Dear Editor:
Cutaneous metastasis from osteosarcoma is exceedingly rare, with only 11 cases reported in the literature1. Giant cell–rich osteosarcoma is a rare variant of osteosarcoma, accounting for 1%~3% of conventional osteosarcomas2. Herein, we present the rare case of a patient with cutaneous metastasis of giant cell–rich osteosarcoma, which closely resembled a giant cell tumor. Owing to the different prognoses and treatment strategies for these tumors, it is important to ensure that the correct differential diagnosis is made.
A 43-year-old man presented with a 6-month history of nodules on his scalp. He had been diagnosed with giant cell-rich osteosarcoma in his right femur along with metastases to multiple organs, including the lungs and the mandible, 1 year ago. The metastatic lung nodules had increased in size despite 6 months of chemotherapy with ifosfamide, adriamycin, and high-dose methotrexate. Subsequently, oncologists changed the regimen to gemcitabine and docetaxel, but the tumor still progressed. Therefore, the regimen was changed once again, and he was admitted to receive a second cycle of cyclophosphamide and etoposide as a third-line regimen.
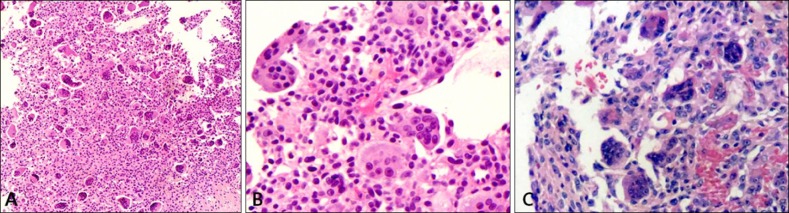
Upon physical examination, several firm skin-colored to erythematous nodules were palpated on his scalp, each measuring approximately 5~12 mm (Fig. 1). Histopathological findings showed many uniformly distributed, multinucleated giant cells containing pleomorphic nuclei. Mononuclear tumor cells had hyperchromatic nuclei with a variety of morphologies, such as round, oval, polygonal, and spindle-shaped (Fig. 2). Although atypical mitoses or dominant osteoid formations were hardly observed, these histological findings were consistent with those of giant cell-rich osteosarcoma, which was previously confirmed by right femur biopsy (Fig. 2). Three months later, he died of sepsis following bone marrow failure caused by the continued chemotherapy.
Fig. 1. Three 5 to 12-mm, flesh-toned to erythematous, firm nodules on the scalp (arrows).
Fig. 2. (A) Hypercellular stroma composed of mononuclear tumor cells and many multinucleated giant cells (H&E, ×40). (B) Mononuclear tumor cells with a variety of morphologies and multinucleated giant cells containing large pleomorphic nuclei (H&E, ×400). (C) Primary tumor of the right femur; numerous multinucleated giant cells and atypical tumor cells (H&E, ×400).
Several studies have reported that giant cell-rich osteosarcomas are sometimes misdiagnosed as giant cell tumors because of their similar clinicopathological features2,3,4. However, these tumors have extremely different clinical courses and prognoses. Giant cell tumors are usually benign with a metastatic rate of <2%, while the clinical course of osteosarcoma is extremely aggressive, with rapid hematogenous systemic dissemination and a tumor-related mortality of 75% within 5 years of diagnosis1,5.
For these reasons, Huang et al.3 suggested the use of some key factors to distinguish these two tumors, including osteoid formation, nuclear pleomorphism, and atypical mitotic figures3. However, osteoid formation cannot be found in small biopsy samples or samples from early lesions4. Tumor cell pleomorphism is not obvious in some cases2. Unless malignant osteoid formation is found, as in this case, it is difficult to confirm an osteosarcoma diagnosis without knowing a patient's cancer history. Unfortunately, not all cases present with features as informative as those in the case reported here.
Among 29 cases of giant cell-rich osteosarcoma, only 1 case of cutaneous metastasis had been reported in English literature2,3,4. With the histological similarity to giant cell tumors, this case emphasizes the value of careful examination of tumor cell pleomorphism and pathological mitoses when patients present with giant cell-rich tumors.
References
- 1.Park SG, Song JY, Song IG, Kim MS, Shin BS. Cutaneous extraskeletal osteosarcoma on the scar of a previous bone graft. Ann Dermatol. 2011;23(Suppl 2):S160–S164. doi: 10.5021/ad.2011.23.S2.S160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang CS, Yin QH, Liao JS, Lou JH, Ding XY, Zhu YB. Giant cell-rich osteosarcoma in long bones: clinical, radiological and pathological features. Radiol Med. 2013;118:1324–1334. doi: 10.1007/s11547-013-0936-9. [DOI] [PubMed] [Google Scholar]
- 3.Huang J, Jiang Z, Zhang H. Clinicopathologic differential diagnosis of giant cell-rich osteosarcoma and giant cell tumor of bone. Zhonghua Bing Li Xue Za Zhi. 2014;43:379–382. [PubMed] [Google Scholar]
- 4.Mariano FV, Corrêa MB, da Costa MV, de Almeida OP, Lopes MA. Labial mucosa metastasis of fibule giant cell-rich osteosarcoma: an unusual presentation. Quintessence Int. 2013;44:783–791. doi: 10.3290/j.qi.a29609. [DOI] [PubMed] [Google Scholar]
- 5.Oliveira AM, Dei Tos AP, Fletcher CD, Nascimento AG. Primary giant cell tumor of soft tissues: a study of 22 cases. Am J Surg Pathol. 2000;24:248–256. doi: 10.1097/00000478-200002000-00011. [DOI] [PubMed] [Google Scholar]