individuals with ASD showed distinct patterns of change over time, with a small group of individuals displaying heightened internalizing and externalizing symptoms over time. By using data from a multicohort, longitudinal study, we identified the potential positive influence of high maternal warmth and low maternal criticism on later trajectories of internalizing and externalizing symptoms. We will discuss our findings relating to the developmental course of internalizing and externalizing symptoms (Aim 1). Then, we will discuss predictors of the developmental course of these outcomes (Aim 2). Finally, we highlight important implications for intervention and future research.
Aim 1: Variations in the developmental course of internalizing and externalizing symptoms
On average, symptoms of psychopathology abated from adolescence through adulthood, in line with patterns of change observed in adults with typical development (Achenbach & Rescorla, 2003; Hofstra et al., 2000) and other intellectual and developmental disabilities (Murphy et al., 2005; Richardson & Koller, 1996). The results from the present study reinforce the notion that the developmental course of psychopathology may be more alike than different for individuals with and without disabilities, although overall levels of psychopathology remain problematic. Nearly one quarter of the sample showed clinically significantinternalizing symptoms andclose toone third showed clinically significant externalizing symptoms in adulthood.
A general pattern of improvement across development was observed, yet change was not uniform across groups. This study builds upon previous evidence of distinct patterns of change in psychopathology among children and adolescents with ASD (Anderson et al., 2011; Gray et al., 2012) by explicitly modeling group-based trajectories using current statistical techniques (Jones et al., 2001; Nagin, 2005) and by extending trajectories into adulthood. Across symptom scales, up to one half of the sample evidenced consistently low symptoms over time. These findings offer a positive and hopeful perspective on outcomes for adults with ASD, which may be masked by general reports of heightened psychopathology in this clinical population. By contrast, a number of adults with ASD in this sample showed elevated symptoms that declined to varying degrees over time. For instance, 14% of the sample showed high levels of both internalizing and externalizing symptoms. It may be the case that research and intervention efforts should focus on this subgroup of individuals at heightened risk. The adults who followed the highest trajectories of internalizing and externalizing symptoms showed the greatest use of psychotropic medication and comorbid mental health diagnoses, underscoring the utility of internalizing and externalizing symptoms as indicators of psychopathology in this population. These adults with heightened trajectories were also less likely to be living in the family home, likely due to residential placement as a result of parent and family stress. Alternatively, characteristics of their community living environments may have engendered a heightened risk of psychopathology. Future research is needed to explore the direction of these effects.
When jointly considering internalizing and externalizing symptoms, a general pattern of correspondence emerged, but there were variations around this general pattern of association, suggesting distinct profiles of symptoms. Among those who experienced high and declining trajectories of internalizing symptoms, for instance, approximately one quarter displayed low and stable patterns of externalizing symptoms. These findings further highlight the range of trajectories of behavioral and emotional problems among individuals with ASD (Anderson et al., 2011; Gray et al., 2012).
Aim 2: Identification of individual and environmental risk factors
Maternal expressed emotion
Expressed emotion is a characteristic of the family environment that may augment existing vulnerabilities to psychopathology (Hooley & Gotlib, 2000). A history of high maternal criticism increased the likelihood of following heightened trajectories of psychopathology in adulthood. Maternal criticism was strongly associated with externalizing symptoms in particular. Mothers who were rated as high in criticism over a 10-year period had children who displayed higher trajectories of aggressive, intrusive, and rule-breaking behavior as well as overall externalizing behaviors. Criticism has been previously noted to have a stronger impact on externalizing than on internalizing behaviors (Baker et al., 2000; McCarty & Weisz, 2002; Peris & Baker, 2000). Maternal criticism also predicted heightened trajectories of withdrawn symptoms and overall internalizing symptoms in the present study, however, suggesting that maternal criticism may have broader implications for symptoms of psychopathology in adults with ASD.
While criticism represents a critical explanatory family process, an exclusive focus on negative aspects of family relationships prevents appreciation of the importance of positive family processes. Above and beyond criticism, maternal warmth was predictive of trajectories of internalizing and externalizing symptoms among adults with ASD in this study. More specifically, more frequent ratings of high maternal warmth over a 10-year period decreased the likelihood of individuals following trajectories of high somatic complaints, overall internalizing symptoms, and aggressive behavior in adulthood. In other words, higher maternal warmth was associated with trajectories of lower symptoms in these domains. These findings are consistent with previous work demonstrating the link between maternal warmth and reduced problematic behaviors in individuals with ASD (Smith et al., 2008). The results from the present study support the notion that various aspects of the family environment have differential effects on outcomes for children and adults (McCarty & Weisz, 2002), because criticism and warmth had independent effects on outcomes in this study.
Adult characteristics
Characteristics of the adults with ASD played a lesser role in predicting trajectories of psychopathology. In line with the findings of Gray et al. (2012), gender did not contribute to risk for internalizing or externalizing symptoms in the present study above and beyond autism symptoms, adaptive behavior, and maternal expressed emotion. Women in this sample did show a greater risk of psychopathology compared to their same-gendered peers, however. With respect to intrusive, rule-breaking, and overall externalizing behaviors, women with ASD departed from the norms for their female peers to a greater extent than did men with ASD in comparison to their male peers. A similar pattern was reported for internalizing problems within a small sample of adolescents with ASD (Solomon et al., 2012). Teen girls with ASD had higher symptoms of depression and anxiety compared to their typically developing female peers, but teen boys with ASD did not show a similar risk compared to their male peers. Of note, boys and girls with ASD did not differ in levels of depression and anxiety in that study. It is unclear why women in the present sample showed vulnerabilities in externalizing behaviors, because the opposite pattern is generally observed. These findings regarding differences in t scores should be interpreted with caution becaues the men and women in this sample were not matched on other relevant characteristics. Nevertheless, the results contribute to the growing literature on gender differences in ASD.
The level of functioning of the adults with ASD was less predictive of psychopathology than was maternal expressed emotion. Autistic symptoms and adaptive behavior were unrelated to most facets of internalizing and externalizing symptoms. As an exception, higher levels of adaptive behavior increased the risk of high and declining levels of anxious and depressed behaviors over time. It may be the case that individuals with ASD are more independent as a result of higher levels of adaptive behavior and therefore have greater exposure to negative experiences with peers (Mayes, Calhoun, Murray, & Zahid, 2011). Alternatively, it may not be adaptive behavior per se, but rather increased self-awareness that contributes to higher symptoms of anxiety and depression. Differences between themselves and their peers may be more salient to these higher functioning individuals. Among children and adolescents with Asperger syndrome, social comparison processes are predictive of depressive symptoms (Hedley & Young, 2006; Vickerstaff, Heriot, Wong, Lopes, & Dossetor, 2006).
Implications for intervention
There is evidence to suggest that maternal criticism and warmth are dynamic aspects of the family environment amenable to intervention. Interventions have shown positive effects on EE in caregivers of several populations with heightened internalizing and externalizing problems, including individuals with schizophrenia (Lenior, Dingemans, Schene, Hart, & Linszen, 2002; Tomas et al., 2011), depressive disorders (Katsuki et al., 2011), and eating disorders (Sepulveda et al., 2010). Several scholars have argued that similar interventions may effectively reduce parental EE within families of children and adults with ASD (Greenberg et al., 2006; Hastings & Lloyd, 2007). Improvements in maternal expressed emotion were observed after mothers of adolescents with ASD participated in an 8-week, multifamily group psychoeducation program, Transitioning Together (Smith, Greenberg, & Mailick, 2012, in press). This a promising model of intervention for parents of individuals with ASD, although additional research is needed to evaluate its long-term impacts.
Limitations and future directions
This study is not without its limitations. First, the sample is primarily of Caucasian descent, thereby limiting the generalizability to other racial or ethnic groups. Second, the mothers included in present analyses had higher levels of education than mothers in the original sample. The results should therefore be extended to other socioeconomic groups with caution. An third limitation is the reliance on mother report for measures of adult psychopathology. It could be the case that mothers with higher criticism and lower warmth perceive their child's behavior more negatively. This study focused on internalizing and externalizing symptoms as key indicators of psychopathology. We linked trajectories of symptoms to medication use and parent-report mental health diagnoses as an additional validity check. In line with previous work with adults with intellectual disabilities (Tenneij & Koot, 2007), the present findings support the validity of the ABCL in adults with ASD. Future research should incorporate additional measures of psychopathology, such as adult self-report of internalizing and externalizing symptoms or clinical diagnostic assessments.
We employed longitudinal data to test the hypothesis that earlier maternal EE related to later adult psychopathology, controlling for the level of functioning of the adult with ASD. The reverse direction of effects may also hold true, although a study of adults with ASD found maternal criticism to predict later internalizing and asocial behaviors, but not the reverse (Greenberg et al., 2006). Future work should further examine the relationship between EE and psychopathology over time in families of adults with ASD.
The sample was evaluated using DSM-IV criteria, given the period during which the sample was recruited. There is concern that individuals diagnosed with pervasive developmental disorder or Asperger syndrome following the DSM-IV criteria will not receive an ASD diagnosis according to the DSM-5 criteria. Research indicates that approximately 90% of those with an existing pervasive developmental disorders would be classified with ASD using the current DSM-5 criteria, however (Huerta, Bishop, Duncan, Hus, & Lord, 2012). Because only 5% of our sample met criteria for pervasive developmental disorder or Asperger syndrome, it is unlikely our results would differ if the sample were restricted to individuals who met current criteria for ASD. Nevertheless, use of DSM-IV criteria limits the generalizability of the findings to individuals with ASD diagnosed today.
Despite its limitations, this study addressed critical gaps in the literature on psychopathology among adults with ASD. For adults with ASD, there are significant long-term consequences of internalizing and externalizing symptoms, including lower social integration, leisure activities, and health and higher feelings of loneliness, depressive symptoms, and difficulties with friendships (Anderson et al., 2011; Gerber et al., 2008). Using longitudinal data from multiple cohorts, individual and environmental risk factors for the development of distinct patterns of internalizing and externalizing symptoms were identified. Following the results of this study, interventions for families of individuals with ASD should target maternal expressed emotion. Interventions aimed at reducing levels of criticism and promoting levels of warmth may function to lessen the odds of adults with ASD following trajectories of heightened symptoms, although additional research is needed in this area. Despite improvements in symptoms over time, rates of clinically significant behavior, mental health diagnoses and psychotropic medication use were high in this sample, underscoring the need to identify and manage symptoms of psychopathology in adults with ASD (Filipek et al., 2000).
Acknowledgments
This manuscript was prepared with support from National Institute on Aging Grant R01 AG08768 (to M.R.M., principal investigator) and National Institute on Child Health & Human Development Grant P30 HD03352 (to M.R.M., principal investigator). We also thank the families who participated in this research.
References
- Achenbach TM, Edelbrock CS. Behavioral problems and competencies reported by parents of normal and disturbed children aged four through sixteen. Monographs of the Society for Research in Child Development. 1981;46:1–82. [PubMed] [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASEBA Adult Forms & Profiles. University of Vermont, Research Center for Children, Youth, and Families; Burlington, VT: 2003. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 2000. [Google Scholar]
- Anderson DK, Maye MP, Lord C. Changes in maladaptive behaviors from midchildhood to young adulthood in autism spectrum disorder. American Journal of Intellectual and Developmental Disabilities. 2011;116:381–397. doi: 10.1352/1944-7558-116.5.381. doi:10.1352/1944-7558-116.5.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker BL, Heller TL, Henker B. Expressed emotion, parenting stress, and adjustment in mothers of young children with behavior problems. Journal of Child Psychology and Psychiatry. 2000;41:907–915. [PubMed] [Google Scholar]
- Baker BL, Neece CL, Fenning RM, Crnic KA, Blacher J. Mental disorders in five-year-old children with or without developmental delay: Focus on ADHD. Journal of Clinical Child and Adolescent Psychology. 2010;39:492–505. doi: 10.1080/15374416.2010.486321. doi:10.1080/15374416.2010.486321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker JK, Seltzer MM, Greenberg JS. Longitudinal effects of adaptability on behavior problems and maternal depression in families of adolescents with autism. Journal of Family Psychology. 2011;25:601–609. doi: 10.1037/a0024409. doi:10.1037/a0024409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck A, Daley D, Hastings RP, Stevenson J. Mothers’ expressed emotion towards children with and without intellectual disabilities. Journal of Intellectual Disability Research. 2004;48:628–638. doi: 10.1111/j.1365-2788.2003.00564.x. doi:10.1111/j.1365-2788.2003.00564.x. [DOI] [PubMed] [Google Scholar]
- Billstedt E, Gillberg C, Gillberg C. Autism after adolescence: Population-based 13- to 22-year follow-up study of 120 individuals with autism diagnosed in childhood. Journal of Autism and Developmental Disorders. 2005;35:351–360. doi: 10.1007/s10803-005-3302-5. doi:10.1007/s10803-005-3302-5. [DOI] [PubMed] [Google Scholar]
- Borkowski JG, Ramey SL, Bristol-Power M. Parenting and the child’s world: Influences on academic, intellectual, and social–emotional development. Erlbaum; Mahwah, NJ: 2001. [Google Scholar]
- Bradley EA, Summers JA, Wood HL, Bryson SE. Comparing rates of psychiatric and behavior disorders in adolescents and young adults with severe intellectual disability with and without autism. Journal of Autism and Developmental Disorders. 2004;34:151–161. doi: 10.1023/b:jadd.0000022606.97580.19. doi:10.1023/B:JADD.0000022606.97580.19. [DOI] [PubMed] [Google Scholar]
- Brereton AV, Tonge BJ, Einfeld SL. Psychopathology in children and adolescents with autism compared to young people with intellectual disability. Journal of Autism and Developmental Disorders. 2006;36:863–870. doi: 10.1007/s10803-006-0125-y. doi:10.1007/s10803-006-0125-y. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control Prevalence of autism spectrum disorders among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2010. Morbidity and Mortality Weekly Report. 2014;63:1–21. [PubMed] [Google Scholar]
- Chadwick O, Walker N, Bernard S, Taylor E. Factors affecting the risk of behaviour problems in children with severe intellectual disability. Journal of Intellectual Disability Research. 2000;44:108–123. doi: 10.1046/j.1365-2788.2000.00255.x. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Toth SL, editors. Internalizing and externalizing expressions of dysfunction. Erlbaum; Hillsdale, NJ: 1991. [Google Scholar]
- Comer RJ. PDR [physician's desk reference] drug guide for mental health professionals. Thomson Medical Economics; Montvale, NJ: 2002. [Google Scholar]
- Davis NO, Kollins SH. Treatment for co-occurring attention deficit/hyperactivity disorder and autism spectrum disorder. Neurotherapeutics. 2012;9:518–530. doi: 10.1007/s13311-012-0126-9. doi:10.1007/s13311-012-0126-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson G. Early behavioral intervention, brain plasticity, and the prevention of autism spectrum disorder. Development and Psychopathology. 2008;20:775–803. doi: 10.1017/S0954579408000370. doi:10.1017/S0954579408000370. [DOI] [PubMed] [Google Scholar]
- de Bildt A, Sytema S, Kraijer D, Sparrow S, Minderaa R. Adaptive functioning and behaviour problems in relation to level of education in children and adolescents with intellectual disability. Journal of Intellectual Disability Research. 2005;49:672–681. doi: 10.1111/j.1365-2788.2005.00711.x. doi:10.1111/j.1365-2788.2005.00711.x. [DOI] [PubMed] [Google Scholar]
- Esbensen AJ, Greenberg JS, Seltzer MM, Aman MG. A longitudinal investigation of psychotropic and non-psychotropic medication use among adolescents and adults with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2009;39:1339–1349. doi: 10.1007/s10803-009-0750-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farley MA, McMahon WM, Fombonne E, Jenson WR, Miller J, Gardner M, et al. Twenty-year outcome for individuals with autism and average or near-average cognitive abilities. Autism Research. 2009;2:109–118. doi: 10.1002/aur.69. doi:10.1002/aur.69. [DOI] [PubMed] [Google Scholar]
- Filipek PA, Accardo PJ, Ashwal S, Baranek GT, Cook EJ, Dawson G, et al. Practice parameter: Screening and diagnosis of autism: Report of the Quality Standards Subcommittee of the American Academy of Neurology and the Child Neurology Society. Neurology. 2000;55:468–479. doi: 10.1212/wnl.55.4.468. [DOI] [PubMed] [Google Scholar]
- Fombonne E. The prevalence of autism. Journal of the American Medical Association. 2003;289:87–89. doi: 10.1001/jama.289.1.87. doi:10.1001/jama.289.1.87. [DOI] [PubMed] [Google Scholar]
- Forster S, Gray KM, Taffe J, Einfeld SL, Tonge BJ. Behavioural and emotional problems in people with severe and profound intellectual disability. Journal of Intellectual Disability Research. 2011;55:190–198. doi: 10.1111/j.1365-2788.2010.01373.x. doi:10.1111/j.1365-2788.2010.01373.x. [DOI] [PubMed] [Google Scholar]
- Gerber F, Baud MA, Giroud M, Carminati GG. Quality of life of adults with pervasive developmental disorders and intellectual disabilities. Journal of Autism and Developmental Disorders. 2008;38:1654–1665. doi: 10.1007/s10803-008-0547-9. doi:10.1007/s10803-008-0547-9. [DOI] [PubMed] [Google Scholar]
- Gillberg C, Coleman M. The biology of the autistic syndromes. 2nd ed. MacKeith Press; London: 1992. [Google Scholar]
- Gray K, Keating C, Taffe J, Brereton A, Einfeld S, Tonge B. Trajectory of behavior and emotional problems in autism. American Journal on Intellectual and Developmental Disabilities. 2012;117:121–133. doi: 10.1352/1944-7588-117-2.121. doi:10.1352/1944-7588-117-2.121. [DOI] [PubMed] [Google Scholar]
- Greenberg JS, Seltzer MM, Hong J, Orsmond GI. Bidirectional effects of expressed emotion and behavior problems and symptoms in adolescents and adults with autism. American Journal on Mental Retardation. 2006;111:229–249. doi: 10.1352/0895-8017(2006)111[229:BEOEEA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Hastings RP, Daley D, Burns C, Beck A. Maternal distress and expressed emotion: Cross-sectional and longitudinal relationships with behavior problems of children with intellectual disabilities. American Journal on Mental Retardation. 2006;111:48–61. doi: 10.1352/0895-8017(2006)111[48:MDAEEC]2.0.CO;2. doi:10.1352/0895-8017(2006)111[48:MDAEEC]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Hastings RP, Lloyd T. Expressed emotion in families of children and adults with intellectual disabilities. Mental Retardation and Developmental Disabilities Research Reviews. 2007;13:339–345. doi: 10.1002/mrdd.20173. doi:10.1002/mrdd.20173. [DOI] [PubMed] [Google Scholar]
- Hastings RP, Mount RH. Early correlates of behavioural and emotional problems in children and adolescents with severe intellectual disabilities: A preliminary study. Journal of Applied Research in Intellectual Disabilities. 2001;14:381–391. doi:10.1046/j.13602322.2001.00079.x. [Google Scholar]
- Hauser-Cram P, Woodman AC. Trajectories of internalizing and externalizing behavior problems in children with developmental disabilities. Journal of Abnormal Child Psychology. 2015:1–11. doi: 10.1007/s10802-015-0055-2. doi:10.1007/s10802-015-0055-2. [DOI] [PubMed] [Google Scholar]
- Hedley D, Young R. Social comparison processes and depressive symptoms in children and adolescents with Asperger syndrome. Autism. 2006;10:139–153. doi: 10.1177/1362361306062020. [DOI] [PubMed] [Google Scholar]
- Hill A, Bölte S, Petrova G, Beltcheva D, Tacheva S, Poustka F. Stability and interpersonal agreement of the interview-based diagnosis of autism. Psychopathology. 2001;34:187–191. doi: 10.1159/000049305. doi:10.1159/000049305. [DOI] [PubMed] [Google Scholar]
- Hofstra MB, van der Ende J, Verhulst FC. Continuity and change of psychopathology from childhood into adulthood: A 14-year follow-up study. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:850–858. doi: 10.1097/00004583-200007000-00013. doi:10.1097/00004583-200007000-00013. [DOI] [PubMed] [Google Scholar]
- Hooley JM, Gotlib IH. A diathesis-stress conceptualization of expressed emotion and clinical outcome. Applied & Preventive Psychology. 2000;9:135–151. doi:10.1016/S0962-1849(05)80001-0. [Google Scholar]
- Huerta M, Bishop SL, Duncan A, Hus V, Lord C. Application of DSM-5 criteria for autism spectrum disorder to three samples of children with DSM-IV diagnoses of pervasive developmental disorders. American Journal of Psychiatry. 2012;169:1056–1064. doi: 10.1176/appi.ajp.2012.12020276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurley RS, Losh M, Parlier M, Reznick JS, Piven J. The broad autism phenotype questionnaire. Journal of Autism and Developmental Disorders. 2007;37:1679–1690. doi: 10.1007/s10803-006-0299-3. [DOI] [PubMed] [Google Scholar]
- Hutton J, Goode S, Murphy M, Couteur AL, Rutter M. New-onset psychiatric disorders in individuals with autism. Autism. 2008;12:373–390. doi: 10.1177/1362361308091650. doi:10.1177/1362361308091650. [DOI] [PubMed] [Google Scholar]
- Jones BL, Nagin DS. Advances in group-based trajectory modeling and an SAS procedure for estimating them. Sociological Methods & Research. 2007;35:542–571. doi:10.1177/0049124106292364. [Google Scholar]
- Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociological Methods & Research. 2001;29:374–393. doi:10.1177/0049124101029003005. [Google Scholar]
- Katsuki F, Takeuchi H, Konishi M, Sasaki M, Murase Y, Naito A, et al. Pre–post changes in psychosocial functioning among relatives of patients with depressive disorders after brief multifamily psychoeducation: A pilot study. BMC Psychiatry. 2011;11:56. doi: 10.1186/1471-244X-11-56. doi:10.1186/1471-244X-11-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JA, Szatmari P, Bryson SE, Streiner DL, Wilson FJ. The prevalence of anxiety and mood problems among children with autism and Asperger syndrome. Autism. 2000;4:117–132. doi:10.1177/1362361300004002002. [Google Scholar]
- Kraatz Keiley M, Bates JE, Dodge KA, Pettit GS. A cross-domain growth analysis: Externalizing and internalizing behaviors during 8 years of childhood. Journal of Abnormal Child Psychology. 2000;28:161–179. doi: 10.1023/a:1005122814723. doi:10.1023/A:1005122814723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landa RJ, Holman KC, Garrett-Mayer E. Social and communication development in toddlers with early and later diagnosis of autism spectrum disorders. Archives of General Psychiatry. 2007;64:853. doi: 10.1001/archpsyc.64.7.853. doi:10.1001/archpsyc.64.7.853. [DOI] [PubMed] [Google Scholar]
- Larsen FW, Mouridsen SE. The outcome in children with childhood autism and Asperger syndrome originally diagnosed as psychotic. A 30-year follow-up study of subjects hospitalized as children. European Child & Adolescent Psychiatry. 1997;6:181–190. doi: 10.1007/BF00539924. doi:10.1007/BF00539924. [DOI] [PubMed] [Google Scholar]
- Leadbeater BJ, Kuperminc GP, Blatt SJ, Hertzog C. A multivariate model of gender differences in adolescents’ internalizing and externalizing problems. Developmental Psychology. 1999;35:1268–1282. doi: 10.1037//0012-1649.35.5.1268. doi:10.1037/0012-1649.35.5.1268. [DOI] [PubMed] [Google Scholar]
- Lenior ME, Dingemans PM, Schene AH, Hart AA, Linszen DH. The course of parental expressed emotion and psychotic episodes after family intervention in recent-onset schizophrenia: A longitudinal study. Schizophrenia Research. 2002;57:183–190. doi: 10.1016/s0920-9964(01)00305-x. doi:10.1016/S0920-9964(01)00305-X. [DOI] [PubMed] [Google Scholar]
- Lord C, Pickles A, McLennan J, Rutter M, Bregman J, Folstein S, et al. Diagnosing autism: Analyses of data from the Autism Diagnostic Interview. Journal of Autism and Developmental Disorders. 1997;27:501–517. doi: 10.1023/a:1025873925661. doi:10.1023/A:1025873925661. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, Le Couteur A. Autism Diagnostic Interview— Revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders. 1994;24:659–685. doi: 10.1007/BF02172145. doi:10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- Maenner MJ, Smith LE, Hong J, Makuch R, Greenberg JS, Mai-lick MR. Evaluation of an activities of daily living scale for adolescents and adults with developmental disabilities. Disability and Health Journal. 2013;6:8–17. doi: 10.1016/j.dhjo.2012.08.005. doi:10.1016/j.dhjo.2012.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magaña AB, Goldstein MJ, Karno M, Miklowitz DJ, Jenkins J, Falloon IR. A brief method for assessing expressed emotion in relatives of psychiatric patients. Psychiatry Research. 1986;17:203–212. doi: 10.1016/0165-1781(86)90049-1. [DOI] [PubMed] [Google Scholar]
- Masten AS, Roisman GI, Long JD, Burt KB, Obradović J, Riley JR, et al. Developmental cascades: Linking academic achievement and externalizing and internalizing symptoms over 20 years. Developmental Psychology. 2005;41:733–746. doi: 10.1037/0012-1649.41.5.733. [DOI] [PubMed] [Google Scholar]
- Mayes SD, Calhoun SL, Murray MJ, Zahid J. Variables associated with anxiety and depression in children with autism. Journal of Developmental and Physical Disabilities. 2011;23:325–337. doi:10.1007/s10882-011-9231-7. [Google Scholar]
- McCarty CA, Lau AS, Valeri SM, Weisz JR. Parent–child interactions in relation to critical and emotionally overinvolved expressed emotion (EE): Is EE a proxy for behavior? Journal of Abnormal Child Psychology. 2004;32:83–93. doi: 10.1023/b:jacp.0000007582.61879.6f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarty CA, Weisz JR. Correlates of expressed emotion in mothers of clinically-referred youth: An examination of the five-minute speech sample. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2002;43:759–768. doi: 10.1111/1469-7610.00090. doi:10.1111/1469-7610.00090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy J, Boyd J. Psychopathology and young people with Down's syndrome: Childhood predictors and adult outcome of disorder. Journal of Intellectual Disability Research. 2001;45:99–105. doi: 10.1046/j.1365-2788.2001.00335.x. doi:10.1046/j.1365-2788.2001.00335.x. [DOI] [PubMed] [Google Scholar]
- McClintock K, Hall S, Oliver C. Risk markers associated with challenging behaviours in people with intellectual disabilities: A meta-analytic study. Journal of Intellectual Disability Research. 2003;47:405–416. doi: 10.1046/j.1365-2788.2003.00517.x. doi:10.1046/j.1365-2788.2003.00517.x. [DOI] [PubMed] [Google Scholar]
- Mouridsen SE, Rich B, Isager T, Nedergaard NJ. Psychiatric disorders in individuals diagnosed with infantile autism as children: A case control study. Journal of Psychiatric Practice. 2008;14:5–12. doi: 10.1097/01.pra.0000308490.47262.e0. doi:10.1097/01.pra.0000308490.47262.e0. [DOI] [PubMed] [Google Scholar]
- Murphy GH, Beadle-Brown J, Wing L, Gould J, Shah A, Holmes N. Chronicity of challenging behaviours in people with severe intellectual disabilities and/or autism: A total population sample. Journal of Autism and Developmental Disorders. 2005;35:405–418. doi: 10.1007/s10803-005-5030-2. doi:10.1007/s10803-005-5030-2. [DOI] [PubMed] [Google Scholar]
- Nagin DS. Analyzing developmental trajectories: A semiparametric, group-based approach. Psychological Methods. 1999;4:139–157. doi: 10.1037/1082-989x.6.1.18. doi:10.1037/1082-989X.4.2.139. [DOI] [PubMed] [Google Scholar]
- Nagin DS. Group-based modeling of development. Harvard University Press; Cambridge, MA: 2005. [Google Scholar]
- Nagin DS, Tremblay RE. Analyzing developmental trajectories of distinct but related behaviors: A group-based method. Psychological Methods. 2001;6:18–34. doi: 10.1037/1082-989x.6.1.18. doi:10.1037/1082-989X.6.1.18. [DOI] [PubMed] [Google Scholar]
- Ormel JJ, Oldehinkel AJ, Ferdinand RF, Hartman CA, De Winter AF, Veenstra RR, et al. Internalizing and externalizing problems in adolescence: General and dimension-specific effects of familial loadings and preadolescent temperament traits. Psychological Medicine. 2005;35:1825–1835. doi: 10.1017/S0033291705005829. doi:10.1017/S0033291705005829. [DOI] [PubMed] [Google Scholar]
- Overbeek G, Stattin H, Vermulst A, Ha T, Engels RCME. Parent–child relationships, partner relationships, and emotional adjustment: A birth-to-maturity prospective study. Developmental Psychology. 2007;43:429–437. doi: 10.1037/0012-1649.43.2.429. doi:10.1037/0012-1649.43.2.429. [DOI] [PubMed] [Google Scholar]
- Pandolfi V, Magyar CI, Dill CA. An initial psychometric evaluation of the CBCL 6–18 in a sample of youth with autism spectrum disorders. Research in Autism Spectrum Disorders. 2009;6:96–108. doi: 10.1016/j.rasd.2011.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandolfi V, Magyar CI, Dill CA. Confirmatory factor analysis of the Child Behavior Checklist 1.5–5 in a sample of children with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2012;39:986–995. doi: 10.1007/s10803-009-0716-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paskiewicz TL. Doctoral dissertation. Temple University; 2009. A comparison of adaptive behavior skills and IQ in three populations: Children with learning disabilities, mental retardation, and autism. [Google Scholar]
- Peris TS, Baker BL. Applications of the expressed emotion construct to young children with externalizing behavior: Stability and prediction over time. Journal of Child Psychology and Psychiatry. 2000;41:457–462. doi:10.1111/1469-7610.00630. [PubMed] [Google Scholar]
- Richardson SA, Koller H. Twenty-two years: Causes and consequences of mental retardation. Harvard University Press; Cambridge, MA: 1996. [Google Scholar]
- Seltzer MM, Krauss MW, Shattuck PT, Orsmond G, Swe A, Lord C. The symptoms of autism spectrum disorders in adolescence and adulthood. Journal of Autism and Developmental Disorders. 2003;33:565–581. doi: 10.1023/b:jadd.0000005995.02453.0b. doi:10.1023/B:JADD.0000005995.02453.0b. [DOI] [PubMed] [Google Scholar]
- Sepulveda AR, Todd G, Whitaker W, Grover M, Stahl D, Treasure J. Expressed emotion in relatives of patients with eating disorders following skills training program. International Journal of Eating Disorders. 2010;43:603–610. doi: 10.1002/eat.20749. doi:10.1002/eat.20749. [DOI] [PubMed] [Google Scholar]
- Shattuck PT, Seltzer MM, Greenberg JS, Orsmond GI, Bolt D, Kring S, et al. Change in autism symptoms and maladaptive behaviors in adolescents and adults with an autism spectrum disorder. Journal of Autism and Developmental Disorders. 2007;37:1735–1747. doi: 10.1007/s10803-006-0307-7. doi:10. 1007/s10803-006-0307-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith LE, Greenberg JS, Mailick MR. Adults with autism: Outcomes, family effects, and the multi-family group psychoeducation model. Current Psychiatry Reports. 2012 doi: 10.1007/s11920-012-0328-1. Advance online publication. doi:10. 1007/s11920-012-0328-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith LE, Greenberg JS, Mailick MR. The family context of autism spectrum disorders: Influence on the behavioral phenotype and quality of life. Child and Adolescent Psychiatric Clinics of North America. doi: 10.1016/j.chc.2013.08.006. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith LE, Greenberg JS, Seltzer MM, Hong J. Symptoms and behavior problems of adolescents and adults with autism: Effects of mother-child relationship quality, warmth, and praise. American Journal on Mental Retardation. 2008;113:387–402. doi: 10.1352/2008.113:387-402. doi:10.1352/2008.113:387-402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon M, Miller M, Taylor SL, Hinshaw SP, Carter CS. Autism symptoms and internalizing psychopathology in girls and boys with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2012;42:48–59. doi: 10.1007/s10803-011-1215-z. doi:10.1007/s10803-011-1215-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taffe JR, Tonge BJ, Gray KM, Einfeld SL. Extracting more information from behaviour checklists by using components of mean based scores. International Journal of Methods in Psychiatric Research. 2008;17:232–240. doi: 10.1002/mpr.260. doi:10.1002/mpr.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tenneij BH, Hoot HM. A preliminary investigation into the utility of the Adult Behavior Checklist in the assessment of psychopathology in people with low IQ. Journal of Applied Research in Intellectual Disabilities. 2007;20:391–400. [Google Scholar]
- Tomas EP, Hurtado G, Noguer S, Domenech C, Garcia M, Lopez N, et al. Effectiveness of family work interventions on schizophrenia: Evidence from a multicentre study in Catalonia. International Journal of Social Psychiatry. 2011;58:587–595. doi: 10.1177/0020764011415595. doi:10.1177/0020764011415595. [DOI] [PubMed] [Google Scholar]
- Totsika V, Felce D, Kerr M, Hastings RP. Behavior problems, psychiatric symptoms, and quality of life for older adults with intellectual disability with and without autism. Journal of Autism and Developmental Disorders. 2010;40:1171–1178. doi: 10.1007/s10803-010-0975-1. doi:10.1007/s10803-010-0975-1. [DOI] [PubMed] [Google Scholar]
- Totsika V, Toogood S, Hastings RP, Lewis S. Persistence of challenging behaviours in adults with intellectual disability over a period of 11 years. Journal of Intellectual Disability Research. 2008;52:446–457. doi: 10.1111/j.1365-2788.2008.01046.x. doi:10.1111/j.1365-2788.2008.01046.x. [DOI] [PubMed] [Google Scholar]
- Tsakanikos E, Costello H, Holt G, Sturmey P, Bouras N. Behavior management problems as predictors of psychotropic medication and use of psychiatric services in adults with autism. Journal of Autism and Developmental Disorders. 2007;37:1080–1085. doi: 10.1007/s10803-006-0248-1. [DOI] [PubMed] [Google Scholar]
- van der Meer JMJ, Oerlemans AM, van Steijn DJ, Lappenschaar MGA, de Sonneville LMJ, Buitelaar JK, et al. Are autism spectrum disorder and attention-deficit/hyperactivity disorder different manifestations of one overarching disorder? Cognitive and symptom evidence from a clinical and population-based sample. Journal of the American Academy of Child & Adolescent Psychiatry. 2012;51:1160–1172. doi: 10.1016/j.jaac.2012.08.024. doi:10.1016/j.jaac.2012.08.024. [DOI] [PubMed] [Google Scholar]
- Vickerstaff S, Heriot S, Wong M, Lopes A, Dossetor D. Intellectual ability, self-perceived social competence, and depressive symptomatology in children with high-functioning autistic spectrum disorders. Journal of Autism and Developmental Disorders. 2007;37:1647–1664. doi: 10.1007/s10803-006-0292-x. [DOI] [PubMed] [Google Scholar]
- Wearden AJ, Tarrier N, Barrowclough C, Zastowny TR, Rahill AA. A review of expressed emotion research in health care. Clinical Psychology Review. 2000;20:633–666. doi: 10.1016/s0272-7358(99)00008-2. [DOI] [PubMed] [Google Scholar]
- Werry JS, Quay HC. The prevalence of behavior symptoms in younger elementary school children. American Journal of Orthopsychiatry. 1971;41:136. doi: 10.1111/j.1939-0025.1971.tb01114.x. [DOI] [PubMed] [Google Scholar]
- Widaman KF. Best practices in quantitative methods for develop-mentalists: Missing data: What to do with or without them. Monographs of the Society for Research in Child Development. 2006;71:42–64. doi: 10.1111/j.1540-5834.2006.07103001.x. doi: http://dx.doi.org.proxy.bc.edu/10.1111/j.1540-5834.2006.00404.x. [DOI] [PubMed] [Google Scholar]
- Williams L, Degnan KA, Perez-Edgar KE, Henderson HA, Rubin KH, Pine DS, et al. Impact of behavioral inhibition and parenting style on internalizing and externalizing problems from early childhood through adolescence. Journal of Abnormal Child Psychology. 2009;37:1063–1075. doi: 10.1007/s10802-009-9331-3. doi:10.1007/s10802-009-9331-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . The ICD-10 classification of mental and behavioral disorders: Clinical descriptions and diagnostic guidelines. Author; Geneva: 1992. [Google Scholar]
- Worley JA, Matson JL. Psychiatric symptoms in children diagnosed with an autism spectrum disorder: An examination of gender differences. Research in Autism Spectrum Disorders. 2011;5:1086–1091. doi:10.1016/j.rasd.2010.12.002. [Google Scholar]
- Zahn-Waxler C, Shirtcliff EA, Marceau K. Disorders of childhood and adolescence: Gender and psychopathology. Annual Review of Clinical Psychology. 2008;4:275–303. doi: 10.1146/annurev.clinpsy.3.022806.091358. doi:10.1146/annurev.clinpsy.3.022806.091358. [DOI] [PubMed] [Google Scholar]